Abstract
We conducted a challenge/rechallenge trial in which 3 alpacas were infected with Middle East respiratory syndrome coronavirus. The alpacas shed virus at challenge but were refractory to further shedding at rechallenge on day 21. The trial indicates that alpacas may be suitable models for infection and shedding dynamics of this virus.
Keywords: coronavirus, Middle East respiratory syndrome, MERS-CoV, severe acute respiratory syndrome, SARS, camel, alpaca, experimental animal model, infection, rechallenge, shedding, vaccine, viruses, zoonoses
Middle East respiratory syndrome coronavirus (MERS-CoV) was first reported in September 2012 (1); since then, >1,600 confirmed cases have been reported to the World Health Organization (http://www.who.int/csr/don/29-february-2016-mers-saudi-arabia/en). The role of domestic animals as an intermediate host for humans was initially suggested by case histories of infected patients who had visited farms or tended sick animals shortly before onset of infection (2). This suggestion was given credence by a study of camel serum samples that showed high levels of neutralizing antibodies in disparate camel populations (3); the findings were subsequently confirmed by virus detection and sequencing (4).
Infection trials in camels have been limited (5,6), mainly because of difficulties in housing and handling the animals in a high-containment facility, which is necessary because the virus has a Biosafety Level 3 classification (7). However, the alpaca, a close relative within the Camelidae family, may provide a temperamentally suitable and valuable animal model for MERS-CoV infection, particularly for developing and testing vaccine candidates for camels. We sought to assess whether alpacas could be infected by means of a natural (oronasal) route, to determine whether viral shedding occurred after reinfection, and to evaluate the development of serologic markers of protection.
The Study
We obtained 3 adult female alpacas (Vicugna pacos) from a commercial supplier in Victoria, Australia, and housed them in the Biosafety Level 3 containment facility at the CSIRO Australian Animal Health Laboratory. Before experiments, the alpacas were allowed to acclimatize for 6 days; during this time, intrauterine temperature data loggers were implanted according to a previously published procedure (8). We found no previous MERS-CoV challenge trial reported in alpacas, so we chose a preliminary dose and rechallenge time on the basis of our experience with other virus infection trials for other emerging infectious diseases (8).
We used a camel isolate of MERS-CoV (Dromedary_MERS-CoV_Al-Hasa_KFU-HKU13/2013; GenBank accession nos. KJ650295–KJ650297) for infection; the isolate was prepared in Vero cells as described (9). The 3 alpacas were exposed oronasally to a 106 50% tissue culture infective dose of MERS-CoV in 5 mL of phosphate-buffered saline. The animals were monitored for 21 days, reexposed to a replicate challenge of MERS-CoV, and observed for 14 more days. Clinical samples of blood (in EDTA for obtaining serum) and swabs (deep and superficial nasal, oral, rectal, and urogenital) were collected immediately before inoculation and thereafter on days 3, 5, 7, 10, 12, 14, 21, 26, 28, 31, 33, and 35. Alpacas were electively euthanized, 1 on day 33 and the others on day 35.
The animals remained clinically healthy except for a reduced condition score that occurred by day 18 in 1 animal (alpaca 2); no signs of upper or lower respiratory tract disease appeared in any animal. Increased temperature was noted in alpaca 2 during days 17–20, but fever (rectal temperature >39°C) was not recorded. Gross abnormalities at postmortem examination were found only in alpaca 2 and comprised extensive adhesions of the caudal sac of compartment 1 of the stomach to the umbilicus; clinical findings in this animal were attributed to this lesion.
RNA extraction and real-time PCR were performed by following specimen-handling procedures established for Hendra virus (8) and were used to identify shedding patterns after each challenge. After initial challenge, viral RNA was detected in each animal from oral and deep and superficial nasal swab samples taken on days 3–12 (Table 1).
