Abstract
Many recent studies point to increasing inequality in mortality in the United States over the past 20 years. These studies often use mortality rates in middle and old age. We used poverty level rankings of groups of U.S. counties as a basis for analyzing inequality in mortality for all age groups in 1990, 2000, and 2010. Consistent with previous studies, we found increasing inequality in mortality at older ages. For children and young adults below age 20, however, we found strong mortality improvements that were most pronounced in poorer counties, implying a strong decrease in mortality inequality. These younger cohorts will form the future adult U.S. population, so this research suggests that inequality in old-age mortality is likely to decline.
Poorer people tend to have shorter lives and are more likely to die than richer people at all ages. Understanding the evolution of these inequalities in mortality is a central concern of economists, policy-makers, and the public. Not surprisingly, a great deal of highly publicized research has investigated changes in inequality in life expectancy and mortality in the United States over the past 20 years. A preponderance of the existing evidence points to alarming increases in inequality in mortality over this time period (1–16). Some studies investigating mortality trends across educational groups and geographic areas argue not only that inequality in life expectancy is widening, but that overall life expectancy is actually falling among the most disadvantaged groups (11–13).
However, much of the recent literature focuses on adults, and in particular on life expectancy at age 40 or 50, exploiting rich data sets that link individuals’ career earnings to deaths at older ages (1–8). By construction, these analyses omit children, teens, and young adults. A second strand of research analyzes demographic subgroups defined by education, location, and/or race (9–16). These studies typically focus on overall life expectancy at birth.
Life expectancy at birth is a summary measure that collapses all of the age-specific mortality rates observed in a given year (and in a certain demographic subgroup) into a single number. It provides information about how long a cohort of newborns can expect to live, under the assumption that the age-specific mortality rates observed in that given year remain constant into the future. This assumption is unlikely to hold in the United States, given that mortality rates at all ages have been continuously changing (mostly improving) over the past century (17).
Changes in infant and childhood mortality have been shown to be important predictors of a cohort’s health and mortality at later ages, and such data may therefore be more informative about the development of future death rates for the current young. Moreover, mortality at young ages is considered a sensitive indicator of social conditions because it responds relatively quickly to changes affecting the entire population, whereas old-age mortality is partly determined by conditions in the past. The infant mortality rate has been shown to be an important indicator of health for whole populations and one that is highly correlated with more complex measures such as disability-adjusted life expectancy (18).
Therefore, to study how inequality in mortality changes over time, it is important to understand age-specific mortality trends and in particular those at younger ages. Life expectancy at birth masks potential differences in age-specific trends, and the measure is also dominated by changes in old-age mortality because that is when most deaths occur. A recent study by Case and Deaton (19) highlights the relevance of examining age-specific mortality rates: They document increases in middle-age mortality for non-Hispanic whites, a striking development that would not be detectable in overall life expectancy at birth.
We followed an empirical approach, based on placing counties into groups, that allows us to analyze trends in age-specific mortality while taking into account population shifts across groups. We ranked all counties in 1990, 2000, and 2010 by their poverty level and then divided them into 20 groups, each representing roughly 5% of the overall U.S. population (fig. S1 and table S1). This enables us to compare, for example, the 5% of the population living in the poorest counties in 1990 with the 5% of the population living in the richest counties in 1990, and analyze how the mortality differences between these groups change over time. We refer to the county groups with the highest fractions of their populations in poverty as the poorest counties, and those with the lowest fractions of their populations in poverty as the richest counties.
Our approach reassigns county groups in 1990, 2000, and 2010 to adjust for changes in county ranking and population size. That is, we compare the poorest counties representing 5% of the population in 1990 with the poorest counties representing 5% of the population in 2010, even if they are not exactly the same counties. The advantages of this procedure and a comparison with other approaches are discussed below. Our county grouping approach is similar to that of Singh and Siahpush (9), who investigated life expectancy trends ranking U.S. counties by a deprivation index (comprising a set of county characteristics) up to 2001. Our approach differs from theirs in that they did not analyze age-specific mortality, analyzed data only up to 2001, and did not reorder county groups over time.
