Summary
Temporal lobe epilepsy (TLE) is typically described as a neurologic disorder affecting a cerebral network comprising the hippocampus proper and several anatomically related extrahippocampal regions. A new level of complexity was recently added to the study of this disorder by the evidence that TLE also appears to chronically alter the activity of several brain-wide neural networks involved in the control of higher order brain functions and not traditionally linked to epilepsy. Recently developed brain imaging techniques such as functional magnetic resonance imaging (fMRI) analysis of resting state connectivity, have greatly contributed to these observations by allowing the precise characterization of several brain networks with distinct functional signatures in the resting brain, and therefore also known as “resting state networks.” These significant advances in imaging represent an opportunity to investigate the still elusive origins of the disabling cognitive and psychiatric manifestations of TLE, and could have important implications for its pathophysiology and, perhaps, its therapy. Herein we review recent studies in this field by focusing on resting state networks that have been implicated in the pathophysiology of psychiatric disorders and cognitive impairment in patients with epilepsy: the default mode network, the attention network, and the reward/emotion network.
Keywords: Attention networks, Blood oxygenation level–dependent fMRI signals, Cognitive impairment, Default-mode network, Psychiatric complications, Reward/emotion network
Temporal lobe epilepsy (TLE) is the most common form of focal epilepsy in humans (Téllez-Zenteno & Hernández-Ronquillo, 2012). Two main forms of TLE were classically distinguished: mesial TLE (mTLE) where seizure activity was assumed to originate from a hippocampal or parahippocampal focus, and neocortical TLE (nTLE) where the epileptic focus is located in lateral temporal lobe neocortex (Kennedy & Schuele, 2012; Tatum, 2012). mTLE accounts for the majority of cases, whereas nTLE represents only about 10% of TLEs (Téllez-Zenteno & Hernández-Ronquillo, 2012). The traditional hypothesis that in focal epilepsies seizure activity originates in a specific, anatomically isolated epileptic focus has been subsided by a more complex view where “focal epileptic seizures are conceptualized as originating within networks limited to one hemisphere” (Berg et al., 2010). Most of this change in perspective derived from studies performed in mTLE. It was shown, indeed, that in this form of epilepsy, ictal and interictal discharges can originate from multiple distinct foci located not only in the hippocampus proper but also in extrahippocampal regions (Spencer & Spencer, 1994; Alarcon et al., 1997; Wendling et al., 1997; Chabardes et al., 1999; Spencer, 2002; Bartolomei et al., 2005, 2008). Electrocorticographic and neuroimaging studies in humans and experiments performed in animal models of TLE have thus led to the concept of a large mTLE network composed not only of the hippocampus but also of limbic structures (i.e., entorhinal and perirhinal cortices and the amygdala), subcortical regions such as the thalamus, and neocortical regions such as the frontal lobes, especially the orbitofrontal region, and the superior, mid, and inferior temporal gyri (Lieb et al., 1991; Spencer & Spencer, 1994; Avoli et al., 2002; Spencer, 2002; Bartolomei et al., 2005). Each of the brain structures included in this network has been found to originate epileptic discharges or contribute to their propagation (Bragin et al., 2000; Spencer, 2002; Briellmann et al., 2004). Therefore, although traditionally classified as a focal disorder, mTLE in fact involves large portions of the brain.
In recent years, evidence has been accumulating to suggest a much more complex scenario. A major breakthrough in the study of TLE has been the recent demonstration that it affects the spontaneous activity of a group of brain networks known as resting state networks. These networks have been identified in functional magnetic resonance imaging (fMRI) studies in normal subjects as discrete groups of brain structures showing a spontaneous synchronized activity that is evident at rest and is modulated during specific functional tasks. Available data strongly support the idea that resting state networks are involved in controlling higher order brain functions such as consciousness, cognition, affective behavior, or attention (Seeley et al., 2007; Buckner et al., 2008; Harrison et al., 2008; Sheline et al., 2010; van den Heuvel & Hulshoff Pol, 2010; Clemens et al., 2011). These networks include brain areas that are often far from the hippocampus proper and thus not traditionally considered as part of the TLE network.
The evidence that TLE affects resting state networks has important implications for understanding why TLE is often accompanied by an impairment of higher order brain functions that are dependent on the coordinated activity of multiple brain regions. Clinicians have known for decades that TLE symptoms are not necessarily “focal,” but psychiatric impairments in these patients have yet to be explained (see Table 1 for a recent classification of psychiatric disorders in epilepsy). TLE complications such as these occur frequently and may significantly impair the quality of life of patients with epilepsy (Gaitzis et al., 2004; Zeber et al., 2007). It has been estimated that 24–72% of patients with TLE have depressive/dysphoric symptoms and 10–19% may present with psychosis (Gaitzis et al., 2004; Nadkarni et al., 2007; Miller et al., 2008). Similarly, cognitive impairment is common in TLE, although precise data on its incidence are missing (Elger et al., 2004). This complication of epilepsy has been described both in adults and in pediatric patients, and often manifests itself as poor performance at school (Dodrill, 2002; Elger et al., 2004; Helmstaedter & Kockelmann, 2006; Gottlieb et al., 2012; Wilson et al., 2012). The concept of TLE as a resting state network disease opens a new perspective for the understanding of the psychiatric and cognitive complications of TLE and for their pharmacologic treatment. Herein we review the evidence of resting state network dysfunction in TLE, and recent data that suggest its involvement in cognitive and psychiatric complications occurring in this epileptic disorder. The majority of the studies that we review were performed in mTLE patients, but some of them evaluated heterogeneous groups composed of both mTLE and nTLE patients; in others no detailed information on the composition of TLE patient group is reported.
Table 1.
