Abstract
Objective
Non-Latino blacks experience a higher proportion of chronic illness and associated disabilities than non-Latino whites. Posttraumatic stress disorder (PTSD) is associated with a greater risk of chronic illness, although few studies have investigated whether the interaction of PTSD with racial disparities may lead to a greater risk of chronic illness among blacks with PTSD than among whites with PTSD.
Methods
We evaluated data from the population-based National Survey of American Life and the National Comorbidity Survey Replication to investigate the association between race, lifetime PTSD and self-reported chronic illness. Weighted linear and Poisson regression models assessed differences in the magnitude of association between PTSD and chronic illness by race on both the additive and multiplicative scales.
Results
The magnitude of the association between lifetime PTSD and diabetes was greater among blacks (RD 0.07, 95% CI 0.02, 0.11; RR 1.9, 95% CI 1.4, 2.5) than whites (RD 0.004, 95% CI −0.02, 0.03; RR 1.2, 95% CI 0.7, 1.9) on the additive (p=0.017) scale. The magnitude of the association between lifetime PTSD and heart disease was greater among blacks (RD 0.09, 95% CI 0.05, 0.13) than whites (RD 0.04, 95% CI 0.01, 0.07) on the additive scale at a level approaching significance (p=0.051).
Conclusion
A lifetime history of PTSD was associated with a significantly greater risk of diabetes among blacks as compared to whites. These findings suggest that continuous exposure to racial inequalities may be associated with a greater risk of PTSD-related health sequela.
Keywords: chronic illness, health disparities, heart disease, posttraumatic stress disorder, race/ethnicity, type 2 diabetes
Introduction
Posttraumatic stress disorder (PTSD) is a psychiatric condition that develops after exposure to a traumatizing event. PTSD involves trauma-related intrusive thoughts, avoidance, and negative alterations in thoughts, mood, and reactivity (1). PTSD is often chronic and causes significant distress and interference in social and occupational functioning (1). It often co-occurs with other mental health conditions, including major depressive disorder and alcohol and substance abuse disorders (2). Individuals with PTSD are at increased risk for several health risk behaviors, including smoking (3, 4), poor sleep (5, 6), low exercise (4, 7), poor diet (5) and medication non-adherence (4). They experience high burdens of biomarkers for chronic illness, including higher levels of c-reactive protein (CRP) (8) and other markers of immune function (9), shorter telomere length (10), and alterations in epigenetic markers related to immune function (11). These risk factors, in turn, may predispose those with PTSD to a greater risk of developing chronic disease. Past research has demonstrated associations between PTSD and hypertension (12–15), obesity (16–20), metabolic disease (21), stroke (22) and type 2 diabetes (23–25). A prospective association between PTSD and incident heart disease has been well-established (26–30).
Non-Latino blacks share a disproportionate burden of chronic illness in the United States. Blacks have a higher prevalence of hypertension (31), stroke (31), obesity (32) and type 2 diabetes (33) as compared to non-Latino whites. The differential burden of chronic illness among blacks may arise in part through stress-mediated mechanisms related to a greater exposure to socioeconomic disadvantage (34) and experience of direct and indirect racism (35, 36). Evidence supporting these mechanisms include research examining differential burdens of biomarkers of stress by race, such as allostatic load (37, 38), as well as shortened telomere length (39, 40) and variations in gene methylation patterns, which may be heritable across generations (41, 42). Blacks also face barriers to receiving preventive medical care not experienced by whites (43, 44), which may additionally contribute to disparities in the development of chronic illness.
Although blacks have a higher lifetime burden of PTSD as compared to whites (8.7% vs. 7.4%, respectively) (45), little epidemiologic research has been conducted identifying whether PTSD is associated with a higher burden of chronic illness among blacks as compared to whites. Potential mechanisms that may lead to an exacerbation of the association between PTSD and chronic illness among blacks include the interaction of stress-mediated mechanisms linked to racial disparities with the physiological effects of PTSD, as well as barriers to utilizing treatment for PTSD (45) and to trauma disclosure (46) which may prolong the course of PTSD and thereby raise the subsequent risk of chronic illness. Research in depression has suggested that the magnitude of association between depression and chronic illness may be greater for blacks as compared to whites. In a cross-sectional study among women participating in NHANES 2001–2003, Read et al. reported a significantly greater association between depression and hypertension among non-Latino blacks than among non-Latino whites (47). In a prospective study of 24,443 participants in the national Reasons for Geographical and Racial Differences in Stroke cohort, Sims et al. found an association between depression and coronary heart disease among blacks, but no association among whites (48). Similarly, in a prospective study of 5,990 participants in the Chicago Health and Aging Project (CHAP), Lewis et al. found a significant association between depression and mortality from cardiovascular disease for African-Americans, but not for non-Latino whites (49).
As PTSD is associated with a higher risk of chronic illness and research has suggested that the link between depression and chronic illness may be greater for blacks as compared to whites, it is possible that a differential association between PTSD and chronic illness by race may also exist. Exploring this heterogeneity is important as the potential differential contribution of PTSD to development of chronic illnesses may further disadvantage a group that already experiences a disproportionate level of both PTSD and chronic disease. The primary aim of this study is to identify whether the association between PTSD and chronic illness is greater among blacks as compared to whites. To investigate this, we employed cross-sectional data from two large nationally-representative surveys.
Methods
This analysis utilized data from the nationally-representative National Survey of American Life (NSAL) (50) and National Comorbidity Survey Replication (NCS-R) (51), both conducted between 2001 and 2003. Both surveys were developed from the original National Comorbidity Survey, and utilized similar methodologies (52). The NCS-R was designed to be representative of the general United States population, and the NSAL was conducted nationally among African Americans and Afro-Caribbeans. This analysis includes non-Latino black participants in both the NSAL and NCS-R and non-Latino white participants in the NCS-R.
Both surveys evaluated the prevalence of and risk factors for psychiatric conditions, and additionally assessed physical comorbidities, including chronic illness. Psychiatric conditions were assessed using the World Health Survey update to the Composite International Diagnostic Interview (WMH-CIDI), a structured clinical interview utilizing Diagnostic and Statistical Manual, 4th edition (DSM-IV) criteria. Participants were selected into the study using a 4-stage sampling frame, with nested samples conducted in the following order: 1) Metropolitan Statistical Areas (MSAs) and counties, 2) area segments within selected MSAs and counties, 3) housing units within selected area segments, and 4) eligible respondents within selected housing units. Interviews were conducted within participants’ homes by trained lay interviewers using a computer-assisted personal interview (CAPI) format (52). Informed consent was obtained from all participants. Implementation of NSAL was approved by the University of Michigan institutional review board and implementation of NSC-R was approved by the Harvard Medical School and University of Michigan review boards. This secondary analysis was reviewed by the Partners Health Care Institutional Review Board.
