Abstract
Objective
We examined the association between physical activity recorded by Actigraphy during therapy sessions (therapy) to therapist rated patient participation and self reported future functional outcomes. We hypothesized those participants who were more active during rehab would have higher participation scores and better functional outcomes following hip fracture compared to those who were less active.
Design
Longitudinal study with 3 and 6 month follow-up.
Setting
Participants were recruited from skilled nursing (SN) and inpatient rehabilitation (IR) facilities.
Participants
Participants included 18 community dwelling older adults admitted to SN or IR facilities after hip fracture. Participants were included if they were ≥ 60 years of age and ambulatory with or without assistance from a device or another person.
Intervention
Not Applicable
Main Outcome Measure
Physical activity was quantified during participants’ rehab using the Actigraph accelerometer worn consecutively over 5 days. The Pittsburgh Participation Rating Scale was used to quantify patient participation during their inpatient therapy sessions. Self reported functional outcomes were measured by the Hip Fracture Functional Recovery Scale (HFRS) at baseline, 3 and 6 months following fracture.
Results
Participants with higher Actigraphy counts during rehab were ranked by their therapists as having excellent participation compared to those who were less active. Participants who were more active reported better functional abilities at both 3 and 6 month time points and achieved 78% and 91% recovery of self reported pre-fracture function compared to those who were less active achieving 64% and 73% recovery.
Conclusion
Actigraphy provides an objective measure of physical activity exhibiting predictive validity for future functional outcomes and concurrent validity against patient participation in patients after hip fracture.
Keywords: Hip Fracture, Physical Activity, Patient Participation
Approximately 250,000 adults sustain hip fractures annually in the United States1 with mortality one year following hip fracture approaching 25%. 2 Factors which predict decreased survival after hip fracture include age, number of co-morbidities, physical activity status at the time of fracture, discharge to a nursing home, and mental deterioration during the hospitalization.3 Of those surviving, nearly 50% of do not regain their former functional level. 4 Therefore, many patients require post acute care rehabilitation that can be delivered in skilled nursing (SN) or inpatient rehabilitation (IR) facilities. A comprehensive rehabilitation program that attempts to return a patient to pre-fracture functional status has been shown to produce positive outcomes. 5,6,7
Patient participation and physical activity during rehabilitation are thought to impact functional outcomes yet seldom are both defined and quantified by health care professionals. A patients’ motivation is a key component of a successful rehabilitation outcome8 however, a reliable measurement of motivation has not been achieved in the rehabilitation setting.9 A proposed alternative to measuring patient motivation is quantifying the observable behavior of patient participation which sometimes can be influenced by intervention.10,11 As rehabilitation stays are shortening, it will be advantageous for clinicians to quickly and accurately assess their patients’ participation.
The amount of physical activity achieved by patients during their rehabilitation stay is often described by documenting the distance the patient walked, the number of stairs they negotiated, the number of repetitions of exercises they performed or the time spent performing certain activities. Research measuring the specific intensity of physical activity during rehabilitation is limited and instead intensity is often described by the hours of therapy received.12 Hours of therapy received are not indicative of the intensity of care received; therefore, healthcare professionals need a way to further quantify the amount and intensity of physical activity their patients achieve during rehabilitation. Previous research in patients with hip fracture have used self report measures to quantify physical activity 13, 14, 15, 16 which are not ideal because patients are less accurate in recalling light to moderate intensity activities such as walking and error associated with recall is estimated to be between 35 and 50%. 17, 18, 19, 20 The purpose for our longitudinal study was two fold 1) to examine the association between therapist rated patient participation and physical activity measured by actigraphy during physical and occupational therapy sessions (therapy) (i.e. concurrent validity) and 2) to examine the association between physical activity during therapy with self reported functional outcomes at 3 and 6 months after hip fracture (predictive validity). We hypothesized those participants who were more active during therapy would have higher participation scores and better functional outcomes at 3 and 6 months following hip fracture compared to those who were less active.
