Abstract
Objective:
Suicide is a significant public health issue, and is especially concerning in adolescents and young adults, who are over-represented both in attempts and completed suicide. Emerging technologies represent a promising new approach to deliver suicide prevention interventions to these populations. The current systematic review aims to identify online and mobile psychosocial suicide prevention interventions for young people, and evaluate the effectiveness of these interventions.
Method:
PsycINFO, Medline, Embase and The Cochrane Library were electronically searched for all articles published between January, 2000 and May, 2015. Peer-reviewed journal articles reporting on interventions for young people aged 12–25 years with suicidality as a primary outcome were eligible for inclusion. No exclusions were placed on study design.
Results:
One study met inclusion criteria, and found significant reductions in the primary outcome of suicidal ideation, as well as depression and hopelessness. Two relevant protocol papers of studies currently underway were also identified.
Conclusions:
There is a paucity of current evidence for online and mobile interventions for suicide prevention in youth. More high quality empirical evidence is required to determine the effectiveness of these novel approaches to improving suicide outcomes in young people.
Keywords: suicide prevention, web-based, internet, mobile, young people, adolescent
Résumé
Objectif:
Le suicide est un enjeu de santé publique significatif, et il est spécialement préoccupant chez les adolescents et les jeunes adultes, qui sont surreprésentés dans les tentatives de suicide et les suicides complétés. Les nouvelles technologies représentent une approche prometteuse pour la prestation d’interventions de prévention du suicide à ces populations. La présente revue systématique vise à identifier les interventions psychosociales en ligne et mobiles de prévention du suicide pour les jeunes, et à évaluer l’efficacité de ces interventions.
Méthode:
Les bases de données PsycINFO, Medline, Embase et The Cochrane Library ont fait l’objet d’une recherche électronique de tous les articles publiés entre janvier 2000 et mai 2015. Les articles de revues révisés par les pairs portant sur les interventions pour les jeunes de 12 à 25 ans dont le résultat principal était la suicidabilité étaient admissibles à l’inclusion. Aucune exclusion ne portait sur la méthode de l’étude.
Résultats:
Une étude satisfaisait aux critères d’inclusion, et constatait des réductions significatives du résultat principal d’idéation suicidaire, ainsi que de la dépression et du désespoir. Deux documents de protocole pertinents d’études en cours ont aussi été identifiés.
Conclusions:
Il y a une rareté de données probantes actuelles sur les interventions en ligne et mobiles de prévention du suicide pour les jeunes. Il faut plus de données probantes empiriques de grande qualité pour déterminer l’efficacité de ces nouvelles approches afin d’améliorer les résultats du suicide chez les jeunes.
Keywords: prévention du suicide, sur le Web, Internet, mobile, jeunes, adolescent
Introduction
Suicide is a serious public health concern and is the second leading cause of death in 15–29 year-olds globally (World Health Organization, 2014). Further, non-fatal suicidal behaviour and attempts are prevalent in youth. While lifetime prevalence of suicidal ideation is very low during childhood, it increases slowly during early adolescence and then exponentially between the ages of 12–17 years (Nock et al., 2013). Recent data from the 2013 Youth Risk Behavior Survey (YRBS), a national school-based survey of health-risk behaviours among young people, indicates that 17% of American youth in grades 9–12 seriously considered attempting suicide in the previous 12 months, with 13.6% making a plan to do so, and 8% actually making an attempt (Kann et al., 2014).
Although efforts are underway to develop effective youth-focused suicide prevention strategies and interventions, research to date has been limited and conclusions tempered by methodological problems. A review of randomised controlled trials examining suicide prevention interventions for young people aged 12–25 years found limited evidence to support the effect of any specific interventions on suicide-related behaviours, though the authors note that approaches using cognitive behavioural therapy have shown some preliminary positive effects (Robinson, Hetrick, & Martin, 2011). Limitations of reviewed studies include small sample sizes, inconsistent definitions of suicidality and the frequent exclusion of suicidal young people from trials due to safety concerns. While there is some evidence to suggest that therapeutic interventions such as Cognitive Behavioural Therapy (CBT) and Dialectical Behaviour Therapy (DBT) may have a positive impact on adolescent self-harm, neither pharmacological nor psychosocial interventions have been found to reduce the risk of suicide attempts, relative to treatment as usual (Ougrin, Tranah, Stahl, Moran, & Asarnow, 2015).