Posttraumatic stress disorder
Lifetime prevalence of PTSD was assessed following DSM-IV criteria using the WMH-CIDI (52). Participants endorsed PTSD if they reported: 1) exposure to a traumatic event, 2) experiencing intense fear, helplessness or horror during the event, 3) persistent re-experiencing of the event, 4) three or more avoidance or numbing behaviors, 5) at least one symptom of increased arousal (e.g., trouble falling asleep, difficulty concentrating, irritability or anger), 6) a duration of symptoms lasting more than one month, and 7) a significant impairment in social or occupational functioning. The CIDI has been shown to have good test-retest (53) and inter-rater (54) reliability for PTSD, good agreement with the PTSD Checklist (PCL) (55), and low to moderate agreement with the clinician-administered World Mental Health Structured Clinical Interview (SCID) (56, 57) and with clinician diagnoses (58).
Chronic health conditions
The lifetime prevalence of several chronic illnesses was assessed in both the NSAL and NSC-R through self-report. Five chronic illnesses were evaluated in this study: hypertension, obesity, heart disease, stroke and diabetes. These chronic illnesses were selected because previous research has suggested a potential association of PTSD with each (12–25) and all five conditions were assessed in both the NSC-R and NSAL with comparable question content. With the exception of obesity, participants were asked whether they had been diagnosed by a physician with a given health condition. Hypertension was assessed as “high blood pressure”, diabetes as “diabetes or high blood sugar” and heart disease as “heart disease” in NCS-R and “heart trouble or have had a heart attack” in NSAL. Obesity was defined as having a body mass index greater than 30 kg/m2, and was calculated from self-report of weight and height. While PTSD and obesity were evaluated for all NCS-R survey participants, participants in NCS-R who were determined to be hard to recruit were asked to complete a shortened version of the NCS-R survey that did not assess chronic illnesses (51). Level of agreement between self-report of chronic illness and chronic illness as recorded in clinical records or established through physical measurement varies by the chronic illness assessed, and is highest for BMI (kappa 0.85) (59) and diabetes (kappa 0.80), moderate for hypertension (kappa 0.66) and acute myocardial infarction (kappa 0.48), and lowest for congestive heart failure (kappa 0.33) and stroke (kappa 0.36) (60).
Covariates
Demographic and health behavior covariates, including age, sex, annual household income (<$15,000, $15,000-<$35,000, $35,000-<$75,000 and ≥$75,000), highest level of education (<12 years, 12 years, ≥12 years) and current smoking, were assessed through self-report. Major depressive disorder was assessed following DSM-IV criteria using the WMH-CIDI (52). The CIDI has been shown to have good test-retest (53) and inter-rater (54) reliability for depression, and moderate agreement with clinician diagnoses (61).
Statistical analysis
All analyses were weighted to account for sampling probabilities with the exception of frequencies. Descriptive statistics were reported as non-weighted frequencies and weighted percents or weighted means and standard errors. The significance of between-group differences in proportions and means were determined through Rao-Scott chi-square tests or weighted linear regression, respectively. Due to the potential role of smoking and socioeconomic factors, including education and household income, to be mediators of the association between race and both PTSD and chronic health conditions, we a priori chose to limit adjustment in our primary multivariable models to age and sex. Because smoking and socioeconomic factors may additionally be confounders of the association between PTSD and chronic health conditions, we conducted secondary analyses adjusting for these factors. Additionally, because major depressive disorder may serve as both a mediator and a confounder of the association between PTSD and chronic health conditions, we initially ran models without major depressive disorder, but controlled for major depressive disorder in secondary analyses.
We assessed interaction on both the additive and multiplicative scales. By investigating interaction on the additive scale using risk differences, we tested the hypothesis that race and PTSD jointly have an association with chronic disease that is either significantly greater or less than that which would be expected if we summed the independent effects of race and PTSD on chronic illness. Similarly, by investigating interaction on the multiplicative scale using risk ratios, we tested the hypothesis that race and PTSD jointly have an association with chronic disease that is either significantly greater or less than that which would be expected if we took the product of the independent effects of race and PTSD on chronic illness. Whether the potential synergy between race and PTSD in their association with chronic illness is best represented on the additive or multiplicative scale is dependent on the complex underlying biological and psychosocial mechanisms of interaction.
To calculate risk differences and assess the significance of effect modification by way of additive statistical interaction, weighted least-squares linear regression using robust standard errors (62) was used to model the association between PTSD and the five chronic health conditions, for unadjusted models and models adjusted for age and sex. A p-value <0.05 for the t-statistic for the interaction term was used to indicate significance of interaction on the additive scale. To calculate risk ratios and assess the significance of effect modification by way of multiplicative statistical interaction, weighted Poisson regression, using robust standard errors (63), was implemented for unadjusted models and models adjusted for age and sex. A p-value <0.05 for the Wald statistic for the interaction term was used to indicate significance of interaction on the multiplicative scale.
We conducted two secondary analyses. First, to investigate the potential for socioeconomic position, smoking and lifetime major depressive disorder to confound the relationship between PTSD and chronic illnesses, we conducted secondary analyses adjusting for these factors. Second, to explore the potential for reverse causation in the cross-sectional design, where chronic illness may lead to development PTSD, secondary analyses were conducted excluding participants with age of onset of PTSD at or later than 35 years. Drawing from previous research, we chose age 35 because it represented an age before which onset of heart disease and stroke was unlikely (31) and at which the national prevalence of diabetes and hypertension was less than 10% (31, 64). All descriptive analyses were conducted using the survey package in SAS 9.3 (SAS Institute Inc., Cary, SC) and weighted least-squares linear and Poisson regression analyses were conducted in STATA (StataCorp. 2015).