Table 1. Virus shedding in 3 alpacas infected with MERS-Cov, as measured by virus isolation and real-time PCR for each sample day*.
| Dpi | Cycle threshold value (virus isolation result)†‡ |
No. positive/no. tested |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Deep nasal swab sample |
Oral swab sample |
Superficial nasal swab sample |
||||||||||||
| Alpaca 1 | Alpaca 2 | Alpaca 3 | Alpaca 1 | Alpaca 2 | Alpaca 3 | Alpaca 1 | Alpaca 2 | Alpaca 3 | Real-time PCR | Virus isolation | ||||
| 0 | U (–) | U (–) | U (–) | U (–) | 40.8 (–) | U (–) | U (–) | U (–) | U (–) | 0/3 | 0/3 | |||
| 3 | 33.4 (+) | 29.0 (–) | U (–) | 34.2 (–) | 31.7 (–) | 42.3 (–) | 35.4 (–) | 40.7 (–) | U (–) | 2/3 | 1/3 | |||
| 5 | 34.9 (–) | 33.5 (–) | 34.2 (–) | 32.0 (–) | 35.4 (–) | 32.0 (+) | 35.0 (–) | 33.0 (–) | 32.5 (–) | 3/3 | 1/3 | |||
| 7 | 29.4 (+) | 18.2 (–) | 31.4 (+) | 32.7 (–) | 30.1 (+) | 28.3 (+) | 31.9 (–) | 28.5 (+) | 38.6 (+) | 3/3 | 3/3 | |||
| 10 | 41.0 (–) | 37.5 (+) | U (–) | 41.3 (–) | 38.0 (–) | 30.5 (+) | 39.9 (–) | 36.0 (+) | U (–) | 3/3 | 2/3 | |||
| 12 | 42.0 (–) | 36.4 (–) | U (–) | U (–) | U (–) | 37.3 (+) | 42.0 (–) | 39.5 (+) | U (–) | 2/3 | 2/3 | |||
| 14 | U (–) | 42.2 (–) | U (–) | 43.0 (–) | 44.0 (–) | 43.0 (–) | U (–) | U (–) | U (–) | 0/3 | 0/3 | |||
| 21 | U (–) | U (–) | U (–) | U (–) | U (–) | U (–) | U (–) | U (–) | U (–) | 0/3 | 0/3 | |||
| 24 | U (–) | U (–) | U (–) | 40.8 (–) | U (–) | U (–) | U (–) | 43.2 (–) | U (–) | 0/3 | 0/3 | |||
| 26 | U (–) | U (–) | U (–) | U (–) | U (–) | U (–) | U (–) | U (–) | U (–) | 0/3 | 0/3 | |||
| 28 | U (–) | U (–) | U (–) | U (–) | U (–) | U (–) | U (–) | U (–) | U (–) | 0/3 | 0/3 | |||
| 31 | U (–) | U (–) | U (–) | U (–) | U (–) | U (–) | U (–) | U (–) | U (–) | 0/3 | 0/3 | |||
| 33 | U (–) | U (–) | U (–) | U (–) | U (–) | U (–) | U (–) | 43.1 (–) | U (–) | 0/3 | 0/3 | |||
| 35§ | U (–) | NA | U (–) | U (–) | NA | U (–) | U (–) | NA | U (–) | 0/2 | 0/2 | |||
*Bold indicates positive results (cycle threshold <40). Gray shading indicates that >1 animal was positive for the sample collected on that day. Dpi, day postinfection for challenge (initial infection); MERS-CoV, Middle East respiratory syndrome coronavirus; NA, not available; U, undetermined; –, negative; +, positive. †Real-time PCR cycle threshold values are an average of the duplicates, except when 1 result was undetermined; then, only the single numeric value is shown. ‡The starting dilution was 1:10; the threshold for a positive result was a dilution of >1:20. §Alpaca 2 was euthanized at day 33, leaving only 2 animals in the study at day 35.
Virus isolation was undertaken with Vero cells by using published protocols (9) and was successful for all 3 animals from all types of samples. Virus recovery was successful from oral and superficial nasal swab samples through day 12; deep nasal swab samples were positive only through day 10. All urogenital and rectal swab samples were negative by both real-time PCR and virus isolation. After rechallenge, viral RNA was not detected with confidence from any sample (Figure).
