Abstract
Objectives. To evaluate African American–White differences in medical debt among older adults and the extent to which economic and health factors explained these.
Methods. We used nationally representative data from the 2007 and 2010 US Health Tracking Household Survey (n = 5838) and computed population-based estimates of medical debt attributable to economic and health factors with adjustment for age, gender, marital status, and education.
Results. African Americans had 2.6 times higher odds of medical debt (odds ratio = 2.62; 95% confidence interval = 1.85, 3.72) than did Whites. Health status explained 22.8% of the observed disparity, and income and insurance explained 19.4%. These factors combined explained 42.4% of the observed disparity. In addition, African Americans were more likely to be contacted by a collection agency and to borrow money because of medical debt, whereas Whites were more likely to use savings.
Conclusions. African Americans incur substantial medical debt compared with Whites, and more than 40% of this is mediated by health status, income, and insurance disparities.
Public health implications. In Medicare, low-income beneficiaries, especially low-income African Americans with poor health status, should be protected from the unintended financial consequences of cost-reduction strategies.
Medical debt—personal debt incurred from health care costs—is a substantial and increasing problem among older Americans, especially African Americans.1,2 Older adults incur medical debt because of high health care needs from multiple chronic conditions and limited financial resources to pay out-of-pocket costs.1,2 According to 2007 data from the Commonwealth Fund Biennial Health Insurance Survey, approximately 1 in 5 low-income older adults had problems paying medical bills or medical debt in the past 12 months.3 Even older adults in the highest income households have been found to experience significant medical debt problems.1,2
Few studies have examined why medical debt may disproportionately occur among older African Americans. Yet, this is an important problem for several reasons. First, older African Americans are particularly vulnerable to medical debt problems because they tend to be in poorer health, to have higher out-of-pocket expenses, and to have fewer financial resources than their White counterparts.2 Low-income African American adults typically qualify for both Medicare and Medicaid coverage, which should alleviate out-of-pocket spending for health care.1,2 However, many low-income African American Medicare beneficiaries are not covered by Medicaid because of the burden of the eligibility and enrollment process, and lack of awareness about eligibility.1 Finally, older African American adults also experience financial barriers to care from a combination of economic and social factors such as working in racially segregated, low-wage jobs that offer no retiree health benefits.4 As a result, avoidance of medical services and nonadherence to prescribed medications because of costs are more prevalent among older African Americans than they are among older Whites, resulting in a reliance on high-cost services when care is finally sought.4,5
Medical debt captures unpredictable and unavoidable trade-offs or choices that individuals make between medical care spending and other household spending (e.g., paying utilities, buying food, paying mortgage or rent) to address serious health needs.6 But the magnitude and distribution of medical debt and related financial consequences between African Americans and Whites is unclear. Moreover, we lack an understanding of how economic and health status factors may explain medical debt disparities. Therefore, we addressed the following questions: (1) What is the prevalence of medical debt among older African Americans and Whites? (2) What proportion of the observed racial/ethnic disparity in medical debt is accounted for by economic measures after control for self-rated health status and other covariates? (3) What proportion of the observed racial/ethnic disparity in medical debt is accounted for by differing self-rated health status after control for economic factors and other covariates? (4) How do the financial consequences of medical debt differ among older African Americans and Whites? Lessons learned from asking these questions may inform policy on health care affordability for a large and growing proportion of our aging population.4
METHODS
We drew the cross-sectional data for our analyses from the 2007 and 2010 Health Tracking Household Survey (HTHS), previously known as the Community Tracking Study Household Survey.7 The HTHS is a nationally representative, telephone-administered survey of civilian, noninstitutionalized individuals grouped into family insurance units (FIUs). The FIU includes an adult household member, spouse, and dependent children aged up to 18 years. The HTHS collects information on access to care, health care experiences, health expenses and bills, insurance coverage, health status, and sociodemographic characteristics. The 2007 HTHS consisted of 17 797 individuals from 9407 FIUs, and the 2010 HTHS consisted of 16 671 individuals from 9165 FIUs. Detailed descriptions of the HTHS and documentation are available from the Health and Medical Care Archives (http://www.icpsr.umich.edu/HMCA) and have been published elsewhere.7 Data from multiple rounds may be combined to increase sample size and to calculate a single “pooled” estimate.8 The pooled sample of adults who were aged at least 65 years included 3261 individuals from 2007 and 3076 from 2010. We restricted our sample to non-Hispanic Whites and African Americans aged 65 years or older (n = 5838).