Mortality rates were constructed at the levels of county group, gender, and age by dividing death counts from the U.S. Vital Statistics by population counts from the decennial Census. We focused on 3-year mortality rates for Census years 1990, 2000, and 2010, based on a total of 21,175,011 deaths. Life expectancy was calculated by constructing a life table based on 19 age groups (see the supplement for additional details regarding the construction of mortality rates and life expectancy). Socioeconomic county characteristics, including poverty rate, median and per capita income, and percentage of high school dropouts, were taken from the Census in 1990 and 2000. For 2010 we used the 2008–2012 American Community Survey (ACS), which replaced the long form of the Census for 2010. Table S1 reports socioeconomic characteristics for the 20 county groups. The county group with the lowest fraction living in poverty had an average poverty rate of 3.75% and a median income (averaged across counties) of $62,445 in 1990. The comparable 2010 figures are 5.58% in poverty and a $62,752 median income. The county group with the highest fraction living in poverty had a 30.47% poverty rate and a median income of $23,595 in 1990. Comparable 2010 figures were 28.30% in poverty and a median income of $25,404.
We start with the analysis of overall life expectancy at birth, so as to make a better comparison with the strand of previous literature that has focused on this measure. Figure 1A plots male and female life expectancies at birth for the 20 county groups in 1990, 2000, and 2010 (see table S2 for numerical values and standard deviations). Standard deviations are within 0.1% of the estimates, and 95% confidence intervals (CIs) would be fully covered by the estimate markers if plotted in Fig. 1A. In addition to the plotted life expectancy values, we have drawn a linear regression line through the 20 dots representing each year (the line for 2000 omits symbols to reduce clutter). A steeper slope of the regression line indicates greater inequality in life expectancy. If there was no difference in life expectancy between richer and poorer county groups, then the line would be entirely flat.
Fig. 1. Life expectancy at birth by poverty percentile and gender.
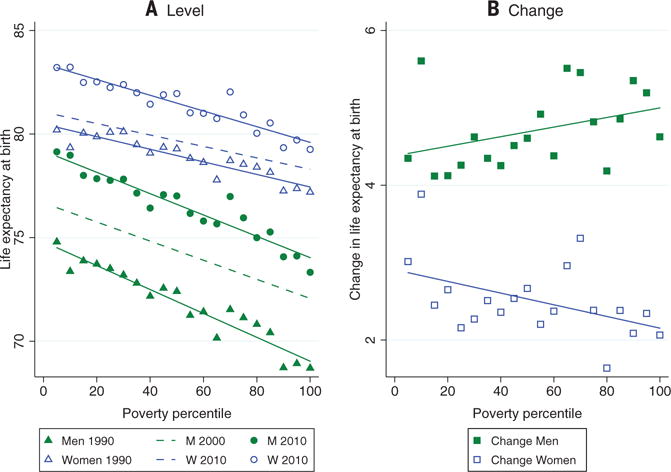
(A) Average male and female life expectancy at birth by poverty percentile. Each bin represents a group of counties with about 5% of the overall population. The solid lines provide the fitted regression lines. Higher percentiles refer to higher poverty levels. A steeper slope implies greater inequality in life expectancy at birth. Magnitudes are reported in table S2. (B) Changes in average male and female life expectancy at birth by poverty percentile. The fitted regression line has a slope of 0.0062 (P = 0.103) for men and a slope of −0.0075 (P = 0.043) for women.
Figure 1A shows that for men, there is a strong gradient in 1990, with those living in the richest counties enjoying 6.10 additional years of life expectancy relative to those living in the poorest counties (74.79 versus 68.70). For women, who have greater life expectancy overall, this gap is smaller at 3.01 years (80.20 versus 77.19). Between 1990 and 2010, life expectancy at birth increased across the entire poverty spectrum, both for men and for women. For men, the fitted lines in 1990 and 2010 are almost parallel, suggesting that life expectancy increased by similar amounts in rich and poor counties. In fact, residents of the poorest counties gained slightly more with 4.63 additional years, whereas those in the richest county group gained 4.35 years. For women, improvements were stronger for those in the richest county group (3.01 versus 2.06 years), and most of these improvements occurred between 2000 and 2010.
Figure 1B plots the changes in life expectancy between 1990 and 2010. For women, the fitted regression line is downward-sloping (P = 0.043), indicating increasing inequality in life expectancy over this period. For men, the slope of the regression line is positive but not significantly different from zero (P = 0.103), consistent with Fig. 1A’s suggestion that decreases in mortality were equally distributed across men in rich and poor counties.
