Abstract
Background
Patients can be harmed by receiving too little or too much oxygen. There is ongoing disagreement about the use of oxygen in medical emergencies.
Methods
This was a mixed methods study (survey, telephone interviews and focus groups) involving patients, the public and healthcare professionals (HCPs).
Results
62 patients with chronic obstructive pulmonary disease (COPD), 65 members of the public, 68 ambulance crew members, 22 doctors, 22 nurses and 10 hospital managers took part. For five factual questions about oxygen therapy, the average score for correct answers was 28% for patients with COPD, 33% for the general public and 75% for HCPs. The HCPs had an average score of 66% for five technical questions. Patients (79%) and members of the public (68%) were more likely than HCPs (36%) to believe that oxygen was beneficial in most medical emergencies and less likely to have concerns that it might harm some people (35%, 25% and 68%). All groups had complex attitudes about research into oxygen use in medical emergencies. Many participants would not wish for themselves or their loved ones to have their oxygen therapy determined by a randomised protocol, especially if informed consent was not possible in an emergency situation.
Conclusions
We have found low levels of factual knowledge about oxygen use among patients with COPD and the general public and many false beliefs about the potential benefits and harms of using oxygen. HCPs had a higher level of factual knowledge. All groups had complex attitudes towards research into emergency oxygen use.
Keywords: COPD Exacerbations
Key messages.
Patients with chronic obstructive pulmonary disease and the general public have low levels of factual knowledge about oxygen therapy, they tend to over-estimate potential benefits and under-estimate potential risks of this treatment.
Health care professionals have a higher level of factual knowledge about oxygen therapy but they expressed concerns about lack of training and equipment for the delivery of optimal oxygen therapy.
All three groups had complex attitudes towards research into emergency oxygen use, we have identified some potential barriers to research in this field.
Introduction
Oxygen is the most widely used drug in emergency medicine, given to about one-third of emergency ambulance patients.1 Although oxygen is a useful drug when used to correct hypoxaemia, the potential harmfulness of high concentrations of oxygen in patients with chronic obstructive pulmonary disease (COPD) has been known for over 50 years.2–7 This is important because there are about 130 000 hospital admissions in the UK annually due to acute exacerbations of COPD (AECOPD).2 A 2010 randomised study of oxygen use in AECOPD by Austin et al8 found that mortality doubled (9% vs 4%) when patients were randomised to receive high-concentration oxygen therapy compared with low-dose controlled oxygen therapy titrated to the needs of the patient to avoid harmful hypoxaemia while also avoiding excessive oxygen therapy. Excessive oxygen use may also cause harm or increase mortality in patients with heart attacks or strokes and potentially, at very high doses, may harm patients in intensive care units, including cardiac arrest survivors, although this is disputed by some authors.9–15 Many patients and healthcare professionals (HCPs) have regarded oxygen as a useful drug for virtually all serious medical conditions and a culture of ‘more is better’ evolved over the course of the 20th century.16
Because of these uncertainties, the British Thoracic Society (BTS), together with 21 other Colleges and Societies published a Guideline for Emergency Oxygen Therapy in 2008.13 This guideline recommends setting a target oxygen saturation range for all patients at risk of low oxygen levels (hypoxaemia). The target range is lower for patients with conditions such as COPD which may give rise to type 2 respiratory failure (hypercapnia) than for patients with other medical conditions (88–92% COPD vs 94–98% others).13 The UK Ambulance Service Oxygen Guidance supports these target ranges.17 However, healthcare professionals’ and patients’ attitudes and beliefs about oxygen present challenges to implementation of best practice and may be a barrier to future clinical trials.8 13 16 18 Austin et al8 for example, found that some patients randomised to controlled oxygen therapy were actually given high-concentration oxygen by ambulance teams due to long-established habits. Burls et al16 reported widespread beliefs among HCPs regarding benefits of oxygen in myocardial infarction, which may present difficulties both in securing funding for and undertaking research in this field. Furthermore, audits show that patients with AECOPD are often given high-concentration oxygen therapy.1 6 7 Our aim was, therefore, to explore knowledge, attitudes and beliefs of healthcare professionals, patients with COPD and the general public concerning oxygen therapy (in clinical practice and trials) and also to identify perceived organisational barriers to optimal delivery of oxygen therapy (eg, missing equipment).
Methods
We undertook a mixed-methods exploratory study (involving surveys, interviews and focus groups).19 A mixed methods design was adopted to enable breadth and depth of exploration. Specifically, an explanatory sequential mixed methods approach was employed with the qualitative element used to further explore and seek understanding of responses to the questionnaires.20
Inclusion criteria were: patients with COPD attending hospital clinics; doctors and registered nurses working in A&E or respiratory wards/services, ambulance staff and members of the general public aged 18+ (survey only). Patients were recruited from chest clinics and patient support groups at a large teaching hospital in North-West England. HCPs were recruited from the same hospital and from its related ambulance service by direct contact and by email. Members of the general public were recruited in public spaces in the surrounding hospital area and as friends or contacts of patients with COPD.
The intended sample size for survey completion was 60 patients, 60 members of the general public and 75 HCPs (doctors, nurses, service managers and commissioners, and ambulance staff). The intended sample size for telephone interviews was as follows: 15 patients, 10 ambulance staff, 10 doctors, 10 nurses, 15 health service managers or service commissioners. Four focus groups (one group each for patients; doctors and nurses; ambulance crews and health service managers) were planned, each involving about eight participants. All sample sizes are consistent with the data type.21
Approval was received from relevant research governance and ethics committees (NRES committee South West; Reference 11/SW/0354 and Salford Royal Foundation NHS Trust). Informed verbal consent was obtained prequestionnaire completion and informed written consent (including for audio-recording) was obtained preinterviews and focus groups.