METHODS
Participants
Participants for this study included 18 community dwelling older adults (mean age 78.6 (8.95) years, 72.2% female) who were admitted to SN or IR after hip fracture. The majority of our participants (89%; 16/18) were in IR versus SN (11%; 2/18).
Participants sustaining a proximal femoral fracture who were interested in the study were included if they were ≥ 60 years of age and ambulatory with or without assistance from a device or another person after their fracture. Participants were excluded if they were non weight bearing after fracture, had bilateral or additional fractures other than the femur, had a medical history of significant cognitive deficits, or were hemodynamically unstable (i.e. active bleeding with hypotension, uncontrolled arrhythmias, uncontrolled hypertension). The study coordinator was contacted after the potential participant expressed interest in the study to the physical or occupational therapist involved in their care within the first week of their rehabilitation stay. The potential participant was then screened by the study coordinator and written informed consent was obtained prior to any data collection. Demographic data and phone contact numbers (personal and alternative) were then collected on the participants. This study was approved by the University of Pittsburgh Institutional Review Board.
Measures
Physical Activity
Physical activity was quantified using the Actigraph accelerometer (Actigraph, LLC, Fort Walton Beach, FL.). Accelerometers are electronic sensors able to measure and store real time estimates of the frequency, intensity, and duration of physical activity. 21,22 The Actigraph accelerometer has been shown to be a reliable tool validated against direct observations, measures of energy expenditure, self report physical activity measures, and other accelerometers.23 The Actigraph has been used in healthy adults and children as well as in participants with gait abnormalities or physical disabilities both in laboratory and field settings. 24–27 Data from the Actigraph can be analyzed in various ways (i.e. activity counts, bouts, steps, intensity categories) but the default output is activity counts. Activity count data provides a number that accounts for the intensity (magnitude) as well as frequency of vertical displacement added over a specific recording time (epoch). Activity counts were collected over one minute epochs. According to the manufacturer, one count per minute is equal to 4 milli G’s of gravitational force per second. The actigraph manufacturer provides the following activity count and MET values based on Dr. Patricia Freedson’s work in 1998 investigating oxygen consumption and Actigraph activity count data in young adult men and women during various speeds of treadmill walking:
Light activity: ≤1952 CPM (< 3 METS)
Moderate activity: 1953 to 5724 CPM (3.0–6.0 METS)
Strenuous activity: 5725 to 9498 CPM (6.0–9.0 METS)
Very Strenuous activity: > 9498 CPM (>9 METS)
The participants were provided with verbal and written instructions for wear of the Actigraph accelerometer and a journal to keep track of the time their physical and occupational therapy sessions occurred. They also recorded when they donned and doffed the accelerometer (A copy of Actigraph information sheet and journal is available upon request). The participants were instructed to place the monitor on the waist band of their pants over their non-fractured hip using a belt clip or an elastic belt dependent upon the participants’ preference. This placement was chosen to best detect vertical accelerations of the trunk. The participants were asked to place the Actigraph on in the morning upon awakening and to remove the monitor when they were ready to sleep in the evening for 5 consecutive days during their rehabilitation stay. Therefore the monitor was worn for 5 days during waking hours including therapy session as well as outside of therapy times. Five days of monitoring has been shown to produce reliable estimates of habitual daily activity.28–30 Since the Actigraph was not waterproof, the monitor was also to be removed when the participant bathed or showered. The participants were masked to their Actigraph output since no visual display of activity counts was present on the accelerometer. The accelerometer was recovered by the study coordinator after the 5 day wear period. Activity counts per minute during rehab were averaged over the 5 day wear time period for each participant (average activity counts per minute).