Turning to our key innovation—the analysis of age-specific mortality for all ages—Figs. 2 and 3 show that the evolution of overall life expectancy at birth masks considerable heterogeneity in trends in mortality rates at different ages. Similar to Fig. 1, each symbol in the figure represents the age-specific 3-year mortality rate in a bin representing 5% of the U.S. population, and the bins are ordered by county poverty rates. Mortality rates are plotted for 1990 and 2010 together with a linear regression line; only the line is shown for 2000. Regression lines are upward-sloping because mortality is higher in poorer counties, but, as in Fig. 1, a flattening of the line over time indicates a decrease in inequality. Tables S3 and S4 report standard errors for the mortality rates and tests for a change in the slope of the fitted regression lines.
Fig. 2. Male 3-year mortality rates by poverty percentile across age groups.
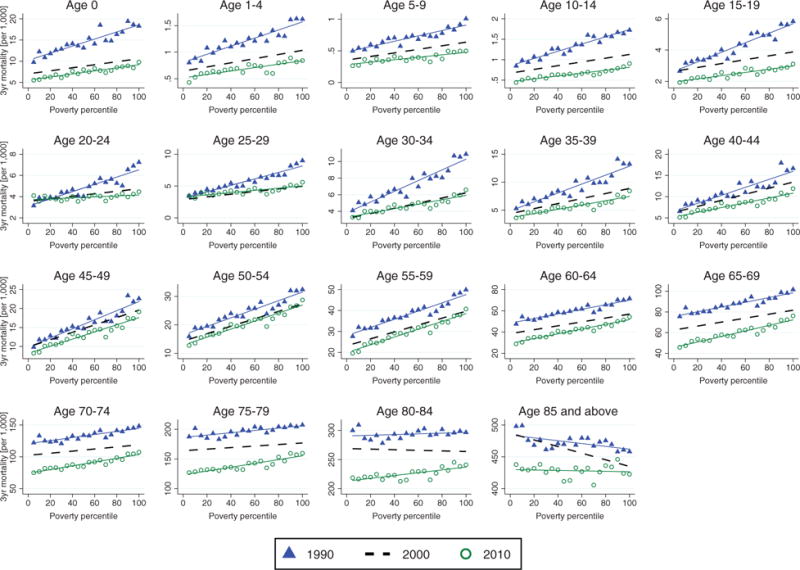
Average 3-year mortality rates are plotted across poverty rate percentiles. Each bin represents a group of counties with about 5% of the overall population in the respective year. Straight lines provide linear fits. Table S3 reports key magnitudes and standard errors.
Fig. 3. Female 3-year mortality rates by poverty percentile across age groups.
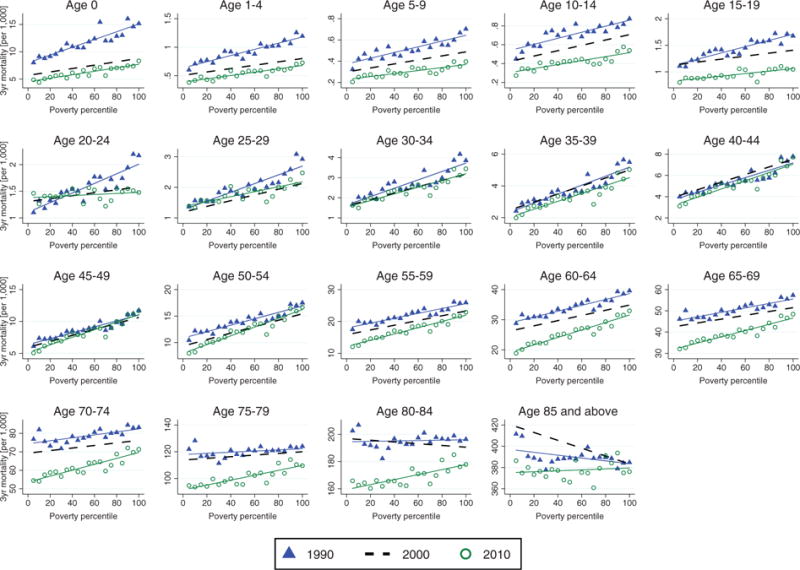
Data are displayed as in Fig. 2. Table S4 reports key magnitudes and standard errors.
The first panel in Fig. 2 shows the evolution of 3-year mortality rates for male newborns, which decreased by 4.2 per 1000 in the group of richest counties between 1990 and 2010, from 9.77 (95% CI, 9.10 to 10.44) to 5.53 (95% CI, 5.06 to 6.00). However, infant mortality in the group of poorest counties decreased by 8.49 deaths per 1000, which is more than twice as much over the same time period, from 18.28 (95% CI, 17.38 to 19.17) to 9.79 (95% CI, 9.22 to 10.37). These strong reductions in mortality in the poorer county groups are reflected in a considerable flattening of the regression line in 2010 relative to 1990. The slope of the regression line through the group values decreases by more than 50%, and this change is highly significant (P < 0.001, table S3). This flattening indicates a marked reduction in inequality in infant mortality.
