Abstract
Objectives. To determine whether proximity to a supermarket modified the effects of an obesity intervention.
Methods. We examined 498 children aged 6 to 12 years with a body mass index (BMI) at or above the 95th percentile participating in an obesity trial in Massachusetts in 2011 to 2013. The practice-based interventions included computerized clinician decision support plus family self-guided behavior change or health coaching. Outcomes were 1-year change in BMI z-score, sugar-sweetened beverage intake, and fruit and vegetable intake. We examined distance to the closest supermarket as an effect modifier.
Results. Distance to supermarkets was an effect modifier of 1-year change in BMI z-score and fruit and vegetable intake but not sugar-sweetened beverage intake. With each 1-mile shorter distance to a supermarket, intervention participants increased their fruit and vegetable intake by 0.29 servings per day and decreased their BMI z-score by −0.04 units relative to controls.
Conclusions. Living closer to a supermarket is associated with greater improvements in fruit and vegetable intake and weight status in an obesity intervention.
The prevalence of childhood obesity remains high despite public health and clinical efforts to prevent and manage obesity.1 Evidence suggests that the etiology and, thus, prevention of obesity may be influenced by the food, beverage, and physical activity environments of children. Understanding the role of environmental factors in obesity and developing interventions to change default environments may have important effects on reductions in obesity incidence and prevalence and public health.
Mounting evidence suggests that aspects of the built environment, including access to healthful food establishments, may facilitate behavior change and improve weight status. For example, studies have shown protective associations of living closer to supermarkets with children’s dietary behaviors and body mass index (BMI).2–5 Because families face budget and time constraints, living closer to a large supermarket could assist families in making healthy dietary and BMI changes by increasing access to affordable healthy food and beverages available in these establishments. Furthermore, the Centers for Disease Control and Prevention has endorsed increasing the number of supermarkets in underserved areas as 1 of the 24 strategies to help communities prevent obesity.6 Additionally, in 2010 the White House Childhood Obesity Task Force emphasized the need to improve access to fresh, healthy, affordable food by eliminating “food deserts”—defined as neighborhoods without access to fresh, healthy, and affordable food.7,8
Although cross-sectional and longitudinal studies support the protective effect of easy access to supermarkets on children’s obesity risk, few studies have examined the modifying effects of the food environment, particularly supermarkets, in facilitating BMI and behavior change in a childhood obesity randomized controlled trial.
We examined the extent to which living closer to supermarkets modified the effects of a childhood obesity randomized controlled trial on changes in BMI and diet. We hypothesized that children in the obesity intervention who lived closer to a large supermarket would have greater decreases in their BMI z-score and their intakes of sugar-sweetened beverages (SSBs) and a greater increase in their fruit and vegetable intake than would those living farther away.
METHODS
Study participants were children participating in the Study of Technology to Accelerate Research (STAR) trial, a cluster-randomized obesity intervention that took place from October 2011 through July 2013.9 The study took place in 14 pediatric practices in eastern Massachusetts. Children were eligible for the study if they were aged 6 to 12 years, had a BMI at or above the 95th percentile, and received well-child care visits at 1 of the 14 practices. Recruitment, eligibility, and study procedures of the STAR trial have been published previously.9,10
We excluded children if they had a residential address outside Massachusetts or their address was a post office box or unidentifiable (n = 43) or if they did not complete the 1-year follow-up survey (n = 8). The sample size for this analysis was 498 (91% of 549 children enrolled in STAR).
Main Exposures
The main exposure was the intervention. We randomly assigned practices to 1 of 3 arms: (1) usual care (4 practices), (2) computerized clinician decision support (CDS) plus a family self-guided behavior change intervention (5 practices), or (3) computerized CDS plus a health coach intervention (CDS + coaching; 5 practices).
We modified the electronic health record to deploy a computerized, point-of-care decision support alert to clinicians at the time of a well-child care visit for a child with a BMI at or above the 95th percentile in the intervention sites.11 The alert contained links to growth charts,12 evidence-based childhood obesity screening and management guidelines,13 and a prepopulated, standardized note template specific for obesity that included options for
documenting and coding for BMI percentile,
documenting and coding for nutrition and physical activity counseling,
placing referrals for weight management programs,
placing orders for laboratory studies if appropriate, and
printing educational materials.