Classification of psychiatric disorders of epilepsy according to the proposal of the ILAE Commission on Psychobiology of Epilepsy (Krishnamoorthy et al., 2007, Epilepsy Behav 10:349–353)
| Clinical presentation | Difference from psychiatric disorders in nonepileptic patients | |
|---|---|---|
| Psychiatric comorbidity | Anxiety and phobic disorders; Minor and major depression; Obsessive compulsive disorder; Other somatoform, dissociative, and neurotic disorders. | Not different from the range of common mental disorders prevalent in the community and in clinic/hospital populations |
| Psychopathology as presenting symptom of epileptic seizures | Altered awareness, confusion, disorientation, memory disturbances, anxiety, dysphoria, hallucinations and paranoid syndromes. | Occurring as part of partial, simple partial and absence status |
| Interictal psychiatric disorders that are specific to epilepsy | Cognitive dysfunction including memory complaints. Psychoses of epilepsy may occur as interictal, postictal, or alternative. Significant affective component but little or no emotional flattening in the interictal form. Hallucination, paranoid delirium, and behavioral disturbances in the postictal or alternative forms. Affective somatoform “dysphoric” disorders (irritability, depressive moods, anergia, insomnia, atypical pains, anxiety, phobic fears, and euphoric moods); they may occur as prodromal, postictal, or interictal. Personality disorders (hyperethical, viscous, labile, mixed, and other). Anxiety and phobias specific to epilepsy. |
Disorders that are seen specifically in patients with epilepsy |
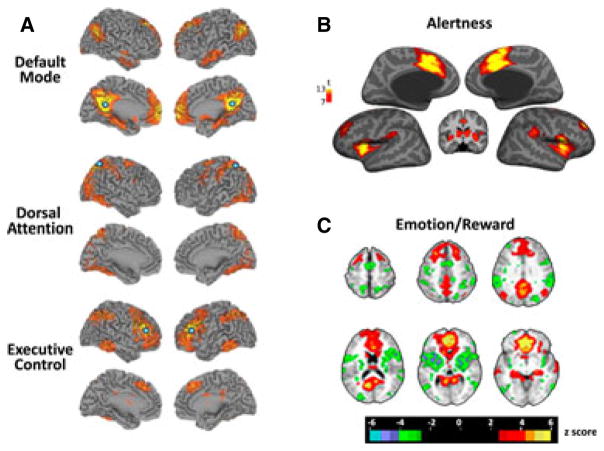
Resting State Networks in Normal and Epileptic Brain
The concept of resting state network originated from the seminal work of Biswal et al. (1995), who were investigating the source of noise in fMRI signals during a simple motor task. Using an experimental paradigm that alternated finger tapping and rest periods, they identified in motor cortex low frequency fluctuations of fMRI signal unrelated to heart beat or respiration. These fluctuations occurred at rest and showed a high degree of correlation, with similar fluctuations in contralateral motor cortex (Biswal et al., 1995; Biswal 2012). Similar coherent fluctuations were also observed in other functionally connected brain regions such as language and visual cortices and were interpreted as an indication of functional connectivity among distant brain regions active also at rest (Biswal, 2012). The fluctuations identified by Biswal et al. (1995) are caused by spontaneous changes in the blood oxygenation level–dependent (BOLD) signal. BOLD signal depends on the changes in the magnetic properties of oxygenated hemoglobin, and thus represents an index of oxygen- and blood flow–dependent neural and glial activity (van den Heuvel & Hulshoff Pol, 2010). Multiple regions show coherent BOLD fluctuations and therefore are believed to be functionally connected and form discrete resting state networks (Biswal et al., 1995; Fox et al., 2005; Damoiseaux et al., 2006; Sadaghiani et al., 2010; van den Heuvel & Hulshoff Pol, 2010; Tomasi & Volkow, 2011). Although resting state networks have been identified due to their activity at rest, they are also relevant for many other aspects of normal brain functioning. It appears that their activity is modulated by internal or external “stimuli.” For example, activation of the default mode network decreases in response to external stimuli, whereas the activity of the other resting state networks increases with similar cues (Fox et al., 2005; Buckner et al., 2008). Therefore, resting state networks can be classified on the basis of their response during different and specific behaviors, and may be subdivided into two groups (see Table 2). The first group includes networks involved in motor and sensory processes. They are the sensorimotor, the visual, and the auditory networks (Xiong et al., 1999; van den Heuvel & Hulshoff Pol, 2010). A second group is made of networks associated with higher order brain functions. Among them, there are the default mode network mentioned above, the dorsal and ventral attention networks, the salience network, the executive control network, the reward/emotion network, and the language networks (Protzner & McAndrews, 2011; Tomasi & Volkow, 2011; Li et al., 2013; Fig. 1). A certain degree of overlap does exist among different networks, as some brain regions belong to many networks. Although there is some evidence that networks involved in motor and sensory processes networks could be dysfunctional in TLE (Zhang et al., 2009a), here we focus on the group of networks that participates in higher order functions due to more widespread evidence of their involvement (see Table S1 for a schematic list of the main nodes of the resting state networks covered in this review).
Table 2.
The main resting state networks of the human brain
| Motor and sensory networks |
| Visual network |
| Auditory network |
| Sensorimotor network |
| Networks mediating higher brain functions |
| Default mode network |
| Attention networks |
| Dorsal attention network |
| Ventral attention network |
| Alertness network |
| Salience network |
| Executive control network |
| Reward emotion network |
| Language networks |
Figure 1.
Schematic representation of the main brain networks affected in TLE. (A) The figure shows connectivity maps of the default, dorsal attention, executive control (A), alertness (B), and reward emotion networks (C) in normal subjects. Connectivity in resting state networks can be quantified by measuring the strength of the correlation of BOLD signals in various portions of the brain in relation to a region of interest or “seed.” The seed regions used to extract the resting state networks shown in panel A are indicated as blue circles. The alertness (B) and the reward emotion networks (C) were identified using as seed regions the dorsal and the subgenual anterior cingulate cortex, respectively. The different colors used in each panel indicate different strength of correlation in BOLD fluctuations between specific brain regions and seed regions, according to the pseudocolor scales in the insets. Specifically, the pseudocolor bar in panel B indicates the values of t obtained in second level one-sample t-test analysis on contrast images corresponding to the seed regressors. The scale in panel C reports, instead, z-score values evaluated with the r to z Fisher transformation. Panels A–C are reproduced with permission from Woodward et al. (2011) Schizophr Res 130:86–93, Sadaghiani et al. (2010) J Neurosci 30:10243–10250, and Sheline et al. (2010) Proc Natl Acad Sci USA 107:11020–11025.
Epilepsia © ILAE
The hypothesis that TLE affects resting state networks is based on several converging lines of evidence. First, fMRI studies showed differences between patients with epilepsy and healthy controls in the spontaneous activity of specific nodes of these networks (Zhang et al., 2010a). Second, in mTLE, there is diffuse impairment in the functional connectivity in nodes of these networks, evaluated as decreased coherence in BOLD fluctuations (Liao et al., 2010; Fahoum et al., 2012). A third, indirect line of evidence is based on studies showing that structural damage may occur in resting network nodes or in the white matter bundles connecting them. Such damage may result from excitotoxicity and consequent sclerosis due to seizure activity (Bonilha et al., 2010a,b). This structural damage may partly account for the decrease in functional connectivity occurring in mTLE. It has been demonstrated, indeed, that functionally linked resting-state networks largely reflect the underlying structural, white matter connectivity architecture of the human brain (van den Heuvel et al., 2009), although functional connectivity can also be found among brain regions not directly connected by corticocortical fibers (Honey et al., 2009). Because the activity of a network is dependent on the functional interaction of its nodes, even small changes in connectivity may cause dysfunction in global brain networks. In TLE, there is the impairment not only of long range but also of short distance connectivity (van Dellen et al., 2009; Liao et al., 2010). Short distance connectivity is essential for the normal activity of the brain, particularly for cognition (Sporns & Zwi, 2004; Stam & Reijneveld, 2007). In keeping with this evidence, the severity of short distance connectivity impairment and the cognitive decline appear correlated in patients with TLE (Vlooswijk et al., 2011; Vaessen et al., 2012).
Abnormalities in the Default-Mode Network
The default-mode network (DMN) is composed of the medial prefrontal and medial, lateral, and inferior parietal cortices, the precuneus, and the cerebellum; it is still controversial whether the medial temporal lobe, including the hippocampus and the parahippocampal cortex, also belongs to this network (Damoiseaux et al., 2006; Buckner et al., 2008; Fransson & Marrelec, 2008; Table S1; Fig. 1A). The activity of the DMN increases during cognitive tasks, memory retrieval, envisioning the future, theory of mind (i.e., interpreting beliefs or intentions of other people), and expressing moral judgments (Buckner et al., 2008). Conversely, its activity is reduced in response to external challenges and during goal-oriented tasks. In TLE, the DMN alterations that have been described so far may result from the rich connections that exist between the hippocampus and several key structures of that network, such as the posterior cingulate cortex (important for memory retrieval) (Greicius et al., 2004; Buckner et al., 2008).