Data collection methods
Survey: Data were collected using study-specific self-complete questionnaires (one version for patients and general public, another for HCPs), with content derived from literature review, pooling of project team knowledge and feedback from patients. Ten questions (five for all participants and five additional questions for HCPs) asked about factual matters, with a single correct answer out of five multiple-choice options. A further five questions examined respondents’ attitudes and opinions and four online supplementary questions (HCPs only) asked about training, equipment and subgroups of patients requiring controlled oxygen therapy (see online appendix for questionnaires and full details of responses). HCPs could complete the questionnaire either on paper or electronically, using ‘Survey Monkey’, with a written reminder that this was an anonymous survey and they should not look up the ‘right answers’ in books or online before completing the questionnaire. HPC invitation letters and emails were sent out via managers. Patients received a paper-based questionnaire distributed either by hand (eg, at clinics, pulmonary rehabilitation sessions or support group meetings) or by post, via designated clinical team members. Members of the general public were offered the choice of completing a paper questionnaire or completing the questionnaire online.
bmjresp-2015-000102supp.pdf (1.7MB, pdf)
Interviews: Audio-recorded telephone interviews were undertaken with both HCPs and patients.19 21 A ‘focused conversation’-style interview approach was adopted, using key items from the questionnaire as a topic guide.
Focus groups: A ‘dual moderator’, audio-recorded approach was adopted.22 Discussion was focused using a topic guide, addressing key issues from the questionnaire. The same topics were used in all interviews and focus groups with probes and prompts adapted for the specific groups.
Data analysis
Questionnaire data were entered into SPSS V.16.0 and analysed descriptively per group (ie, patients, general community, doctors, nurses and paramedics). Interview and focus group recordings were transcribed verbatim and analysed using ‘Framework Analysis’.23 This allowed comparison of findings within and between groups/data sources. Framework analysis is an approach to qualitative data analysis, which is widely used in health services research and is particularly useful where multiple data sources are being compared, as was the case in the present study. We followed the steps in analysis as indicated by Ritchie and Spencer that is, transcription; familiarisation; coding; developing an analytical framework; applying the analytical framework; charting data into the framework matrix and interpreting the data.24
Results
Sixty-five members of the public, 62 patients with COPD and 122 HCPs completed the questionnaires; 49 participants completed telephone interviews and 13 participants took part in focus groups (see table 1 for details). The study ran from March 2012 to May 2013.
Table 1.
Number of participants in each part of the study
| Public | Patients with COPD | Managers and commissioners |
Doctors | Nurses | Ambulance crews | ||
|---|---|---|---|---|---|---|---|
| Questionnaires | 65 | 62 | 10 | 22 | 22 | 68 | |
| (Target) | (60) | (60) | (15) | (20) | (20) | (20) | |
| Paper | 65 | 62 | 8 | 1 | 5 | 4 | |
| Electronic | 0 | 0 | 2 | 21 | 17 | 64 | |
| Gender | |||||||
| Male | 26 | 27 | |||||
| Female | 37 | 29 | |||||
| Not stated | 2 | 6 | |||||
| Age ranges | |||||||
| 16–39 | 12 | NA | Years qualified | ||||
| 40–49 | 11 | NA | 0–5 | 10 | 20 | 22 | 62 |
| 50–59 | 18 | 9 | ≥6 | 0 | 0 | 0 | 0 |
| 60–69 | 11 | 22 | Not stated | 0 | 2 | 0 | 8 |
| 70–79 | 8 | 22 | |||||
| ≥80 years | 2 | 7 | |||||
| Not stated | 3 | 2 | |||||
| Telephone Interviews | NA | 18 | None agreed | 10 | 10 | 11 | |
| (Target) | (15) | (15) | (10) | (10) | (10) | ||
| Focus Groups |
NA | Focus group with 6 participants | None agreed to take part | None agreed to take part or times not convenient | Focus group with 7 participants | ||
| (Target) | (8) | (8) | (8) | (8) | |||
COPD, chronic obstructive pulmonary disease; NA, not applicable.
Questionnaire responses
Of 249 questionnaires completed, 145 (58%) were paper-based (including all from patients with COPD and members of the public)—table 2 summarises responses to the 10 factual questions, table 3 to opinion-based questions and table 4 questions about training and equipment.
Table 2.
Per cent of correct responses to factual questions (the correct answer is in brackets)
| Question | General public (n=65) | Patients with COPD (n=62) | Managers (n=10) | Ambulance crew (n=68) | Nurses (n=22) | Doctors (n=22) | |
|---|---|---|---|---|---|---|---|
| 1 | Per cent oxygen in room air (21%) | 15 | 15 | 90 | 82 | 82 | 86 |
| 2 | Is oxygen needed for an acute asthma episode with normal saturation (no) | 22 | 31 | 20 | 56 | 55 | 45 |
| 3 | Is controlled oxygen therapy required in acute COPD (yes) | 40 | 40 | 100 | 88 | 86 | 82 |
| 4 | Effect of oxygen in ‘Oxygen Bars’ (no benefit or harm) | 29 | 23 | 100 | 79 | 73 | 82 |
| 5 | Correct use of oxygen for heart attack (give oxygen if the saturation is low) | 57 | 31 | 70 | 66 | 86 | 73 |
| Average score for five factual questions | 33% | 28% | 76% | 74% | 76% | 74% | |
| 6 | Target saturation for most patients with COPD (88–92%) | – | – | – | 69 | 55 | 73 |
| 7 | Target range for most patients (94–98%) | – | – | – | 73 | 82 | 73 |
| 8 | Patient with COPD with major trauma (target 94–98 until ABG available) | – | – | – | 32 | 45 | 36 |
| 9 | Oxygen for palliative care patient with SpO2 94% (no benefit in trials) | – | – | – | 78 | 68 | 73 |
| 10 | Which poisoning needs high dose oxygen, ignoring SpO2? (carbon monoxide) | – | – | – | 73 | 73 | 82 |
| Average score for five advanced questions | 70% | 70% | 70% | ||||
| Average per cent of incorrect answers | 64 | 67 | 22 | 22 | 12 | 17 | |
| Average per cent of blank answers | 3 | 5 | 2 | 8 | 16 | 13 |
COPD, chronic obstructive pulmonary disease.
