Abstract
Objectives. To examine rates at which people suffering medical emergencies on public streets receive help from bystanders, that is, laypersons who first arrive on the scene, and how this varies across patient race and incident locations.
Methods. We analyzed data on 22 487 patients from the 2011 National Emergency Medical Services Information System, which we linked to characteristics of counties where the incidents occurred.
Results. Bystanders provided help to patients suffering a wide range of medical emergencies, but only about 1 in 39 patients (2.57%) received bystander support. Black patients were significantly less likely to receive bystander support (odds ratio = 0.42; 95% confidence interval = 0.35, 0.50). Bystander support and county socioeconomic status have a curvilinear relationship; patients in the most disadvantaged counties are least likely to receive bystander support.
Conclusions. Help from bystanders is rare and less likely among Black patients and those in the poorest counties.
Each year, Americans make approximately 36 million calls for emergency medical services (EMS).1 Laypersons are often the first to arrive at medical emergencies in public places, and help they provide can improve patient outcomes.2 For example, bystander-performed cardiopulmonary resuscitation doubles the chance of survival from cardiac arrest.3 Bystanders can also perform the Heimlich maneuver, apply pressure to a wound, attach a splint, rinse a patient’s skin, or assist with medications. These actions stem from basic first aid training,2 whereas other forms of support, such as providing water, a blanket, or a cold compress, require no training at all.
Previous research estimates that about a quarter of cardiac arrest patients in the United States receive bystander cardiopulmonary resuscitation. Rates are lower among those with less income or education, racial/ethnic minorities, and those in socioeconomically disadvantaged neighborhoods.4 Disparities in the availability of cardiopulmonary resuscitation training programs contribute to these patterns.5 However, less is known about the distribution of forms of bystander support that do not require specialized training.
Social scientific research suggests that bystanders’ willingness to provide help may be shaped by the context in which a crisis occurs. According to the “bystander effect,” the presence of multiple bystanders leads to a diffusion of responsibility that reduces helping.6 Localized socioeconomic disadvantage may also erode trust, social cohesion, and informal control among residents, leading to a lack of collective efficacy7 and, potentially, reluctance to help others during a crisis.8
We extend research on community responses to medical emergencies by examining the availability of bystander support across a wide range of patient conditions and locations. We used multistate data from the National Emergency Management Information Systems (NEMSIS) to examine rates at which patients suffering medical emergencies on public streets receive bystander support. We also considered how such support varies across patient race and across population density and socioeconomic disadvantage in incident locations.
METHODS
The 2011 NEMSIS data set includes 185 480 adult patients who suffered non–traffic-related medical emergencies on public streets and sidewalks in 33 states.9 EMS providers indicated whether patients received help from a bystander before EMS arrival. EMS providers also noted patient symptoms and racial/ethnic background. Because of the underrepresentation of Hispanic patients, we focused on Black and White patients.
We drew a case–cohort subsample retaining all patients who received bystander support (n = 1900) and a random 11.2% sample of patients who did not (n = 20 587). This afforded a 10 to 1 ratio of nonbystander support cases to bystander support cases in all of our analyses. For each case in the subsample, NEMSIS staff linked selected characteristics of incident counties from the 2010 US Census and 2007–2011 American Community Surveys.
We assessed population density using the county’s decile ranking of population per square mile in the 2010 US Census. To capture localized socioeconomic disadvantage, we combined county decile rankings from the 2007–2011 American Community Surveys for median household income, education levels, and poverty. These items load on 1 factor (eigenvalue = 2.8; all loadings > 0.76) with excellent reliability (Cronbach α = 0.90). We calculated factor regression scores in SDs, weighting each item by its factor loading. (Summary statistics are available in Tables A and B, available as a supplement to the online version of this article at http://www.ajph.org.) We conducted statistical analyses using Stata version 13 (StataCorp LP, College Station, TX).
RESULTS
In the NEMSIS data, 1 in 39 patients (2.57%) who suffered medical emergencies on public streets received bystander support. Consistent with research on bystander cardiopulmonary resuscitation, 22.68% of patients with cardiac arrest received bystander support.4,10 However, most (80.22%) of the patients who received bystander support suffered noncardiac symptoms, such as bleeding or a wound from a traumatic injury, seizure, fainting, and respiratory issues (Table B).