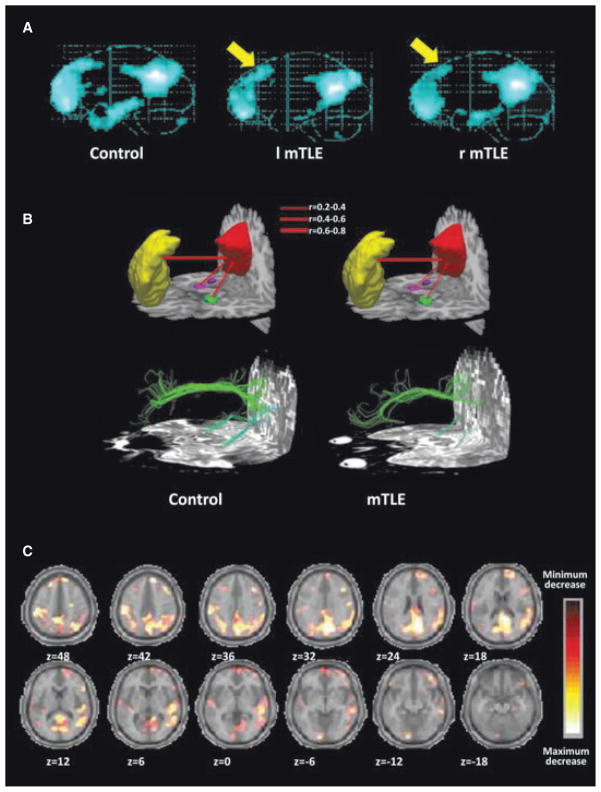
As shown in Fig. 2A, the overall area of activation of the DMN is reduced in mTLE patients, especially in the prefrontal cortex (Zhang et al., 2010b). Moreover, both the activity of the DMN and the functional connectivity of its nodes are decreased in mTLE as compared with healthy subjects (Liao et al., 2010, 2011; Fig. 2B), reflected as diminished coherence of the spontaneous BOLD fluctuations occurring in these brain structures. The mechanisms responsible for this decrease in connectivity are unknown but could result from accumulating structural damage due to seizures. This hypothesis is supported by evidence showing that the decrease in connectivity is proportional to both duration and severity of mTLE (Liao et al., 2010; Voets et al., 2012). In addition, studies performed with diffusion tensor imaging (DTI) demonstrated relevant damage in white matter bundles connecting the different DMN nodes (Liao et al., 2011; Fig. 2C). Finally, significant alterations in DMN connectivity were observed in mTLE patients with unilateral or bilateral hippocampal sclerosis (Zhang et al., 2010b; Pittau et al., 2012). Recently, Haneef et al. (2012) proposed that the most characteristic alteration of DMN in both left and right lateralized TLE was the loss of the functional connectivity between its anterior and posterior regions including the ventromedial prefrontal cortex and the precuneus, respectively. Although functional DMN connectivity is generally decreased in mTLE, few nodes are actually hyperconnected. This hyperconnectivity occurs, for instance, in the case of posterior cingulate cortex or right middle frontal gyrus (Zhang et al., 2010b; Pittau et al., 2012), and it may play a compensatory role for the loss of functional connections in other regions of the network. An alternative hypothesis to explain hyperconnectivity is “dynamic diaschisis,” that is, the change in functional properties occurring in anatomically remote brain regions after focal brain lesions (Price et al., 2001; Campo et al., 2012). Dynamic diaschisis is considered the consequence of disturbed integration among functionally connected brain regions and has been proposed already as an explanation of the hyperconnectivity between inferior frontal cortex and medial temporal lobe in the contralesional hemisphere of patients with in temporal lobe epilepsy and left hippocampal sclerosis (Campo et al., 2012).
Figure 2.
TLE affects activity and connectivity of the default mode network (DNM). (A) Comparison of the DMN in control subjects, and right and left TLE patients. The images represent the averages of DMN signals reconstructed from the analysis of BOLD coherent fluctuations, in 29 control subjects, 27 right and 25 left TLE patients. Note the significantly smaller areas of the dorsal medial prefrontal cortex, and of the mesial and inferior temporal lobe in TLE patients in comparison with controls. Reproduced with permission from Zhang et al. (2010b) Brain Res 1323:152–160. (B) The connectivity among different regions of the default mode network is lower in TLE than in normal subjects. The top of the panel reports a schematic representation of fMRI functional connectivity between precuneus/posterior cingulate cortex (in red) and medial prefrontal cortex (in yellow), right (in magenta), and left (green) mesial temporal cortex. Functional connectivity was evaluated measuring the correlation coefficients of BOLD fluctuations in the aforementioned regions. The different strengths of correlations are represented as different thickness of the segments connecting these regions as specified in the inset of panel. Note that the connectivity between precuneus/posterior cingulate cortex and both right and left temporal lobes is weaker in TLE patients than in controls. The bottom of the panel shows a DTI reconstruction of the white matter fiber bundles connecting the same regions. Note that the thickness of these fibers is reduced in TLE patients as compared with normal controls. Reproduced with permission from Liao et al. (2011), Hum Brain Mapp 32:883–895. (C) Areas of the brain where BOLD signal decreases during the propagation of interictal epileptic activity. The panel shows the mean decreases in BOLD signals recorded during interictal epileptic discharges in nine different patients with TLE undergoing simultaneous fMRI and EEG monitoring. The data were expressed in pseudocolor using an arbitrary scale, and projected as colored areas onto axial slices (Z coordinates given below each slice) of a template average brain. Reproduced with permission from Laufs et al. (2007), Hum Brain Mapp 28:1023–1032.
Epilepsia © ILAE
The DMN activity in patients with TLE is decreased by epileptic activity that causes DMN deactivation in a similar fashion to natural sensory stimulation. Electroencephalography (EEG)–fMRI studies performed by simultaneously recording BOLD and EEG signals showed that the activity of the DMN decreases simultaneously with appearance of interictal discharges on EEG (Kobayashi et al., 2006; Laufs et al., 2007; Fahoum et al., 2012; Fig. 1C). In particular, a significant decrease in BOLD signal was observed in posterior cingulate, precuneus, and left and right frontal and parietal lobes (Kobayashi et al., 2006; Laufs et al., 2007; Fahoum et al., 2012). Less information is available about the consequences of ictal discharges on DMN activity. The only available data derive from one single-photon emission computed tomography (SPECT) study that showed a decrease in blood perfusion in areas belonging to the DMN during ictal seizure activity (Blumenfeld et al., 2004). These data suggest that epileptic discharges may deactivate the DMN, but it remains to be firmly established how DMN responds to physiologic stimuli in patients with TLE. However, one study has shown that the DMN response to a visuospatial memory challenge was significantly lower in patients with TLE than in healthy controls (Frings et al., 2009).
Alterations in the physiologic activities controlled by DMN such as abstract thinking, cognitive tasks, or memory retrieval are observed in TLE as well as in other conditions such as Alzheimer’s disease, autism, and attention deficit/hyperactivity disorder (Broyd et al., 2009). In light of this evidence, it was posited that loss in DMN connectivity along with its recurrent deactivation by interictal discharges may have a role in decreasing the cognitive performance in patients with TLE (Laufs et al., 2007). This is further supported by findings suggesting that the degree of DMN impairment in these clinical settings is correlated with the severity of cognitive loss (Broyd et al., 2009; Miao et al., 2011; Binnewijzend et al., 2012; Brier et al., 2012). Due to the involvement of DMN in memory retrieval (Buckner et al., 2008; Spreng & Grady, 2010; McCormick et al., 2013), its dysfunction could also have a role in memory deficits commonly observed in TLE patients (Bell & Giovagnoli, 2007). Finally, recent evidence has demonstrated that the increase in connectivity that occurs in restricted DMN regions may have clinical implications in TLE, since temporo-prefrontal connectivity in the hemisphere with predominant seizure-onset activity is higher in psychotic than in nonpsychotic patients (Canuet et al., 2010, 2011a,b).