Figure.
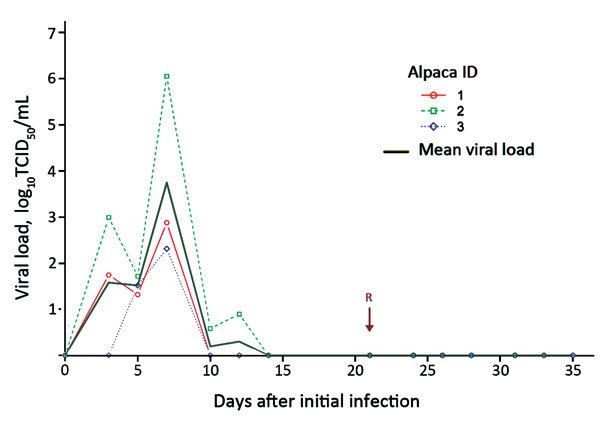
Virus shedding of MERS-CoV from 3 infected alpacas as detected from the deep nasal swab samples by day after initial infection and reinfection. Viral load was estimated from real-time cycle threshold values and a calibration experiment. Arrow indicates day 21, when the animals were reinfected with MERS-CoV. MERS-COV, Middle East respiratory syndrome coronavirus; TCID, tissue culture infective dose.
Serum samples were assessed for immunologic responses by using a virus neutralization test (VNT) and a Luminex bead assay to the nucleocapsid protein. We used in-house assays modeled after those previously developed to assess the serologic status of feral camels in central Australia (10). All animals were seronegative by both Luminex and VNT before challenge. Antibody was first detected by Luminex on day 10 or day 12 in each animal (Table 2); neutralizing antibody titers were 1:20 to 1:40 in alpaca 2 from day 10. Neutralizing antibody titers of 1:10 to 1:20 were detected in alpaca 1 from day 21 on but not in alpaca 3 at any time during the study. For controls, we used MERS-CoV positive and negative serum samples from Egypt and Australia (Technical Appendix Table).
Table 2. Serologic responses in 3 infected alpacas, as measured by virus neutralization tests and Luminex bead assays for selected sample days*.
| Dpi | Serologic results |
No. positive/no. tested)§ |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| VNT titer† |
Luminex assay MFI‡ |
|||||||||
| Alpaca 1 | Alpaca 2 | Alpaca 3 | Alpaca 1 | Alpaca 2 | Alpaca 3 | VNT | Luminex | |||
| 0 | Negative | Negative | Negative | 787 | 889 | 167 | 0/3 | 0/3 | ||
| 3 | Negative | Negative | Negative | 373 | 814 | 152 | 0/3 | 0/3 | ||
| 5 | Negative | Negative | Negative | 418 | 945 | 223 | 0/3 | 0/3 | ||
| 7 | Negative | Negative | Negative | 272 | 932 | 249 | 0/3 | 0/3 | ||
| 10 | Negative | 1:40 | Negative | 478 | 2,869 | 58 | 1/3 | 1/3 | ||
| 12 | Negative | 1:40 | Negative | 928 | 10,274 | 331 | 1/3 | 1/3 | ||
| 14 | Negative | 1:40 | Negative | 1,041 | 7,658 | 899 | 1/3 | 1/3 | ||
| 21 | 1:10 | 1:40 | Negative | 877 | 6,893 | 629 | 1/3 | 1/3 | ||
| 24 | 1:20 | 1:20 | Negative | 1,506 | 3,324 | 678 | 2/3 | 1/3 | ||
| 26 | 1:20 | 1:20 | Negative | 853 | 4,161 | 667 | 2/3 | 1/3 | ||
| 28 | 1:20 | 1:20 | Negative | 773 | 4,682 | 724 | 2/3 | 1/3 | ||
| 31 | 1:20 | 1:40 | Negative | 548 | 11,259 | 649 | 2/3 | 1/3 | ||
| 33 | 1:10 | 1:20 | Negative | 688 | 6,090 | 455 | 1/3 | 1/3 | ||
| 35§ | 1:10 | NA | Negative | 510 | NA | 586 | 0/2 | 0/2 | ||
*Bold indicates positive results. Gray shading indicates that >1 animal was positive for the sample collected on that day. Dpi, day postinfection for challenge (initial infection); MFI, median fluorescent intensity; VNT, virus neutralization test. †The starting dilution was 1:10, and the threshold for a positive result was a dilution of >1:20. ‡The MFI threshold for a positive result for the Luminex assay was 2,500. §Alpaca 2 was euthanized at day 33, leaving only 2 animals in the study at day 35.