Table 3.
Summary of responses to five opinion-based questions (all results are percentages)
| Question | General public (n=65) | Patients with COPD (n=62) | Managers (n=10) | Ambulance crew (n=68) | Nurses (n=22) | Doctors (n=22) | |
|---|---|---|---|---|---|---|---|
| 1 | If you had a heart attack and were told that there was disagreement among scientists as to whether oxygen might help you get better or may possibly make you worse what would be your view? | ||||||
| a | I would trust the ambulance crew to give the right dose of oxygen | 77 | 63 | 30 | 48 | 14 | 18 |
| b | I would want oxygen as a precaution | 3 | 15 | 20 | 15 | 5 | 18 |
| c | I would not want oxygen in case it might harm me | 3 | 2 | 0 | 3 | 9 | 0 |
| d | I would want to discuss various options | 12 | 16 | 20 | 28 | 32 | 50 |
| e | I have a different view | 0 | 0 | 20 | 1 | 9 | 0 |
| Blank | 5 | 5 | 10 | 4 | 32 | 14 | |
| 2 | If you had a heart attack, how would you feel about taking part in a trial of oxygen therapy? | ||||||
| a | I would be keen to take part | 37 | 29 | 10 | 28 | 9 | 27 |
| b | I would not want to take part | 18 | 13 | 20 | 10 | 9 | 9 |
| c | I would want a detailed explanation | 26 | 40 | 20 | 40 | 32 | 32 |
| d | Happy to take part and to discuss later | 8 | 6 | 30 | 7 | 14 | 9 |
| e | I have a different view | 3 | 5 | 10 | 7 | 5 | 9 |
| Blank | 8 | 6 | 10 | 7 | 32 | 14 | |
| 3 | Do you believe that oxygen is helpful for most medical emergencies? | 68 | 79 | 20 | 41 | 18 | 36 |
| 4 | Do you have any concerns that oxygen may be harmful in some medical emergencies? | 25 | 35 | 100 | 73 | 64 | 55 |
| 5a | Do you think that it is right to allow researchers to undertake a randomised trial of oxygen therapy in circumstances where a patient is acutely unwell and cannot realistically give informed consent at the time when treatment is needed? | 43 | 45 | 70 | 60 | 50 | 68 |
| 5b | Would it be reasonable to place patients in such a trial in an emergency and obtain consent later? | 55 | 56 | 40 | 57 | 50 | 73 |
COPD, chronic obstructive pulmonary disease.
Table 4.
Organisational issues; training and equipment
| Ambulance crews n=68 | Nurses n=22 | Doctors n=22 | |
|---|---|---|---|
| Have you had any specific training in oxygen use? (Number saying ‘Yes’) | 34/47 | 15/15 | 9/15 |
| Do you think you have had adequate training in oxygen use? | 26/43 | 9/15 | 11/17 |
| When treating patients with acute exacerbations of COPD, do you have access to the following equipment (usually or always) Answers given as per cent of those who replied | |||
| Simple face mask | 92 | 100 | 93 |
| Reservoir mask | 98 | 100 | 88 |
| Nasal cannulae | 63 | 42 | 75 |
| 24% Venturi mask | 45 | 28 | 60 |
| 28% Venturi mask | 59 | 53 | 49 |
| Oxygen driven nebuliser | 94 | 100 | 88 |
| Air-driven nebuliser | 33 | 0 | 37 |
| Finger oximeter | 100 | 93 | 100 |
COPD, chronic obstructive pulmonary disease.
For the five factual questions answered by all participants, HCPs scored more highly than patients with COPD and the general public (table 1 and figure 1). Mean correct scores for these five questions were highest for HCPs (74–76%) and lowest for patients with COPD (33%). There was little difference between the scores of ambulance crew, nurses and doctors across all sections of the survey (table 2).
Figure 1.
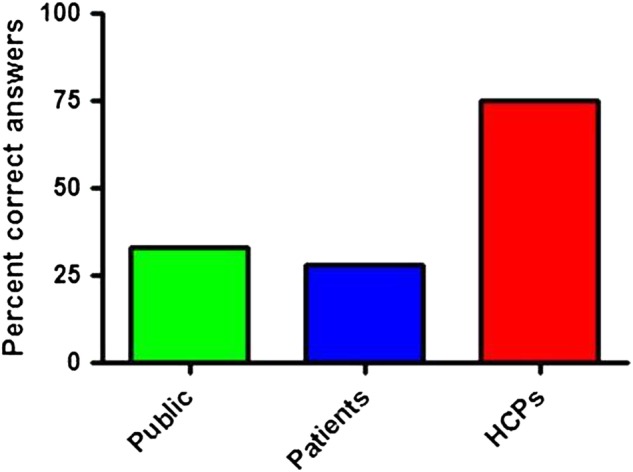
Per cent of correct answers by the general public, patients and health care professionals (HPCs) to five factual questions about oxygen therapy.
An additional knowledge-based question asked clinical HCPs to identify the correct oxygen target saturation range for 10 medical conditions of which 4 would require 88–92% target range. The overall response rate to this question was low (37%), making results difficult to interpret. Only 55% of completed responses were correct and it is likely that many of the blank answers would have been incorrect so we did not tabulate these results.
Responses of patients and the public differed markedly from those of HCPs for opinion-based questions (table 3 and figure 2). Patients and the public were more than twice as likely as HCPs to believe that oxygen was helpful for most medical emergencies and half as likely to be aware that oxygen can be harmful in some medical emergencies. They were less likely than HCPs (44% vs 60%) to agree that it would be right to enter acutely unwell patients who could not give informed consent into a trial of emergency treatment, but more likely to trust ambulances team to know the right oxygen dose for their condition (70% vs 35%).