Abnormalities in the Activity of Attention Networks
When a human subject directs his attention toward the external world, the DMN systemically deactivates, whereas attention networks become active. This pattern of activity strongly suggests that these two systems operate in an opposing fashion in the human brain (Fox et al., 2005). The first system controls internally directed activities, such as introspective thought, whereas the second is responsible for responsiveness to the external world (Fox et al., 2005; Buckner et al., 2008). Two main attention networks have been identified: the ventral and the dorsal attention networks (Corbetta & Shulman, 2002; Fox et al., 2006). The dorsal attention network mediates the top-down attention, that is, the process in which the subject voluntarily directs his attention to a specific object during a cognitive task such as examining a specific aspect of a painting (Corbetta & Shulman, 2002). In contrast, the ventral attention network mediates bottom-up attention, that is, the attentive process triggered by sudden, unexpected sensory stimulations such as a ringing bell (Corbetta & Shulman, 2002). The likelihood of the attention networks being activated is regulated by another system known as the alertness network (Fan et al., 2005; Sadaghiani et al., 2010; Clemens et al., 2011; Petersen & Posner, 2012).
Changes in the ventral and dorsal attention networks as well as in the alertness network (see Fig. 1B and Table S1) have been described in TLE. For instance, Zhang et al. (2009b) showed that the functional connectivity of the different areas of the dorsal attention network during a top-down attention task is significantly lower in mTLE patients than in normal controls (see also Liao et al., 2010; Yang et al., 2010). Bocquillon et al. (2009) also reported evidence of a dysfunction of the ventral attention network in TLE patients by using high-density EEG recordings to compare the sources of P300 wave during an “oddball paradigm.” Source analysis showed a marked decrease in P300 sources in frontal and temporal areas of the patients, suggesting an impairment of the ventral attention network.
Recently, Zheng et al. (2012) reported dysfunction in the alertness network occurring in TLE patients. Specifically, they found that the overall area and intensity of BOLD responses to a specific alertness test were smaller in patients with TLE than in healthy controls (Zheng et al., 2012). It is important to note that the severity of the impairment of the alertness network correlated well with poor performance in the behavioral attention test. Functional connectivity among the different nodes of this network may also be impaired in TLE as demonstrated for the frontal lobe and right cerebellum (Yang et al., 2010). This evidence suggests that the impairment in attention networks might explain why patients with TLE often have worse performances than healthy controls in attention tests (Fleck et al., 2002; Stella & Maciel, 2003; Zheng et al., 2012).
Abnormalities in the Executive Control Network
The executive control network (see Fig. 1 and Table S1) is responsible for the control of executive functions (Seeley et al., 2007). This broad term encompasses diverse aspects in the execution of goal-directed behaviors including motor and ideational planning, initiation, and sequencing (Seeley et al., 2007). Both structural and functional abnormalities in the executive control network have been observed in TLE. For example, a significant thinning at voxel-based morphometry has been described in areas of this network including the ventrolateral and dorsolateral prefrontal cortices and frontal operculum (Seidenberg et al., 2005; Lin et al., 2008; McDonald et al., 2008; Riederer et al., 2008; Bernhardt et al., 2009, 2010; Bonilha et al., 2010a). In addition, the atrophy of several subcortical nuclei belonging to the executive control network including caudate and striatum was also observed (Dreifuss et al., 2001; Bouilleret et al., 2008). Evidence of impaired activity of the executive frontal network was first reported in 1997 by Jokeit et al., who reported a marked hypometabolism in prefrontal cortex at fluorodeoxyglucose–positron emission tomography (FDG-PET). More recently, Vlooswijk et al. (2011) found a reduction in functional connectivity at fMRI in the executive control network in patients with TLE showing impairment in working memory.
Impairments in problem-solving ability, in abstract reasoning, and in working memory capabilities are also frequently observed in patients with TLE (Martin et al., 2000). Although a role in the genesis of these symptoms has also been attributed to hippocampal damage, brain structures of the executive control network, such as the prefrontal cortex, may additionally be involved (Martin et al., 2000). Their participation in executive dysfunction of TLE is supported by the close correlation between the severity of network damage and the impairment of executive function. Specifically, Keller et al. (2009) demonstrated a linear relationship between the volume of the prefrontal cortex and the performance at the working memory component of the Wechsler Memory Scale test, and at the Controlled Oral Word Association Test (measuring verbal fluency). Moreover, in mTLE patients, the performance at the Wisconsin Card Sorting Test, a well-accepted measure of cognitive flexibility and adaptability (Heaton et al., 1993), seems to be related to the volume of the caudate (Riley et al., 2011). In the same study, the score in the Trail Making Test B, evaluating psychomotor speed and ability to manage parallel tasks (Kortte et al., 2002), was inversely related to the damage of white matter connections between prefrontal cortex and caudate measured with DTI (Riley et al., 2011). Finally, in patients with cryptogenic TLE, the decrease of functional connectivity measured with fMRI between the prefrontal cortex, anterior cingulate cortex, and inferior frontal gyrus correlated with the impairment of working memory evaluated with the Sternberg paradigm (Vlooswijk et al., 2011).
Executive dysfunction is characteristic of schizophrenia and is thought to be central to the disorganization of thought typical of psychosis (Boeker et al., 2006; Eisenberg & Berman, 2010). Based on these observations, it has been proposed that damage in the executive control network could be involved in the genesis of the so-called psychosis of epilepsy (Table 1). Canuet et al. (2010, 2011b) recently reported several arguments in support of this hypothesis. They performed magnetoencephalographic recordings during the execution of the Sternberg test in TLE patients with psychosis and found that the severity of both working memory impairment and psychotic symptoms correlated with magnetoencephalographic signs of prefrontal cortex dysfunction (Canuet et al., 2010, 2011b).
Abnormalities in the Reward/Emotion Network
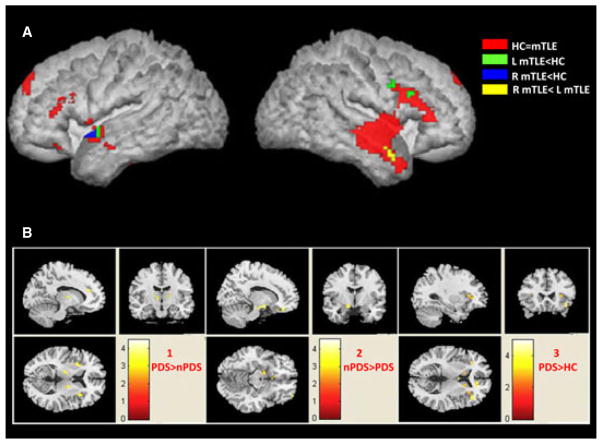
The reward-emotion network (see Fig. 1C and Table S1) controls mood, affective behavior and the response to emotional stimuli (Sheline et al., 2010; Tomasi & Volkow, 2011). Among resting state networks, the reward-emotion network is the one with the weakest spontaneous activity (Tomasi & Volkow, 2011). It can be, however, significantly activated by exposing the subject to emotional or motivational cues (Kinnison et al., 2012). The amygdala, which has a well-established role in the seizure genesis (Gloor, 1992, 1997), is the hub of this network that shows the largest potential overlap with the DMN (Sheline et al., 2010; Tomasi & Volkow, 2011). Voxel-based morphometry has shown changes in volume of the amygdala in TLE (Pitkänen et al., 1998), whereas BOLD fMRI showed higher resting activity in patients than in controls (Zhang et al., 2010a). In addition, a marked decrease in the functional connectivity of this region with the ventromedial prefrontal cortex was reported (Pittau et al., 2012). Not only basal but also evoked BOLD activity seems to be abnormal in mTLE. Indeed, in lateralized TLE, BOLD responses evoked in the amygdala by images of fearful faces are lower than normal ipsilaterally to the epileptic focus, especially if it is located in the right lobe (Meletti et al., 2003, 2009; Schacher et al., 2006a; Hlobil et al., 2008). Finally, the coactivation with amygdala of other nodes of the reward/emotion network is decreased in TLE patients as compared with normal controls (Broicher et al., 2012; Fig. 3A).
Figure 3.