Results
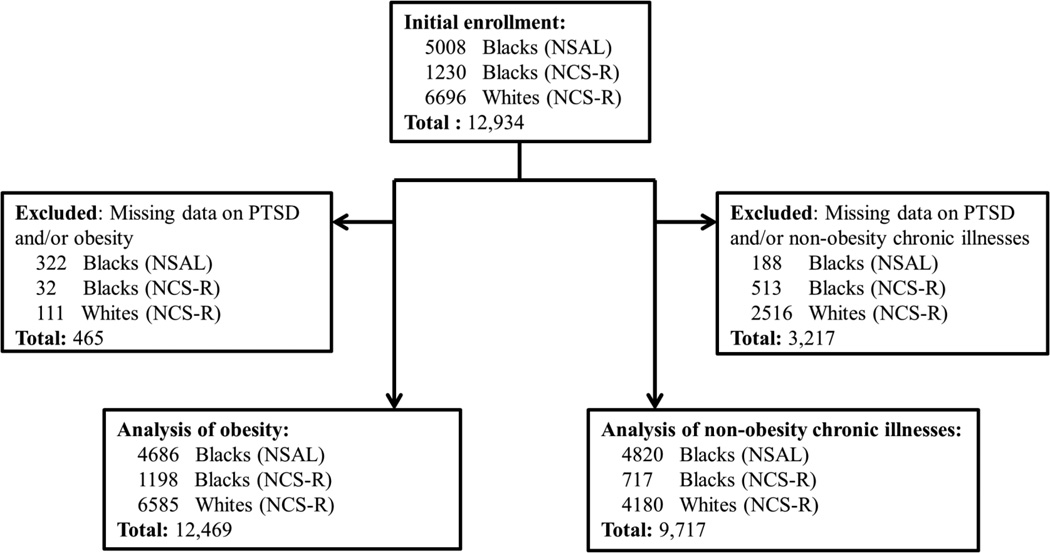
In total, 5,008 non-Latino blacks participated in NSAL and 1,230 non-Latino blacks and 6,696 non-Latino whites participated in NCS-R, for a total initial sample of 12,934 (Figure). In analyses investigating the association between PTSD and obesity, 465 participants were missing data on PTSD and/or obesity for a final sample size of 12,469. In analyses investigating PTSD and all other chronic health conditions, 3,217 were missing data on PTSD and/or all of the non-obesity chronic health conditions, for a final sample size of 9,717. Participants excluded from the analysis of PTSD and non-obesity chronic health conditions were significantly more likely to be older, male, have a lower income, be married/cohabitating, not smoke and not have a lifetime history of major depressive disorder.
Figure.
Flow chart for selecting participants into analysis from the National Survey of American Life (NSAL) and National Comorbidity Survey Replication (NCS-R)
Black participants were in general younger than white participants, and more likely to be female, have a lower household income, have less years of education, to not be married/cohabitating and to smoke. White participants were more likely to report lifetime major depressive disorder. Black participants had a higher prevalence of lifetime PTSD (weighted % 8.3% blacks and 6.3% whites) (Table 2), although no significant difference in mean age at onset was observed (weighted mean (SEM) 21.4 (0.8) blacks and 21.0 (0.8) whites). Lifetime prevalence of hypertension, obesity, heart disease and diabetes were significantly higher among black participants as compared to white participants, and no significant difference in lifetime prevalence of stroke was observed.
Table 2.
Posttraumatic stress disorder (PTSD) and chronic conditions by race.
| Non-Latino black |
Non-Latino white |
||||
|---|---|---|---|---|---|
| Unweighted n with chronic condition/total |
Weighted % |
Unweighted n with chronic condition/total |
Weighted % |
P1 | |
| Exposure | |||||
| DSM-IV PTSD (Lifetime) | |||||
| Endorsed | 486 | 8.3 | 432 | 6.3 | <0.001 |
| Not endorsed | 5564 | 91.7 | 6264 | 93.7 | |
| Outcomes | |||||
| Hypertension | |||||
| Yes | 1755 | 33.1 | 989 | 24.4 | <0.001 |
| No | 3806 | 66.9 | 3188 | 75.6 | |
| Obesity | |||||
| Yes (BMI ≥30 kg/m2) | 1986 | 34.5 | 1518 | 22.9 | <0.001 |
| No (BMI<30 kg/m2) | 3923 | 65.5 | 5067 | 77.1 | |
| Heart disease | |||||
| Yes | 388 | 7.1 | 241 | 5.5 | 0.012 |
| No | 5175 | 92.9 | 3935 | 94.5 | |
| Stroke | |||||
| Yes | 161 | 3.1 | 109 | 2.7 | 0.37 |
| No | 5402 | 96.9 | 4068 | 97.3 | |
| Diabetes | |||||
| Yes | 608 | 11.0 | 274 | 6.6 | <0.001 |
| No | 4959 | 89.0 | 3919 | 93.4 | |
Rao-Scott chi-square test or weighted linear regression
Hypertension
In unadjusted models, PTSD was not significantly associated with hypertension among either black or white participants. In models adjusting for age and sex, PTSD was associated with a significantly greater risk of hypertension among both black and white participants (Table 3). No statistical interaction between PTSD and race on risk of hypertension was observed on the additive or multiplicative scales.
Table 3.
Modification1 of the effect of Lifetime PTSD on chronic conditions by ethnicity; Unadjusted and adjusted risk differences and risk ratios2
| Model 1: Unadjusted, Linear | Model 2: Unadjusted, Poisson |
Model 3: Age and sex, Linear | Model 4: Age and sex, Poisson |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RD | (95% CI) | P | RR | (95% CI) | P | RD | (95% CI) | P | RR | (95% CI) | P | |
| Hypertension | ||||||||||||
| Non-Latino black | 0.050 | (−0.01, 0.11) | 0.10 | 1.15 | (0.98, 1.35) | 0.081 | 0.089 | (0.033, 0.14) | 0.002 | 1.41 | (1.21, 1.65) | <0.001 |
| Non-Latino white | −0.005 | (−0.06, 0.05) | 0.85 | 0.98 | (0.80, 1.21) | 0.85 | 0.048 | (−0.001 0.096) | 0.055 | 1.33 | (1.09, 1.63) | 0.006 |
| Interaction: | 0.054 | (−0.02, 0.13) | 0.17 | 1.18 | (0.90, 1.53) | 0.23 | 0.041 | (−0.032, 0.11) | 0.27 | 1.06 | (0.83, 1.36) | 0.64 |
| Obesity | ||||||||||||
| Non-Latino black | 0.067 | (0.010, 0.12) | 0.022 | 1.20 | (1.04, 1.38) | 0.014 | 0.073 | (0.016, 0.13) | 0.012 | 1.23 | (1.06, 1.42) | 0.005 |
| Non-Latino white | 0.064 | (0.012, 0.12) | 0.016 | 1.28 | (1.07, 1.54) | 0.007 | 0.071 | (0.019, 0.12) | 0.007 | 1.32 | (1.10, 1.59) | 0.003 |
| Interaction: | 0.004 | (−0.073, 0.080) | 0.93 | 0.93 | (0.74, 1.18) | 0.56 | 0.002 | (−0.074, 0.079) | 0.96 | 0.93 | (0.74, 1.17) | 0.52 |
| Heart Disease | ||||||||||||
| Non-Latino black | 0.070 | (0.03, 0.11) | 0.001 | 2.07 | (1.48, 2.91) | <0.001 | 0.088 | (0.046, 0.13) | <0.001 | 3.28 | (2.35, 4.58) | <0.001 |
| Non-Latino white | 0.014 | (−0.02, 0.045) | 0.39 | 1.25 | (0.78, 2.01) | 0.35 | 0.037 | (0.006, 0.067) | 0.018 | 2.40 | (1.51, 3.80) | <0.001 |
| Interaction | 0.056 | (0.003, 0.11) | 0.039 | 1.65 | (0.92, 2.96) | 0.09 | 0.051 | (−0.0004, 0.10) | 0.051 | 1.37 | (0.78, 2.40) | 0.28 |
| Stroke | ||||||||||||
| Non-Latino black | 0.018 | (−0.01, 0.047) | 0.21 | 1.62 | (0.87, 3.03) | 0.13 | 0.026 | (−0.003, 0.054) | 0.075 | 2.42 | (1.30, 4.51) | 0.005 |
| Non-Latino white | 0.015 | (−0.009, 0.039) | 0.23 | 1.57 | (0.84, 2.94) | 0.16 | 0.025 | (0.001, 0.48) | 0.044 | 2.79 | (1.49, 5.26) | 0.001 |
| Interaction | 0.003 | (−0.03, 0.04) | 0.86 | 1.03 | (0.43, 2.50) | 0.94 | 0.001 | (−0.036, 0.038) | 0.95 | 0.87 | (0.36, 2.06) | 0.75 |
| Diabetes | ||||||||||||
| Non-Latino black | 0.055 | (0.010, 0.10) | 0.017 | 1.52 | (1.14, 2.04) | 0.005 | 0.067 | (0.023, 0.11) | 0.003 | 1.91 | (1.44, 2.54) | <0.001 |
| Non-Latino white | −0.012 | (−0.041, 0.016) | 0.40 | 0.82 | (0.50, 1.34) | 0.43 | 0.004 | (−0.024, 0.032) | 0.790 | 1.16 | (0.71, 1.89) | 0.55 |
| Interaction | 0.068 | (0.014, 0.12) | 0.014 | 1.85 | (1.05, 3.28) | 0.034 | 0.063 | (0.011, 0.12) | 0.017 | 1.65 | (0.95, 2.86) | 0.076 |
Difference in risk differences used to calculate interaction on the additive scale and ratio of relative risks used to calculate interaction on the multiplicative scale