We also trained the clinicians in the intervention practices to use motivational interviewing to negotiate a follow-up weight management plan with the patient and family.
To augment the clinical intervention and support families in behavior change, we developed a comprehensive set of educational materials for clinicians to provide to their patients that focused on individual- and family-level behaviors. These behaviors included
decreases in screen time,
decreases in consumption of SSBs,
increases in moderate and vigorous physical activity,
improvement of sleep duration and quality, and
improving diet quality, including increasing fruit and vegetable intake.
Families in the CDS arm also received 4 newsletters throughout the intervention period encouraging self-guided behavior change, including increasing their fruit and vegetable intake, and a subscription to CHOP CHOP, a magazine that provides healthy kid-friendly recipes that are focused on fruits and vegetables.
In the CDS + coaching intervention, families received individualized coaching. We assigned families a health coach, who used motivational interviewing14 to support families by telephone at 1, 3, 6, and 9 months. We also invited parents to participate in an interactive text message program. Text messages included the following:
For your child, replace 1 high-calorie snack a day with fruit or a vegetable. Keep washed, cut, ready to eat fruits and veggies on hand for easy snacking.
Crunch! Fruits and veggies make great kid snacks. Cut back on high-calorie snacks and munch on carrots with low-fat ranch dressing or fruit with yogurt.
Any parent who chose not to receive texts had the option to receive the same messages by e-mail. Twice-weekly texts over 1 year provided behavior change support for the patient and family.
We used the Centers for Disease Control and Prevention growth curves to define the participants BMI z-score.12 Children in the CDS intervention had a similar change in BMI z-score over 1 year (–0.06 units; 95% confidence interval [CI] = −0.11, −0.02) compared with the CDS + coaching intervention (–0.05; 95% CI = −0.09, 0.00; P = .52).10 Children in the CDS + coaching intervention had a greater decrease in SSBs (–0.26 servings per day; 95% CI = –0.57, 0.05) compared with the CDS intervention (0.07 servings per day; 95% CI = −0.22, 0.37; P = .03) and slightly greater increase in fruit and vegetable intake (0.32 servings per day; 95% CI = 0.01, 0.64) compared with those in the CDS intervention (0.09 servings per day; 95% CI = −0.21, 0.39; P = .24). Because there were no significant differences in the effect sizes between the 2 intervention arms for BMI z-score (P = .52) and fruit and vegetable intake (P = .24), we combined the 2 intervention arms to increase our ability to detect effect modification by the neighborhood food environment.
Documentation of nutrition or physical activity counseling in the 2 intervention arms significantly improved compared with controls. In the CDS arm, there was a 45% increase in documentation of nutrition or physical activity counseling (95% CI = 37, 53). In the CDS + coaching arm, the documentation increased by 25% (95% CI = 14, 40) compared with usual care.
Change in Dietary Behavior and Body Mass Index z-Score
The outcome measures for this analysis were 1-year changes in BMI z-score, SSB intake, and fruit and vegetable intake. We used validated questions from a food frequency questionnaire to measure SSB intake change and fruit and vegetable intake in servings per day.15 We gave parents a list of a variety of fruits and vegetables and asked them on average in the past month how often their child had eaten them. The response categories included never, less than once per week, once per week, 2 to 4 times per week, about once per day, or twice or more per day. We combined the responses and calculated a per day average. We also asked parents on average in the past month how often did their child drink a serving of regular soda, juice, fruit drinks, or sports drinks. Response categories were open ended per day, per week, or per month. We summed and averaged these responses per day. We asked parents these questions at baseline and at 1-year follow-up using telephone surveys.
We derived children’s age- and gender-specific BMI z-scores from the height and weight measurements recorded in the electronic health record at enrollment and at their 1-year well-child visits. At each well-child visit, medical assistants measured height and weight following a written standardized protocol, which is consistent with the standard of care in pediatric primary care (described in detail in previously published work16).
Effect Modifier
We examined distance to large supermarkets as an effect modifier of the relationship between intervention and 1-year outcomes (BMI z-score change and dietary change). We located supermarkets using the North American Industry Classification System. This classification system is the standard that federal statistical agencies use to classify and analyze the US business economy.17 We defined large supermarkets as those with more than 50 employees.