Conclusions
Our study confirms that alpacas are susceptible to MERS-CoV infection; this finding is consistent with a previous report showing that alpaca kidney cell lines possessing the dipeptidyl peptidase-4 receptor could be infected in vitro (11). Our challenge/rechallenge trial was planned as a first stage in the assessment of the alpaca as a potential surrogate for camels for MERS-CoV vaccine testing. Consequently, the trial was not designed for direct comparison with 2 previous MERS-CoV challenge trials reported in camels (5,6). Our trial used a lower challenge dose and a different timeframe for observation; nevertheless, some preliminary comparative observations may be useful. In the previous studies, as in ours, the animals were inoculated by the oronasal route, and live virus was detected through day 7 postinfection. Similarly, neutralizing antibodies were detected beginning 7–8 days postinfection. However, findings in the trials with camels differed considerably from findings in our trial. The trials with camels detected live virus from nasal washes at days 1–3, a nasal discharge, and transient temperature rises; viral RNA was detected by real-time PCR for an extended period. Furthermore, the VNT titers for camels were much higher than those for the alpacas in our study. These differences possibly represent underlying dissimilarities in immune responses to MERS-CoV for the 2 species but may also result from the higher infecting dose (107 50% tissue culture infective dose) used in the camel studies.
Our study showed that alpacas secreted live virus after oronasal infection and that the immune response to the initial infection prevented further excretion following reinfection. An underlying assumption in our trial is that the initial infection equates to natural vaccination and that the lack of viral excretion thus follows an induced immune memory response. However, our results indicate that this immunologic response is complex; although a strong serologic response developed in only 1 alpaca, all 3 alpacas were refractory to reinfection.
This study has several limitations. First, it was a preliminary study with only 3 animals and functioned more as proof of concept than a definitive study of the use of alpacas as a model for studying infection dynamics of MERS-CoV in camelids. Second, our observation period of 21 days before rechallenge is informative but does not provide complete information on duration of protective immunity. Future studies should have a larger sample and a longer period of study postinoculation. Third, our study did not seek to understand the pathogenesis of infection; we did not conduct histopathology or immunohistochemistry to understand the site of initial viral replication and the role of mucosal immunity in mounting an effective immune response upon infection.
Notwithstanding these limitations, we believe that the alpaca might be a useful model that could greatly facilitate the development and testing of vaccine candidates. We recommend further research and trials to substantiate this potential.
Note Added in Proof: Adney et al. also report infection, replication, and transmission of Middle East respiratory syndrome coronavirus in alpacas in this issue of Emerging Infectious Diseases (12).
Technical Appendix. Results from virus neutralizing tests and Luminex assays for control sera used in study of 3 alpacas experimentally infected with MERS-CoV.
Acknowledgments
We thank Kaylene Selleck, Leah Frazer, Jean Payne, Rachel Arkinstall, and Mahen Perera for providing technical assistance and support for this study.
The study was endorsed by the CSIRO AAHL Animal Ethics Committee under protocol AAEC #1762. The project was funded by CSIRO appropriation fund. L.-F.W. is supported in part by a National Research Foundation grant (NRF2012NRF-CRP001-056) in Singapore.
Biography
Mr. Crameri is a virologist with the CSIRO Australian Animal Health Laboratory. He has pioneered work in the high biocontainment facility at CSIRO and worked on Hendra, Nipah, SARS, MERS, Ebola, and many other viruses with high impact to human and animal health.