TLE affects the reward/emotion network. (A) Areas coactivated with the amygdala in TLE patients and in healthy controls in response to the vision of fearful faces. The areas that coactivate with the amygdala in healthy controls (HC) are colored in red. They include left temporal pole, left inferior frontal gyrus, left superior medial frontal gyrus, left anterior cingulate cortex, left middle temporal gyrus, and right cerebellum. The regions showing less activation in left TLE patients are indicated in green (left hippocampus, left superior temporal gyrus, and right inferior frontal gyrus), whereas those showing less activation in right TLE are in blue (left hippocampus, left temporal pole, and left anterior cingulate cortex). The regions showing less activation in right than in left TLE are in yellow (right temporal pole, and left inferior frontal gyrus and right middle temporal gyrus). Reproduced from Broicher et al. (2012) J Neurol 259:2546–2554. (B) Differences in resting activity of the reward/emotion network in TLE patients with depressive symptoms (PDS), in TLE patients without depressive symptoms (nPDS), and in healthy controls (HC). The colored areas represent regions showing significant differences when performing a voxel-based comparison of the maps of low-frequency BOLD fluctuation amplitude between nPDS and PDS (panel 1 and 2) or HC and PDS (panel 3). Note that PDS have higher resting activity compared to nPDS in right anterior cingulate and in bilateral thalamus and insula (panel 1), whereas nPDS have higher resting activity compared to PDS in left amygdala and left medial prefrontal cortex (panel 2). The panels in 3 show that PDS have higher resting activity compared to HC in right anterior cingulate and bilateral caudate and insula. Reproduced with permission from Chen et al. (2012), Neuroimage 60:299–304.
Epilepsia © ILAE
mTLE is also typically associated with damage in the hippocampus and extrahippocampal regions. A rich literature on this issue exists and will not be examined here. The interested reader may find detailed information in recent extensive reviews (Malmgren & Thom, 2012; Ozkara & Aronica, 2012). Significant alterations in the functional connectivity between the hippocampus and prefrontal cortex have also been reported (Pittau et al., 2012). In TLE, a decreased gray matter volume was also observed at voxel-based morphometry in orbitofrontal cortex, another key node of the reward/emotion network that is richly connected with the amygdala (Barbas & De Olmos, 1990; Riederer et al., 2008).
The above-described alterations in reward/emotion network could have a role in causing some of the disturbances in the affective behavior reported to occur in TLE patients. A severe atrophy of the amygdala was observed in a subgroup of patients with intermittent explosive disorder, a condition consisting of paroxysmal episodes of violent aggression (Tebartz van Elst et al., 2000). The amygdala was also atrophic in TLE patients with ictal or postictal fear, anxiety, or frank panic (Cendes et al., 1994), but not in those with interictal psychosis of epilepsy where affective symptoms predominate (Tebartz Van Elst et al., 2002). The functional impairment of the amygdala could cause the aforementioned inappropriate social behavior by decreasing theory of mind abilities of the epileptic patient, that is, his ability to decode thoughts and behavior of other human beings (Schacher et al., 2006b). As mentioned above, the amygdala BOLD response to fearful faces is impaired in TLE (Meletti et al., 2003, 2009; Schacher et al., 2006a; Hlobil et al., 2008). Recently, Broicher et al. (2012) showed that this impairment in fear recognition strongly correlates with the poor performance in behavioral tests evaluating the theory of mind abilities.
An enlargement of the amygdala has been frequently observed in depressed patients with epilepsy, correlating with the severity of the disease (Richardson et al., 2007). In TLE patients with affective somatoform dysphoric disorder (Table 1) the volume of the amygdala is larger than normal when the depressive symptoms predominate, whereas it is smaller than average when aggressiveness and irritability are preponderant (Tebartz van Elst et al., 2009). As with major depression, the hippocampus is atrophic in TLE, and its atrophy seems to be particularly severe in epileptic patients with depression (Baxendale et al., 2005; Shamim et al., 2009; Kanner, 2011). A recent study showed that the orbitofrontal cortex that, as mentioned in the introduction, is one of the first propagation sites of mesial temporal epileptic discharges (Lieb et al., 1991), is thickened in depressed mTLE patients (Butler et al., 2012). Of interest, the severity of depression was linearly correlated with the thickness of this region (Butler et al., 2012). The hypothesis that the orbitofrontal cortex could be affected in depressed mTLE patients is consistent with the evidence of its marked hypometabolism at FDG-PET in these subjects (Bromfield et al., 1992; Salzberg et al., 2006). Moreover, fMRI connectivity analysis showed that in depressed mTLE patients, the functional connectivity between the anterior prefrontal cortex and the limbic system and the temporal cortex is significantly reduced in comparison to nondepressed mTLE patients and in healthy controls (Chen et al., 2012; Fig. 3B). Depressed mTLE patients also have altered resting activity of some nodes of the resting emotion/reward network and/or DMN. Specifically, the activity of the left amygdala and of left medial prefrontal cortex is lower, whereas that of bilateral caudate, thalamus, and insula, and of right anterior cingulate cortex is higher than in nondepressed TLE patients and in healthy controls (Chen et al., 2012; Fig. 3B).
Conclusions and Future Perspectives
The evidence reviewed here shows important differences in the activity of the major resting state networks in patients with TLE when compared to normal subjects. Remarkably, these differences are present interictally. These observations suggest that TLE modifies chronically the activity of brain networks that control basic functions such as attention, emotion, and cognition. This represents a major change in perspective from the classical view of TLE as a disease of a discrete set of structures involved in seizure generation and propagation. Most of the data reviewed here were made possible by advancement in functional brain imaging. In epileptology, as in many other fields of clinical neurology, fMRI is providing a new powerful tool to explore network activity in living patients. The information obtained with this technique can be combined with that of simultaneous high-resolution EEG, structural MRI, DTI, or magnetoencephalography. With this integrated approach, a through functional evaluation of brain function of the epileptic patients in absence of seizure activity is also possible. The evidence that TLE affects resting state network activity could help understanding of some of the clinical manifestations of TLE that are currently unexplained. As recently emphasized by Laufs (2012), who proposed a “network heuristic” of epilepsy, the involvement of large extratemporal networks could explain, for instance, the appearance of nonfocal symptoms in “focal” epilepsy or why the clinical presentation of epilepsy may be evolving with time as the pattern of the interested networks changes. Many of the studies reviewed here indicate that the dysfunction of resting state network could have a role in the genesis of the cognitive or psychiatric complications of TLE. This hypothesis, however, remains largely speculative. Its demonstration will require clinical studies designed to directly assess the correlation between the severity of these clinical conditions and resting state network impairment.
Acknowledgments
This work was supported by the CIHR Operating Grants 8109 and 74609 to M.A. and by the CIHR clinician scientist award 201009MC2-233335 to E.V.S.
Footnotes
Disclosure
None of the authors has any conflict of interest to disclose. We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Supporting Information
Additional Supporting Information may be found in the online version of this article:
Table S1. Nodes of the main resting state networks of the human brain.