Two recent systematic reviews of school-based suicide prevention programs found improvements in suicide-related knowledge, attitudes and help-seeking, but limited evidence for reduced suicidal ideation and behaviour (Cusimano & Sameem, 2011; Katz et al., 2013). These reviews covered age ranges from 13–19 years and birth to 18 years, respectively. Amongst them, only two evidence-based interventions were found to impact upon suicide attempts. Signs of Suicide (SOS) is a prevention program that includes suicide awareness, education and screening components, and was found to reduce suicide attempts (but not ideation) relative to classes as usual (Aseltine & DeMartino, 2004; Aseltine, James, Schilling, & Glanovsky, 2007). The other evidence-based intervention, the Good Behavior Game (GBG) is a universal intervention designed to improve the classroom environment and reduce disruptive behaviours. Despite the fact that its primary purpose is not to reduce suicidality, there is evidence to support the program’s impact on both suicidal ideation and attempts (Wilcox et al., 2008). Notably, none of the aforementioned reviews reported on the impact of suicide prevention programs on suicide completion rates.
Taken together, there is some evidence for the effectiveness of existing suicide prevention programs on more distal measures of suicidality (e.g., attitudes), however, the ultimate impact of these programs in terms of saving lives is not yet known. This may be due, in part, to the relatively low base rates for suicide attempts and completion, making it difficult to assess the true impact of therapeutic interventions on these outcomes. There is preliminary evidence, however, to support the effectiveness of reducing suicidal behaviour in adults. Specifically, a recent review found that post-discharge follow up (e.g., in the form of contact letters or phone calls) to at-risk individuals was found to reduce both suicide attempts and completion in five of 11 included studies (Luxton, June, & Comtois, 2015). Whether this is also the case in youth is yet to be tested.
A key limitation of the suicide prevention literature in youth is that the large majority is focused on face-to-face interventions (delivered at a group, family, community or individual level). Recently, a new approach to suicide prevention has emerged in the context of the burgeoning fields of electronic and mobile healthcare practices (eHealth; mHealth). Indeed, current evidence suggests that electronic therapies can have a positive impact on symptoms of depression and anxiety in young people at risk of developing, or those already diagnosed with these disorders (Pennant et al., 2015). Due to the low-cost, convenient, and accessible nature of web-based and mobile applications, novel interventions utilising technology are increasingly being developed to target public and mental health difficulties. Yet, web-based applications and sites are not without their risks. The largely uncontrolled and unmoderated nature of the internet raises concerns about the kinds of information that vulnerable youth may be able to access, the way in which suicidal thoughts, feelings and behaviours may be communicated, and how others may respond. Indeed, the internet may be used for cyber-bullying, to normalise self-harm, encourage suicidal acts, or discourage help-seeking, (Alao, Soderberg, Pohl, & Alao, 2006; Daine et al., 2013). However, evidence suggests that is more commonly used for assistance and support (Daine et al., 2013).
Further, despite these potential risks, it is clear that the internet and mobile phones are increasingly being used to receive and share information, especially by young people. Indeed, 92% of teenagers report going online daily, with nearly one quarter endorsing that they are ‘almost constantly’ connected. This is partly due to the advent of Internet-enabled smartphones, which are owned or accessed by nearly three quarters of American adolescents (Lenhart et al., 2015). Additionally, young people have reported finding online and mobile interventions to be acceptable, discrete, low effort and enjoyable to use (Dennison, Morrison, Conway, & Yardley, 2013). Therefore, technology-based approaches to suicide prevention offer significant potential for engaging young people, increasing adherence and improving outcomes.
Two reviews of online suicide prevention strategies have been conducted recently (Christensen, Batterham, & O’Dea, 2014; Lai, Maniam, Chan, & Ravindran, 2014). Both indicate that there are potential benefits of web-based strategies for suicide prevention that need to be explored; however, the preliminary nature of this evidence was noted by the authors. Lai et al. highlighted the overall poor quality of the literature, with the majority of included studies being rated as low to medium quality. Further, Christensen and colleagues reported that suicide prevention efforts to date have typically targeted mechanisms that are known to be associated with suicidality, such as depression. While this approach intuitively makes sense, it nonetheless ignores the fact that not all suicidal individuals experience depression, and underscores the need for interventions to explicitly target suicidal ideation and behaviour. To date, only one randomised controlled trial (RCT) reporting on the effects of a web-based program targeting suicidal thoughts has been published (van Spijker, van Straten, & Kerkhof, 2014). In an adult sample, the authors found that the program had a small effect (d = .28) on suicidal thoughts and hopelessness, relative to a waitlist control condition, indicating preliminary effectiveness of this novel approach to suicide prevention.