We obtained the large supermarket information from the 2009 InfoUSA database, which is available in the ArcGIS Business Analyst Tool. Using ArcGIS, version 10 Network Analyst Extension Closest Facility tool and StreetMap USA detailed streets (ESRI, Redlands CA), we calculated distances along the street network from each participant’s residence to the closest large supermarket. We examined distance as a continuous variable.
Covariates
We obtained children’s gender and age from the electronic health record and their race/ethnicity from parent report on the baseline survey. We obtained parent age and country of birth from the surveys. We obtained neighborhood median income by linking the child’s geocoded residential addresses with 2006 to 2010 American Community Survey data at the US census tract level. We defined fast-food restaurants using North American Industry Classification System codes, which included pizza restaurants and fast-food franchise codes.
We obtained networked street distance to the nearest fast-food restaurant using the same protocol for networked street distance to large supermarkets. We adjusted for fast food because large supermarkets are often located near a fast-food restaurant. Although we had data on parent’s individual income, we did not find this to be a statistically significant covariate.
Statistical Analysis
We examined the descriptive and bivariate associations of proximity to a large supermarket and the outcomes and covariates first. We used generalized linear mixed effects regression to examine the main effects of the intervention on 1-year changes in BMI z-score, SSB intake, and fruit and vegetable intake. All analyses included a random effect for primary care to account for clustering by site. This is an accepted statistical method to evaluate cluster-randomized controlled trials because the analysis treats the primary care centers as nested within the treatment arm and as a random effect, and the proximity is treated as a crossed and fixed effect.18
We included a multiplicative interaction term between networked distance to a large supermarket and intervention status in the models; this allowed us to determine effect modification in the relationship between intervention status and the outcomes by children’s proximity to large supermarkets. Model 1 included no additional covariates. Model 2 was adjusted for children’s race/ethnicity, gender, age, parental age, parent’s country of birth, neighborhood median income, and networked street distance to the nearest fast-food restaurant. We made adjustments for distance to fast-food restaurants because of the perception that distance to large supermarkets simply captured distance to a commercial area. Controlling for distance to fast-food allowed us, in part, to control for this possibility. We conducted statistical analyses using SAS version 9.3 (SAS Institute Inc., Cary, NC).
RESULTS
At baseline, mean ±SD age of the children was 9.7 ±1.9 years. Mean ±SD change in BMI z-score over 1 year was −0.07 ±0.22. Approximately half of the participants were girls and 52% were non-Hispanic White. The participants’ mean ±SD census tract median neighborhood household income was $73 571 ±$29 381. By comparison, the median neighborhood household income in Massachusetts from 2007 to 2011 was $65 981.19 The mean ±SD networked distance from participants’ residence to the closest large supermarket and fast-food restaurant was 1.44 ±0.96 miles and 0.73 ±0.63 miles, respectively. The mean distance to large supermarkets by town is available in Figure A, available as a supplement to the online version of this article at http://www.ajph.org. Towns with the largest mean distances from both large supermarkets are generally farther away from Boston.
In bivariate analyses, more children in the intervention versus usual care were White (56% vs 44%; P = .02, after adjustment for clustering P = .95; Table 1). More parents were born outside the United States in usual care versus intervention (31% vs 22%; P = .03, after adjustment for clustering P = .88). Over the 1-year study period, children in the intervention decreased their BMI z-score by −0.09 units versus −0.04 in the usual care group (P = .01; Table 2). Children in the intervention increased their fruit and vegetable intake and decreased their SSB intake more than did those in usual care, although neither change was statistically significant.