Linear regression with robust variance used to calculate risk differences and modified Poisson regression used to calculate risk ratios Totals: Hypertension n=9712, Obesity n=12,469, heart disease and diabetes n=9713, stroke n=9714
Obesity
In unadjusted models, PTSD was associated with a higher risk of obesity among both black and white participants. In models adjusting for age and sex, PTSD remained associated with a greater risk of obesity among both black and white participants. No statistical interaction between PTSD and race on risk of obesity was observed on the additive or multiplicative scales.
Heart disease
In unadjusted models, PTSD was associated with a greater risk of heart disease only among black participants, with a significant statistical interaction observed on the additive scale. In models adjusting for age and sex, PTSD was associated with a greater risk of heart disease among both black and white participants. In adjusted models, PTSD was associated with a close to significant greater risk of heart disease among black participants as compared to white participants on the additive scale (RD 0.088, 95% CI 0.046, 0.13 black; RD 0.037, 95% CI 0.006, 0.067 white; p-interaction=0.051). No significant difference by race was observed on the multiplicative scale (RR 3.28, 95% CI 2.35, 4.58 black; RR 2.40, 95% CI 1.51, 3.80 white; p-interaction=0.28).
Stroke
In unadjusted models, PTSD was not significantly associated with stroke among either black or white participants. After adjustment for age and sex, PTSD was associated with a greater risk of stroke among both black and white participants. No statistical interaction between PTSD and race on risk of stroke was observed on the additive or multiplicative scales.
Diabetes
In unadjusted models, PTSD was associated with a greater risk of diabetes only among black participants, with a significant statistical interaction observed between PTSD and race on both the additive and multiplicative scales. In models adjusting for age and sex, PTSD remained significantly associated with diabetes only among black participants. In adjusted models, the association between PTSD and diabetes among black participants was significantly greater than the association among white participants on the additive scale (RD 0.067, 95% CI 0.023, 0.11 black; RD 0.004, 95% CI −0.024, 0.032 white; p-interaction=0.017) but did not reach significance on the multiplicative scale (RR 1.91, 95% CI 1.44, 2.54 black; RR 1.16, 95% CI 0.71, 1.89 white; p-interaction=0.076).
Additional analyses
Adjusting models for socioeconomic position and smoking in addition to age and sex had little effect on estimates, although the estimates for stroke were slightly attenuated (Supplemental table A). Additionally adjusting for major depressive disorder led to a small attenuation of most estimates, although the majority of findings significant in the main models remained significant in the fully-adjusted models, with the exception of the risk difference for obesity (RD 0.018, 95% CI −0.060, 0.096) and stroke (RD 0.021, 95% CI −0.001, 0.004) for white participants. Notably, the difference in the association between PTSD and heart disease by race reached significance on the additive scale after adjustment for socioeconomic position, smoking and depression (RD 0.084, 95% CI 0.042, 0.13 black; RD 0.032, 95% CI 0.001, 0.062 white; p-interaction=0.044).
After excluding participants who developed PTSD at or later than age 35 (Supplemental table B), the majority of effect estimates remained similar to those in the main analyses, although the risk differences were notably attenuated for hypertension (RD 0.065, 95% CI 0.003, 0.13 blacks; RD 0.039, 95% CI −0.012, 0.091 whites) and diabetes (RD 0.051, 95% CI 0.005, 0.096 blacks; RD 0.011, 95% CI −0.020, 0.041 whites). None of the interaction terms for race and PTSD reached significance in this subset.
Discussion
In this cross-sectional analysis in two comparable nationally-representative surveys, we found that PTSD was associated with a greater risk of chronic illness among both black and white participants, with the exception of the association between PTSD and type 2 diabetes among whites. After adjusting for age and sex, we found that the association between PTSD and risk of type 2 diabetes was significantly greater among black participants than among white participants on an additive scale. We also found that the association between PTSD and heart disease was close to significantly greater among black participants than among white participants on the additive scale, and that this interaction became significant after additionally adjusting for socioeconomic position, smoking and major depressive disorder. Although past research has demonstrated associations between PTSD and chronic illness overall (12–30) and differential associations between depression and chronic illnesses by race (47–49), the findings in this study of a differential association between PTSD and chronic illness by race are novel.
PTSD was significantly associated with hypertension among both black and white participants (41% and 33% greater risk, respectively) in adjusted models, with estimates similar to or lower than those found in previous research (12–15). In a study of 9,463 participants in the National Epidemiological Survey of Alcohol and Related Conditions (NESARC), Pietrzak et al. found PTSD to be associated with a significant 30% greater odds of hypertension (14). Our findings of no significant differences in the association between PTSD and hypertension by race contrast with findings for depression and hypertension by Read et al., where the authors report a significantly greater magnitude of association between depression and hypertension among blacks as compared to whites (47). The lack of significant findings for interaction in our study may be due to misclassification in self-reported hypertension.