References
- Alarcon G, Garcia Seoane JJ, Binnie CD, Martin Miguel MC, Juler J, Polkey CE, Elwes RD, Ortiz Blasco JM. Origin and propagation of interictal discharges in the acute electrocorticogram. Implications for pathophysiology and surgical treatment of temporal lobe epilepsy. Brain. 1997;120:2259–2282. doi: 10.1093/brain/120.12.2259. [DOI] [PubMed] [Google Scholar]
- Avoli M, D’Antuono M, Louvel J, Köhling R, Biagini G, Pumain R, D’Arcangelo G, Tancredi V. Network and pharmacological mechanisms leading to epileptiform synchronization in the limbic system in vitro. Prog Neurobiol. 2002;68:167–207. doi: 10.1016/s0301-0082(02)00077-1. [DOI] [PubMed] [Google Scholar]
- Barbas H, De Olmos J. Projections from the amygdala to basoventral and medio-dorsal prefrontal regions in the rhesus monkey. J Comp Neurol. 1990;300:549–571. doi: 10.1002/cne.903000409. [DOI] [PubMed] [Google Scholar]
- Bartolomei F, Khalil M, Wendling F, Sontheimer A, Regis J, Ranjeva JP, Guye M, Chauvel P. Entorhinal cortex involvement in human mesial temporal lobe epilepsy: an electrophysiologic and volumetric study. Epilepsia. 2005;46:677–687. doi: 10.1111/j.1528-1167.2005.43804.x. [DOI] [PubMed] [Google Scholar]
- Bartolomei F, Chauvel P, Wendling F. Epileptogenicity of brain structures in human temporal lobe epilepsy: a quantified study from intracerebral EEG. Brain. 2008;131:1818–1830. doi: 10.1093/brain/awn111. [DOI] [PubMed] [Google Scholar]
- Baxendale SA, Thompson PJ, Duncan JS. Epilepsy & depression: the effects of comorbidity on hippocampal volume-a pilot study. Seizure. 2005;14:435–438. doi: 10.1016/j.seizure.2005.07.003. [DOI] [PubMed] [Google Scholar]
- Bell BD, Giovagnoli AR. Recent innovative studies of memory in temporal lobe epilepsy. Neuropsychol Rev. 2007;17:455–476. doi: 10.1007/s11065-007-9049-3. [DOI] [PubMed] [Google Scholar]
- Berg AT, Berkovic SF, Brodie MJ, Buchhalter J, Cross JH, van Emde Boas W, Engel J, French J, Glauser TA, Mathern GW, Moshé SL, Nordli D, Plouin P, Scheffer IE. Revised terminology and concepts for organization of seizures and epilepsies: report of the ILAE Commission on Classification and Terminology, 2005–2009. Epilepsia. 2010;51:676–685. doi: 10.1111/j.1528-1167.2010.02522.x. [DOI] [PubMed] [Google Scholar]
- Bernhardt BC, Worsley KJ, Kim H, Evans AC, Bernasconi A, Bernasconi N. Longitudinal and cross-sectional analysis of atrophy in pharmacoresistant temporal lobe epilepsy. Neurology. 2009;72:1747–1754. doi: 10.1212/01.wnl.0000345969.57574.f5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernhardt BC, Bernasconi N, Concha L, Bernasconi A. Cortical thickness analysis in temporal lobe epilepsy: reproducibility and relation to outcome. Neurology. 2010;74:1776–1784. doi: 10.1212/WNL.0b013e3181e0f80a. [DOI] [PubMed] [Google Scholar]
- Binnewijzend MA, Schoonheim MM, Sanz-Arigita E, Wink AM, van der Flier WM, Tolboom N, Adriaanse SM, Damoiseaux JS, Scheltens P, van Berckel BN, Barkhof F. Resting-state fMRI changes in Alzheimer’s disease and mild cognitive impairment. Neurobiol Aging. 2012;33:2018–2028. doi: 10.1016/j.neurobiolaging.2011.07.003. [DOI] [PubMed] [Google Scholar]
- Biswal BB. Resting state fMRI: a personal history. Neuroimage. 2012;62:938–944. doi: 10.1016/j.neuroimage.2012.01.090. [DOI] [PubMed] [Google Scholar]
- Biswal B, Yetkin FZ, Haughton VM, Hyde JS. Functional connectivity in the motor cortex of resting human brain using echoplanar MRI. Magn Reson Med. 1995;34:537–541. doi: 10.1002/mrm.1910340409. [DOI] [PubMed] [Google Scholar]
- Blumenfeld H, McNally KA, Vanderhill SD, Paige AL, Chung R, Davis K, Norden AD, Stokking R, Studholme C, Novotny EJ, Jr, Zubal IG, Spencer SS. Positive and negative network correlations in temporal lobe epilepsy. Cereb Cortex. 2004;14:892–902. doi: 10.1093/cercor/bhh048. [DOI] [PubMed] [Google Scholar]
- Bocquillon P, Dujardin K, Betrouni N. Attention impairment in temporal lobe epilepsy: a neurophysiological approach via analysis of the P300 wave. Hum Brain Mapp. 2009;30:2267–2277. doi: 10.1002/hbm.20666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boeker H, Kleiser M, Lehman D, Jaenke L, Bogerts B, Northoff G. Executive dysfunction, self, and ego pathology in schizophrenia: an exploratory study of neuropsychology and personality. Compr Psychiatry. 2006;47:7–19. doi: 10.1016/j.comppsych.2005.04.003. [DOI] [PubMed] [Google Scholar]
- Bonilha L, Elm JJ, Edwards JC, Morgan PS, Hicks C, Lozar C, Rumboldt Z, Roberts DR, Rorden C, Eckert MA. How common is brain atrophy in patients with medial temporal lobe epilepsy? Epilepsia. 2010a;51:1774–1779. doi: 10.1111/j.1528-1167.2010.02576.x. [DOI] [PubMed] [Google Scholar]
- Bonilha L, Edwards JC, Kinsman SL, Morgan PS, Fridriksson J, Rorden C, Rumboldt Z, Roberts DR, Eckert MA, Halford JJ. Extrahippocampal gray matter loss and hippocampal deafferentation in patients with temporal lobe epilepsy. Epilepsia. 2010b;51:519–528. doi: 10.1111/j.1528-1167.2009.02506.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouilleret V, Semah F, Chassoux F, Mantzaridez M, Biraben A, Trebossen R, Ribeiro MJ. Basal ganglia involvement in temporal lobe epilepsy: a functional and morphologic study. Neurology. 2008;70:177–184. doi: 10.1212/01.wnl.0000297514.47695.48. [DOI] [PubMed] [Google Scholar]
- Bragin A, Wilson CL, Engel J., Jr Chronic epileptogenesis requires development of a network of pathologically interconnected neuron clusters: a hypothesis. Epilepsia. 2000;41(Suppl 6):S144–S152. doi: 10.1111/j.1528-1157.2000.tb01573.x. [DOI] [PubMed] [Google Scholar]
- Briellmann RS, Jackson GD, Pell GS, Mitchell LA, Abbott DF. Structural abnormalities remote from the seizure focus: a study using T2 relaxometry at 3T. Neurology. 2004;63:2303–2308. doi: 10.1212/01.wnl.0000148646.31755.59. [DOI] [PubMed] [Google Scholar]
- Brier MR, Thomas JB, Snyder AZ, Benzinger TL, Zhang D, Raichle ME, Holtzman DM, Morris JC, Ances BM. Loss of intranetwork and internetwork resting state functional connections with Alzheimer’s disease progression. J Neurosci. 2012;32:8890–8899. doi: 10.1523/JNEUROSCI.5698-11.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broicher SD, Frings L, Huppertz HJ, Grunwald T, Kurthen M, Krämer G, Jokeit H. Alterations in functional connectivity of the amygdala in unilateral mesial temporal lobe epilepsy. J Neurol. 2012;259:2546–2554. doi: 10.1007/s00415-012-6533-3. [DOI] [PubMed] [Google Scholar]
- Bromfield EB, Altshuler L, Leiderman DB, Balish M, Ketter TA, Devinsky O, Post RM, Theodore WH. Cerebral metabolism and depression in patients with complex partial seizures. Arch Neurol. 1992;49:617–623. doi: 10.1001/archneur.1992.00530300049010. [DOI] [PubMed] [Google Scholar]