TABLE 1—
Baseline Characteristics of 498 Children Aged 6–12 Years Participating in the Study of Technology to Accelerate Research Trial: Massachusetts, 2011–2013
| Intervention Status, No. (%) or Mean ±SD |
|||
| Characteristic | Usual Care (n = 169) | Intervention (n = 329) | P |
| Children | |||
| Gender | .61 | ||
| Male | 94 (56) | 175 (53) | |
| Female | 75 (44) | 154 (47) | |
| Race/ethnicity | .02 | ||
| White | 74 (44) | 183 (56) | |
| Black | 36 (21) | 64 (20) | |
| Hispanic | 38 (23) | 31 (9) | |
| Asian | 9 (5) | 16 (5) | |
| Other | 11 (7) | 34 (10) | |
| Age, y | 9.7 ±1.9 | 9.7 ±1.9 | .89 |
| Parents | |||
| US-born | .03 | ||
| Yes | 117 (69) | 257 (78) | |
| No | 52 (31) | 72 (22) | |
| Age, y | 40.0 ±7.5 | 42.0 ±6.1 | .01 |
| Household income, $ | .15 | ||
| ≤ 50 000 | 58 (36) | 93 (29) | |
| > 50 000 | 105 (64) | 226 (71) | |
| Neighborhood | |||
| Median household income, $ | 69 450 ±25 793 | 75 689 ±30 888 | .03 |
| Distance to a large supermarket, miles | 1.37 (0.88) | 1.47 (1.00) | .29 |
| Distance to a fast-food restaurant, miles | 0.76 (0.66) | 0.66 (0.57) | .12 |
TABLE 2—
Baseline and 1-Year Change in Dietary Behaviors and BMI z-Score: Study of Technology to Accelerate Research, Massachusetts, 2011–2013
| Intervention Status, Mean ±SD |
|||
| Behavior Change | Usual Care (n = 169) | Intervention (n = 320) | P |
| Baseline | |||
| Fruit and vegetable intake, servings per day | 2.66 ±1.36 | 2.55 ±1.26 | .38 |
| SSB intake, servings per day | 1.40 ±1.10 | 1.60 ±1.50 | .12 |
| BMI z-scorea | 2.05 ±0.30 | 2.04 ±0.30 | .96 |
| 1-y change | |||
| Fruit and vegetable intake, servings per day | 0.10 ±1.35 | 0.28 ±1.32 | .16 |
| SSB intake, servings per day | −0.32 ±1.47 | −0.40 ±1.36 | .56 |
| BMI z-scorea | −0.04 ±0.22 | −0.09 ±0.22 | .01 |
Note. BMI = body mass index; SSB = sugar-sweetened beverage.
We used the Centers for Disease Control and Prevention growth curves to define the participants' BMI z-scores.12
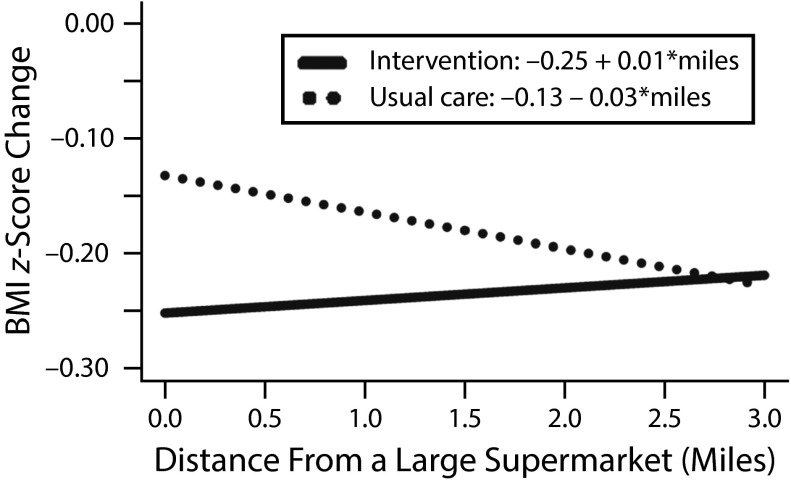
In unadjusted models there was a significant interaction (interaction term P = .02) between intervention status and networked distance to a large supermarket and 1-year change in BMI z-score. BMI z-score decreased by 0.05 units (95% CI = −0.01, −0.10) for every mile closer participants lived to a large supermarket in the intervention compared with usual care arm. This change reflects a difference in slopes: people living closer to supermarkets in the intervention arm had a greater BMI z-score decrease over 1 year than did those who lived farther away. A change of 0.05 BMI z-score units for a girl aged 9 years in the 95th percentile for BMI (50th percentile for height and 95th percentile for weight) is 1.1 pounds.20 After adjustment for neighborhood and parental covariates, networked distance to a large supermarket was a weaker effect modifier, with a P = .07 (Figure 1). For example, children living 1 mile away from a large supermarket decreased their BMI z-score by 0.24 units in the intervention group compared with 0.16 units in the usual care group. At 2 miles children in the intervention group decreased their BMI z-score by 0.23 units, whereas children in the usual care group decreased theirs by 0.20 units.