Dependent and Independent Variables
The dependent variables of interest were a dichotomous variable assessing medical debt and 5 dichotomous variables indicating self-reported financial consequences of medical debt. The HTHS used the following question to assess medical debt: “During the past 12 months, have you or has your family had any problems paying medical bills?” If an individual reported “yes” to having problems paying medical bills, they were asked the following questions (categorized as financial consequences of medical debt):
Because of problems paying medical bills during the past 12 months, have you and your family [question 1] been contacted by a collection agency; [question 2] had problems paying for other necessities; [question 3] put off major purchases, such as a new car; [question 4] had to take money out of savings; or [question 5] had to borrow money?
All responses were coded as yes or no. All respondents reporting medical debt experienced at least 1 financial consequence.
The main independent variable of interest was race/ethnicity (non-Hispanic White, African American, both mutually exclusive). The proposed mediators were economic (income and insurance) and health status. We categorized income level as a percentage of the federal poverty level (based on the 2002 and 2007 US Census Bureau poverty guidelines for the size of the Census family given)7,8 as low (0%–199%), medium (200%–399%), or high (≥ 400%). “Low” indicates less income and more poverty, whereas “high” indicates more income and less poverty. We assessed insurance type as Medicare only, Medicare and public insurance, and Medicare and private coverage. Therefore, we coded this variable so that greater values indicated better insurance status. These economic measures enable purchase of health services and are highly amenable to social or policy changes.9 We categorized perceived health status, assessed on a 5-point scale, as (1) poor or fair, (2) good, and (3) very good or excellent, with greater coded values indicating better health. Other covariates included age (continuous), gender (male or female), marital status (single or married), and education level (less than high school, high school, some college, or college and above). We included these covariates because of their association with health care utilization and outcomes.2,5,9
Statistical Analysis
We first examined data distributions and descriptive summaries. Bivariate analyses compared older African Americans and Whites on all study variables. To account for complex survey characteristics, we based statistical significance on the Pearson χ2 test with the Rao and Scott second-order correction for categorical variables and the t test with the robust variance estimator (continuous variables).10,11 Next, we used logistic regression—adjusted for age, gender, marital status, and education—to assess the relationship between race/ethnicity and medical debt. We used odds ratios (ORs), confidence intervals (CIs), and P values to characterize associations. We used the c-statistic to assess how well the model can discriminate between people who reported having medical debt from those who did not have medical debt.12
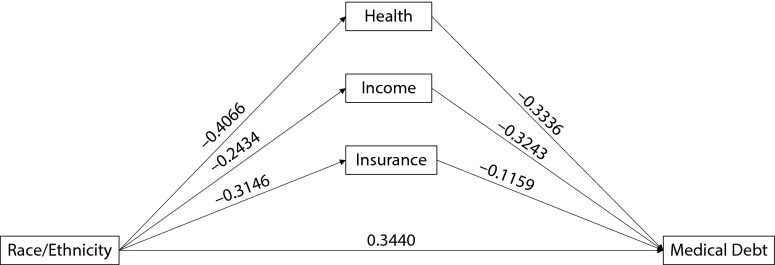
We performed mediation analysis according to approaches outlined by MacKinnon.13 For this analysis, we postulated that race/ethnicity leads to problems with medical debt through 3 indirect (mediated) pathways and a direct pathway. The mediators for the 3 indirect pathways were health status, income level, and insurance status, with each cast as a 3-level ordinal variable. These paths are depicted in the mediation diagram in Figure 1.