Participation
Participant participation was ranked using the Pittsburgh Participation Rating Scale (PRPS), a clinician rated measure that quantifies a patient’s participation during their inpatient therapy.11 The PRPS is a 6-point Likert-type measure with higher scores indicating better participation (1= none, 2 = poor, 3= fair, 4 = good, 5 = very good and 6 = excellent). The PRPS relies on clinicians’ observation requiring no self report data from the participants. Previous work in over 200 patients with varying diagnoses in rehabilitation had found the PPRS to exhibit inter-rater reliability (ICC= .91–.96) and predictive validity against change in motor FIM scores. 11 It has been proposed that the PRPS may have particular utility in populations who are older, frail and in which outcomes are less universally favorable such as those with hip fracture or stroke. 11
The PRPS was introduced and explained to the physical and occupational therapists at the initiation of the study. The physical and occupational therapists were asked to rank the participants’ participation after each therapy session over the course of the 5 days the participant wore the accelerometer. The physical and occupational therapists who ranked the participation were masked to the Actigraph physical activity data results which were analyzed by the study coordinator.
Functional Outcomes
Functional outcomes were measured by the Hip Fracture Functional Recovery Scale (HFRS). 31,31,32 The HFRS is a self report measure designed to be administered in person or over the phone with 11 total questions and 3 main components; activities of daily living (bathing, dressing, feeding, toileting), instrumental activities of daily living (shopping, housework, laundry, food preparation, banking, public transportation) and mobility (walking). For each question the participant is asked “How much help do you need with the following activities?” with answer choices including cannot do, a large amount, a moderate amount, a minimal amount, none at all. Basic activities of daily living comprise 44% of the score, instrumental activities of daily living 23% and mobility 33%. Possible scores on the HFRS range from 0 to 100 with 100 indicating complete independence. The HFRS was found to have test-retest reliability, discriminate validity, predictive validity and responsiveness. 31,32 Zuckerman found the HFRS exhibited discriminate validity in that pre-fracture scores (asking the participant to rank their functional level before their fracture) were significantly different amongst participants based on their number of co-morbidities and operative risk. Also, the HFRS exhibited predictive validity since significant differences were found in comparing pre-fracture HFRS scores of those who died during the first year after fracture, were re-hospitalized or were admitted to a nursing home against those who returned to community dwelling. 32
The HFRS was administered during the participants’ rehabilitation stay by asking the participant to rank their functional abilities prior to their hip fracture (pre-fracture score). According to previous work by Zuckerman et al in 2000, scores can be utilized to determine pre fracture status retrospectively as well as to assess restoration of function. The participant was then called on the telephone at their residence at 3 and 6 months to administer the HFRS.
Data Analysis
All statistical analysis was performed by using version 15.0 SPSS software (SPSS Inc. Chicago IL). First, a Pearson’s correlation coefficient was used to assess the association of average participation scores for each participant over the 5 day wear period and average activity counts per minute during therapy sessions. A median split of baseline average activity counts per minute during therapy sessions was then calculated to classify participants into more active and less active groups. Next using independent samples T tests, average participation scores were compared for the more and less active groups. A 2 by 2 mixed analysis of variance was then performed on average HFRS scores as a function of activity level during therapy sessions (more and less active) and time following hip fracture (3 months and 6 months). Finally, mean functional recovery at 3 and 6 months after fracture was quantified by the “percent functional recovery”. This was defined as the percentage of pre-fracture HFRS score which was regained. For instance, a participant would have 100% functional recovery if at 6 months their HFRS score equaled their pre-fracture score. A 2 by 2 mixed ANOVA was performed on percent functional recovery as a function of activity level during therapy sessions (more and less active) and time following fracture (3 months and 6 months). A p value of ≤ 0.05 (2 tailed) was considered a significant effect on PRPS scores and HFRS scores.
RESULTS
The participants in this study (n= 18) had a mean physical activity output of 53.6 (median 36.8) counts per minute during therapy sessions and wore the Actigraph accelerometer during therapy sessions for an average of 142 (34.7) minutes per day. The two participants who were in skilled nursing rehabilitation did not differ in mean participation scores, median physical activity during therapy sesssions, or baseline HFRS scores compared to the 16 participants in inpatient rehabilitation. However on average, participants in skilled nursing rehabilitation spent less time in therapy per day and were older than those in inpatient rehabilitation. (Refer to Table 1 for further details).
Table 1.