Figure 2.
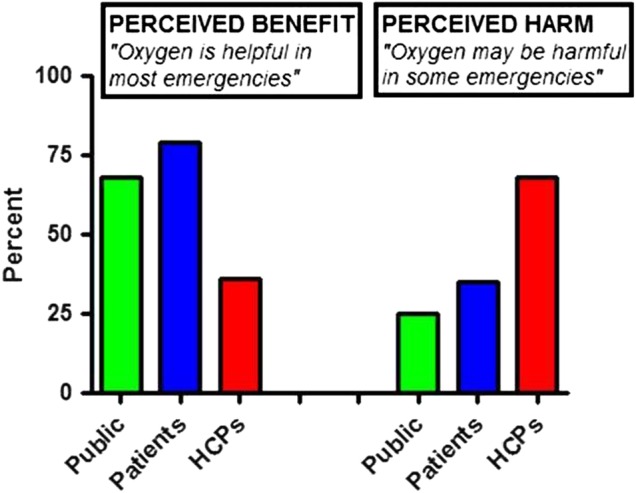
Contrasting views about benefits and possible harm from oxygen therapy. Per cent of general public, patients and health care professionals (HPCs) agreeing with each point of view.
Only 64% of HCPs responded to questions about training. However, the available data suggests that many front-line HCPs believe that they have not had adequate training in oxygen therapy and that equipment needed to deal effectively with hypercapnic patients (Venturi masks and air-driven nebuliser compressors) was not available to most respondents (table 4). Although some questions may have been misunderstood because most nurses at our hospital have access to air compressors and wall air sockets to drive nebulisers but all of those who responded said that they did not have such access,
Interview and focus group results
Interviews and focus groups assessed topics linked with the survey: (1) general views about oxygen use in emergency situations; (2) under/overuse of oxygen (3) adequacy of oxygen training; (4) availability of correct oxygen equipment; and (5) views regarding clinical trials of oxygen use in emergency situations.
General views about oxygen use in emergency situations:
Hospital staff (doctors and nurses) were confident that oxygen was usually used correctly in respiratory and high dependency environments, with staff in these areas being perceived as more aware of potential risks of overuse:
I think that it's used, certainly on my ward [respiratory], in the correct way. I don't think that that can be guaranteed out of a respiratory environment. [nurse 7]
Some doctors felt the ambulance crew/paramedics overused oxygen, although there was acknowledgement that the situation is improving:
If you include paramedics then I'd be inclined to say that it’'s overused, but if it’'s just within the hospital setting then I think it’'s probably just about right, from my experience’ [Doctor 8] and ‘I think, in the ambulance service, historically it's been overused. Recently there's been a big emphasis on more appropriate use of oxygen so I think the situation is improving. [Doctor 7]
Paramedics generally agreed that oxygen was traditionally overused, although guidelines were acknowledged as improving provision of evidence-based care:
The new oxygen guidelines have come out which are evidence based and they are making their way through pre-hospital care but there are still a lot of staff members that still will give 100 per cent O2 to any critical patients regardless of whether they need it or not. [Paramedic 7]
The time lag between guideline publication and implementation was identified as a barrier. There was recognition that the recent guidelines
Represented a bit of a culture-shock to a lot of people…we [paramedics] have been guilty, the organisation, and even personally, for giving too much oxygen to patients. [paramedic, focus group]
There was general agreement that that newly qualified paramedics followed the oxygen guidelines more stringently.
Many HCPs reflected on witnessing medial disagreements about emergency oxygen use (box 1).
Box 1. Medical disagreement about oxygen use.
The majority of Doctors and nurses felt that there are differing views regarding emergency oxygen use: “I think the disagreement is still…I remember the debate, 3 to 4 years ago, then and having been told on my clinical placement that I shouldn't be using high flow oxygen on anyone who is at risk of type two failure and then I was told, if there’'s any doubt just put them on high flow oxygen.” [Doctor 2]. Training often reflected the ongoing debate: “There was, I think it's still going on now at the hospital but we are taught during ALS (Advanced Life Support) training that whether they're COPD or not you still give them 15 litres but, yeah, we do still get people (both nurses and doctors) question and say, if they are COPD do we still increase it…” [Nurse 4].
The disagreement was also noted to be at the organisational level: “…. suggest there is some disagreement between the College of Anaesthetists and the British Thoracic Society in terms of what constitutes too much oxygen.” [Doctor 7]. This view was supported by a paramedic: “I think using the guidelines there actually seems to be some kind of disagreement and obviously they do reach consensus statement towards the end of it but as part of the narrative or discussion there does seem, disagree with their self quite a lot all the way through.” [Paramedic 8].
Specific incidents of mixed views were recalled: “I have heard some doctors on the A&E Department saying hypoxic drives are a load of rubbish and there's no such thing. But obviously if you take a patient in with COPD and you've got them on a quite a high concentration of oxygen you're frowned upon. So there is definitely a mixed message.” [Paramedic 2]; and “I know there's still arguments now as to whether we should be giving about 100 per cent oxygen through masks to certain, you know, certain patients and certain patient streams.” [Paramedic 1]. Some paramedics felt undermined by hospital staff although the perceptions was that this is improving: “…we were coming into hospital and being challenged on why this patient hadn't been given oxygen and having to explain our actions, that there was obviously no need for oxygen in a patient who was saturating at 100 per cent or 98 per cent.” “Not so much now, it's less but it's still there.” [Paramedic 3].
There was also concern that some patients with COPD refuse oxygen because it's been drilled into them that they should not have it and it's bad for them. [doctor 7] making it difficult to treat them. Patients themselves were mostly of the view that oxygen saved lives; and in some cases their own.