Only one review of technology-focused suicide prevention strategies for young people has been conducted to date. Specifically, a recent systematic review of web-based and mobile interventions for internalising problems in youth aged 5–25 years included ‘suicide’ as a search term (Reyes-Portillo et al., 2014), however, no web-based interventions for suicide prevention were identified. In addition, the search was only conducted up until December, 2013. Given the rapid advances in the fields of eHealth and mHealth, it is both appropriate and necessary to conduct an updated review of web-based and mobile suicide prevention strategies for young people. The current review will not only determine the current evidence base for online youth suicide prevention, but will also highlight gaps in the literature that will guide future research in this critically important field. This systematic review aims to evaluate available literature describing online and mobile psychosocial suicide prevention interventions for young people, and to determine the effectiveness of these interventions in reducing suicidal ideation, behaviour, attempts and completion.
Methods
Search Strategy
PsycINFO, Medline, Embase and The Cochrane Library were electronically searched for all articles published between January, 2000 and May, 2015. The following search terms were used to represent the constructs of: i) technology; ii) intervention; iii) youth; and, iv) suicide: (app* OR computer* OR cyber OR cyberspace OR electronic OR electronic mail OR email OR e-mail OR internet* OR net OR online OR virtual OR web* OR www OR e-health OR m-health OR mobile* OR smartphone OR text messag* OR SMS OR social media OR social network* OR blog OR forum OR Twitter OR Facebook OR Instagram) AND (screen* OR assess* OR interven* OR * prevent* or treat* OR track* OR support*) AND (adolescen* OR child* OR youth OR young person OR young adult OR young people OR emerging adult* OR teen*) AND (suicid*). A separate electronic search (using the same terms) was also conducted in the peer-reviewed journal Internet Interventions, as it is not currently listed in these databases. Additionally, reference lists from studies meeting inclusion criteria, as well as recent reviews in the field, were hand-searched.
Inclusion Criteria
Studies were included in the current review if: (a) the intervention tested explicitly targeted suicidality; (b) the primary outcome was suicidal ideation, attempts or completion; (c) the intervention was primarily (at least 75%) delivered through a mobile, computer or web-based application; (d) the mean age of participants ranged from 12 years, 0 months to 25 years, 0 months; and, (e) published in an English language peer-review journal. Studies examining interventions for non-suicidal self-injury were excluded from the review, as were those that explicitly targeted mechanisms related to suicidality (such as depression), unless suicidality was cited as the primary outcome. Interventions targeting adults involved in the care of young people (e.g. mental health clinicians or educators) were also excluded from the present review. No restrictions were placed on personnel involvement (e.g., guided vs. unguided online therapy), intervention length, session frequency, or concurrent treatment (e.g., other psychosocial therapy or medication).
Data extraction
Data extraction for studies meeting inclusion criteria (and associated study protocols) was performed by one of the study authors (YP – initials removed to facilitate blind review). Data outlining the study design, aims, sample, nature of the intervention, involvement of personnel, outcome measures, key findings, limitations and conclusions were extracted. Given the limited number of relevant articles, this information is presented narratively.
Results
Search results
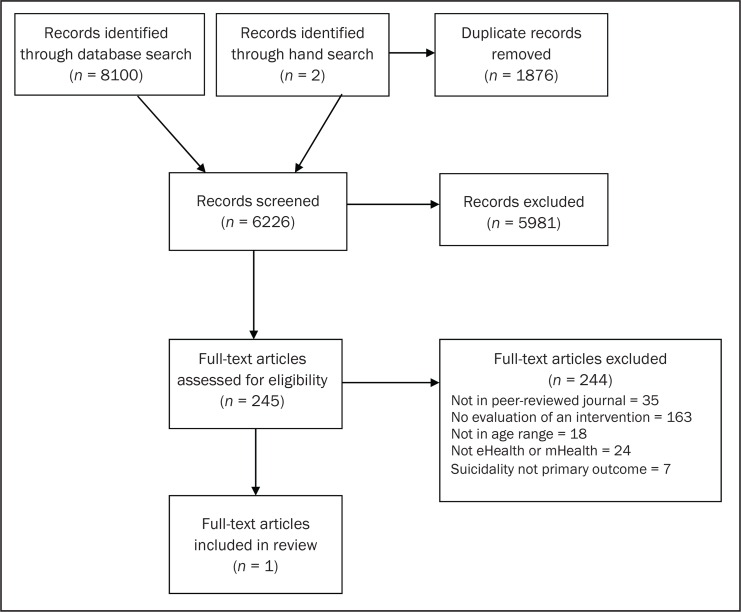
Search results are presented in the PRISMA Flow Diagram in Figure 1.