A similar decline in mortality inequality can be observed up to age 20, although improvements for young children were greatest between 1990 and 2000. For older children, there were also large declines between 2000 and 2010. Looking at older ages, inequality decreased (i.e., the slope of the fitted regression line decreased significantly; see table S3 for P values) among males up to age 50. Between ages 50 and 75 there was no significant change in inequality in mortality, but after age 75, mortality inequality increased significantly among males. It is also striking that for adult men between 20 and 34, there was virtually no improvement in mortality rates between 2000 and 2010.
Figure 3 shows that the patterns are somewhat different for females. As it did for males, female mortality decreased strongly for age groups up to age 19, and these improvements were significantly stronger in the poorest counties, implying that inequality in mortality decreased sharply (see table S4 for P values of the differences in the slopes). However, although inequality decreased significantly for males until age 50, this trend is observed for females only up to age 30. For ages 30 to 45, there is no significant change in mortality inequality, whereas for all age groups over 45, inequality in mortality increases.
Turning to the mortality rates themselves, it is noteworthy that there was practically no improvement in mortality among women aged 30 to 45 between 1990 and 2010. This is a striking development in light of the progress made in other age categories. A further remarkable fact is that mortality rates actually increased in some of the richest counties among females aged 20 to 29. After age 45, there are mortality declines, but they are larger in the richer county groups, driving the increase in mortality inequality noted above.
The results discussed so far are all based on ranking counties by poverty rates, which is arguably the most relevant measure if one is focusing on differences between the rich and poor. However, several additional measures of socioeconomic status are available at the county level. The age-specific trends in mortality are very similar when ranking counties by these alternative measures, including the share of high school dropouts, median income, and average life expectancy (figs. S2 to S4).
In contrast to many recent analyses of inequality in mortality that focus on life expectancy at middle age, we find overall improvements in life expectancy at birth both in counties with high poverty rates and counties with low poverty rates. However, we argue that life expectancy measures are not (despite their name) intended to be predictive of the number of future years of life that any particular cohort can expect to attain, and that it is more informative to examine age-specific mortality rates. Our analysis of these rates indicates that inequality in mortality between rich and poor counties has strongly declined among infants, children, and young adults up to age 30 of either gender, as well as among adult males up to age 50. Among older adults, mortality has continued to decline, although declines are generally greatest in the richest counties, indicating increasing inequality in mortality, which is in line with the literature that has focused on inequality trends at older ages (1–8).
Our focus on using county groups to examine inequality has advantages and disadvantages. Unlike subgroups defined by race and education or by individual counties, county groups are large enough to provide precise mortality estimates in age ranges with low mortality. Moreover, the county of residence is consistently reported both in the Vital Statistics and the Census data, which makes mortality rates by county group subject to less measurement error than using other demographic groups that can be constructed with these data sets. For example, education is often missing from death certificates, and education measures were switched from years of schooling to degrees for some states in the mortality files but not in the Census. Even race is not always consistently reported. For example, the Census introduced multiple race categories in 2000 while the Vital Statistics reports permit only single-race identification. These changes in the reporting of race and education introduce a fundamental bias because of their different impacts on the numerator and denominator of a given subgroup’s mortality rate. And because these biases change over time, they confound the estimation of trends in inequality.
Changes in the composition of the analyzed demographic subgroups present another serious source of bias (20–23). For example, Olshansky et al. (13) documented decreasing life expectancy among non-Hispanic white women without a high school degree between 1990 and 2008. But the share of the population of white non-Hispanic females in this education category fell by about two-thirds between 1990 and 2010, which suggests that the average female high school dropout today is much more disadvantaged relative to her peers than the average female high school dropout in 1990. Bound et al. (20) argued that there is in fact no decrease in life expectancy for the least educated once these compositional changes are accounted for. Similarly, single counties that experienced declining life expectancy (11, 12) tend to be poor places that have lost population over the past 20 years. If the healthiest people leave, then the ones who remain will be less healthy on average, biasing the estimated changes in mortality inequality. Our approach accounts for potential compositional changes by reordering county groups so that they represent constant shares of the population over time. In the context of county groups, however, such compositional changes do not seem to play a crucial role, as our results look very similar when we keep the county groups assigned in 1990 fixed and follow them up to 2010 (fig. S6).