Demographic Characteristics of the Study Participants by Type of Rehabilitation Facility (N=18)
| Characteristic | IRFs (n=16) | SNFs (n=2) |
|---|---|---|
| Age in years (mean) | 78.0 | 86.0 |
| Minutes in therapy (mean) | 150.0 | 75.5 |
| Activity counts per minute (median) | 36.8 | 48.2 |
| PRPS scores (mean) | 5.0 | 5.2 |
| Baseline HFRS (mean) | 95.6 | 93.5 |
Abbreviations: HFRS, Hip Fracture Functional Recovery Scale; PRPS, Pittsburgh Participation Rating Scale.
Participation and Physical Activity
Participation data was ranked by the physical or occupational therapist on 15 of the 18 participants (mean age 79.1 (8.3) years; 73% female and 86% in inpatient rehabilitation). The PRPS was not completed by the physical or occupational therapists in 3 of 18 participants accounting for the missing data. The therapists ranked the participants as having fair (3.0) to excellent (6.0) participation (average PRPS score = 5.0; median 5.3) over the 5 day time period in which the participant wore the Actigraph monitor. Daily participant participation scores were positively associated with average activity counts per minute during therapy sessions (Pearson’s r = 0.30, p = 0.045) indicating that 9% of the variability in participation scores could be explained by physical activity. Participants who were more active (n = 7) during therapy sessions on average were ranked by their occupational and physical therapists as having excellent participation compared to those who were less active (n = 8) being ranked as good participators (PRPS mean (SD) = 5.5 (0.4) and 4.4 (1.2) respectively; t = −2.51, p = 0.048).
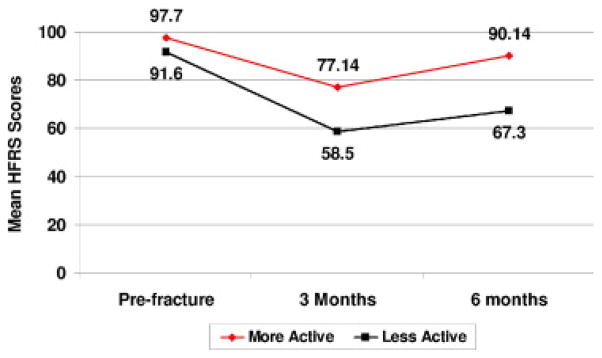
Functional Outcomes and Physical Activity
Complete HFRS data was obtained on 15 of the 18 participants (mean age 79.8 (9.2) years; 73.3% female and 87% in acute rehabilitation). Of the 17% (3 of 18) of participants who did not have HFRS data at 3 or 6 months, one had died and two were unavailable for follow-up (phone lines were disconnected and alternate numbers were not provided). The participants with missing data on HFRS at 3 and 6 months were similar in participation rankings (4.69 versus 4.96) and physical activity during rehab (32.9 versus 34.8 median activity counts per minute). For the 2 by 2 mixed ANOVA, assumptions of normality (Shapiro Wilk statistic 0.78 to 0.87 p = 0.09 to 0.19) and homogeneity of covariance were met (Box’s M = 11.836, p=0.02). Participants who were more active (n = 7) during therapy sessions reported better mean functional abilities on the HFRS scale at both 3 month [77.14 (17.0) versus 58.5 (29.0)] and 6 month time points [90.14 (11.1) versus 67.3 (36.4); F = 3.21, p = 0.09] compared to those who were less active (Figure 1). No interaction was found for HFRS scores between time points following fracture and activity groups. Mean pre fracture HFRS scores were not significantly different for the more and less active groups [97.7 (6.0) and 91.6 (10.2) respectively; t= −1.378, p = 0.19]. Participants who were more active during therapy sessions achieved 78% and 91% recovery of self reported pre-fracture function at 3 and 6 months compared to those who were less active achieving 64% and 73% recovery at 3 and 6 months respectively (F = 1.48, p= 0.24).
Fig. 1.
Mean Hip Fracture Functional Recovery Scores (HFRS) at baseline, 3 months, and 6 months for activity groups (n=15).