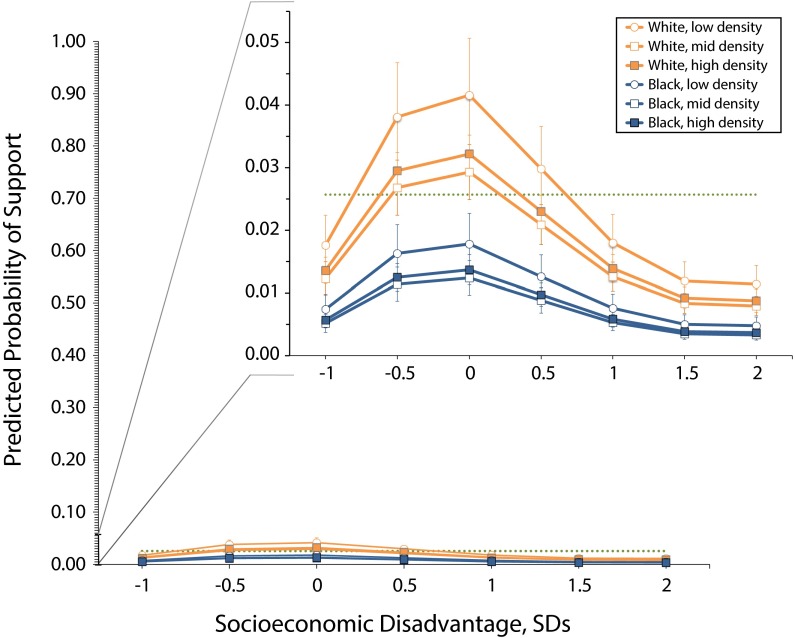
Figure 1 presents predicted probabilities of bystander support, which we calculated from weighted logistic regression models, across patient race and incident county characteristics (Table C, available as a supplement to the online version of this article at http://www.ajph.org). Black patients are about 57% less likely than are White patients to receive bystander support (odds ratio = 0.42; 95% confidence interval = 0.35, 0.50; predicted probabilities: 0.018 for Black patients; 0.042 for White patients). Black patients are significantly less likely than are White patients to receive bystander support across all incident contexts.
FIGURE 1—
Probability of Receiving Bystander Support, by Patient Race and Population Density and Socioeconomic Disadvantage Within the Incident County: National Emergency Medical Services Information System, United States, 2011
Within racial groups, patients in counties with low population densities are most likely to receive help. Variation in bystander support across population densities is not as wide as is that across levels of socioeconomic disadvantage. Patients in the most disadvantaged counties are least likely to receive help from a bystander.
When combined, patient race and local socioeconomic disadvantage create substantial disparities in access to bystander support. About 1 in 30 White patients (3.22%) in high-density counties with average socioeconomic levels receive bystander support, compared with about 1 in 260 Black patients (0.38%) in high-density, socioeconomically disadvantaged counties.
DISCUSSION
We found that bystanders help patients who are suffering a wide range of medical emergencies, including but not limited to cardiac arrest. However, bystander support is rare. In the NEMSIS data, only about 1 in 39 patients (2.57%) on public streets receive help from a bystander.
Strikingly, Black patients are less than half as likely as are White patients to receive bystander support. We found that this disparity is not attributable to socioeconomic differences across incident counties. However, it is possible that residential segregation concentrates Black patients in neighborhoods lacking services and institutions, which may reduce bystander support.10 Disparities in bystander support may also stem from racial biases that shape how Black individuals are perceived in public spaces.
Experimental research suggests that implicit bias reduces prosocial behavior toward Black individuals and underlies racial disparities in police officers’ use of force.11 Further research should consider how residential segregation and racial bias may contribute to lower rates of bystander support for Black patients, leaving them to wait longer for help.
Consistent with models of the bystander effect, rates of bystander support are highest among patients in low-density areas.6 However, differences across county levels of socioeconomic disadvantage are more pronounced. Lower rates of bystander support among patients in disadvantaged counties may reflect a lack of first aid training in poor communities,5 but many forms of bystander support require no training. Another possibility is that the social organization of incident contexts shapes bystanders’ willingness to provide help.
Sociological research suggests that community-level socioeconomic disadvantage weakens social bonds, erodes trust, and limits informal control within communities—all of which reduce collective efficacy and may contribute to a local normative orientation that discourages support and concern for others.7,8 Concentrated poverty and crime also precipitate distrust and fear,12 which may lead people to avoid interactions with strangers. Exploring how local social processes shape behavior during crises such as medical emergencies and disasters is an important direction for further research.