One limitation of our approach is that it necessarily focuses on differences between groups of counties, whereas much of the increase in (for example) individual income inequality may be occurring within counties. However, by its nature, mortality must be calculated relative to some reference group. Using county groups as the reference allows one to cleanly answer questions about inequality between these groups in a way that may not be possible with respect to other reference groups, such as education.
What are potential causes for the different age-specific trends that we observe? Aizer and Currie (24) highlighted many possible reasons for large reductions in infant mortality among the poor, which have reduced inequality in mortality among infants. We are not aware of any research that has looked at the causes of reductions in mortality inequality among older children and young adult males. Some possibilities include expansions of public health insurance (25–29), other social safety net programs such as Head Start (30, 31), and reductions in pollution, which tend to have disproportionate effects on the poor (32).
Among older adults, it is likely that at least some of the increasing disparities in mortality reflect differential patterns of both taking up and quitting smoking over their life cycles. For example, better-educated people stopped smoking much more quickly after the U.S. Surgeon General’s 1964 report on the dangers of smoking (33, 34). Improvements in medical care for conditions such as heart disease also tend to benefit the rich before they reach the poor. The outbreak of the opioid epidemic is another factor that may be driving increased mortality inequality and actual increases in mortality rates in middle age (19). As Case and Deaton (19) showed, it may be possible to get some insight into these questions by studying the causes of death in the Vital Statistics mortality data, although changes in measurement, measurement error, and missing data about causes mean that these data have to be interpreted cautiously.
Our results point to decreasing inequality in mortality, particularly among the younger cohorts who will form the future adult and elderly population of the United States. It is possible that survivors who would otherwise have died will be in poor health as they age and thus reduce the average level of health in the population. However, another possibility is that the declines in mortality at younger ages reflect improvements in the entire underlying distribution of health (35). In at least one important example—the case of expansions of public health insurance for poor infants and young children in the late 1980s and early 1990s—the reduced early death rates in these cohorts are associated with better health (27–29) and higher earnings (25) as these cohorts reach young adulthood. Thus, there appears good reason to hope that today’s young will also be healthier when they reach old age, and that inequality in mortality will decrease among these elderly in the future.
Supplementary Material
Acknowledgments
We thank M. Barbieri, A. Case, A. Deaton, J. Goldstein, I. Kuziemko, R. Lee, and K. Wachter, as well as seminar participants at Berkeley, the Chicago Federal Reserve, Fundação Getúlio Vargas São Paulo, Bonn University, University of Munich, Princeton University, ETH Zurich, and the University of Zurich for comments. Supported by Princeton Center for Translational Research on Aging grant 2P30AG024928. Data and code are available at http://dx.doi.org/10.7910/DVN/C2VYNM.
Footnotes
SUPPLEMENTARY MATERIALS
www.sciencemag.org/content/352/6286/708/suppl/DC1
Materials and Methods
References (36–38)
REFERENCES AND NOTES
- 1.Bosworth BP, Burke K. Differential Mortality and Retirement Benefits in the Health and Retirement Study. Brookings Institution; 2014. [Google Scholar]
- 2.Bosworth B, Zhang K. Evidence of Increasing Differential Mortality: A Comparison of the HRS and SIPP. Center for Retirement Research at Boston College Working Paper 2015-13. 2015 [Google Scholar]
- 3.Chetty R, et al. JAMA. 2016 doi: 10.1001/jama.2016.4226. [DOI] [Google Scholar]
- 4.National Research Council, Committee on the Long-Run Macroeconomic Effects of the Aging U.S. Population. The Growing Gap in Life Expectancy by Income: Implications for Federal Programs and Policy Responses. 2015. [PubMed] [Google Scholar]
- 5.Pijoan-Mas J, Ríos-Rull JV. Demography. 2014;51:2075–2102. doi: 10.1007/s13524-014-0346-1. [DOI] [PubMed] [Google Scholar]