FIGURE 1—
Proposed Mediation Pathways Linking African American Race/Ethnicity With Medical Debt: 2007 and 2010 US Health Tracking Household Survey, Respondents Aged 65 Years or Older
Note. All standardized path coefficients are adjusted for age, gender, marital status, and education.
We adjusted the main mediation models for age, gender, marital status, and education. We also ran the mediation models without marital status and education. Because the outcomes for the mediation equations were dichotomous or ordinal, we standardized path coefficients to account for the variance of the assumed underlying latent outcome.14 We accomplished maximum likelihood estimation with mean-variance adaptive quadrature,15 by using the generalized structural equation modeling module of Stata version 14.1 (StataCorp LP, College Station, TX). We calculated the total contribution of each path as the product of the path coefficients. We calculated mediated proportions as the ratio of a specific path contribution (or combination of paths) to the total contribution of all paths. Therefore, the mediated proportion approximately represented the proportion of the total effect of the independent variable that was transmitted through the mediator16 after we considered covariates in the model. We generated CIs based on linear approximation from a Taylor expansion.17 In addition, we developed separate mediation models within each of the 3 strata of income.
Finally, we performed logistic regression analyses to assess how the 5 financial consequences of medical debt (i.e., been contacted by a collection agency, had problems paying for other necessities, put off major purchases, had to take money out of savings, and had to borrow money) differed among older Whites and African Americans. We adjusted all regression models for age, gender, marital status, and education. To facilitate more intuitive comparison based on these logistic regression models, adjusted percentages (i.e., model-adjusted risks) and standard errors directly contrasted the financial consequences of medical debt between Whites and African Americans.18 We considered all results statistically significant at P ≤ .05.
We conducted all statistical analysis with Stata version 14, which is designed to analyze complex sample survey data like those of the HTHS.7 Sampling weights provided with the HTHS represent the total US civilian noninstitutionalized population with adjustments for oversampling and nonresponse.
RESULTS
Table 1 summarizes the characteristics of our study sample and population. Approximately 9% of the sample was African American. More African Americans than Whites had low income, Medicare-only insurance, and poor or fair health status. Approximately 7.1% of Whites had medical debt versus 21.4% of African Americans. Table 2 shows results from the logistic regression model assessing self-reported medical debt. After adjustment for age, gender, marital status, and education, older African Americans had 2.6 times higher odds of having medical debt than did Whites (OR = 2.62; 95% CI = 1.85, 3.72). Increasing age and increasing education were associated with lower odds of medical debt.
TABLE 1—
Characteristics of Study Sample and Population by Race/Ethnicity: 2007 and 2010 US Health Tracking Household Survey, Respondents Aged 65 Years and Older
| Weighted %a (SE) or Mean ±SE |
|||
| Characteristic | Total (n = 66 019 000) | White (n = 59 832 575) | African American (n = 6 186 426) |
| Gender | |||
| Male | 43.1 (0.65) | 43.9 (0.68) | 34.9 (2.43) |
| Female | 56.9 (0.65) | 56.1 (0.68) | 65.1 (2.43) |
| Married | |||
| Yes | 60.4 (1.04) | 63.1 (1.07) | 34.6 (3.28) |
| No | 39.6 (1.04) | 36.9 (1.07) | 65.4 (3.28) |
| Education level | |||
| < high school | 18.1 (0.83) | 16.1 (0.84) | 37.1 (3.00) |
| High school | 35.3 (0.91) | 35.5 (0.96) | 32.6 (2.52) |
| Some college | 22.4 (0.82) | 23.0 (0.87) | 17.2 (2.22) |
| ≥ college | 24.2 (0.85) | 25.3 (0.90) | 13.0 (1.68) |
| Income level | |||
| Low (0%–199% FPLb) | 30.7 (0.99) | 28.1 (1.00) | 55.8 (3.11) |
| Medium (200%–399% FPL) | 33.0 (1.05) | 34.6 (1.12) | 18.3 (2.01) |
| High (≥ 400% FPL) | 36.3 (1.09) | 37.4 (1.16) | 26.0 (2.63) |
| Insurance | |||
| Medicare only | 15.2 (0.80) | 14.2 (0.84) | 24.4 (2.57) |
| Medicare and public insurance | 10.0 (0.62) | 9.1 (0.63) | 19.7 (2.55) |
| Medicare and private insurance | 74.8 (0.95) | 76.7 (0.99) | 55.9 (2.97) |
| Perceived health status | |||
| Poor or fair | 25.9 (0.84) | 23.9 (0.85) | 45.6 (2.88) |
| Good | 30.3 (0.86) | 30.4 (0.94) | 29.0 (2.47) |
| Very good or excellent | 43.8 (0.95) | 45.7 (1.01) | 25.4 (2.22) |
| Medical debt | |||
| No | 91.5 (0.61) | 92.9 (0.62) | 78.6 (2.43) |
| Yes | 8.5 (0.61) | 7.1 (0.62) | 21.4 (2.43) |
| Age, y | 74.0 ±0.13 | 74.1 ±0.14 | 73.8 ±0.38 |
Percentages may not add to 100 because of rounding.