DISCUSSION
Therapist-rated patient participation was associated with objective measures of physical activity, which in turn added insight into future functional outcomes. This supports that actigraphy provides an objective measure of physical activity exhibiting concurrent validity against patient participation and predictive validity for future functional outcomes after hip fracture.
A significant loss in independent function during the first three months after hip fracture was found in this study and has been supported in previous work. 7,32,33 However in our study, greater functional recovery was achieved at both 3 and 6 months by those participants who were more active during their therapy sessions. This poses the question “How can we maximize our patients’ physical activity during their therapy sessions to potentially impact their future function?” Further examination of factors that contribute to physical activity of patients in rehabilitation after hip fracture is necessary and includes pain level, motivation, past medical history, or previous physical activity level. Also, does a therapists’ schedule and number of patients per hour have an impact on how much physical activity a patient receives? As mentioned in the methods section, previous work by Actigraph, LLC, Fort Walton Beach, FL and Freedson P et al in 1998 established activity level guidelines based on activity counts per one minute epochs in which light activity is considered less than or equal to 1952 counts (less than 2.99 METS).24 In our study, 18 participants had average activity counts collected in one minute epochs ranging from 18.3 to 129.5 indicating their substantial level of inactivity even during their therapy sessions. Since the Actigraph accelerometer was worn on the waist, it would not detect physical activity including upper extremity exercises or the increased effort taken to push or pull objects and walk on uneven terrains and inclines which may be typical activities performed during therapy sessions.
This study had several strengths. The longitudinal nature of our study allowed for the temporal association of physical activity and future functional outcomes to be explored. We were able to use accelerometers to measure physical activity during waking hours over a 5 day period for reliable estimates of habitual daily physical activity. Accelerometers to date have most often been used to measure physical activity in general healthy population and research that has been performed in patient populations thus far has mostly investigated the reliability and validity of accelerometers against measures of energy expenditure and other accelerometers. Measuring physical activity using accelerometers was feasible in this patient population. None of the accelerometers provided to the participants were lost or broken. Additionally, the PRPS which has been previously validated, was simple to use in both rehabilitation settings, did not produce any participant burden and required minimal training by therapists supporting its use in clinical and research settings.11
When interpreting the results of this study, several limitations should be considered. First, we did not account for potential factors that could have confounded the relation between physical activity, participation and functional outcomes. For instance, we did not record any surgical or medical complications or diagnostic tests which may have affected activity. We also did not collect data on factors such as body mass index or number of co-morbidities which also could affect activity levels. Second, 3 of the 18 participants (17%) did not complete their Actigraph journal during their 5 day wear period. In these cases, the physical and occupational therapists’ daily schedules were used to obtain PT and OT times. Also, since the number of participants in skilled nursing facilities was limited (2/18) it was impossible to draw a comparison between participants in inpatient rehabilitation facilities versus those in skilled nursing rehabilitation facilities. Finally, this study most likely suffered from a Type II error since the p values were slightly higher than 0.05 but the values appeared to be clinically meaningful. Considering grouping based on activity level (more or less active groups), a post hoc power calculation based on the mean and standard deviation of PRPS scores indicated that collecting data on 30 people (15 in each group) would have provided 89% power to find a difference with an alpha level of 0.05 in a two tailed test. With a power calculation based on the mean and standard deviation of the HFRS scores at 6 months, collecting data on 50 people total would have provided 84% power to find a difference.
Future directions would include repeating this study to increase the number of participants especially from the skilled nursing rehabilitation facilities to compare actigraphy in settings that offer different amounts of therapy per day. Additionally, establishing mean Actigraph activity count and functional levels in a large sample of older adults following hip fracture in rehabilitation would assist in providing further meaning to the count values. It would also be beneficial to assess actigraphy measures of physical activity with an objective measure of physical function in addition to self reported function at both 3 and 6 months following fracture.
Conclusion
Therapist-rated patient participation was associated with objective measures of patient activity, which added insight into future functional outcomes in patients after hip fracture.
