Abstract
Objectives. To examine pharmacy-based influenza vaccination using diffusion of innovation theory.
Methods. We used 1993 to 2013 Behavioral Risk Factor Surveillance System data to generate weighted prevalence rates of influenza vaccination, stratified by age (18–64 years vs ≥ 65 years) and state of residence. The diffusion of innovation theory adopter categories were residents of states allowing pharmacist vaccination before 1996 (“innovator/early adopters”), between 1996 and 1998 (“early majority”), between 1999 and 2004 (“late majority”), and in 2007 or later (“laggards”).
Results. For adults aged 18 to 64 years, vaccination rates were similar before the innovation (1993), diverged as the innovation reached the majority (2003), and were significantly lower for laggard states by 2013. Younger adults’ vaccination rates steadily increased from 12% to 16% in 1993 to 29% to 36% in 2013. For older adults, there was no significant difference in vaccination rates between adopter categories in any year and no advantage associated with adoption category.
Conclusions. Key features of pharmacy-based vaccination, including relative advantage and compatibility, are most relevant to younger adults; different interventions are warranted for older adults.
Seasonal influenza carries a public health burden of more than $87 billion per year, accounting for work absenteeism, outpatient visits, hospitalization, and mortality.1 Prevention strategies, including vaccinations, can dramatically reduce the burden of this disease.2 Efforts to increase rates of influenza vaccination among community-dwelling adults are especially effective when they use nonphysician vaccination providers.3
In 1996, the Pharmacy-Based Vaccination Program began training pharmacists to provide vaccinations in the community; by 2009, all US states allowed pharmacists to vaccinate against influenza.4,5 In an analysis of 16 states in 1995 and 1999, influenza vaccination rates were seen to be significantly higher in states that allowed pharmacists to vaccinate.6 We extended this analysis with more recent data from all US states, using diffusion of innovation—a conceptual framework for modeling how an innovative service, in this case pharmacist-delivered vaccination, spreads over time.7,8 Diffusion of innovation suggests a difference between early adopters and late adopters in early stages but less difference over time as the innovation spreads to the majority.9
METHODS
We obtained data from the 1993, 1998, 2003, 2008, and 2013 Behavioral Risk Factor Surveillance System, a nationally representative telephone survey. We weighted prevalence rates of influenza vaccination to account for the complex survey design.10 We then stratified these rates by age group (18–64 years vs ≥ 65 years) and state-level pharmacy vaccination adopter status on the basis of diffusion of innovation adopter categories and the year that each state allowed pharmacists to provide influenza vaccinations.6,9,11 “Innovator/early adopters” are residents of states that allowed pharmacist vaccination before 1996; “early majority” could receive pharmacist vaccination starting between 1996 and 1998, “late majority” between 1999 and 2004, and “laggards” in 2007 or later. We conducted our analyses using SAS version 9.3 (SAS Institute, Cary, NC).
RESULTS
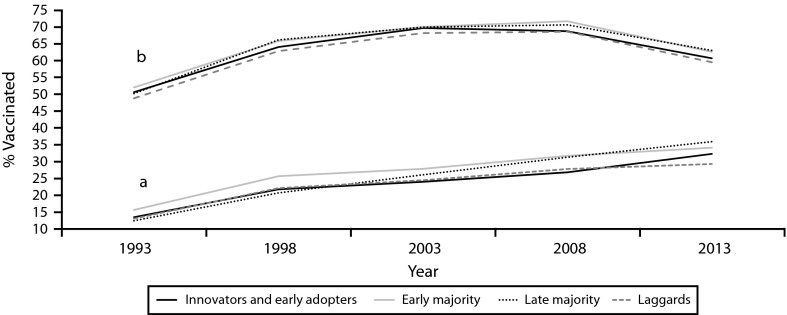
For adults aged 18 to 64 years, vaccination rates were similar before the innovation (1993), diverged as the innovation reached the majority (2003), and were significantly lower for laggard states by 2013 (Figure 1a). Younger adults’ vaccination rates steadily increased from 12% to 16% in 1993 to 29% to 36% in 2013. For older adults, there was no significant difference in vaccination rates between adopter categories in any year (Figure 1b). For younger adults, 95% confidence intervals showed significant differences between early and late majority versus others in 2008 and between all groups in 2013. Older adults’ vaccination rates increased from 49% to 52% in 1993 to 69% to 72% in 2008 and then decreased to 60% to 63% by 2013. For older adults, 95% confidence intervals for each group overlapped in all years.
FIGURE 1—
Influenza Vaccination Rates Over 20 Years in 5-Year Intervals for (a) Adults Aged 18–64 Years and (b) Adults Aged 65 Years and Older: Behavioral Risk Factor Surveillance System, United States, 1993–2013
Note. “Innovators and early adopters” indicates states that allowed pharmacist vaccination before 1996 (AL, CA, CO, GA, IL, MI, MT, SC, WA). “Early majority” indicates states that began to allow pharmacist vaccination in 1996 to 1998 (AK, AR, ID, KS, KY, MS, ND, NE, NM, OK, SD, TN, TX, VA, WI). “Late majority” indicates states that began to allow pharmacist vaccination in 1999 to 2004 (DE, HI, IA, IN, LA, MA, MD, MN, MO, NC, NJ, NV, OH, OR, PA, UT, WY). “Laggards” indicates states that began to allow pharmacist vaccination in 2007 or later (AZ, CT, FL, ME, NH, NY, RI, VT, WV).