FPL = federal poverty level based on the 2002 US Census Bureau poverty level for the size of the census family given.7,8
TABLE 2—
Adjusted Odd Ratios and 95% Confidence Intervals for Having Medical Debt: 2007 and 2010 US Health Tracking Household Survey, Respondents Aged 65 Years or Older
| Characteristic | Medical Debt, %a (95% CI) | OR (95% CI) |
| Race/ethnicity | ||
| African American | 21.4 (17.0, 26.5) | 2.62 (1.85, 3.72) |
| White | 7.1 (6.0, 8.4) | 1 (Ref) |
| Gender | ||
| Female | 8.6 (7.2, 10.2) | 0.81 (0.64, 1.03) |
| Male | 8.4 (7.1, 9.9) | 1 (Ref) |
| Age | . . . | 0.96 (0.93, 0.98) |
| Marital status | ||
| Not married | 9.9 (8.2, 11.9) | 1.38 (0.96, 1.98) |
| Married | 7.5 (6.1, 9.2) | 1 (Ref) |
| Education level | ||
| < high school | 13.8 (10.8, 17.4) | 2.95 (1.74, 5.00) |
| High school | 8.9 (7.1, 11.0) | 1.85 (1.17, 2.94) |
| Some college | 8.1 (5.9, 11.0) | 1.57 (0.93, 2.66) |
| ≥ college | 4.2 (3.0, 5.9) | 1 (Ref) |
Note. CI = confidence interval; OR = odds ratio. Unweighted n = 5838; weighted n = 66 019 000. The relationship between race/ethnicity and problems paying medical bills was only adjusted for gender, age, marital status, and education. C-statistic (area under the receiver-operating-characteristic curve) = 0.683.
Percentages for medical debt are unadjusted.
Table 3 shows the results from the analysis exploring the contribution of economic and health status factors to the observed disparity in medical debt. Together, economic factors explained 19.4% of the medical debt disparity between African Americans and Whites, with income being more important than insurance status. Health factors explained 22.8% of the disparity. Combined, economic and health factors explained 42.2% of the racial/ethnic disparity in medical debt. Omitting education and marital status as confounders slightly increased the mediated effect, but did not substantively alter the findings. In stratified analyses, the proportion of medical debt disparity explained by health status was 31.1% (95% CI = 8.8%, 53.5%) for those in the lowest income category, 24.8% (95% CI = 9.9%, 39.6%) for those in the middle income category, and 12.0% (95% CI = 0.0%, 25.5%) for those in the highest income category.
TABLE 3—
Percentage of Disparity in Medical Debt Problems for African Americans and Whites Explained by Health and Economic Factors: 2007 and 2010 US Health Tracking Household Survey, Respondents Aged 65 Years and Older
| Variable | Percentage Explained (95% CI)a | Percentage Explained (95% CI)b |
| Health | 22.8 (14.1, 31.5) | 23.5 (15.9, 31.1) |
| Economic factors | ||
| Income | 13.3 (4.5, 22.1) | 23.0 (14.0, 31.9) |
| Insurance | 6.1 (0.9, 11.4) | 8.0 (1.5, 14.4) |
| Subtotal explained by economic factors | 19.4 (8.6, 30.2) | 30.9 (19.8, 42.0) |
| Total proportion explained | 42.2 (27.2, 57.1) | 54.4 (40.3, 68.5) |
Note. CI = confidence interval. Unweighted n = 5838; weighted n = 66 019 000. Income, insurance, and health were coded as 3-level variables.