Acknowledgments
Source of Support: Pittsburgh Claude D. Pepper Older Americans Independence Center P30 AG024827, Promotion of Doctoral Studies Award I and II American Physical Therapy Association, The University of Pittsburgh Hip Fracture Study (Munin, MC) R21 HD043202-01 NIH/NICHHD
The authors would like to thank the participants who participated in this study. The primary author Dr. Jaime Berlin Talkowski is supported by the University of Pittsburgh Department of Physical Therapy. Additional funding for Jaime Berlin Talkowski was provided by the Geriatric Section’s Adopt a Doc Scholarship from the American Physical Therapy Association. Dr. Jennifer Brach is supported by a National Institutes on Aging and American Federation of Aging Research Paul Beeson Career Development Award (K23 AG026766-01).
List of Abbreviations
- IR
inpatient rehabilitation
- SN
skilled nursing
- HFRS
hip fracture functional recovery scale
- PRPS
Pittsburgh Participation Rating Scale
Footnotes
Preliminary data from this manuscript was presented at Combined Sections Meeting of the American Physical Therapy Association in San Diego, CA in February 2006 and at the American Geriatric Society Meeting in Seattle, WA in May 2007.
Financial Disclosure: We certify that no party having a direct interest in the results of the research supporting this article has or will confer a benefit on us or on any organization with which we are associated AND, if applicable, we certify that all financial and material support for this research (eg, NIH or NHS grants) and work are clearly identified in the title page of the manuscript.
Contributor Information
Jaime B Talkowski, Email: jberlin@pitt.edu, Research Associate and Instructor, Department of Physical Therapy, University of Pittsburgh, 6035 Forbes Tower, Pittsburgh, PA 15260 (USA) 412-383-6645 (phone)/412-648-5970 (fax).
Eric J. Lenze, Associate Professor, Department of Psychiatry, Washington University School of Medicine, St. Louis MO.
Michael C. Munin, Associate Professor, Department of Physical Medicine and Rehabilitation, University of Pittsburgh School of Medicine, Pittsburgh PA.
Christopher C Harrison, Physical Therapist Rehabilitation Team Leader, UPMC Institute for Rehabilitation & Research Montefiore Hospital, Centers for Rehab Services, Pittsburgh PA.
Jennifer S Brach, Assistant Professor, Department of Physical Therapy, University of Pittsburgh, Pittsburgh PA.
Reference List
- 1.Barrett-Connor E. The economic and human costs of osteoporotic fracture. [Review] [63 refs] American Journal of Medicine. 1995;98(2A):3S–8S. doi: 10.1016/s0002-9343(05)80037-3. [DOI] [PubMed] [Google Scholar]
- 2.Lu-Yao GL, Baron JA, Barrett JA, Fisher ES. Treatment and survival among elderly Americans with hip fractures: a population-based study. American Journal of Public Health. 1994;84(8):1287–91. doi: 10.2105/ajph.84.8.1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Poor G, Atkinson EJ, O’Fallon WM, Melton LJ., III Determinants of reduced survival following hip fractures in men. Clinical Orthopaedics & Related Research. 1995;(319):260–5. [PubMed] [Google Scholar]
- 4.Stevens JA, Olson S. Reducing falls and resulting hip fractures among older women. Morbidity & Mortality Weekly Report Recommendations & Reports. 2000;49(RR-2):3–12. [PubMed] [Google Scholar]
- 5.Goldstein FC, Strasser DC, Woodard JL, Roberts VJ. Functional outcome of cognitively impaired hip fracture patients on a geriatric rehabilitation unit.[see comment] Journal of the American Geriatrics Society. 1997;45(1):35–42. doi: 10.1111/j.1532-5415.1997.tb00975.x. [DOI] [PubMed] [Google Scholar]