Knowledge and views about potential harm of under/over use of oxygen
The importance of knowing your patient was stated by some clinicians to be the key to providing appropriate treatment:
So, it's just understanding your patient group basically and knowing which ones will benefit from oxygen and which ones it's harmful to. [nurse 5]
Time restrictions were seen as a barrier to optimising oxygen assessment and administration by paramedics:
You've got to get as much history as you can but you're in quite a small timeframe…you're not having as much time as you maybe would require to do a really comprehensive history before you commence your treatment. [paramedic 1]
Patients were aware that too little oxygen could be harmful, but less sure about the effects of too much oxygen. Their views varied widely:
Premature babies…that [oxygen] did cause some brain damage. [patient 2]
Some patients were aware of potential harm from oxygen therapy in COPD:
People with COPD if you give them too much they'll be harmed…it's probably because their lungs not being able to take too much and it can't circulate round their body quick enough. [patient 3]
Adequacy of training in oxygen therapy
There were differing views among clinical staff regarding training in oxygen use. Some reported access to few training opportunities:
I don't actually remember having any training. [nurse 1]
It's [oxygen] just mentioned during basic life support training days. [nurse 4]
Some interviewees were quite specific in what training was required:
It sounds stupid, but even down to the flow rates, the delivery rates, what the difference is between a flow rate and a percentage delivery and things like that. [Doctor 3]
Concerns were raised about the quality of teaching about oxygen therapy:
I did my ALS [advanced life support] course a couple of weeks ago, and … the tutors whose knowledge must be a little old and backdated, were still saying,…you give 15 litres, which concerned me a bit I suppose!. [Paramedic 10]
The appointment of ‘Respiratory champions’ was suggested to make paramedics aware of oxygen guidelines and to assist them in adhering to guidelines.
One patient stated that staff were somewhat blasé about use of oxygen:
I don't know, if they're all trained up or not, but in other wards [non-specialist]…then last time I went to hospital it was just a matter of, it's oxygen it doesn't matter. [patient 4]
Access to oxygen equipment in healthcare settings
Most of the clinicians interviewed agreed that they had access to the correct equipment most of the time. However, concern was raised that specific equipment was only available in respiratory areas:
We were allowed to have these points [oxygen and air outlets] because we're a respiratory ward. Across the rest of the Trust I think there are still restrictions. [Nurse 7]
Lack of availability of compressed air to deliver nebulisers was also noted as an issue:
If you've got more than two people at once with an exacerbation of COPD they're going to have to take it in turns. So, that's a bit of issue. [Doctor 4]
Responses from paramedics were variable, with differences in availability of equipment between sites causing some dissatisfaction. Key concerns included:
What they're lacking is methods of actually delivering lower rates of oxygen. [Paramedic 1]
Often there was no choice, but to use inappropriate equipment:
Yet we've got to give them our nebuliser that's delivered by oxygen which, in the long run, could be doing them more harm than good really, but it's the only equipment that we've got; frustrating. [Paramedic 7]
There was an expectation from patients that the correct equipment should always be available:
You would expect with the training that they'd have everything ready and everything should be there. Maybe I'm expecting too much, I don't know’ [patient 1].
Views regarding clinical trials of oxygen use in emergency situations
Interviewees acknowledged the need for a strong evidence-base for the use of oxygen in emergency situations, but some could not envisage how a clinical trial could be conducted:
I think it'll be very difficult to convince an ethics committee to say that in a life threatening situation we're going to change things for the purposes of research. [Doctor 1]
Despite the apparent challenges, clinicians were inclined to favour more research in emergency situations
Because we need to know what we're doing right or wrong. [Nurse 2]
There was a view that because oxygen is a drug it should be subjected to appropriate research:
It’'s important that we do clinical trials, because oxygen is like any other drug, and we'd want to only use it if there’'s evidence for it. [Doctor 9]
There was overall support from patients for clinical trials to occur ‘whether it’s oxygen or anything else so that they [clinical staff] know exactly how far to go with oxygen’ [patient 3].
There were mixed views on waiving consent and whether or not it was ethical. Both nursing and medical interviewees tended not to favour waiving of consent:
I don't think, I don't think I could deliver that care. [nurse 10]
Some paramedics also raised concerns about waiving consent:
That's a difficult one really. I think consent is vital. I think if you waive consent then later on it might raise issues, so no I think consent's essential really. [Paramedic 2]
A few interviewees held strong views in favour of research
Yeah. I think I'd be okay with that actually, again to just get some evidence documented down that it works or doesn't work. [Nurse 2]
One doctor justified waiving consent with the utilitarian argument:
There are situations when you need to develop a wider evidence base, and from an ethical perspective, I'd take the totalitarian[sic] approach, the good of the most people outweighs the thoughts and opinions of the few. [Doctor 7]
It was suggested by some clinicians that next-of-kin could provide consent:
If there’'s a next of kin that could consent, that would seem to be an acceptable substitute in my eyes. [Doctor 2]
Among those paramedics who disagreed with randomised trials of oxygen or who had concernsabout consent issues, there were concerns over what the patient's family would feel and some feared potential subsequent reprecussions
It's not the patient too much but it's also the patient's family and they want to feel as though their relative is receiving the best possible treatment. [paramedic 5]
Most patients indicated that it would be unacceptable to waive consent as they would
Have to be fully aware of what's going on and what everything's for. [patient 1]
Asking next-of-kin to provide consent was more acceptable.
Participants’ views on whether they would/would not be willing to consent for themselves/their relatives to take part in a clinical trial of emergency oxygen are presented in box 2.
Box 2. Views on giving consent for a relative to participate in a randomised trial.