Figure 1.
PRISMA Flow Diagram
The initial search produced 8100 records, with an additional two records obtained through hand searching recent reviews. No relevant articles were found in the Internet Interventions journal. Duplicate articles (n = 1876) were removed and the remaining titles and abstracts (n = 6226) were screened by YP (initials removed to facilitate blind review) to determine their relevance to this review. Completely irrelevant articles were excluded at this stage, and potentially relevant studies (n = 245) were retained and the full-text article obtained for full review by two independent coders (YP, AWS - initials removed to facilitate blind review). Any discrepancies were resolved in consultation with a third author (AC - initials removed to facilitate blind review). Only one full-text article met inclusion criteria for this review and was retained for data extraction. Two additional study protocols that do not meet inclusion criteria are also described below, as it was deemed appropriate to provide insight into the most up to date ongoing research in the field. Once completed, these studies would meet the current inclusion criteria.
Studies meeting inclusion criteria
The only article that met the inclusion criteria reported on a recent pilot study examining the effects of an online intervention for suicidal ideation in secondary school students (Robinson, Hetrick, Cox, Bendall, Yuen, et al., 2014). Students aged 14–18 years who presented to a member of the school wellbeing team reporting suicidal ideation in the previous month were invited to take part in an eight week trial of the Reframe-IT intervention. This intervention included traditional components of CBT such as cognitive restructuring and behavioural activation, with a specific focus on problem solving around suicidal ideation. The content was delivered via an adult ‘host’ character who verbally delivered the therapy, as well as factsheets and MP3s. Additional features of the program included video diaries of young people (actors) telling their story, activities to complete, a message board (without social networking functionality), as well as a personalised safety plan which was completed and uploaded to the site following the baseline assessment. The intervention was delivered online on a weekly basis within the school setting and facilitated by the researchers, with additional support provided by a researcher-clinician, who provided standardised responses to activities, responses to the message board and managed risk in response to regular distress checks. After completing each module in school, the student was granted access to that module in their own time via a secure login.
Thirty-two adolescents completed the baseline assessment, however only 21 finished the intervention and the post-intervention assessment; this latter group served as the observed case sample. Statistically significant reductions in the primary outcome of suicidal ideation, as well as secondary outcomes of depression and hopelessness, were observed. Moderate effect sizes for suicidal ideation (ηp2 = 0.66) and clinician-rated depression (ηp2 = 0.60), and small effect sizes for self-reported depression (ηp2 = 0.48) and hopelessness (ηp2 = 0.46) were reported. The authors note that these findings were tempered by some significant limitations, including the lack of intent-to-treat analyses, small sample size and high attrition rate. Further, given that this study did not include a control group, it is not possible to determine whether the effects of the intervention were genuine, or simply due to the passage of time. Nevertheless, given that this pilot study represents the first investigation into the effectiveness of online suicide prevention interventions in young people, the findings are promising and at the very least warrant further research.1
Study protocols for ongoing trials
Subsequent to conducting the pilot study described above, Robinson and colleagues published a study protocol for a full-scale randomised controlled trial (RCT) of the Reframe-IT intervention (Robinson, Hetrick, Cox, Bendall, Yung, Yuen, et al., 2014). This trial aims to recruit N = 170 participants from up to 28 schools over a two year period in order to compare the effectiveness of Reframe-IT with treatment as usual, which will be monitored via a questionnaire. Key differences between the RCT and the initial pilot study include a longer, ten week intervention phase, the inclusion of a 12 week follow-up assessment and the use of school wellbeing staff (rather than researchers) to administer intervention modules and manage risk in response to distress checks. Additional outcome measures for this trial include suicidal acts (not only ideation) and anxiety (in students), as well as attitudes, confidence, perceived skill, and changes in practice for school staff.