FIGURE 1—
Adjusted Estimates of Body Mass Index z-Score Change: Study of Technology to Accelerate Research, Massachusetts, 2011–2013
Note. We used the Centers for Disease Control and Prevention growth curves to define the participants' BMI z-scores.12 Models were adjusted for child’s race/ethnicity, age, gender, parental age, whether parent is US born, neighborhood median income, and networked street distance to nearest fast-food restaurant. P = .07 for difference between the intervention and usual care lines.
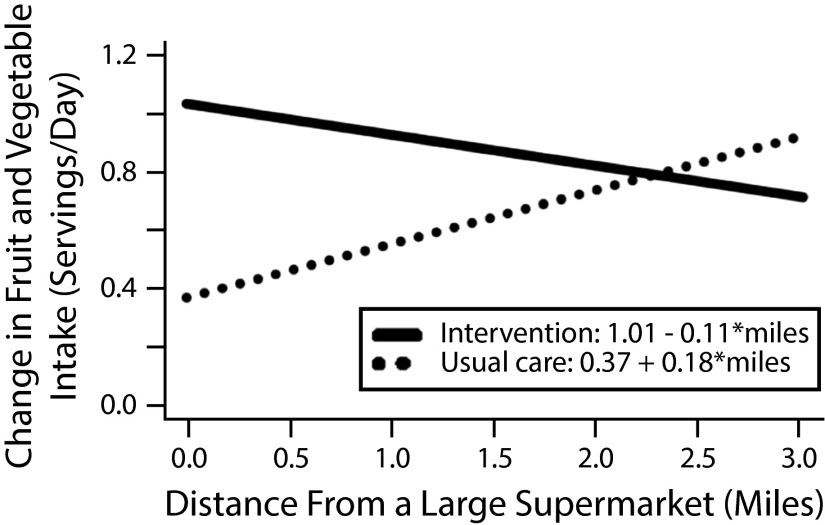
In unadjusted models, for 1-year change in fruit and vegetable intake there was a significant interaction (interaction term P = .03) between intervention status and networked distance to the closest large supermarket and 1-year change in fruit and vegetable intake. For each 1 mile closer that participants lived to large supermarkets, children in the intervention arms increased their fruit and vegetable intake by 0.31 servings per day (95% CI = 0.03, 0.59) compared with usual care. Adjustment for individual, parent, and neighborhood covariates attenuated the estimate to 0.29 servings per day (95% CI = 0.01, 0.57). Similar to results for BMI z-score, this estimate demonstrates that children living closer to supermarkets in the intervention arm increased their fruit and vegetable intake more than did those living farther away (Figure 2). For example, for children living 1 mile away from a large supermarket, those in the intervention group increased their fruit and vegetable intake by 0.91 servings per day, whereas those in the usual care group increased theirs by 0.55 servings per day. Distance to a large supermarket was not an effect modifier of SSB intake (interaction P = .36).
FIGURE 2—
Adjusted Estimates of Fruit and Vegetable Intake Change: Study of Technology to Accelerate Research, Massachusetts, 2011–2013
Note. Models were adjusted for child’s race/ethnicity, age, gender, parental age, whether parent is US born, neighborhood median income, and networked street distance to nearest fast-food restaurant. P = .04 for difference between the intervention and usual care lines.
DISCUSSION
In this study of 498 children participating in a childhood obesity cluster-randomized trial, distance to a large supermarket was an effect modifier of 1-year changes in BMI z-score and fruit and vegetable intake. The data suggest that children who received the STAR intervention and who lived closer to a large supermarket showed greater 1-year declines in their BMI z-score and increased their fruit and vegetable intake more than did those living farther away. Distance to large supermarkets was not an effect modifier of the relationship between the intervention and SSB intake.
This study is one of the few studies to examine effect modification of an intervention by aspects of children’s built environments. In a study of 191 children in an obesity intervention, Epstein et al. found that children with access to 3 or more supermarkets within a 5-minute drive decreased their BMI z-score less than did children with no supermarkets within a 5-minute drive (0.20 units vs 0.37 units).21 We speculate that our results differed because we examined the closest supermarket and they examined access to 3 or more supermarkets. Having access to 3 or more supermarkets within a short distance is more likely a marker of high food establishment density and access to other food establishments, such as fast-food restaurants.