PTSD was significantly associated with obesity among both black and white participants (23% and 32% greater risk, respectively) in adjusted models, with estimates similar to or lower than those found in previous research (16–20). Among 463 African Americans participating in the Detroit Neighborhood Health Study, Mitchell et al. found that PTSD was associated with a greater than 4-fold increase in odds of obesity among women, but was not associated with obesity among men (20). We did not find that the magnitude of the association between PTSD and obesity was significantly different by race. It is possible that gender may serve as an additional moderator of the association between PTSD, race and obesity, and we were underpowered to observe this complex set of interactions.
PTSD was significantly associated with heart disease among both black and white participants (3.3-fold and 2.4-fold greater risk, respectively) in adjusted models, with estimates exceeding the majority of those found in prospective studies (26–30). In a systematic review of 5 prospective studies published in 2013, Edmondson et al. found that PTSD was associated with a 27% greater risk of incident coronary heart disease after adjustment for depression (26). Our findings of a close to significant greater magnitude of association between PTSD and heart disease among blacks as compared to whites is similar to past studies investigating racial disparities in the association between depression and cardiovascular disease, with two studies having found that depression was associated with a greater risk of cardiovascular disease among blacks but not among whites (48, 49). Our findings add to this evidence base, further supporting a potential interaction between racial disparities and psychological distress in increasing risk of heart disease.
PTSD was significantly associated with stroke among both black and white participants (2.4-fold and 2.8-fold greater risk, respectively) in adjusted models, similar to findings from one previous study. Among 5,217 participants in the Taiwan National Health Insurance Research Database, Chen et al. found that PTSD was associated with a greater than 3-fold risk of developing stroke (22). We did not find that the magnitude of the association between PTSD and stroke differed significantly by race. It should be noted that due to the cross-sectional nature of our study, we could not control for the potential for reverse causation, with stroke leading to the development of PTSD (65). Indeed, after excluding participants who developed PTSD after age 35, the estimates were attenuated, yet still significant on the ratio scale.
PTSD was significantly associated with a 90% greater risk of type 2 diabetes among black participants in adjusted models, but was not significantly associated with type 2 diabetes among white participants. The estimate for the association between PTSD and type 2 diabetes among blacks was similar to or lower than estimates found in previous studies (23–25). Among 49,730 women participating in the Nurses’ Health Study II, Roberts et al. found that having 6–7 trauma symptoms as compared to no trauma symptoms was associated with an 80% greater odds of incident type 2 diabetes (24). To our knowledge, our findings of a significant difference in the magnitude of association between PTSD and type 2 diabetes by race has not been demonstrated for depression and type 2 diabetes.
There are several key limitations that should be taken into account in the interpretation of our findings. First, because this study is observational, causal relationships could not be determined, and because this study is cross-sectional, temporal associations between PTSD and chronic illnesses could not be established. It is possible that some of the chronic illnesses assessed, particularly stroke, may have led to development of PTSD. To investigate this issue, we conducted a secondary analysis excluding participants who developed PTSD at or later than age 35, and although we found some attenuation of estimates, the majority of the associations between PTSD and the chronic illnesses remained similar. However, because all data was collected at one time-point, and potentially subject to recall bias, we cannot adequately assess temporality. Future longitudinal research is needed to establish both the temporality of these relationships and better isolate potential underlying mechanisms of action.
Second, chronic illnesses were assessed through self-report, likely leading to misclassification. We do not anticipate that misclassification of chronic illnesses would be related to endorsement of PTSD or to race, although past research on validity of self-report of chronic illness by PTSD and race is sparse (66, 67). Previous research has demonstrated that self-report of some chronic illnesses, notably stroke and heart disease, have moderate to low agreement with clinical records, and therefore the findings for these chronic illnesses may be more severely biased towards the null (Muggah, 2013; Machon, 2013). Third, a large proportion of participants in NCS-R were not assessed for chronic illnesses other than obesity, and these participants differed on many sociodemographic and behavioral factors from those included in analyses. It is possible this exclusion led to a selection bias, although this was likely minimized through the use of sampling weights accounting for this non-response. Finally, the NCS-R and NSAL were conducted between 2001 and 2003, and therefore our results should be generalized to the present with caution, particularly in relation to recent changes in potential mediating factors. This includes changes such as increased access to medical care under the Patient Protection and Affordable Care Act, which may reduce some of the racial inequities in both access to treatment for PTSD and access to preventive care for heart disease and diabetes.
The findings of a differential association between PTSD and type 2 diabetes by race, and a close to significant differential association between PTSD and heart disease by race, provides further evidence that the impact of stress-related mental health conditions on chronic disease may be greater among individuals affected by the social and economic disadvantages generated through institutional racism. Because PTSD is often a long-term chronic illness, targeting early treatment to individuals at high risk of PTSD-related sequela may help reduce future risk of chronic disease. While blacks have a higher prevalence of PTSD than whites (45) and may experience a higher risk of PTSD-related sequela, research has shown that blacks have low levels of access to mental health services (68). Therefore, addressing low access to care for individuals experiencing trauma in the black community is vital. Further, more research is needed to understand how the sources of stress associated with racism coupled with a diagnosis of PTSD may contribute to some but not all chronic illnesses. In addition to medical intervention at the individual level, such efforts could inform broader upstream strategies aimed at reducing health inequities.
Supplementary Material
Table 1.
Study population characteristics by race.
| Non-Latino black (n=6238) |
Non-Latino white (n=6696) |
||||
|---|---|---|---|---|---|
| n | % | n | % | P1 | |
| Age (mean, SEM) | 42.2 | 0.3 | 46.3 | 0.2 | <0.001 |
| Sex | |||||
| Female | 3942 | 55.4 | 3618 | 51.6 | <0.001 |
| Male | 2296 | 44.6 | 3078 | 48.4 | |
| Income | |||||
| <$15,000 | 1498 | 24.7 | 519 | 12.9 | <0.001 |
| $15,000–<$30,000 | 1977 | 32.6 | 845 | 20.3 | |
| $30,000–<$50,000 | 1670 | 31.0 | 1516 | 35.7 | |
| $50,000+ | 580 | 11.6 | 1300 | 31.2 | |
| Education | |||||
| 0–11 years | 1440 | 23.7 | 824 | 13.0 | <0.001 |
| 12 years | 2171 | 36.7 | 1983 | 31.3 | |
| 13+ years | 2627 | 39.6 | 3889 | 55.8 | |
| Marital Status | |||||
| Married/cohabitating | 2315 | 40.8 | 4052 | 59.5 | <0.0 01 |
| Divorced/separated/widowed | 1834 | 26.3 | 1446 | 19.9 | |
| Never married | 2081 | 32.9 | 1198 | 20.6 | |
| Current smoker | |||||
| Yes | 1426 | 26.7 | 1660 | 24.9 | 0.051 |
| No | 4613 | 73.3 | 5035 | 75.1 | |
| Lifetime major depression | |||||
| Yes | 640 | 10.5 | 1202 | 17.8 | <0.001 |
| No | 5430 | 89.5 | 5494 | 82.2 | |
Rao-Scott chi-square test or weighted linear regression
Research highlights.