“…I think I'd be inclined to say, go along with it, because I believe that they're giving the best benefit for the most patients, and it's right that we move along science…” [Doctor 7]. Of those who disagreed, one felt they would prefer therapy that has been tried and tested and the other that it should not be a relative who made the decision: “No, I wouldn't actually, it was my mother I'd want therapy that's been used for everyone else and I would want it to be a therapy that is tried and tested.” [Doctor 1]. Medical history played a role in determining if some people would consent to take part in a trial: “Me personally now at this stage, yeah, I probably would give it a whirl but if I've suffered with 20 years of airway disease and then you're going to play with me for a little bit then I probably wouldn't be as willing.” [Nurse 10] and similarly, “I suppose it would depend what I was acutely unwell with. If it were a trauma or something like that, then I think I'd be a lot more accepting, but if I had any sort of respiratory problem……..I don't think there'd be any way that I could be convinced to not have oxygen as it was required for my oxygen stats.” [Doctor 4].
All of the paramedics interviewed stated that they would agree to take part in a randomised trial, some with the proviso that it was ethically approved and wasn't going to do any harm: “I think so because if it's gone through a…as long as it's gone through an ethics committee it's not going to do me any harm; it's not going to make me any worse but…and, so…and there's potential to make me better.” [Paramedic 1]. In some cases the decisions was based on their clinical background and were unsure whether the general public would be able to make the decision: “…most members of the public faced with an emergency situation would find it difficult to give that consent but, personally, I would…” [Paramedic 9].
There was a concern from some patients about changing practice and asking for consent during emergency situations—one patient stated that “they could have given me a dose of arsenic if they'd wanted to, because I'd have believed it would have made me better. It depends how ill you are” [patient 2]. Assurance that close monitoring would occur was central to patients consenting to take part in a clinical trial involving oxygen: “I would have no objection myself provided that the levels of oxygen in the blood were monitored closely on the nurse's normal check-ups”. [patient 6].
Discussion
Although oxygen supplementation is one of the most commonly used interventions in medical emergencies, there are few randomised trials of emergency oxygen use. Consequently, most use of oxygen in medical emergencies prior to the publication of the BTS Emergency Oxygen Guideline in 2008 was based on custom and practice and treatment still largely remains opinion, rather than evidence-based.13 Many clinicians and members of the public do not realise that medical oxygen is a drug. This study has confirmed that many are not aware that oxygen can cause complications and side effects and many still believe that it should be given in situations such as acute asthma despite normal saturation level, a situation where oxygen is not indicated and may contribute slightly to hypercapnia and acidosis.13
The study's main strength was inclusion of 249 individuals from very different backgrounds; this is the first study comparing attitudes and beliefs about oxygen therapy of HCPs, patients and members of the public using the same methodology. The study had a number of limitations. These were convenience samples, however, we had no reason to suspect systematic bias among participants. Recruitment of service managers/commissioners for focus groups proved impossible and we were unable to schedule focus groups for nurses or doctors, primarily due to difficulties with several of these being simultaneously out of the clinical area; the one-to-one interviews conducted with HCPs nonetheless yielded valuable information. The views of medical and nursing staff represent those from only one large teaching hospital and one ambulance service; there has been a drive to optimise oxygen therapy in the hospital, hence, if anything, these participants may have been better informed than is typical. Views of patients and members of the public are likely to be more generalisable.
We observed differences in knowledge about oxygen therapy between lay people and HCPs, as might be expected, but there was little difference between doctors, nurses and ambulance crews. Patients and members of the public completed paper questionnaires but most HCPS completed the survey online so we cannot exclude the possibility that some HCPs checked the answers to some of the factual questions on their computers. Hospital managers had scores similar to HCPs and much higher than patients with COPD and the general public, possibly due above average educational levels and exposure to healthcare systems and some of the managers may have had nursing backgrounds. The survey also identified significant gaps in the knowledge of some HCPs and the professionals themselves identified gaps in training (oxygen delivery is not part of essential mandatory training at the study site, or in most UK hospitals).
Patients with COPD did not score higher than the general public; while this may seem surprising, it should be set in context of other studies which have shown poor condition-related knowledge in these patients.25–27 This further underscores the need for improved condition-related education in people with COPD. Survey and interview responses from patients and members of the public indicated that they had stronger beliefs than HCPs that ‘oxygen is a good thing’ and fewer concerns about possible harm; this suggests a need to better inform both groups about the potential risks associated with oxygen use.
Our participants described a complex mix of attitudes to oxygen research in acute medical emergencies. People at risk of hypercapnia due to excessive oxygen therapy can be difficult to identify.2 13 The importance of thorough patient assessment was raised by many interviewees. This can be challenging, especially for ambulance staff. Time constraints limit the ability to fully assess patients prior to arrival at hospital, resulting in many patients being administered 100% oxygen despite being at risk of hypercapnic respiratory failure. Evidence suggests that once people at risk have been identified, they should be warned of the danger and issued with oxygen alert cards.13 This strategy may reduce inappropriate oxygen administration in emergency settings. On the other hand, caution is needed when educating patients with COPD on the risks of oxygen—some ambulance staff commented that they had encountered patients who refused oxygen treatment despite having SpO2 below 88% because the possible dangers had been ‘drilled into them’.
HCPs acknowledged the challenges of administering emergency oxygen according to BTS guidelines. Ambulance staff mentioned the need for cultural change in order for the service to embrace available guidance fully; the difficulties of achieving this are widely acknowledged.28
One problem with implementing emergency oxygen guidelines is that their underpinning evidence base is largely dependent on observational studies and expert opinion because of a scarcity of randomised trials. The scarcity of such trials partly reflects the general difficulty of conducting research in emergency situations, due to ethical challenges, not least in obtaining informed consent and because treatments must be administered immediately.