Models were adjusted for age, gender, marital status, and education.
Models were adjusted for age and gender.
Among those with medical debt (n = 453), 38.3% were contacted by a collection agency, 42.9% put off major purchases, 57.9% used savings, 33.9% borrowed money, and 59.6% had difficulty paying for necessities (results not shown). More African Americans than Whites were contacted by a collection agency (61.4% vs 31.1%; P < .001) and borrowed money (52.4% vs 28.2%; P = <.001), whereas more Whites than African Americans used savings (63.5% vs 39.8%; P = .002) because of medical debt (results not shown). Because of medical debt, older African Americans had significantly higher rates than older Whites had of being contacted by a collection agency (56.7% vs 32.3%; P ≤ .001) and borrowing money (50.4% vs 28.6%; P = .001). Older Whites had a significantly higher rate than older African Americans had of using savings because of medical debt (62.1% vs 44.7%; P = .018). Figure A, available as a supplement to the online version of this article at http://www.ajph.org, shows the adjusted percentages (i.e., model-adjusted risks) for the financial consequences of medical debt.
DISCUSSION
We found that older African Americans had a higher (2.6 times) prevalence of problems paying medical bills than did older Whites. Perceived health status explained about 35% of the racial/ethnic disparity in problems paying medical bills, and economic factors explained an additional 39%. We also found that older African Americans were more likely than were Whites to be contacted by a collection agency and to borrow money, whereas older Whites were more likely to use savings because of medical bill problems.
These results suggest that older African Americans incur substantial medical debt because they lack the income or insurance coverage to pay for needed medical care. The income gap between African Americans and Whites is a well-documented and persistent issue across the lifespan.19 Many older adults live on low or modest incomes, but older African Americans are almost 3 times more likely to live in poverty than are their White counterparts.2 Income inequality has been linked to a variety of adverse health and health care outcomes.19 Although low-income African Americans may be dually covered by Medicare and Medicaid, states’ variation in Medicaid benefit packages leaves many dual beneficiaries with burdensome out-of-pocket costs, which can greatly press budgets of older adults on fixed incomes and with other financial obligations.1,2 As out-of-pocket expenses continue to rise and older adults face the prospect of shrinking income,20 medical debt represents a major threat to the economic security of older African Americans. Although the 2010 Affordable Care Act will reduce the financial burden of medical care on older adults by closing the “doughnut hole” in Medicare Part D, African Americans—who need and have to use more health services because of poor health—will continue to incur considerable medical debt because of out-of-pocket costs for deductibles and copayments.
We also found that increasing age was associated with less medical debt. On first consideration, this finding may appear to be paradoxical because it is well recognized that medical expenditures increase with age and, on average, peak near time of death.21 However, in this context, it is important to note that all respondents in our sample were at aged 65 years or older and, therefore, potentially eligible for Medicare. We suspect that enrollment in Medicare resulted in a substantial decrease in the acquisition of new debt and also provided an opportunity to pay down existing debt. It is reasonable to assume that this effect could begin after enrollment and continue to accumulate with passing years. Although African Americans have, on average, shorter life expectancies than Whites,22 we do not suspect that the age-related decline in medical debt results from a depletion of African Americans from our sample. In support of this assertion, we note that the racial/ethnic composition of our sample remained remarkably constant with age. Furthermore, the finding of an age-related decline in medical debt persisted in subanalyses for both African Americans and Whites. Nonetheless, the age-related decline in medical debt is an interesting finding and warrants further study.