Posttraumatic stress disorder (PTSD) is linked to a greater risk of chronic illness
Exposure to social inequities may lead to a greater susceptibility to PTSD sequelae
We evaluated moderation of the relationship between PTSD and chronic illness by race
PTSD was more strongly associated with diabetes among blacks versus whites
Social inequities and mental health may contribute synergistically to chronic illness
Acknowledgments
Time for this manuscript was funded in part by a grant from the National Institute of Mental Health (NIMH K23 MH096029-01A1) awarded to Dr. Luana Marques.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®) American Psychiatric Pub. 2013 [Google Scholar]
- 2.Schnurr PP, Friedman MJ, Bernardy NC. Research on posttraumatic stress disorder: epidemiology, pathophysiology, and assessment. Journal of clinical psychology. 2002;58(8):877–889. doi: 10.1002/jclp.10064. [DOI] [PubMed] [Google Scholar]
- 3.Feldner MT, Babson KA, Zvolensky MJ. Smoking, traumatic event exposure, and post-traumatic stress: A critical review of the empirical literature. Clinical psychology review. 2007;27(1):14–45. doi: 10.1016/j.cpr.2006.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zen AL, Whooley MA, Zhao S, Cohen BE. Post-traumatic stress disorder is associated with poor health behaviors: findings from the heart and soul study. Health psychology : official journal of the Division of Health Psychology, American Psychological Association. 2012;31(2):194–201. doi: 10.1037/a0025989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gavrieli A, Farr OM, Davis CR, Crowell JA, Mantzoros CS. Early life adversity and/or posttraumatic stress disorder severity are associated with poor diet quality, including consumption of trans fatty acids, and fewer hours of resting or sleeping in a US middle-aged population: A cross-sectional and prospective study. Metabolism: clinical and experimental. 2015;64(11):1597–1610. doi: 10.1016/j.metabol.2015.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Talbot LS, Rao MN, Cohen BE, Richards A, Inslicht SS, O’Donovan A, et al. Metabolic risk factors and posttraumatic stress disorder: the role of sleep in young, healthy adults. Psychosomatic medicine. 2015;77(4):383–391. doi: 10.1097/PSY.0000000000000176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Godfrey KM, Lindamer LA, Mostoufi S, Afari N. Posttraumatic stress disorder and health: a preliminary study of group differences in health and health behaviors. Annals of general psychiatry. 2013;12(1):30. doi: 10.1186/1744-859X-12-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Heath NM, Chesney SA, Gerhart JI, Goldsmith RE, Luborsky JL, Stevens NR, et al. Interpersonal violence, PTSD, and inflammation: potential psychogenic pathways to higher C-reactive protein levels. Cytokine. 2013;63(2):172–178. doi: 10.1016/j.cyto.2013.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vidovic A, Gotovac K, Vilibic M, Sabioncello A, Jovanovic T, Rabatic S, et al. Repeated assessments of endocrine- and immune-related changes in posttraumatic stress disorder. Neuroimmunomodulation. 2011;18(4):199–211. doi: 10.1159/000322869. [DOI] [PubMed] [Google Scholar]
- 10.Jergovic M, Tomicevic M, Vidovic A, Bendelja K, Savic A, Vojvoda V, et al. Telomere shortening and immune activity in war veterans with posttraumatic stress disorder. Progress in neuro-psychopharmacology & biological psychiatry. 2014;54:275–283. doi: 10.1016/j.pnpbp.2014.06.010. [DOI] [PubMed] [Google Scholar]
- 11.Uddin M, Aiello AE, Wildman DE, Koenen KC, Pawelec G, de Los Santos R, et al. Epigenetic and immune function profiles associated with posttraumatic stress disorder. Proceedings of the National Academy of Sciences of the United States of America. 2010;107(20):9470–9475. doi: 10.1073/pnas.0910794107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kibler JL, Joshi K, Ma M. Hypertension in relation to posttraumatic stress disorder and depression in the US National Comorbidity Survey. Behavioral medicine (Washington, DC) 2009;34(4):125–132. doi: 10.3200/BMED.34.4.125-132. [DOI] [PubMed] [Google Scholar]
- 13.Paulus EJ, Argo TR, Egge JA. The impact of posttraumatic stress disorder on blood pressure and heart rate in a veteran population. Journal of traumatic stress. 2013;26(1):169–172. doi: 10.1002/jts.21785. [DOI] [PubMed] [Google Scholar]
- 14.Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Physical health conditions associated with posttraumatic stress disorder in U.S. older adults: results from wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of the American Geriatrics Society. 2012;60(2):296–303. doi: 10.1111/j.1532-5415.2011.03788.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abouzeid M, Kelsall HL, Forbes AB, Sim MR, Creamer MC. Posttraumatic stress disorder and hypertension in Australian veterans of the 1991 Gulf War. Journal of psychosomatic research. 2012;72(1):33–38. doi: 10.1016/j.jpsychores.2011.08.002. [DOI] [PubMed] [Google Scholar]
- 16.Dedert EA, Becker ME, Fuemmeler BF, Braxton LE, Calhoun PS, Beckham JC. Childhood traumatic stress and obesity in women: the intervening effects of PTSD and MDD. Journal of traumatic stress. 2010;23(6):785–763. doi: 10.1002/jts.20584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pagoto SL, Schneider KL, Bodenlos JS, Appelhans BM, Whited MC, Ma Y, et al. Association of post-traumatic stress disorder and obesity in a nationally representative sample. Obesity (Silver Spring, Md) 2012;20(1):200–205. doi: 10.1038/oby.2011.318. [DOI] [PubMed] [Google Scholar]
- 18.Farr OM, Ko BJ, Joung KE, Zaichenko L, Usher N, Tsoukas M, et al. Posttraumatic stress disorder, alone or additively with early life adversity, is associated with obesity and cardiometabolic risk. Nutrition, metabolism, and cardiovascular diseases : NMCD. 2015;25(5):479–488. doi: 10.1016/j.numecd.2015.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kubzansky LD, Bordelois P, Jun HJ, Roberts AL, Cerda M, Bluestone N, et al. The weight of traumatic stress: a prospective study of posttraumatic stress disorder symptoms and weight status in women. JAMA psychiatry. 2014;71(1):44–51. doi: 10.1001/jamapsychiatry.2013.2798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mitchell KS, Aiello AE, Galea S, Uddin M, Wildman D, Koenen KC. PTSD and obesity in the Detroit neighborhood health study. General hospital psychiatry. 2013;35(6):671–673. doi: 10.1016/j.genhosppsych.2013.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rosenbaum S, Stubbs B, Ward PB, Steel Z, Lederman O, Vancampfort D. The prevalence and risk of metabolic syndrome and its components among people with posttraumatic stress disorder: a systematic review and meta-analysis. Metabolism: clinical and experimental. 2015;64(8):926–933. doi: 10.1016/j.metabol.2015.04.009. [DOI] [PubMed] [Google Scholar]