Our participants’ acknowledged the challenges of conducting research in emergency situations, in particular research regarding oxygen delivery, not least owing to its prior ubiquitous use in emergency situations. Burls et al16 undertook an online study of 524 UK clinical staff from ambulance teams, cardiology departments and emergency departments in 2007. They reported that there was a widespread belief among HCPs regarding benefits of oxygen in myocardial infarction and they suggested that this could make it difficult to persuade funders of the importance of this issue and convince HCPs to enrol patients into a trial where oxygen dosage would be randomised.16 Interestingly, Austin et al8 colleagues overcame this by using a cluster design, whereby half of the participating ambulance teams gave high-concentration oxygen to all patients with COPD (their usual practice at that time) and the other half administered controlled oxygen therapy (which was found to be associated with a 50% reduction in mortality). They thus argued that consent from individual patients was not required, because paramedics who gave high-concentration oxygen were just continuing their usual practice, whereas those who were trained to use controlled oxygen were following what is regarded as best practice. The issue of oxygen research involving patients with heart attacks is even more controversial. We chose this topic partly because it is a scenario that most people can relate to and partly because the work of Burls et al16 had indicated that healthcare staff had strong views on this matter. Despite these problems, the Australian AVOID trial team managed to randomise 441 patients with ST elevation myocardial infarction with oxygen saturation ≥94% to receive either oxygen or air during ambulance journeys and emergency department care and during primary intervention, confirming that it is possible (In Victoria, Australia, the medical treatment act allows for enrolment in clinical trials in the prehospital setting with subsequent formal consent being obtained by the patient or ‘person responsible’ at a later stage).29 The results of this study suggest that the ‘tried and trusted’ treatment of heart attacks with oxygen may actually increase infarct size, thus emphasising the need for further randomised trials of oxygen therapy in common medical emergencies.30
To our knowledge, ours is the first study to report the views of both HCPs and patients regarding conduct of research in this area. Previous systematic searches by Kelly and Maden31 32 were essentially negative with regards to HCPs ‘None of the studies addressed the research question directly’ and with regards to patients ‘Few studies directly addressing the research question were evident, therefore studies were selected on the basis that some aspect of, or reference to the study's findings included patients’ perceptions of oxygen therapy’. Like us, they found that oxygen therapy was often misunderstood by patients and by healthcare providers and many had false beliefs about the benefits of oxygen therapy. Kelly and Maden discussed the interesting hypothesis that oxygen may be ‘a therapy for health-care professionals’ because they feel that they are doing something for breathless patients. They commented that patients had an underlying faith in HCPs who themselves had false beliefs about the benefits of oxygen therapy.
On the whole, all groups studied were supportive of further research, but informed consent was a contentious issue and the subject of waived consent roused strong opinions; many HCPs stated that they would not agree to their own loved ones taking part in a randomised controlled trial of emergency oxygen therapy. This raises concerns for the development of adequately controlled and high quality studies being conducted in real world scenarios.
In summary, we have explored the views of patients, members of the public and HCPs about oxygen therapy and related research and we have identified a tendency among patients and the public to regard oxygen therapy as an unequivocal good thing, whereas HCPs tend to have a more realistic view that oxygen may cause harm as well as benefit. These attitudes and beliefs (compounded by deficiencies in training and in availability of equipment) may pose problems for optimal oxygen use for some time to come. All of the groups studied had complex views about the practicality and ethics of trials of oxygen in medical emergencies.
Acknowledgments
The authors would like to thank Professor Ashley Woodcock for his support and encouragement of this project.
Footnotes
Funding: This project was funded by a grant from Manchester Academic Health Sciences Centre.
Competing interests: None declared.
Ethics approval: NRES committee South West; Reference 11/SW/0354.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Hale KE, Gavin C, O'Driscoll BR. Audit of oxygen use in emergency ambulances and in a hospital emergency department. Emerg Med J 2008;25:773–6. doi:10.1136/emj.2008.059287 [DOI] [PubMed] [Google Scholar]
- 2.National Institute for health and Care Excellence CG101 Chronic obstructive pulmonary disease (update) full guideline. October 2010. http://guidance.nice.org.uk/CG101/Guidance/pdf/English Viewed January 2014.
- 3.Campbell EJ. Respiratory failure: the relation between oxygen concentrations of inspired air and arterial blood. Lancet 1960;2:10–11. doi:10.1016/S0140-6736(60)92659-3 [DOI] [PubMed] [Google Scholar]