By measuring distance to the nearest large supermarket and adjusting for distance to the nearest fast-food restaurant, we are more likely to be measuring access to affordable healthy food. Kerr et al. examined whether the built environment modified a physical activity intervention in 441 men.22 In that study, men in the intervention living in low walkable neighborhoods increased their daily walking time by 29 minutes compared with those in high walkable neighborhoods, who decreased their walking time by 10 minutes; this may suggest that the intervention was able to overcome neighborhood barriers. Similarly, perhaps the STAR intervention encouraged families to choose more healthy foods at their nearby supermarket and this is why we saw the differing effects of proximity to supermarkets on the usual care versus the intervention arms.
Several potential mechanisms can explain the observed relationships with fruit and vegetable intake and proximity to a large supermarket. It has been shown that living closer to a large supermarket is associated with greater fruit and vegetable intake.23,24 In Detroit, Michigan, women shopping at supermarkets versus those shopping at independent grocers had higher fruit and vegetable intake.25 Families face time and budget constraints. If a supermarket is located closer to their homes they are more likely to have the opportunity to purchase fruit and vegetables. By encouraging physicians to counsel families on nutrition, the STAR intervention likely had an impact on how families interacted with their nearby supermarket. We also provided families with educational materials focused on nutrition and a subscription to CHOP CHOP, which may have also increased their use of their nearby supermarket.
Several studies indicate that replacing energy-dense foods with fruit and vegetables has a protective association with BMI26,27 and that higher prices of fruit and vegetables are inversely associated with higher BMI.28 Furthermore, supermarkets have been shown to have more availability of fruit and vegetables29 than do other food stores, and often at a lower price. Although we could not explicitly test this, it is possible that being closer to large supermarkets provided families with the ability to replace energy-dense foods with fruit and vegetables. This replacement would theoretically lead to decreasing the children’s overall energy intake and decreasing their BMI z-score over the 1-year intervention period.
There was no difference in the magnitude of change in SSB intake between the intervention and usual care groups (P = .56). This may be because SSBs are available in many other types of food establishments and may make the intervention less likely to succeed.
Strengths and Limitations
This study has numerous strengths, including the use of effect modification of an intervention by proximity to a healthful food establishment, the availability and adjustment for potential individual- and neighborhood-level covariates, and the use of objective BMI measures from an electronic medical record. Another strength is that we adjusted for proximity to fast-food restaurants because fast-food restaurants and supermarkets are often located near each other.
This study also has several limitations. First, data quality from commercial business listings such as InfoUSA can be a concern in this type of research because of misclassification of business type. In previously published articles, InfoUSA classified 81% of supermarkets correctly.30
We did not ask participants where they purchased food for their families, and previous studies have shown that adults do not always shop at the closest grocery store.31 We also did not have information on the foods offered in the supermarkets or participants’ schools. Distance to large supermarkets could be a proxy for other favorable neighborhood characteristics, such as parks, that we did not account for. Additionally, the most recent address for the children was the only address we obtained, and thus we could not account for moving during the intervention period.
We did not have information on whether families owned cars. Perhaps parents with cars did not shop at their closest supermarket but at a preferred store farther away that they could reach by car. Furthermore, we did not adjust for physical activity or sleep duration, which could confound our change in BMI z-score results. Because we conducted this study in Massachusetts, where nearly all children have health care insurance, results may not be generalizable to uninsured populations.
Conclusions
Proximity to large supermarkets was an effect modifier of changes in BMI z-score and fruit and vegetable intake in a cluster-randomized, obesity intervention, further highlighting that access to healthy food is an important factor in reducing the risk of childhood obesity. Future public health efforts could explicitly examine children’s environments and target interventions to take advantage of families’ proximity to supermarkets or seek ways to help families who do not have readily available supermarkets. Policymakers and community leaders should continue to look for creative ways to improve families’ access to healthy foods, including incentives for building supermarkets in low-income areas and decreasing the cost of fruit and vegetables.