DISCUSSION
After almost 2 decades, the innovation of pharmacy-based influenza vaccination is associated with distinct patterns in vaccination rates by adopter categories; younger residents of the last states to adopt the innovation report lower vaccination rates than do earlier adopting states. Although vaccination rates have increased, they still fall short of Centers for Disease Control and Prevention goals. Interventions to increase vaccination coverage broaden options, increase demand, and overcome barriers.12 Relevant interventions include the Affordable Care Act; patient, community, and provider education and outreach; and vaccination clinics in workplaces, schools, and pharmacies. One of those interventions, pharmacist vaccination, increases access by allowing people to receive a vaccination, often covered by health insurance, during a trip to their pharmacy or grocery store without an appointment. Pharmacists can further increase access with outreach to underserved populations that primarily seek vaccination at physician offices.13
Patterns reflecting diffusion of innovation were apparent for younger adults but not older adults. This may be because older adults were urged to receive vaccination stemming from high risk before 199314 and were not affected by the interventions. Characteristics that increase the rate of diffusion of innovation, such as compatibility with needs and relative advantage over traditional delivery, are more likely to appeal to younger adults seeking convenient preventive health services. Decreasing vaccination rates for older adults after 2008 are consistent with published rates showing a slight decrease and fluctuation since 2009,15 when the H1N1 pandemic scare occurred. However, vaccination rates for younger adults increased steadily throughout the period that pharmacy-based immunization were adopted,4 suggesting that innovative interventions to improve access to preventive care may be especially useful when targeted to this age group.
HUMAN PARTICIPANT PROTECTION
The institutional review board at the University of the Sciences in Philadelphia approved this analysis of publicly available de-identified data.
REFERENCES
- 1.Molinari NA, Ortega-Sanchez IR, Messonnier ML et al. The annual impact of seasonal influenza in the US: measuring disease burden and costs. Vaccine. 2007;25(27):5086–5096. doi: 10.1016/j.vaccine.2007.03.046. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Estimated influenza illnesses and hospitalizations averted by vaccination—United States, 2013–14 influenza season. MMWR Morb Mortal Wkly Rep. 2014;63(49):1151–1154. [PMC free article] [PubMed] [Google Scholar]
- 3.Lau D, Hu J, Majumdar SR, Storie DA, Rees SE, Johnson JA. Interventions to improve influenza and pneumococcal vaccination rates among community-dwelling adults: a systematic review and meta-analysis. Ann Fam Med. 2012;10(6):538–546. doi: 10.1370/afm.1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hogue MD, Grabenstein JD, Foster SL, Rothholz MC. Pharmacist involvement with immunizations: a decade of professional advancement. J Am Pharm Assoc. 2006;46(2):168–179. doi: 10.1331/154434506776180621. [DOI] [PubMed] [Google Scholar]
- 5.Traynor K. With Maine on board, pharmacists in all 50 states can vaccinate: H1N1 prompts emergency vaccination rules for pharmacists. Am J Health Syst Pharm. 2009;66(21):1892–1894. doi: 10.2146/news090081. [DOI] [PubMed] [Google Scholar]
- 6.Steyer TE, Ragucci KR, Pearson WS, Mainous AG., 3rd The role of pharmacists in the delivery of influenza vaccinations. Vaccine. 2004;22(8):1001–1006. doi: 10.1016/j.vaccine.2003.08.045. [DOI] [PubMed] [Google Scholar]
- 7.Greenberg MR. The diffusion of public health innovations. Am J Public Health. 2006;96(2):209–210. doi: 10.2105/AJPH.2005.078360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rogers EM. Diffusion of Innovations. 5th ed. New York, NY: Free Press; 2003. [Google Scholar]
- 9.DiClemente RJ, Salazar LF, Crosby RA. Health Behavior Theory for Public Health: Principles, Foundations, and Applications. Burlington, MA: Jones & Bartlett Learning; 2013. [Google Scholar]
- 10.Chen X, Gorrell P. An introduction to the SAS survey analysis PROCs. Available at: http://www.lexjansen.com/nesug/nesug08/sa/sa06.pdf. Accessed September 29, 2015.
- 11.American Pharmacists Association. Pharmacist authority to administer influenza vaccine—number of states authorizing pharmacist-delivered influenza vaccine vs. number of pharmacists trained to do so. 2015. Available at: http://www.pharmacist.com/sites/default/files/files/Pharmacist_IZ_Authority_toadmin_2_12_15.pdf. Accessed September 29, 2015.
- 12.Stinchfield PK. Practice-proven interventions to increase vaccination rates and broaden the immunization season. Am J Med. 2008;121(7) suppl 2:S11–S21. doi: 10.1016/j.amjmed.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 13.Uscher-Pines L, Maurer J, Harris KM. Racial and ethnic disparities in uptake and location of vaccination for 2009-H1N1 and seasonal influenza. Am J Public Health. 2011;101(7):1252–1255. doi: 10.2105/AJPH.2011.300133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention. Update on adult immunization. Recommendations of the Immunization Practices Advisory Committee (ACIP) MMWR Recomm Rep. 1991;40(RR-12):1–94. [PubMed] [Google Scholar]
- 15.Lu PJ, Singleton JA, Euler GL, Williams WW, Bridges CB. Seasonal influenza vaccination coverage among adult populations in the United States, 2005–2011. Am J Epidemiol. 2013;178(9):1478–1487. doi: 10.1093/aje/kwt158. [DOI] [PMC free article] [PubMed] [Google Scholar]