Another recently published study protocol that warrants mention reports on a planned trial to examine the effectiveness of a self-help, tablet-based suicide prevention app for indigenous Australian youth (Shand, Ridani, Tighe, & Christensen, 2013). The aims of this RCT are to:
determine the impact of the app in reducing suicidal thoughts, distress and impulsivity;
evaluate the acceptability of the app to Indigenous youth;
assess the feasibility of the methodology within this especially vulnerable population;
examine the uptake and adherence to the intervention; and,
evaluate safety and support protocols.
A sample of N = 150 Indigenous Australians aged 18–30 years who have experienced suicidal thoughts in the previous two weeks will be recruited to participate in the trial and randomly allocated to the iBobbly intervention or a waitlist control group. Severely suicidal and psychotic individuals will be excluded. iBobbly is a self-paced program based on principles of Acceptance and Commitment Therapy and Mindfulness Based Cognitive Therapy. It consists of three modules, which are completed sequentially over six weeks, targeting: i) identification of and diffusion from thoughts; ii) emotion regulation through mindfulness, acceptance, self-soothing; and, iii) identifying values and setting goals. All text is accompanied by audio to accommodate participants with low literacy. While the app is unguided, all participants will be supported by 24 hour telephone crisis lines and contacted by researchers half way through the intervention phase for a brief risk assessment. Assessment of the following outcomes will be conducted at baseline, post-intervention and six weeks; frequency and intensity of suicidal thoughts (primary outcome), depression, psychological distress and impulsivity.
A pilot RCT examining the effects of iBobbly versus wait-list control in N = 61 participants is now complete, and a full scale RCT is underway.
Discussion
The current review highlights the dearth of online and mobile interventions designed specifically to reduce suicidality in young people. Only one published pilot study, conducted by researchers at Orygen in Melbourne, Australia, was found to meet inclusion criteria, with promising results reported. Of note, a randomised controlled trial of the same intervention is currently underway. Another tablet-based app targeting suicidal ideation in Indigenous youth is also currently being examined. This demonstrates that some progress has been made in the field since the last published review of online suicide prevention for youth (Reyes-Portillo et al., 2014). Based on these limited findings, it is still too early to determine the overall effectiveness of eHealth interventions for suicide prevention in young people, however, it is clear that Australian researchers are leading the way in this emerging and important field. Given the pervasive use of both the internet and mobile phones by adolescents and emerging adults (Australian Communications and Media Authority, 2015; Lenhart et al., 2015), together with the finding that suicidal adolescents are often reluctant to seek help from traditional mental health services (Carlton & Deane, 2000; Deane, Wilson, & Ciarrochi, 2001), it is clear that further exploration of these novel, technology-based interventions is warranted. It is particularly important to note that there are currently no published studies on mobile phone-based interventions for youth suicide prevention, suggesting an important gap in the literature that requires investigation.
One reason for the lack of empirical research in this field may be due to the practical and ethical difficulties associated with conducting research with suicidal individuals, and in particular, with the especially vulnerable group of adolescents. Indeed, as noted by Reyes-Portillo and colleagues, suicidality is frequently cited as an exclusion criterion, even in studies that explicitly target young people with severe depression. Regrettably, this limits the ability of youth with significant distress to access treatments that may be effective for them. Further, by eschewing intervention research in youth suicide prevention, it is difficult to determine what is and is not effective in reducing risk for these individuals. Nonetheless, the fact that three new web-based intervention studies targeting suicidality in young people have emerged in the past 18 months offers hope that researchers (and ethics committees) are beginning to recognise the value of empirically exploring the potential of this novel approach.
Despite the lack of intervention research in this field, a number of other web-based approaches to youth suicide prevention are emerging. Screening and assessment of risk in young people in primary care (e.g., Chisolm, Klima, Gardner, & Kelleher, 2009; Diamond et al., 2010), hospital (e.g., Fein et al., 2010; Pailler & Fein, 2009), school (e.g., Hallfors et al., 2006) and college (e.g., Haas et al., 2008) settings appears to be increasingly moving online. The potential benefits of this approach in clinical settings include automation and standardisation of the screening process to reduce costs and improve fidelity, as well the potential to design screening programs that allow providers to not only receive individual results, but meaningful summaries and interpretations of client risk. In schools, widespread screening through online technology may be conducted privately and efficiently, allowing for potential identification of at-risk youth who might otherwise be unlikely to come into contact with mental health services.