Income, insurance, and health status are interrelated factors that influence health care disparities23; these factors combined explained 42% of the African American–White disparity. We suspect that the impact of economic factors was not fully captured because our measures did not consider the broader construct of wealth. A robust body of research supports the link between self-reported health status and health care utilization and cost,24 which may lead to increased medical debt, especially in the setting of low resources. This is consistent with our finding that the explanatory power of health for medical debt disparity was greater for those in lower income categories.
Previous research has documented that medical debt is associated with forgoing and rationing needed medical care,2,3,6,25,26 adverse health outcomes,27 and medical bankruptcy.28 It is contended that Americans make financial trade-offs with other goods and services because of medical debt. Consistent with these studies, we found that older adults with medical debt experience serious financial consequences (i.e., debt collection, problems paying for necessities, putting off major purchases, using savings, and borrowing money). There were statistically significant differences between African Americans and Whites on being contacted by a collection agency, borrowing money, and using savings. Older African Americans experience more debt collection hassle. Racial/ethnic minorities have been found in other studies to disproportionately experience aggressive and unfair debt collection practices.26 In keeping with the well-described income and wealth differences,2,29 older African Americans borrow money, whereas older Whites use savings to pay medical bills.
Limitations
Although this study makes an important contribution to the literature on medical debt among older African American and White adults, our findings should be considered in light of the study’s limitations. First, data were cross-sectional, which precludes causal inferences. Cross-sectional data may also provide biased estimates of mediation effects.30 Second, data were self-reported and thus subject to recall and other forms of self-report bias.31 However, basing the query on recent events as an anchor point, as in our survey, decreases cognition errors of forgetting, fabrication, and telescoping.32
Third, self-rated health is a broad measure that captures aspects of mental and physical health, and can be biased by social desirability, individuals’ expectations, and relative deprivation.33 However, self-rated health is well-validated as a strong predictor of mortality and has been found to be associated with chronic and specific serious conditions including cancer and diabetes.34 Fourth, it is also possible that there is an inverse relationship between self-rated health status and medical debt; that is, medical debt leads to poor health and vice versa. Establishing this bidirectional link would require contextual factors including timing and duration of medical debt. Some individuals experience problems paying medical bills within the past year, are gradually paying off medical bills, or have longstanding bills that they are unable to pay,25 which we were unable to assess.
Finally, we lacked an adequate measure of wealth, which consists of accumulated assets in addition to income.29 Wealth has been shown to be associated with self-reported health status, chronic conditions, and mortality.35 Control for factors such as wealth, credit card debt, debt counseling, or debt management services might have enhanced our ability to account for the race effect in medical bill problems.25
Conclusions
Medical debt is a significant source of financial distress among older adults, particularly African Americans. Medicare plays an important role in alleviating financial burden, but it does not cover all medical care costs.2 Policymakers have proposed changes to Medicare (including increasing beneficiary premiums and cost sharing, and reducing provider payment levels) to reduce the national debt and maintain Medicare solvency.20 But cost-cutting strategies that may burden White Medicare beneficiaries may cause catastrophic hardships for minority beneficiaries. Although changes are necessary to sustain Medicare for the future,20 policymakers need to explicitly consider the impact that cost-cutting strategies will have on African American beneficiaries.
ACKNOWLEDGMENTS
This research was funded by the Robert Wood Johnson Foundation New Connections Program under grant 70289 and was partially supported by a grant from the National Institute of Minority Health and Health Disparities (1 P60 MD006912-02).
HUMAN PARTICIPANT PROTECTION
This research involved public-use data and was deemed exempt from review by the University of South Florida institutional review board.
REFERENCES
- 1.Komisar H, Cubanski J, Dawson L, Neuman T. Key issues in understanding the economics and health security of current and future generations of seniors. Kaiser Family Foundation Medicare Policy. 2012. Available at: https://kaiserfamilyfoundation.files.wordpress.com/2013/01/8289.pdf. Accessed November 11, 2014.
- 2.Cubanski J, Swoope C, Damico A, Neuman T. Health care on a budget: the financial burden of health spending by Medicare households. 2014. Available at: http://kff.org/medicare/issue-brief/health-care-on-a-budget-the-financial-burden-of-health-spending-by-medicare-households. Accessed May 14, 2014.