We acknowledge several limitations of this study. First, while the NEMSIS sample is large, it is not nationally representative; we could not estimate national rates of bystander support. Second, Hispanic patients are underrepresented in the data, which may reflect state-level differences in NEMSIS participation, EMS providers’ errors in coding Hispanic ethnicity, or lower rates of EMS activation among Hispanic patients. Finally, the incident county is the smallest geographic unit for which NEMSIS could provide information.9
To our knowledge, this study is the first to consider rates of generalized bystander support during medical emergencies. We found that bystander support is rare and unequally distributed, with lower rates for Black patients and those in socioeconomically disadvantaged areas. We urge further research on racial bias and community social contexts in the provision of bystander support. Inequalities in bystander support across millions of medical emergencies each year in the United States may contribute to persistent racial and socioeconomic disparities in health.
ACKNOWLEDGMENTS
We thank N. Clay Mann and Mengtao Dai at the National Emergency Medical Services Information System (NEMSIS) Technical Assistance Center for their assistance with the NEMSIS data. We are also grateful to Benjamin Cornwell, Oliver Jacob, Kim Weeden, and participants in the Cornell Center for the Study of Inequality Workshop for comments during the development of this article.
The National Highway Traffic Safety Administration (NHTSA) collects and maintains the NEMSIS database. The content reproduced from the NEMSIS database remains the property of NHTSA. The NHTSA is not responsible for any claims arising from works on the basis of the original data, text, tables, or figures.
HUMAN PARTICIPANT PROTECTION
This study did not require institutional review board approval because it involved secondary analysis of existing, publicly available data that cannot be linked to identifiable individuals.
REFERENCES
- 1.Federal Interagency Committee on Emergency Medical Services. National EMS assessment. 2012. Available at: https://www.nasemso.org/documents/National_EMS_Assessment_Final_Draft_12202011.pdf. Accessed June 5, 2015.
- 2.Markenson D, Ferguson JD, Chameides L et al. Part 17: first aid: 2010 American Heart Association and American Red Cross guidelines for first aid. Circulation. 2010;122(18) suppl 3:S934–S946. doi: 10.1161/CIRCULATIONAHA.110.971150. [DOI] [PubMed] [Google Scholar]
- 3.Hasselqvist-Ax I, Riva G, Herlitz J et al. Early cardiopulmonary resuscitation in out-of-hospital cardiac arrest. N Engl J Med. 2015;372(24):2307–2315. doi: 10.1056/NEJMoa1405796. [DOI] [PubMed] [Google Scholar]
- 4.Sasson C, Magid DJ, Chan P et al. Association of neighborhood characteristics with bystander-initiated CPR. N Engl J Med. 2012;367(17):1607–1615. doi: 10.1056/NEJMoa1110700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sasson C, Meischke M, Abella BS et al. Increasing cardiopulmonary resuscitation provision in communities with low bystander cardiopulmonary resuscitation rates: a science advisory from the American Heart Association for healthcare providers, policymakers, public health departments, and community leaders. Circulation. 2013;127(12):1342–1350. doi: 10.1161/CIR.0b013e318288b4dd. [DOI] [PubMed] [Google Scholar]
- 6.Fischer P, Krueger JI, Greitemeyer T et al. The bystander-effect: a meta-analytic review on bystander intervention in dangerous and not-dangerous emergencies. Psychol Bull. 2011;137(4):517–537. doi: 10.1037/a0023304. [DOI] [PubMed] [Google Scholar]
- 7.Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: a multilevel study of collective efficacy. Science. 1997;277(5328):918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- 8.Browning CR, Feinberg SL, Wallace D, Cagney KA. Neighborhood social processes, physical conditions, and disaster-related mortality: the case of the 1995 Chicago heat wave. Am Sociol Rev. 2006;71(4):661–678. [Google Scholar]
- 9.NEMSIS Technical Assistance Center. National EMS Database: NEMSIS Research Data Set v. 2.2.1 2011 User Manual. Washington, DC: National Highway Traffic Safety Administration; 2012. [Google Scholar]
- 10.Iwashyna TJ, Christakis NA, Becker LB. Neighborhoods matter: a population-based study of provision of cardiopulmonary resuscitation. Ann Emerg Med. 1999;34(4):459–468. doi: 10.1016/s0196-0644(99)80047-x. [DOI] [PubMed] [Google Scholar]
- 11.Banks RB, Eberhardt JL, Ross L. Discrimination and implicit bias in a racially unequal society. Calif Law Rev. 2006;94(4):1169–1190. [Google Scholar]
- 12.Ross CE, Mirowsky J, Pribesh S. Powerlessness and the amplification of threat: neighborhood disadvantage, disorder, and mistrust. Am Sociol Rev. 2001;66(4):568–591. [Google Scholar]