- 22.Chen MH, Pan TL, Li CT, Lin WC, Chen YS, Lee YC, et al. Risk of stroke among patients with post-traumatic stress disorder: nationwide longitudinal study. The British journal of psychiatry : the journal of mental science. 2015;206(4):302–307. doi: 10.1192/bjp.bp.113.143610. [DOI] [PubMed] [Google Scholar]
- 23.Lukaschek K, Baumert J, Kruse J, Emeny RT, Lacruz ME, Huth C, et al. Relationship between posttraumatic stress disorder and type 2 diabetes in a population-based cross-sectional study with 2970 participants. Journal of psychosomatic research. 2013;74(4):340–345. doi: 10.1016/j.jpsychores.2012.12.011. [DOI] [PubMed] [Google Scholar]
- 24.Roberts AL, Agnew-Blais JC, Spiegelman D, Kubzansky LD, Mason SM, Galea S, et al. Posttraumatic stress disorder and incidence of type 2 diabetes mellitus in a sample of women: a 22-year longitudinal study. JAMA psychiatry. 2015;72(3):203–210. doi: 10.1001/jamapsychiatry.2014.2632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jacob MM, Gonzales KL, Calhoun D, Beals J, Muller CJ, Goldberg J, et al. Psychological trauma symptoms and Type 2 diabetes prevalence, glucose control, and treatment modality among American Indians in the Strong Heart Family Study. Journal of diabetes and its complications. 2013;27(6):553–557. doi: 10.1016/j.jdiacomp.2013.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Edmondson D, Kronish IM, Shaffer JA, Falzon L, Burg MM. Posttraumatic stress disorder and risk for coronary heart disease: a meta-analytic review. American heart journal. 2013;166(5):806–814. doi: 10.1016/j.ahj.2013.07.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Beristianos MH, Yaffe K, Cohen B, Byers AL. PTSD and Risk of Incident Cardiovascular Disease in Aging Veterans. The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry. 2014 doi: 10.1016/j.jagp.2014.12.003. [DOI] [PubMed] [Google Scholar]
- 28.Sumner JA, Kubzansky LD, Elkind MS, Roberts AL, Agnew-Blais J, Chen Q, et al. Trauma Exposure and Posttraumatic Stress Disorder Symptoms Predict Onset of Cardiovascular Events in Women. Circulation. 2015;132(4):251–259. doi: 10.1161/CIRCULATIONAHA.114.014492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kubzansky LD, Koenen KC, Spiro A, 3rd, Vokonas PS, Sparrow D. Prospective study of posttraumatic stress disorder symptoms and coronary heart disease in the Normative Aging Study. Archives of general psychiatry. 2007;64(1):109–116. doi: 10.1001/archpsyc.64.1.109. [DOI] [PubMed] [Google Scholar]
- 30.Hendrickson CM, Neylan TC, Na B, Regan M, Zhang Q, Cohen BE. Lifetime trauma exposure and prospective cardiovascular events and all-cause mortality: findings from the Heart and Soul Study. Psychosomatic medicine. 2013;75(9):849–855. doi: 10.1097/PSY.0b013e3182a88846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–e322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 32.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. Jama. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Selvin E, Parrinello CM, Sacks DB, Coresh J. Trends in prevalence and control of diabetes in the United States, 1988–1994 and 1999–2010. Annals of internal medicine. 2014;160(8):517–525. doi: 10.7326/M13-2411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Geronimus AT. The weathering hypothesis and the health of African-American women and infants: evidence and speculations. Ethnicity & disease. 1992;2(3):207–221. [PubMed] [Google Scholar]
- 35.Harrell CJP, Burford TI, Cage BN, Nelson TM, Shearon S, Thompson A, et al. Multiple pathways linking racism to health outcomes. Du Bois review: social science research on race. 2011;8(01):143–157. doi: 10.1017/S1742058X11000178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Williams DR. Race, socioeconomic status, and health the added effects of racism and discrimination. Annals of the New York Academy of Sciences. 1999;896(1):173–188. doi: 10.1111/j.1749-6632.1999.tb08114.x. [DOI] [PubMed] [Google Scholar]
- 37.Doamekpor LA, Dinwiddie GY. Allostatic load in foreign-born and US-born blacks: evidence from the 2001–2010 National Health and Nutrition Examination Survey. American journal of public health. 2015;105(3):591–597. doi: 10.2105/AJPH.2014.302285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Beckie TM. A systematic review of allostatic load, health, and health disparities. Biological research for nursing. 2012;14(4):311–346. doi: 10.1177/1099800412455688. [DOI] [PubMed] [Google Scholar]
- 39.Chae DH, Nuru-Jeter AM, Adler NE, Brody GH, Lin J, Blackburn EH, et al. Discrimination, racial bias, and telomere length in African-American men. American journal of preventive medicine. 2014;46(2):103–111. doi: 10.1016/j.amepre.2013.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Diez Roux AV, Ranjit N, Jenny NS, Shea S, Cushman M, Fitzpatrick A, et al. Race/ethnicity and telomere length in the Multi-Ethnic Study of Atherosclerosis. Aging cell. 2009;8(3):251–257. doi: 10.1111/j.1474-9726.2009.00470.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kuzawa CW, Sweet E. Epigenetics and the embodiment of race: developmental origins of US racial disparities in cardiovascular health. American journal of human biology : the official journal of the Human Biology Council. 2009;21(1):2–15. doi: 10.1002/ajhb.20822. [DOI] [PubMed] [Google Scholar]
- 42.Halfon N, Larson K, Lu M, Tullis E, Russ S. Lifecourse health development: past, present and future. Maternal and child health journal. 2014;18(2):344–365. doi: 10.1007/s10995-013-1346-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gaskin DJ, Dinwiddie GY, Chan KS, McCleary R. Residential segregation and disparities in health care services utilization. Medical care research and review : MCRR. 2012;69(2):158–175. doi: 10.1177/1077558711420263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pathman DE, Fowler-Brown A, Corbie-Smith G. Differences in access to outpatient medical care for black and white adults in the rural South. Medical care. 2006;44(5):429–438. doi: 10.1097/01.mlr.0000207487.85689.a8. [DOI] [PubMed] [Google Scholar]