ACKNOWLEDGMENTS
This study was supported by the Harvard Clinical and Translational Science Center (grant UL1 RR 025758) and the American Recovery and Reinvestment Act (grant R18 AE000026). L. Fiechtner was supported by the National Institute of Diabetes and Digestive and Kidney Diseases (training grant 2T32DK007477-31A1). J. Block was supported by the National Institutes of Health (career development award K23HL111211-01A1). E. R. Cheng was supported by a Eunice Kennedy Shriver National Institute of Child Health and Human Development training grant (1T32HD075727-02) to the Harvard-Wide Pediatric Health Services Research Fellowship.
An abstract of this article was published as part of the proceedings of the 2014 Annual Meeting of the Pediatric Academic Societies; May 3, 2014; Vancouver, Canada.
HUMAN PARTICIPANT PROTECTION
The Harvard Vanguard institutional review board approved the study protocol, and we obtained written informed consent from participants.
Footnotes
See also Galea and Vaughan, p. 394.
REFERENCES
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lamichhane AP, Mayer-Davis EJ, Puett R, Bottai M, Porter DE, Liese AD. Associations of built food environment with dietary intake among youth with diabetes. J Nutr Educ Behav. 2012;44(3):217–224. doi: 10.1016/j.jneb.2011.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Skidmore P, Welch A, van Sluijs E et al. Impact of neighbourhood food environment on food consumption in children aged 9–10 years in the UK SPEEDY (Sport, Physical Activity and Eating behaviour: Environmental Determinants in Young people) study. Public Health Nutr. 2010;13(7):1022–1030. doi: 10.1017/S1368980009992035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Powell LM, Auld MC, Chaloupka FJ, O’Malley PM, Johnston LD. Associations between access to food stores and adolescent body mass index. Am J Prev Med. 2007;33(4 suppl):S301–S307. doi: 10.1016/j.amepre.2007.07.007. [DOI] [PubMed] [Google Scholar]
- 5.Morland K, Diez Roux AV, Wing S. Supermarkets, other food stores, and obesity: the Atherosclerosis Risk in Communities study. Am J Prev Med. 2006;30(4):333–339. doi: 10.1016/j.amepre.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Recommended community strategies and measurements to prevent obesity in the United States. MMWR. Recomm Rep. 2009;58(RR–7):1–26. [PubMed] [Google Scholar]
- 7.The White House. Childhood obesity task force unveils action plan: solving the problem of childhood obesity within a generation. 2010. Available at: https://www.whitehouse.gov/the-press-office/childhood-obesity-task-force-unveils-action-plan-solving-problem-childhood-obesity-. Accessed April 21, 2015.
- 8.US Department of Agriculture. Food deserts. Available at: https://apps.ams.usda.gov/fooddeserts/foodDeserts.aspx. Accessed July 21, 2014.
- 9.Taveras EM, Marshall R, Horan CM et al. Rationale and design of the STAR randomized controlled trial to accelerate adoption of childhood obesity comparative effectiveness research. Contemp Clin Trials. 2013;34(1):101–108. doi: 10.1016/j.cct.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 10.Taveras EM, Marshall R, Kleinman KP et al. Comparative effectiveness of childhood obesity interventions in pediatric primary care: a cluster-randomized clinical trial. JAMA Pediatr. 2015;169(6):535–542. doi: 10.1001/jamapediatrics.2015.0182. [DOI] [PubMed] [Google Scholar]
- 11.Taveras EM, Marshall R, Horan CM et al. Improving children’s obesity-related health care quality: process outcomes of a cluster-randomized controlled trial. Obesity (Silver Spring) 2014;22(1):27–31. doi: 10.1002/oby.20612. [DOI] [PubMed] [Google Scholar]
- 12.Kuczmarski RJ, Ogden CL, Guo SS et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat 11. 2002;246:1–190. [PubMed] [Google Scholar]
- 13.Spear BA, Barlow SE, Ervin C et al. Recommendations for treatment of child and adolescent overweight and obesity. Pediatrics. 2007;120(suppl 4):S254–S288. doi: 10.1542/peds.2007-2329F. [DOI] [PubMed] [Google Scholar]
- 14.Resnicow K, DiIorio C, Soet JE, Ernst D, Borrelli B, Hecht J. Motivational interviewing in health promotion: it sounds like something is changing. Health Psychol. 2002;21(5):444–451. [PubMed] [Google Scholar]
- 15.Blum RE, Wei EK, Rockett HR et al. Validation of a food frequency questionnaire in Native American and Caucasian children 1 to 5 years of age. Matern Child Health J. 1999;3(3):167–172. doi: 10.1023/a:1022350023163. [DOI] [PubMed] [Google Scholar]
- 16.Wen X, Gillman MW, Rifas-Shiman SL, Sherry B, Kleinman K, Taveras EM. Decreasing prevalence of obesity among young children in Massachusetts from 2004 to 2008. Pediatrics. 2012;129(5):823–831. doi: 10.1542/peds.2011-1833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.US Census Bureau. North American industry classification system. 2014. Available at: https://www.census.gov/eos/www/naics. Accessed August 25, 2014.