Footnotes
Suggested citation for this article: Crameri G, Durr PA, Klein R, Foord A, Yu M, Riddell S, et al. Experimental infection and response to rechallenge of alpacas with Middle East respiratory syndrome coronavirus. Emerg Infect Dis. 2016 Jun [date cited]. http://dx.doi.org/10.3201/eid2206.160007
References
- 1.Zaki AM, van Boheemen S, Bestebroer TM, Osterhaus AD, Fouchier RA. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N Engl J Med. 2012;367:1814–20. 10.1056/NEJMoa1211721 [DOI] [PubMed] [Google Scholar]
- 2.Drosten C, Seilmaier M, Corman VM, Hartmann W, Scheible G, Sack S, et al. Clinical features and virological analysis of a case of Middle East respiratory syndrome coronavirus infection. Lancet Infect Dis. 2013;13:745–51. 10.1016/S1473-3099(13)70154-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reusken CB, Haagmans BL, Müller MA, Gutierrez C, Godeke GJ, Meyer B, et al. Middle East respiratory syndrome coronavirus neutralising serum antibodies in dromedary camels: a comparative serological study. Lancet Infect Dis. 2013;13:859–66. 10.1016/S1473-3099(13)70164-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Haagmans BL, Al Dhahiry SH, Reusken CB, Raj VS, Galiano M, Myers R, et al. Middle East respiratory syndrome coronavirus in dromedary camels: an outbreak investigation. Lancet Infect Dis. 2014;14:140–5. 10.1016/S1473-3099(13)70690-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Adney DR, van Doremalen N, Brown VR, Bushmaker T, Scott D, de Wit E, et al. Replication and shedding of MERS-CoV in upper respiratory tract of inoculated dromedary camels. Emerg Infect Dis. 2014;20:1999–2005. 10.3201/eid2012.141280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haagmans BL, van den Brand JM, Raj VS, Volz A, Wohlsein P, Smits SL, et al. An orthopoxvirus-based vaccine reduces virus excretion after MERS-CoV infection in dromedary camels. Science. 2016;351:77–81. 10.1126/science.aad1283 [DOI] [PubMed] [Google Scholar]
- 7.Kumar M, Mazur S, Ork BL, Postnikova E, Hensley LE, Jahrling PB, et al. Inactivation and safety testing of Middle East respiratory syndrome coronavirus. J Virol Methods. 2015;223:13–8. 10.1016/j.jviromet.2015.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Middleton D, Pallister J, Klein R, Feng YR, Haining J, Arkinstall R, et al. Hendra virus vaccine, a one health approach to protecting horse, human, and environmental health. Emerg Infect Dis. 2014;20:372–9. 10.3201/eid2003.131159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hemida MG, Chu DK, Poon LL, Perera RA, Alhammadi MA, Ng HY, et al. MERS coronavirus in dromedary camel herd, Saudi Arabia. Emerg Infect Dis. 2014;20:1231–4. 10.3201/eid2007.140571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Crameri G, Durr PA, Barr J, Yu M, Graham K, Williams OJ, et al. Absence of MERS-CoV antibodies in feral camels in Australia: implications for the pathogen’s origin and spread. One Health. 2015;1:76–82.. 10.1016/j.onehlt.2015.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eckerle I, Corman VM, Müller MA, Lenk M, Ulrich RG, Drosten C. Replicative capacity of MERS coronavirus in livestock cell lines. Emerg Infect Dis. 2014;20:276–9. 10.3201/eid2002.131182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Adney DR, Bielefeldt-Ohmann H, Hartwig AE, Bowen RA. Infection, replication, and transmission of Middle East respiratory syndrome coronavirus in alpacas. Emerg Infect Dis. 2016;22:1037–43. 10.3201/eid2206.160192 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Technical Appendix. Results from virus neutralizing tests and Luminex assays for control sera used in study of 3 alpacas experimentally infected with MERS-CoV.