- 3.Doty MM, Collins SR, Rustgi SD, Kriss JL. Seeing red: the growing burden of medical bills and debt faced by U.S. families. Issue Brief (Commonw Fund) 2008;42:1–12. [PubMed] [Google Scholar]
- 4.Randall V. African Americans, nursing home care, and the law. In: Katz PR, Mezey MD, Kapp M, editors. Vulnerable Populations in the Long Term Care Continuum. Vol. 5. New York, NY: Springer Publishing Company Inc; 2004. pp. 73–97. [Google Scholar]
- 5.Mahmoudi E, Jensen GA. Exploring disparities in access to physician services among older adults: 2000–2007. J Gerontol B Psychol Sci Soc Sci. 2013;68(1):128–138. doi: 10.1093/geronb/gbs105. [DOI] [PubMed] [Google Scholar]
- 6.Cunningham PJ. Explaining the increase in family financial pressures from medical bills between 2003 and 2007: do affordability thresholds change over time? Med Care Res Rev. 2011;68(3):352–366. doi: 10.1177/1077558710378122. [DOI] [PubMed] [Google Scholar]
- 7.Strause R, Carlson B, Hall J, Cybulski K. Washington, DC: Center for Studying Health System Change; 2009. Community Tracking Study: Household Survey Methodology Report 2007 (Round Five) [Google Scholar]
- 8. 2010 Health Tracking Household Survey public use file: user’s guide (Release 1). Washington, DC: Center for Studying Health System Change; 2012. Report no. 83.
- 9.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1–10. [PubMed] [Google Scholar]
- 10.Sribney WM. Two-way contingency tables for survey or clustered data. Stata Tech Bull. 1998;45:33–49. [Google Scholar]
- 11.Rao JN, Wu C. Resampling inference with complex survey data. J Am Stat Assoc. 1988;83(401):231–241. [Google Scholar]
- 12.LaValley MP. Logistic regression. Circulation. 2008;117(18):2395–2399. doi: 10.1161/CIRCULATIONAHA.106.682658. [DOI] [PubMed] [Google Scholar]
- 13.MacKinnon DP. Introduction to Statistical Mediation Analysis. 103–125. New York, NY: Lawrence Erlbaum Associates; 2008. pp. 297–321. [Google Scholar]
- 14.MacKinnon DP, Dwyer JH. Estimating mediated effects in prevention studies. Eval Rev. 1993;17(2):144–158. [Google Scholar]
- 15.Rabe-Hesketh S, Skrondal A, Pickles A. Maximum likelihood estimation of limited and discrete dependent variable models with nested random effects. J Econom. 2005;128:301–323. [Google Scholar]
- 16.Hafeman DM. “Proportion explained”: a causal interpretation for standard measures of indirect effect? Am J Epidemiol. 2009;170(11):1443–1448. doi: 10.1093/aje/kwp283. [DOI] [PubMed] [Google Scholar]
- 17.Xu J, Long S. Confidence intervals for predicted outcomes in regression models for categorical outcomes. Stata J. 2005;5(4):537–559. [Google Scholar]
- 18.Graubard BI, Korn EL. Predictive margins with survey data. Biometrics. 1999;55(2):652–659. doi: 10.1111/j.0006-341x.1999.00652.x. [DOI] [PubMed] [Google Scholar]
- 19.Williams DR, Sternthal M. Understanding racial–ethnic disparities in health sociological contributions. J Health Soc Behav. 2010;51(1 suppl):S15–S27. doi: 10.1177/0022146510383838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Henry J Kaiser Family Foundation. Policy Options to Sustain Medicare for the Future. 2013. Available at: http://kaiserfamilyfoundation.files.wordpress.com/2013/02/8402.pdf. Accessed November 11, 2014. [Google Scholar]