Another suicide prevention strategy that has typically been conducted in face-to-face contexts but may be moving into the online space is gatekeeper training. A recently published article describes the protocol for an RCT examining the effects of a series of e-learning modules for school-based and clinical mental health professionals on perceived and actual knowledge regarding adolescent suicidality, as well as perceived self-confidence when interacting with suicidal youth (Ghoncheh, Kerkhof, & Koot, 2014). The authors suggest the potential benefits of this online approach include allowing gatekeepers to learn at their own pace and from any given location, and to flexibly customise their own training whilst still learning the key steps involved in adolescent suicide prevention. Although this intervention does not target youth as its participants, it highlights the possibility of translating youth-focused gatekeeper programs into a similar format.
Finally, peer approaches to suicide prevention in young people also represent an area of tremendous potential. In particular, the use of social media to identify individuals at risk is receiving increasing attention in the literature (see Robinson et al., 2015 for a comprehensive review). Although the field is still in its infancy, the extraordinary reach of social media platforms, and potential for individuals to anonymously share experiences and support those who express suicidality suggest that there is significant opportunity to exploit the power of social media to reduce suicidality. This potential may be even greater in young people, who habitually utilise these platforms to communicate.
The lack of relevant literature to review is a key limitation of the current paper, which constrains our ability to draw firm conclusions regarding the value of technology-based suicide prevention interventions in young people. However, this limitation simultaneously highlights the importance of continued work in this field. Further, this review illustrates that we are on the cusp of an exciting era in which a range of innovative approaches to this significant problem will be explored, as evidenced by studies that are already underway (Robinson, Hetrick, Cox, Bendall, Yung, Yuen, et al., 2014; Shand et al., 2013). Given the magnitude and impact of youth suicide on our communities, and the potential advantages associated with online and mobile strategies to address this issue, it is imperative that the need for high quality, empirical research in this field is both recognised and prioritised.
Acknowledgements / Conflicts of Interest
HC is supported by NHMRC John Cade Fellowship 1056964. ALC is supported by NHMRC Early Career Fellowship 1013199. The authors have no other financial relationships to disclose.
Footnotes
In addition to the key outcomes, two related study which did not meet inclusion criteria reported on secondary outcomes from this pilot study. Participants reported enjoying completing the intervention and that they would recommend it to a friend (Robinson, Hetrick, Cox, Bendall, Yung, & Pirkis, 2014). Further, Reframe-IT was also found to improve skill deficits including negative problem-solving orientation and reduce emotion-focused coping (Hetrick et al., 2014), both of which have been observed in adolescents with suicidal ideation.
References
- Alao AO, Soderberg M, Pohl EL, Alao AL. Cybersuicide: Review of the role of the internet on suicide. CyberPsychology & Behavior. 2006;9(4):489–493. doi: 10.1089/cpb.2006.9.489. [DOI] [PubMed] [Google Scholar]
- Aseltine RH, Jr, DeMartino R. An outcome evaluation of the SOS Suicide Prevention Program. American Journal of Public Health. 2004;94(3):446–451. doi: 10.2105/ajph.94.3.446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aseltine RH, Jr, James A, Schilling EA, Glanovsky J. Evaluating the SOS suicide prevention program: A replication and extension. BMC Public Health. 2007;7:161. doi: 10.1186/1471-2458-7-161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Australian Communications and Media Authority 2015. Aussie Teens Online Retrieved 20 May, 2015, from http://www.acma.gov.au/theACMA/engage-blogs/engage-blogs/Research-snapshots/Aussie-teens-online.