- 18.Murray DM, Varnell SP, Blitstein JL. Design and analysis of group-randomized trials: a review of recent methodological developments. Am J Public Health. 2004;94(3):423–432. doi: 10.2105/ajph.94.3.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.US Census Bureau. Massachusetts quick facts. 2014. Available at: http://quickfacts.census.gov/qfd/states/25000.html. Accessed June 19, 2014.
- 20.Children’s Hospital of Philadelphia. Pediatric z-score calculator. Available at: http://stokes.chop.edu/web/zscore/result.php. Accessed August 25, 2014.
- 21.Epstein LH, Raja S, Daniel TO et al. The built environment moderates effects of family-based childhood obesity treatment over 2 years. Ann Behav Med. 2012;44(2):248–258. doi: 10.1007/s12160-012-9383-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kerr J, Norman GJ, Adams MA et al. Do neighborhood environments moderate the effect of physical activity lifestyle interventions in adults? Health Place. 2010;16(5):903–908. doi: 10.1016/j.healthplace.2010.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zenk SN, Lachance LL, Schulz AJ, Mentz G, Kannan S, Ridella W. Neighborhood retail food environment and fruit and vegetable intake in a multiethnic urban population. Am J Health Promot. 2009;23(4):255–264. doi: 10.4278/ajhp.071204127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rose D, Richards R. Food store access and household fruit and vegetable use among participants in the US Food Stamp Program. Public Health Nutr. 2004;7(8):1081–1088. doi: 10.1079/PHN2004648. [DOI] [PubMed] [Google Scholar]
- 25.Zenk SN, Schulz AJ, Hollis-Neely T et al. Fruit and vegetable intake in African Americans income and store characteristics. Am J Prev Med. 2005;29(1):1–9. doi: 10.1016/j.amepre.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 26.Azagba S, Sharaf MF. Fruit and vegetable consumption and body mass index: a quantile regression approach. J Prim Care Community Health. 2012;3(3):210–220. doi: 10.1177/2150131911434206. [DOI] [PubMed] [Google Scholar]
- 27.Leahy KE, Birch LL, Fisher JO, Rolls BJ. Reductions in entrée energy density increase children’s vegetable intake and reduce energy intake. Obesity (Silver Spring) 2008;16(7):1559–1565. doi: 10.1038/oby.2008.257. [DOI] [PubMed] [Google Scholar]
- 28.Morrissey TW, Jacknowitz A, Vinopal K. Local food prices and their associations with children’s weight and food security. Pediatrics. 2014;133(3):422–430. doi: 10.1542/peds.2013-1963. [DOI] [PubMed] [Google Scholar]
- 29.Millichamp A, Gallegos D. Comparing the availability, price, variety and quality of fruits and vegetables across retail outlets and by area-level socio-economic position. Public Health Nutr. 2013;16(1):171–178. doi: 10.1017/S1368980012000766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Han E, Powell LM, Zenk SN, Rimkus L, Ohri-Vachaspati P, Chaloupka FJ. Classification bias in commercial business lists for retail food stores in the US. Int J Behav Nutr Phys Act. 2012;9:46. doi: 10.1186/1479-5868-9-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Aggarwal A, Cook AJ, Jiao J et al. Access to supermarkets and fruit and vegetable consumption. Am J Public Health. 2014;104(5):917–923. doi: 10.2105/AJPH.2013.301763. [DOI] [PMC free article] [PubMed] [Google Scholar]