- 6.Behavioral Disorders in Dementia: Agitation, Aggression, and Psychosis. Bethesda, MD: 1998. [Google Scholar]
- 7.Munin MC, Seligman K, Dew MA, Quear T, Skidmore ER, Gruen G, et al. Effect of rehabilitation site on functional recovery after hip fracture.[see comment] Archives of Physical Medicine & Rehabilitation. 2005;86(3):367–72. doi: 10.1016/j.apmr.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 8.Maclean N, Pound P. A critical review of the concept of patient motivation in the literature on physical rehabilitation. [Review] [69 refs] Social Science & Medicine. 2000;50(4):495–506. doi: 10.1016/s0277-9536(99)00334-2. [DOI] [PubMed] [Google Scholar]
- 9.Maclean N, Pound P, Wolfe C, Rudd A. The concept of patient motivation: a qualitative analysis of stroke professionals’ attitudes. Stroke. 2002;33(2):444–8. doi: 10.1161/hs0202.102367. [DOI] [PubMed] [Google Scholar]
- 10.Lenze EJ, Munin MC, Quear T, Dew MA, Rogers JC, Begley AE, et al. Significance of poor patient participation in physical and occupational therapy for functional outcome and length of stay. Archives of Physical Medicine & Rehabilitation. 2004;85(10):1599–601. doi: 10.1016/j.apmr.2004.03.027. [DOI] [PubMed] [Google Scholar]
- 11.Lenze EJ, Munin MC, Quear T, Dew MA, Rogers JC, Begley AE, et al. The Pittsburgh Rehabilitation Participation Scale: reliability and validity of a clinician-rated measure of participation in acute rehabilitation. Archives of Physical Medicine & Rehabilitation. 2004;85(3):380–4. doi: 10.1016/j.apmr.2003.06.001. [DOI] [PubMed] [Google Scholar]
- 12.Jette DU, Warren RL, Wirtalla C. Rehabilitation in skilled nursing facilities: effect of nursing staff level and therapy intensity on outcomes. American Journal of Physical Medicine & Rehabilitation. 2004;83(9):704–12. doi: 10.1097/01.phm.0000137312.06545.d0. [DOI] [PubMed] [Google Scholar]
- 13.Jones GR, Jakobi JM, Taylor AW, Petrella RJ, Vandervoort AA. Community exercise program for older adults recovering from hip fracture: a pilot study. Journal of Aging & Physical Activity. 2006;14(4):439–55. doi: 10.1123/japa.14.4.439. [DOI] [PubMed] [Google Scholar]
- 14.Wainwright SA, Marshall LM, Ensrud KE, Cauley JA, Black DM, Hillier TA, et al. Hip fracture in women without osteoporosis. Journal of Clinical Endocrinology & Metabolism. 2005;90(5):2787–93. doi: 10.1210/jc.2004-1568. [DOI] [PubMed] [Google Scholar]
- 15.Mussolino ME. Depression and hip fracture risk: the NHANES I epidemiologic follow-up study.[see comment] Public Health Reports. 2005 Feb;120(1):71–5. doi: 10.1177/003335490512000112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stel VS, Pluijm SM, Deeg DJ, Smit JH, Bouter LM, Lips P. Functional limitations and poor physical performance as independent risk factors for self-reported fractures in older persons. Osteoporosis International. 2004;15(9):742–50. doi: 10.1007/s00198-004-1604-7. [DOI] [PubMed] [Google Scholar]
- 17.Ward DS, Evenson KR, Vaughn A, Rodgers AB, Troiano RP. Accelerometer use in physical activity: best practices and research recommendations. Medicine & Science in Sports & Exercise. 2005;37(11 Suppl):S582–8. doi: 10.1249/01.mss.0000185292.71933.91. [DOI] [PubMed] [Google Scholar]
- 18.Welk G, Blair S, Wood K, Jones S, Thompson R. A comparitive evaluation of three accelerometry-based physical activity monitors. Med Sci Sports Exerc. 2000;32:S489–S498. doi: 10.1097/00005768-200009001-00008. [DOI] [PubMed] [Google Scholar]