- Carlton PA, Deane FP. Impact of attitudes and suicidal ideation on adolescents’ intentions to seek professional psychological help. Journal of Adolescence. 2000;23(1):35–45. doi: 10.1006/jado.1999.0299. [DOI] [PubMed] [Google Scholar]
- Chisolm DJ, Klima J, Gardner W, Kelleher KJ. Adolescent behavioral risk screening and use of health services. Administration & Policy in Mental Health. 2009;36(6):374–380. doi: 10.1007/s10488-009-0245-8. [DOI] [PubMed] [Google Scholar]
- Christensen H, Batterham PJ, O’Dea B. E-health interventions for suicide prevention. International Journal of Environmental Research and Public Health. 2014;11(8):8193–8212. doi: 10.3390/ijerph110808193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cusimano MD, Sameem M. The effectiveness of middle and high school-based suicide prevention programmes for adolescents: a systematic review. Injury Prevention. 2011;17(1):43–49. doi: 10.1136/ip.2009.025502. [DOI] [PubMed] [Google Scholar]
- Daine K, Hawton K, Singaravelu V, Stewart A, Simkin S, Montgomery P. The power of the web: A systematic review of studies of the influence of the internet on self-harm and suicide in young people. PLoS ONE. 2013;8(10):e77555. doi: 10.1371/journal.pone.0077555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deane FP, Wilson CJ, Ciarrochi J. Suicidal ideation and help-negation: Not just hopelessness or prior help. Journal of Clinical Psychology. 2001;57(7):901–914. doi: 10.1002/jclp.1058. [DOI] [PubMed] [Google Scholar]
- Dennison L, Morrison L, Conway G, Yardley L. Opportunities and challenges for smartphone applications in supporting health behavior change: Qualitative study. Journal of Medical Internet Research. 2013;15(4) doi: 10.2196/jmir.2583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diamond G, Levy S, Bevans KB, Fein JA, Wintersteen MB, Tien A, Creed T. Development, validation, and utility of internet-based, behavioral health screen for adolescents. Pediatrics. 2010;126(1):e163–170. doi: 10.1542/peds.2009-3272. [DOI] [PubMed] [Google Scholar]
- Fein JA, Pailler ME, Barg FK, Wintersteen MB, Hayes K, Tien AY, Diamond GS. Feasibility and effects of a web-based adolescent psychiatric assessment administered by clinical staff in the pediatric emergency department. Archives of Pediatrics & Adolescent Medicine. 2010;164(12):1112–1117. doi: 10.1001/archpediatrics.2010.213. [DOI] [PubMed] [Google Scholar]
- Ghoncheh R, Kerkhof AJ, Koot HM. Effectiveness of adolescent suicide prevention e-learning modules that aim to improve knowledge and self-confidence of gatekeepers: Study protocol for a randomized controlled trial. Trials [Electronic Resource] 2014;15:52. doi: 10.1186/1745-6215-15-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haas A, Koestner B, Rosenberg J, Moore D, Garlow SJ, Sedway J, Nemeroff CB. An interactive web-based method of outreach to college students at risk for suicide. Journal of American College Health. 2008;57(1):15–22. doi: 10.3200/JACH.57.1.15-22. [DOI] [PubMed] [Google Scholar]
- Hallfors D, Brodish PH, Khatapoush S, Sanchez V, Cho H, Sleekier A. Feasibility of screening adolescents for suicide risk in “real-world” high school settings. American Journal of Public Health. 2006;96(2):282–287. doi: 10.2105/AJPH.2004.057281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hetrick S, Yuen HP, Cox G, Bendall S, Yung A, Pirkis J, Robinson J. Does cognitive behavioural therapy have a role in improving problem solving and coping in adolescents with suicidal ideation? The Cognitive Behaviour Therapist. 2014;7 [Google Scholar]
- Kann L, Kinchen S, Shanklin SL, Flint KH, Kawkins J, Harris WA, Chyen D. Youth risk behavior surveillance - United States, 2013. MMWR Surveill Summ. 2014;63(Suppl 4):1–168. [PubMed] [Google Scholar]
- Katz C, Bolton SL, Katz LY, Isaak C, Tilston-Jones T, Sareen J. A systematic review of school-based suicide prevention programs. Depression and Anxiety. 2013;30(10):1030–1045. doi: 10.1002/da.22114. [DOI] [PubMed] [Google Scholar]