- Broyd SJ, Demanuele C, Debener S, Helps SK, James CJ, Sonuga-Barke EJ. Default-mode brain dysfunction in mental disorders: a systematic review. Neurosci Biobehav Rev. 2009;33:279–296. doi: 10.1016/j.neubiorev.2008.09.002. [DOI] [PubMed] [Google Scholar]
- Buckner RL, Andrews-Hanna JR, Schacter DL. The brain’s default network: anatomy, function, and relevance to disease. Ann N Y Acad Sci. 2008;1124:1–38. doi: 10.1196/annals.1440.011. [DOI] [PubMed] [Google Scholar]
- Butler T, Blackmon K, McDonald CR, Carlson C, Barr WB, Devinsky O, Kuzniecky R, DuBois J, French J, Halgren E, Thesen T. Cortical thickness abnormalities associated with depressive symptoms in temporal lobe epilepsy. Epilepsy Behav. 2012;23:64–67. doi: 10.1016/j.yebeh.2011.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campo P, Garrido MI, Moran RJ, Maestu F, Garcia-Morales I, Gil-Nagel A, Del Pozo F, Dolan RJ, Friston KJ. Remote effects of hippocampal sclerosis on effective connectivity during working memory encoding: a case of connectional diaschisis? Cereb Cortex. 2012;22:1225–1236. doi: 10.1093/cercor/bhr201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canuet L, Ishii R, Iwase M, Ikezawa K, Kurimoto R, Takahashi H, Currais A, Azechi M, Nakahachi T, Hashimoto R, Takeda M. Working memory abnormalities in chronic interictal epileptic psychosis and schizophrenia revealed by magnetoencephalography. Epilepsy Behav. 2010;17:109–119. doi: 10.1016/j.yebeh.2009.11.002. [DOI] [PubMed] [Google Scholar]
- Canuet L, Ishii R, Pascual-Marqui RD, Iwase M, Kurimoto R, Aoki Y, Ikeda S, Takahashi H, Nakahachi T, Takeda M. Resting-state EEG source localization and functional connectivity in schizophrenia-like psychosis of epilepsy. PLoS ONE. 2011a;6:e27863. doi: 10.1371/journal.pone.0027863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canuet L, Ishii R, Iwase M, Ikezawa K, Kurimoto R, Takahashi H, Currais A, Azechi M, Aoki Y, Nakahachi T, Soriano S, Takeda M. Psychopathology and working memory-induced activation of the prefrontal cortex in schizophrenia-like psychosis of epilepsy: evidence from magnetoencephalography. Psychiatry Clin Neurosci. 2011b;65:183–190. doi: 10.1111/j.1440-1819.2010.02179.x. [DOI] [PubMed] [Google Scholar]
- Cendes F, Andermann F, Gloor P, Gambardella A, Lopes-Cendes I, Watson C, Evans A, Carpenter S, Olivier A. Relationship between atrophy of the amygdala and ictal fear in temporal lobe epilepsy. Brain. 1994;117:739–746. doi: 10.1093/brain/117.4.739. [DOI] [PubMed] [Google Scholar]
- Chabardes S, Kahane P, Hoffman D, Munari C, Benabid AL. Role of the temporo-polar region in the genesis of temporal lobe seizures. Epilepsia. 1999;40(Suppl 7):78. [Google Scholar]
- Chen S, Wu X, Lui S, Wu Q, Yao Z, Li Q, Liang D, An D, Zhang X, Fang J, Huang X, Zhou D, Gong QY. Resting-state fMRI study of treatment-naïve temporal lobe epilepsy patients with depressive symptoms. Neuroimage. 2012;60:299–304. doi: 10.1016/j.neuroimage.2011.11.092. [DOI] [PubMed] [Google Scholar]
- Clemens B, Zvyagintsev M, Sack A, Heinecke A, Willmes K, Sturm W. Revealing the functional neuroanatomy of intrinsic alertness using fMRI: methodological peculiarities. PLoS ONE. 2011;6:e25453. doi: 10.1371/journal.pone.0025453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corbetta M, Shulman GL. Control of goal-directed and stimulus-driven attention in the brain. Nat Rev Neurosci. 2002;3:201–215. doi: 10.1038/nrn755. [DOI] [PubMed] [Google Scholar]
- Damoiseaux JS, Rombouts SA, Barkhof F, Scheltens P, Stam CJ, Smith SM, Beckmann CF. Consistent resting-state networks across healthy subjects. Proc Natl Acad Sci USA. 2006;103:13848–13853. doi: 10.1073/pnas.0601417103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodrill CB. Progressive cognitive decline in adolescents and adults with epilepsy. Prog Brain Res. 2002;135:399–407. doi: 10.1016/S0079-6123(02)35037-4. [DOI] [PubMed] [Google Scholar]
- Dreifuss S, Vingerhoets FJ, Lazeyras F, Andino SG, Spinelli L, Delavelle J, Seeck M. Volumetric measurements of subcortical nuclei in patients with temporal lobe epilepsy. Neurology. 2001;57:1636–1641. doi: 10.1212/wnl.57.9.1636. [DOI] [PubMed] [Google Scholar]
- Eisenberg DP, Berman KF. Executive function, neural circuitry, and genetic mechanisms in schizophrenia. Neuropsychopharmacology. 2010;35:258–277. doi: 10.1038/npp.2009.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elger CE, Helmstaedter C, Kurthen M. Chronic epilepsy and cognition. Lancet Neurol. 2004;3:663–672. doi: 10.1016/S1474-4422(04)00906-8. [DOI] [PubMed] [Google Scholar]
- Fahoum F, Lopes R, Pittau F, Dubeau F, Gotman J. Widespread epileptic networks in focal epilepsies: EEG-fMRI study. Epilepsia. 2012;53:1618–1627. doi: 10.1111/j.1528-1167.2012.03533.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan J, McCandliss BD, Fossella J, Flombaum JI, Posner MI. The activation of attentional networks. Neuroimage. 2005;26:471–479. doi: 10.1016/j.neuroimage.2005.02.004. [DOI] [PubMed] [Google Scholar]
- Fleck DE, Shear PK, Strakowski SM. A reevaluation of sus-tained attention performance in temporal lobe epilepsy. Arch Clin Neuropsychol. 2002;17:399–405. [PubMed] [Google Scholar]
- Fox MD, Snyder AZ, Vincent JL, Corbetta M, Van Essen DC, Raichle ME. The human brain is intrinsically organized into dynamic, anticorrelated functional networks. Proc Natl Acad Sci USA. 2005;102:9673–9678. doi: 10.1073/pnas.0504136102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox MD, Corbetta M, Snyde AZ, Vincent JL, Raichle ME. Spontaneous neuronal activity distinguishes human dorsal and ventral attention systems. Proc Natl Acad Sci USA. 2006;103:10046–10051. doi: 10.1073/pnas.0604187103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fransson P, Marrelec G. The precuneus/posterior cingulate cortex plays a pivotal role in the default mode network: evidence from a partial correlation network analysis. Neuroimage. 2008;42:1178–1184. doi: 10.1016/j.neuroimage.2008.05.059. [DOI] [PubMed] [Google Scholar]
- Frings L, Schulze-Bonhage A, Spreer J, Wagner K. Remote effects of hippocampal damage on default network connectivity in the human brain. J Neurol. 2009;256:2021–2029. doi: 10.1007/s00415-009-5233-0. [DOI] [PubMed] [Google Scholar]
- Gaitzis A, Trimble MR, Sander JW. The psychiatric comorbidity of epilepsy. Acta Neurol Scand. 2004;110:207–220. doi: 10.1111/j.1600-0404.2004.00324.x. [DOI] [PubMed] [Google Scholar]