- 45.Roberts AL, Gilman SE, Breslau J, Breslau N, Koenen KC. Race/ethnic differences in exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking for post-traumatic stress disorder in the United States. Psychological medicine. 2011;41(1):71–83. doi: 10.1017/S0033291710000401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tillman S, Bryant-Davis T, Smith K, Marks A. Shattering silence: exploring barriers to disclosure for African American sexual assault survivors. Trauma, violence & abuse. 2010;11(2):59–70. doi: 10.1177/1524838010363717. [DOI] [PubMed] [Google Scholar]
- 47.Read JG, Gorman BK. Racial/ethnic differences in hypertension and depression among US adult women. Ethnicity & disease. 2007;17(2):389–396. [PubMed] [Google Scholar]
- 48.Sims M, Redmond N, Khodneva Y, Durant RW, Halanych J, Safford MM. Depressive symptoms are associated with incident coronary heart disease or revascularization among blacks but not among whites in the Reasons for Geographical and Racial Differences in Stroke study. Annals of epidemiology. 2015;25(6):426–432. doi: 10.1016/j.annepidem.2015.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lewis TT, Guo H, Lunos S, Mendes de Leon CF, Skarupski KA, Evans DA, et al. Depressive symptoms and cardiovascular mortality in older black and white adults: evidence for a differential association by race. Circulation Cardiovascular quality and outcomes. 2011;4(3):293–299. doi: 10.1161/CIRCOUTCOMES.110.957548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jackson JS, Torres M, Caldwell CH, Neighbors HW, Nesse RM, Taylor RJ, et al. The National Survey of American Life: a study of racial, ethnic and cultural influences on mental disorders and mental health. International journal of methods in psychiatric research. 2004;13(4):196–207. doi: 10.1002/mpr.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kessler RC, Berglund P, Chiu WT, Demler O, Heeringa S, Hiripi E, et al. The US National Comorbidity Survey Replication (NCS-R): design and field procedures. International journal of methods in psychiatric research. 2004;13(2):69–92. doi: 10.1002/mpr.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pennell BE, Bowers A, Carr D, Chardoul S, Cheung GQ, Dinkelmann K, et al. The development and implementation of the National Comorbidity Survey Replication, the National Survey of American Life, and the National Latino and Asian American Survey. International journal of methods in psychiatric research. 2004;13(4):241–269. doi: 10.1002/mpr.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wittchen HU, Lachner G, Wunderlich U, Pfister H. Test-retest reliability of the computerized DSM-IV version of the Munich-Composite International Diagnostic Interview (M-CIDI) Social psychiatry and psychiatric epidemiology. 1998;33(11):568–578. doi: 10.1007/s001270050095. [DOI] [PubMed] [Google Scholar]
- 54.Wittchen HU. Reliability and validity studies of the WHO--Composite International Diagnostic Interview (CIDI): a critical review. Journal of psychiatric research. 1994;28(1):57–84. doi: 10.1016/0022-3956(94)90036-1. [DOI] [PubMed] [Google Scholar]
- 55.Lang AJ, Laffaye C, Satz LE, Dresselhaus TR, Stein MB. Sensitivity and specificity of the PTSD checklist in detecting PTSD in female veterans in primary care. Journal of traumatic stress. 2003;16(3):257–264. doi: 10.1023/A:1023796007788. [DOI] [PubMed] [Google Scholar]
- 56.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of general psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 57.Kessler RC, Santiago PN, Colpe LJ, Dempsey CL, First MB, Heeringa SG, et al. Clinical reappraisal of the Composite International Diagnostic Interview Screening Scales (CIDI-SC) in the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS) International journal of methods in psychiatric research. 2013;22(4):303–321. doi: 10.1002/mpr.1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Komiti AA, Jackson HJ, Judd FK, Cockram AM, Kyrios M, Yeatman R, et al. A comparison of the Composite International Diagnostic Interview (CIDI-Auto) with clinical assessment in diagnosing mood and anxiety disorders. The Australian and New Zealand journal of psychiatry. 2001;35(2):224–230. doi: 10.1046/j.1440-1614.2001.00868.x. [DOI] [PubMed] [Google Scholar]
- 59.Ahluwalia IB, Tessaro I, Rye S, Parker L. Self-reported and clinical measurement of three chronic disease risks among low-income women in West Virginia. Journal of women’s health (2002) 2009;18(11):1857–1862. doi: 10.1089/jwh.2009.1360. [DOI] [PubMed] [Google Scholar]
- 60.Muggah E, Graves E, Bennett C, Manuel DG. Ascertainment of chronic diseases using population health data: a comparison of health administrative data and patient self-report. BMC public health. 2013;13:16. doi: 10.1186/1471-2458-13-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kessler RC, Wittchen H-U, Abelson JM, Mcgonagle K, Schwarz N, Kendler KS, et al. Methodological studies of the Composite International Diagnostic Interview (CIDI) in the US national comorbidity survey (NCS) 1998 [Google Scholar]
- 62.Cheung YB. A modified least-squares regression approach to the estimation of risk difference. American journal of epidemiology. 2007;166(11):1337–1344. doi: 10.1093/aje/kwm223. [DOI] [PubMed] [Google Scholar]
- 63.Zou G. A modified poisson regression approach to prospective studies with binary data. American journal of epidemiology. 2004;159(7):702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 64.National Center for Disease Control and Prevention. National Diabetes Statistics Report: Estimates of Diabetes and Its Burden in the United States, 2014. Atlanta, GA: US Department of Health and Human Services; 2014. [Google Scholar]
- 65.Edmondson D, Richardson S, Fausett JK, Falzon L, Howard VJ, Kronish IM. Prevalence of PTSD in survivors of stroke and transient ischemic attack: a meta-analytic review. 2013 doi: 10.1371/journal.pone.0066435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gillum RF, Sempos CT. Ethnic variation in validity of classification of overweight and obesity using self-reported weight and height in American women and men: the Third National Health and Nutrition Examination Survey. Nutrition journal. 2005;4:27. doi: 10.1186/1475-2891-4-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.McAdams MA, Van Dam RM, Hu FB. Comparison of self-reported and measured BMI as correlates of disease markers in US adults. Obesity (Silver Spring, Md) 2007;15(1):188–196. doi: 10.1038/oby.2007.504. [DOI] [PubMed] [Google Scholar]
- 68.Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Archives of general psychiatry. 2005;62(6):629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.