- Lai MH, Maniam T, Chan LF, Ravindran AV. Caught in the web: A review of web-based suicide prevention. Journal of Medical Internet Research. 2014;16(1):e30. doi: 10.2196/jmir.2973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenhart A, Duggan M, Perrin A, Stepler R, Rainie H, Parker K. Teens, Social Media & Technology Overview 2015 2015 [Google Scholar]
- Luxton DD, June JD, Comtois KA. Can postdischarge follow-up contacts prevent suicide and suicidal behavior? Crisis. 2015 doi: 10.1027/0227-5910/a000158. [DOI] [PubMed] [Google Scholar]
- Nock MK, Green JG, Hwang I, McLaughlin KA, Sampson NA, Zaslavsky AM, Kessler RC. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: Results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry. 2013;70(3):300–310. doi: 10.1001/2013.jamapsychiatry.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ougrin D, Tranah T, Stahl D, Moran P, Asarnow JR. Therapeutic interventions for suicide attempts and self-harm in adolescents: Systematic review and meta-analysis. Journal of the American Academy of Child & Adolescent Psychiatry. 2015;54(2):97–107. doi: 10.1016/j.jaac.2014.10.009. [DOI] [PubMed] [Google Scholar]
- Pailler ME, Fein JA. Computerized behavioral health screening in the emergency department. Pediatric Annals. 2009;38(3):156–160. doi: 10.3928/00904481-20090301-08. [DOI] [PubMed] [Google Scholar]
- Pennant ME, Loucas CE, Whittington C, Creswell C, Fonagy P, Fuggle P, Kendall T. Computerised therapies for anxiety and depression in children and young people: A systematic review and meta-analysis. Behaviour Research and Therapy. 2015;67:1–18. doi: 10.1016/j.brat.2015.01.009. [DOI] [PubMed] [Google Scholar]
- Reyes-Portillo JA, Mufson L, Greenhill LL, Gould MS, Fisher PW, Tarlow N, Rynn MA. Web-based interventions for youth internalizing problems: A systematic review. Journal of the American Academy of Child & Adolescent Psychiatry. 2014;53(12):1254–1270. e1255. doi: 10.1016/j.jaac.2014.09.005. [DOI] [PubMed] [Google Scholar]
- Robinson J, Cox G, Bailey E, Hetrick S, Rodrigues M, Fisher S, Herrman H. Social media and suicide prevention: A systematic review. Early Intervention in Psychiatry. 2015 Feb; doi: 10.1111/eip.12229. [DOI] [PubMed] [Google Scholar]
- Robinson J, Hetrick S, Cox G, Bendall S, Yuen HP, Yung A, Pirkis J. Can an Internet-based intervention reduce suicidal ideation, depression and hopelessness among secondary school students: Results from a pilot study. Early Intervention in Psychiatry. 2014 doi: 10.1111/eip.12137. [DOI] [PubMed] [Google Scholar]
- Robinson J, Hetrick S, Cox G, Bendall S, Yung A, Pirkis J. The safety and acceptability of delivering an online intervention to secondary students at risk of suicide: Findings from a pilot study. Early Intervention in Psychiatry. 2014 doi: 10.1111/eip.12136. [DOI] [PubMed] [Google Scholar]
- Robinson J, Hetrick S, Cox G, Bendall S, Yung A, Yuen HP, Pirkis J. The development of a randomised controlled trial testing the effects of an online intervention among school students at risk of suicide. BMC Psychiatry. 2014;14:155. doi: 10.1186/1471-244X-14-155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson J, Hetrick SE, Martin C. Preventing suicide in young people: Systematic review. Australian and New Zealand Journal of Psychiatry. 2011;45(1):3–26. doi: 10.3109/00048674.2010.511147. [DOI] [PubMed] [Google Scholar]
- Shand FL, Ridani R, Tighe J, Christensen H. The effectiveness of a suicide prevention app for indigenous Australian youths: Study protocol for a randomized controlled trial. Trials. 2013;14(1) doi: 10.1186/1745-6215-14-396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Spijker BA, van Straten A, Kerkhof AJ. Effectiveness of online self-help for suicidal thoughts: Results of a randomised controlled trial. PLoS ONE [Electronic Resource] 2014;9(2):e90118. doi: 10.1371/journal.pone.0090118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilcox HC, Kellam SG, Brown CH, Poduska JM, Ialongo NS, Wang W, Anthony JC. The impact of two universal randomized first-and second-grade classroom interventions on young adult suicide ideation and attempts. Drug and Alcohol Dependence. 2008;95:S60–S73. doi: 10.1016/j.drugalcdep.2008.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . Preventing suicide: A global imperative. World Health Organization; 2014. [Google Scholar]