- 6.Waldron H. Soc Secur Bull. 2007;67:1–28. [PubMed] [Google Scholar]
- 7.Waldron H. Soc Secur Bull. 2013;73:1–37. [PubMed] [Google Scholar]
- 8.Wilmoth J, Boe C, Barbieri M. In: International Differences in Mortality at Older Ages: Dimensions and Sources. Crimmins EM, Preston SH, Cohen B, editors. National Academies Press; Washington, DC: 2011. pp. 337–372. [PubMed] [Google Scholar]
- 9.Singh GK, Siahpush M. Int J Epidemiol. 2006;35:969–979. doi: 10.1093/ije/dyl083. [DOI] [PubMed] [Google Scholar]
- 10.Ezzati M, Friedman AB, Kulkarni SC, Murray CJ. PLOS Med. 2008;5:e66. doi: 10.1371/journal.pmed.0050066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Murray CJ, et al. PLOS Med. 2006;3:e260. doi: 10.1371/journal.pmed.0030260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang H, Schumacher AE, Levitz CE, Mokdad AH, Murray CJ. Popul Health Metr. 2013;11:8. doi: 10.1186/1478-7954-11-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Olshansky JS, et al. Health Aff. 2011;31:1803–1813. doi: 10.1377/hlthaff.2011.0746. [DOI] [PubMed] [Google Scholar]
- 14.Meara ER, Richards S, Cutler DM. Health Aff. 2008;27:350–360. doi: 10.1377/hlthaff.27.2.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cutler DM, Lange F, Meara E, Richards-Shubik S, Ruhm CJ. J Health Econ. 2011;30:1174–1187. doi: 10.1016/j.jhealeco.2011.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Montez JK, Berkman LF. Am J Public Health. 2014;104:e82–e90. doi: 10.2105/AJPH.2013.301526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Human Mortality Database; www.mortality.org
- 18.Reidpath DD, Allotey P. J Epidemiol Community Health. 2003;57:344–346. doi: 10.1136/jech.57.5.344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Case A, Deaton A. Proc Natl Acad Sci USA. 2015;112:15078–15083. doi: 10.1073/pnas.1518393112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bound J, Geronimus A, Rodriguez J, Waidman T. The Implications of Differential Trends in Mortality for Social Security Policy. University of Michigan Retirement Research Center Working Paper 2014-314. 2014 [Google Scholar]
- 21.Dowd JB, Hamoudi A. Int J Epidemiol. 2014;43:983–988. doi: 10.1093/ije/dyu120. [DOI] [PubMed] [Google Scholar]
- 22.Goldring T, Lange F, Richards-Shubik S. Testing for Changes in the SES-Mortality Gradient When the Distribution of Education Changes Too. National Bureau of Economic Research Working Paper 20993. 2015 doi: 10.1016/j.jhealeco.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 23.Hendi AS. Int J Epidemiol. 2015;44:946–955. doi: 10.1093/ije/dyv062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Aizer A, Currie J. Science. 2014;344:856–861. doi: 10.1126/science.1251872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brown D, Kowalski A, Lurie I. Medicaid as an Investment in Children: What Is the Long-Term Impact on Tax Receipts? National Bureau of Economic Research Working Paper 20835. 2015 [Google Scholar]
- 26.Cahodes S, Kleiner S, Lovenhem MF, Grossman M. Effect of Child Health Insurance Access on Schooling. National Bureau of Economic Research Working Paper 20178. 2014 [Google Scholar]
- 27.Miller S, Wherry LR. The Long-Term Health Effects of Early Life Medicaid Coverage. Social Science Research Network Working Paper 2466691. 2015 [Google Scholar]
- 28.Wherry LR, Meyer B. Saving Teens: Using and Eligibility Discontinuity to Estimate the Effects of Medicaid Eligibility. National Bureau of Economic Research Working Paper 18309. 2013 [Google Scholar]
- 29.Wherry LR, Miller S, Kaestner R, Meyer BD. Childhood Medicaid Coverage and Later Life Health Care Utilization. National Bureau of Economic Research Working Paper 20929. 2015 doi: 10.1162/REST_a_00677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ludwig J, Miller DL. Q J Econ. 2007;122:159–208. [Google Scholar]
- 31.Hoynes H, Whitmore-Schanzanbach D, Almond D. Long Run Impacts of Childhood Access to the Safety Net. National Bureau of Economic Research Working Paper 18535. 2012 [Google Scholar]
- 32.Isen A, Rossin-Slater M, Walker R. Every Breath You Take Every Dollar You’ll Make: The Long-Term Consequences of the Clean Air Act of 1970. National Bureau of Economic Research Working Paper 19858. 2014 [Google Scholar]
- 33.Fenelon A, Preston SH. Demography. 2012;49:797–818. doi: 10.1007/s13524-012-0108-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.de Walque D. J Hum Resour. 2010;45:682–717. [Google Scholar]
- 35.Finch CE, Crimmins EM. Science. 2004;305:1736–1739. doi: 10.1126/science.1092556. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