- 21.Hoover DR, Crystal S, Kumar R, Sambamoorthi U, Cantor JC. Medical expenditures during the last year of life: findings from the 1992–1996 Medicare current beneficiary survey. Health Serv Res. 2002;37(6):1625–1642. doi: 10.1111/1475-6773.01113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Harper S, MacLehose RF, Kaufman JS. Trends in the Black-White life expectancy gap among US states, 1990–2009. Health Aff (Millwood) 2014;33(8):1375–1382. doi: 10.1377/hlthaff.2013.1273. [DOI] [PubMed] [Google Scholar]
- 23.Niewczyk PM, Lwebuga-Mukasa JS. Is poverty the main factor contributing to health care disparities? An investigation of individual level factors contributing to health care disparities. J Equity Health. 2008;1(1):22–40. [Google Scholar]
- 24.DeSalvo KB, Fan VS, McDonell MB, Fihn SD. Predicting mortality and healthcare utilization with a single question. Health Serv Res. 2005;40(4):1234–1246. doi: 10.1111/j.1475-6773.2005.00404.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pollitz K, Cox C, Lucia K, Keith K. Medical debt among people with health insurance. 2014. Available at: https://kaiserfamilyfoundation.files.wordpress.com/2014/01/8537-medical-debt-among-people-with-health-insurance.pdf. Accessed November 11, 2014.
- 26.Rukavina M, Haase LW, Kercheval J. Tarnish on the Golden State: how medical debt threatens family financial stability. 2011. Available at: https://static.newamerica.org/attachments/3738-tarnish-on-the-golden-state/Tarnish-on-the-Golden-State.e9f96c2b2cf54289adf63c8cf94f219e.pdf. Accessed November 11, 2014.
- 27.Rahimi AR, Spertus JA, Reid KJ, Bernheim SM, Krumholz HM. Financial barriers to health care and outcomes after acute myocardial infarction. JAMA. 2007;297(10):1063–1072. doi: 10.1001/jama.297.10.1063. [DOI] [PubMed] [Google Scholar]
- 28.Himmelstein DU, Thorne D, Woolhandler S. Medical bankruptcy in Massachusetts: has health reform made a difference? Am J Med. 2011;124(3):224–228. doi: 10.1016/j.amjmed.2010.11.009. [DOI] [PubMed] [Google Scholar]
- 29.Brown T. The intersection and accumulation of racial and gender inequality: Black women’s wealth trajectories. Rev Black Polit Econ. 2012;39(2):239–258. [Google Scholar]
- 30.Cole DA, Maxwell SE. Testing mediational models with longitudinal data: questions and tips in the use of structural equation modeling. J Abnorm Psychol. 2003;112(4):558–577. doi: 10.1037/0021-843X.112.4.558. [DOI] [PubMed] [Google Scholar]
- 31.Grimes DA, Schulz KF. Bias and causal associations in observational research. Lancet. 2002;359(9302):248–252. doi: 10.1016/S0140-6736(02)07451-2. [DOI] [PubMed] [Google Scholar]
- 32.Schmier JK, Halpern MT. Patient recall and recall bias of health state and health status. Expert Rev Pharmacoecon Outcomes Res. 2004;4(2):159–163. doi: 10.1586/14737167.4.2.159. [DOI] [PubMed] [Google Scholar]
- 33.Eriksson I, Unden AL, Elofsson S. Self-rated health. Comparisons between three different measures. Results from a population study. Int J Epidemiol. 2001;30(2):326–333. doi: 10.1093/ije/30.2.326. [DOI] [PubMed] [Google Scholar]
- 34.Manor O, Matthews S, Power C. Self-rated health and limiting longstanding illness: inter-relationships with morbidity in early adulthood. Int J Epidemiol. 2001;30(3):600–607. doi: 10.1093/ije/30.3.600. [DOI] [PubMed] [Google Scholar]
- 35.Pollack CE, Chideya S, Cubbin C, Williams B, Dekker M, Braveman P. Should health studies measure wealth? A systematic review. Am J Prev Med. 2007;33(3):250–264. doi: 10.1016/j.amepre.2007.04.033. [DOI] [PubMed] [Google Scholar]