- 4.Plant PK, Owen JL, Elliott MW. One year period prevalence study of respiratory acidosis in acute exacerbations of COPD: implications for the provision of non-invasive ventilation and oxygen administration. Thorax 2000;55:550–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Murphy R, Driscoll P, O'Driscoll R. Emergency oxygen therapy for the COPD patient. Emerg Med J 2001;18:333–9. doi:10.1136/emj.18.5.333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Price LC, Lowe D, Hosker HS et al. British Thoracic Society and the Royal College of Physicians Clinical Effectiveness Evaluation Unit (CEEu). UK national COPD audit 2003: impact of hospital resources and organisation of care on patient outcome following admission for acute COPD exacerbation. Thorax 2006;61:837–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roberts CM, Stone RA, Buckingham RJ et al. National Chronic Obstructive Pulmonary Disease Resources and Outcomes Project implementation group. Acidosis, non-invasive ventilation and mortality in hospitalised COPD exacerbations. Thorax 2011;66:43–8. doi:10.1136/thx.2010.153114 [DOI] [PubMed] [Google Scholar]
- 8.Austin MA, Wills KE, Blizzard L et al. Effect of high flow oxygen on mortality in chronic obstructive pulmonary disease patients in pre-hospital setting: randomised controlled trial. BMJ 2010;341:c5462 doi:10.1136/bmj.c5462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cabello JB, Burls A, Emparanza JI et al. Oxygen therapy for acute myocardial infarction. Cochrane Database Syst Rev 2010;6:CD007160 doi:10.1002/14651858.CD007160.pub2 [DOI] [PubMed] [Google Scholar]
- 10.Ronning OM, Guldvog B. Should stroke victims routinely receive supplemental oxygen? A quasi-randomized controlled trial. Stroke 1999;30:2033–7. [DOI] [PubMed] [Google Scholar]
- 11.de Jonge E, Peelen L, Keijzers PJ et al. Association between administered oxygen, arterial partial oxygen pressure and mortality in mechanically ventilated intensive care unit patients. Crit Care 2008;12:R156 doi:10.1186/cc7150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kilgannon JH, Jones AE, Shapiro NI et al. Emergency Medicine Shock Research Network (EMShockNet) Investigators. Association between arterial hyperoxia following resuscitation from cardiac arrest and in-hospital mortality. JAMA 2010;303:2165–71. doi:10.1001/jama.2010.707 [DOI] [PubMed] [Google Scholar]
- 13.O'Driscoll BR, Howard LS, Davison AG, British Thoracic Society . BTS guideline for emergency oxygen use in adult patients. Thorax 2008;63(Suppl 6):vi1–68. doi:10.1136/thx.2008.102947 [DOI] [PubMed] [Google Scholar]
- 14.Bellomo R, Bailey M, Eastwood GM et al. , Study of Oxygen in Critical Care (SOCC) Group. Arterial hyperoxia and in-hospital mortality after resuscitation from cardiac arrest. Crit Care 2011;15:R90 doi:10.1186/cc10090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eastwood G, Bellomo R, Bailey M et al. Arterial oxygen tension and mortality in mechanically ventilated patients. Intensive Care Med 2012;38:91–8. doi:10.1007/s00134-011-2419-6 [DOI] [PubMed] [Google Scholar]
- 16.Burls A, Emparanza JI, Quinn T et al. Oxygen use in acute myocardial infarction: an online survey of health professionals’ practice and beliefs. Emerg Med J 2010;27:283–6. doi:10.1136/emj.2009.077370 [DOI] [PubMed] [Google Scholar]
- 17.JRCALC Clinical Practice Guidelines. Oxygen Update April 2009. http://www2.warwick.ac.uk/fac/med/research/hsri/emergencycare/prehospitalcare/jrcalcstakeholderwebsite/clinicalpracticeupdates/oxygen_guideline_combined_final_published_version_22apr09sb.pdf (accessed Jan 2014).
- 18.O'Driscoll BR, Beasley R. Avoidance of high concentration oxygen in chronic obstructive pulmonary disease. BMJ 2010;341:c5549 doi:10.1136/bmj.c5549 [DOI] [PubMed] [Google Scholar]
- 19.Creswell JW, Plano-Clark VL. Designing and conducting mixed methods research. 2nd edn London: Sage Publications Inc, 2011. [Google Scholar]
- 20.Ivankova NV, Creswell JW, Stick SL. Using mixed-methods sequential explanatory design: from theory to practice. Field Methods 2006;18:3–20. [Google Scholar]
- 21.Burns N, Grove SK. Understanding nursing research: building an evidence-based practice. 5th edn Maryland Heights, MO: Elsevier, 2011. [Google Scholar]
- 22.Greenbaum T. Moderating focus groups. Thousand Oaks, CA: Sage Publications, Inc, 2000. [Google Scholar]
- 23.Ritchie J, Lewis J. Qualitative research practice: a guide for social science students and researchers. London: Sage, 2003. [Google Scholar]
- 24.Ritchie J, Spencer E. Qualitative data analysis for applied policy research. In, Bryman A, Burgess RG, eds. Analyzing qualitative data. London: Routledge, 1994:173–94. [Google Scholar]
- 25.Jones RCM, Hyland ME, Hanney KE. Preliminary data from the Lung information Needs Questionnaire (LINQ). Prim Care Respir J 2005;14:270–1. doi:10.1016/j.pcrj.2005.06.008 [Google Scholar]
- 26.Hernandez P, Meyer B, Bourbeau J et al. Living with chronic obstructive pulmonary disease: a survey of patients’ knowledge and attitudes. Respir Med 2009;103:1004–12. doi:10.1016/j.rmed.2009.01.018 [DOI] [PubMed] [Google Scholar]
- 27.Ray SM, Helmer RS, Barger Stevens A et al. Clinical Utility of the Chronic Obstructive Pulmonary Disease Knowledge Questionnaire. Fam Med 2013;45:197–200. [PubMed] [Google Scholar]
- 28.Dixon-Woods M, Baker R, Charles K et al. Culture and behaviour in the English National Health Service: overview of lessons from a large multimethod study. BMJ Qual Saf 2014;23:106–15. doi:10.1136/bmjqs-2013-001947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stub D, Smith K, Bernard S et al. A randomized controlled trial of oxygen therapy in acute myocardial infarction Air Verses Oxygen In myocarDial infarction study (AVOID Study). Am Heart J 2012;163:339–345.e1. doi:10.1016/j.ahj.2011.11.011 [DOI] [PubMed] [Google Scholar]
- 30.Stub D, Smith K, Bernard S et al. AVOID Investigators. Air Versus Oxygen in ST-Segment-Elevation Myocardial Infarction. Circulation 2015;131:2143–50. doi:10.1161/CIRCULATIONAHA.114.014494 [DOI] [PubMed] [Google Scholar]
- 31.Kelly CA, Maden M. How do health-care professionals perceive oxygen therapy? A critical interpretive synthesis of the literature. Chron Respir Dis 2015;12:11–23. doi:10.1177/1479972314562408 [DOI] [PubMed] [Google Scholar]
- 32.Kelly CA, Maden M. How do respiratory patients perceive oxygen therapy? A critical interpretative synthesis of the literature. Chron Respir Dis 2014;11:209–28. doi:10.1177/1479972314551561 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjresp-2015-000102supp.pdf (1.7MB, pdf)