- 19.Taylor CB, Coffey T, Berra K, Iaffaldano R, Casey K, Haskell WL. Seven-day activity and self report compared to direct measure of physical activity. Am J epidemiol. 1984;120:818–824. doi: 10.1093/oxfordjournals.aje.a113954. [DOI] [PubMed] [Google Scholar]
- 20.Kriska AM, Knowler W, Laporte R. Development of a questionnaire to examine the relationship of physical activity and diabetes in Pima Indians. Diabetes Care. 1990;13:401–411. doi: 10.2337/diacare.13.4.401. [DOI] [PubMed] [Google Scholar]
- 21.Laporte R, Montoye H, Casperson C. Assessment of physical activity in epidemiologic research: problems and prospects. Public Health Reports. 1985;100(2):131–146. [PMC free article] [PubMed] [Google Scholar]
- 22.Freedson PS, Miller K. Objective monitoring of physical activity using motion sensors and heart rate. Research Quarterly for Exercise & Sport. 2000;71(2):21–29. doi: 10.1080/02701367.2000.11082782. [DOI] [PubMed] [Google Scholar]
- 23.Welk GJ, Differding JA, Thompson RW. The utility of the digi-walker step counter to assess daily activity patterns. Med Sci Sports Exerc. 2000;32(9):S481–8. doi: 10.1097/00005768-200009001-00007. [DOI] [PubMed] [Google Scholar]
- 24.Freedson P, Melanson E, Sirard J. Calibration of the Computer Science and Applications, inc. accelerometer. MSSE. 1998;30:777–781. doi: 10.1097/00005768-199805000-00021. [DOI] [PubMed] [Google Scholar]
- 25.Janz K. Validation of the CSA accelerometer for assessing children’s physical activity. Med Sci Sports Exerc. 1994;26:369–375. [PubMed] [Google Scholar]
- 26.Melanson E, Freedson P. Validity of the Computer Science and Applications Inc. (CSA) activity motor. Med Sci Sports Exerc. 1995;27:934–940. [PubMed] [Google Scholar]
- 27.Metcalf B, Curnow J, Evans C, Voss L, Wilkin T. Technical reliability of the CSA activity monitor: the Early Bird study. Med Sci Sports Exerc. 2002;34:1533–1537. doi: 10.1097/00005768-200209000-00022. [DOI] [PubMed] [Google Scholar]
- 28.Matthews CE. Use of self-report instruments to assess physical activity. In: Welk GJ, editor. Physical activity assessments for health-related research. Champaign, IL: Human Kinetics; 2002. pp. 107–123. [Google Scholar]
- 29.Pols MA, Peeters PH, Kemper HC, Grobbee DE. Methodological aspects of physical activity assessment in epidemiological studies. European Journal of Epidemiology. 1998;14(1):63–70. doi: 10.1023/a:1007427831179. [DOI] [PubMed] [Google Scholar]
- 30.Levin S, Jacobs D, Ainsworth Richardson M, Leon A. Intra-individual variation and estimates of usual physical activity. Ann Epidemiol. 1999;9:481–488. doi: 10.1016/s1047-2797(99)00022-8. [DOI] [PubMed] [Google Scholar]
- 31.Zuckerman JD, Koval KJ, Aharonoff GB, Hiebert R, Skovron ML. A functional recovery score for elderly hip fracture patients: I. Development. Journal of Orthopaedic Trauma. 2000;14(1):20–5. doi: 10.1097/00005131-200001000-00005. [DOI] [PubMed] [Google Scholar]
- 32.Zuckerman JD, Koval KJ, Aharonoff GB, Skovron ML. A functional recovery score for elderly hip fracture patients: II. Validity and reliability. Journal of Orthopaedic Trauma. 2000;14(1):26–30. doi: 10.1097/00005131-200001000-00006. [DOI] [PubMed] [Google Scholar]
- 33.Mossey JM, Mutran E, Knott K, Craik R. Determinants of recovery 12 months after hip fracture: the importance of psychosocial factors. American Journal of Public Health. 1989;79(3):279–86. doi: 10.2105/ajph.79.3.279. [DOI] [PMC free article] [PubMed] [Google Scholar]