- Gloor P. Role of the amygdala in temporal lobe epilepsy. In: Aggleton J, editor. The amygdala: neurobiological aspects of emotion, memory and mental dysfunction. Wiley-Liss; New York: 1992. pp. 505–538. [Google Scholar]
- Gloor P. The temporal lobe and limbic system. Oxford University Press; New York: 1997. [Google Scholar]
- Gottlieb L, Zelko FA, Kim DS, Nordli DR. Cognitive proficiency in pediatric epilepsy. Epilepsy Behav. 2012;23:146–151. doi: 10.1016/j.yebeh.2011.10.024. [DOI] [PubMed] [Google Scholar]
- Greicius MD, Srivastava G, Reiss AL, Menon V. Default-mode network activity distinguishes Alzheimer’s disease from healthy aging: evidence from functional MRI. Proc Natl Acad Sci USA. 2004;101:4637–4642. doi: 10.1073/pnas.0308627101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haneef Z, Lenartowicz A, Yeh HJ, Engel J, Jr, Stern JM. Effect of lateralized temporal lobe epilepsy on the default mode network. Epilepsy Behav. 2012;25:350–357. doi: 10.1016/j.yebeh.2012.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison BJ, Pujol J, Ortiz H, Fornito A, Pantelis C, Yücel M. Modulation of brain resting-state networks by sad mood induction. PLoS ONE. 2008;3:e1794. doi: 10.1371/journal.pone.0001794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heaton RK, Chelune GJ, Talley JL, Kay GG, Curtiss G. Wisconsin Card Sorting Test (WCST) manual, revised and expanded. Psychological Assessment Resources Inc; Odessa, FL: 1993. [Google Scholar]
- Helmstaedter C, Kockelmann E. Cognitive outcomes in patients with chronic temporal lobe epilepsy. Epilepsia. 2006;47(Suppl 2):96–98. doi: 10.1111/j.1528-1167.2006.00702.x. [DOI] [PubMed] [Google Scholar]
- Hlobil U, Rathore C, Alexander A, Sarma S, Radhakrishnan K. Impaired facial emotion recognition in patients with mesial temporal lobe epilepsy associated with hippocampal sclerosis (MTLE-HS): side and age at onset matters. Epilepsy Res. 2008;80:150–157. doi: 10.1016/j.eplepsyres.2008.03.018. [DOI] [PubMed] [Google Scholar]
- Honey CJ, Sporns O, Cammoun L, Gigandet X, Thiran JP, Meuli R, Hagmann P. Predicting human resting-state functional connectivity from structural connectivity. Proc Natl Acad Sci USA. 2009;106:2035–2040. doi: 10.1073/pnas.0811168106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jokeit H, Seitz RJ, Markowitsch HJ, Neumann N, Witte OW, Ebner A. Prefrontal asymmetric interictal glucose hypometabolism and cognitive impairment in patients with temporal lobe epilepsy. Brain. 1997;120:2283–2294. doi: 10.1093/brain/120.12.2283. [DOI] [PubMed] [Google Scholar]
- Kanner AM. Hippocampal atrophy: another common pathogenic mechanism of depressive disorders and epilepsy? Epilepsy Curr. 2011;11:149–150. doi: 10.5698/1535-7511-11.5.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keller SS, Baker G, Downes JJ, Roberts N. Quantitative MRI of the prefrontal cortex and executive function in patients with temporal lobe epilepsy. Epilepsy Behav. 2009;15:186–195. doi: 10.1016/j.yebeh.2009.03.005. [DOI] [PubMed] [Google Scholar]
- Kennedy JD, Schuele SU. Neocortical temporal lobe epilepsy. J Clin Neurophysiol. 2012;29:366–370. doi: 10.1097/WNP.0b013e31826bd78b. [DOI] [PubMed] [Google Scholar]
- Kinnison J, Padmala S, Choi JM, Pessoa L. Network analysis reveals increased integration during emotional and motivational processing. J Neurosci. 2012;32:8361–8372. doi: 10.1523/JNEUROSCI.0821-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobayashi E, Bagshaw AP, Bénar CG, Aghakhani Y, Andermann F, Dubeau F, Gotman J. Temporal and extratemporal BOLD responses to temporal lobe interictal spikes. Epilepsia. 2006;47:343–354. doi: 10.1111/j.1528-1167.2006.00427.x. [DOI] [PubMed] [Google Scholar]
- Kortte KB, Horner MD, Windham WK. The trail making test, Part B: cognitive flexibility or ability to maintain set? Appl Neuropsychol. 2002;9:106–109. doi: 10.1207/S15324826AN0902_5. [DOI] [PubMed] [Google Scholar]
- Krishnamoorthy ES, Trimble MR, Blumer D. The classification of neuropsychiatric disorders in epilepsy: a proposal by the ILAE Commission on Psychobiology of Epilepsy. Epilepsy Behav. 2007;10:349–53. doi: 10.1016/j.yebeh.2006.10.002. [DOI] [PubMed] [Google Scholar]
- Laufs H. Functional imaging of seizures and epilepsy: evolution from zones to networks. Curr Opin Neurol. 2012;25:194–200. doi: 10.1097/WCO.0b013e3283515db9. [DOI] [PubMed] [Google Scholar]
- Laufs H, Hamandi K, Salek-Haddadi A, Kleinschmidt AK, Duncan JS, Lemieux L. Temporal lobe interictal epileptic discharges affect cerebral activity in “default mode” brain regions. Hum Brain Mapp. 2007;28:1023–1032. doi: 10.1002/hbm.20323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li R, Wu X, Chen K, Fleisher AS, Reiman EM, Yao L. Alterations of directional connectivity among resting-state networks in Alzheimer disease. AJNR Am J Neuroradiol. 2013;34:340–345. doi: 10.3174/ajnr.A3197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao W, Zhang Z, Pan Z, Mantini D, Ding J, Duan X, Luo C, Lu G, Chen H. Altered functional connectivity and small-world in mesial temporal lobe epilepsy. PLoS ONE. 2010;5:e8525. doi: 10.1371/journal.pone.0008525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao W, Zhang Z, Pan Z, Mantini D, Ding J, Duan X, Luo C, Wang Z, Tan Q, Lu G, Chen H. Default mode network abnormalities in mesial temporal lobe epilepsy: a study combining fMRI and DTI. Hum Brain Mapp. 2011;32:883–895. doi: 10.1002/hbm.21076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieb JP, Dasheiff RM, Engel J., Jr Role of the frontal lobes in the propagation of mesial temporal lobe seizures. Epilepsia. 1991;32:822–837. doi: 10.1111/j.1528-1157.1991.tb05539.x. [DOI] [PubMed] [Google Scholar]
- Lin JJ, Riley JD, Juranek J, Cramer SC. Vulnerability of the frontal-temporal connections in temporal lobe epilepsy. Epilepsy Res. 2008;82:162–170. doi: 10.1016/j.eplepsyres.2008.07.020. [DOI] [PubMed] [Google Scholar]
- Malmgren K, Thom M. Hippocampal sclerosis-origins and imaging. Epilepsia. 2012;53(Suppl 4):19–33. doi: 10.1111/j.1528-1167.2012.03610.x. [DOI] [PubMed] [Google Scholar]
- Martin RC, Sawrie SM, Gilliam FG, Palmer CA, Faught E, Morawetz RB, Kuzniecky RI. Wisconsin card sorting performance in patients with temporal lobe epilepsy: clinical and neuroanatomical correlates. Epilepsia. 2000;41:1626–1632. doi: 10.1111/j.1499-1654.2000.001626.x. [DOI] [PubMed] [Google Scholar]
- McCormick C, Quraan M, Cohn M, Valiante TA, McAndrews MP. Default mode network connectivity indicates episodic memory capacity in mesial temporal lobe epilepsy. Epilepsia. 2013;54:809–818. doi: 10.1111/epi.12098. [DOI] [PubMed] [Google Scholar]
- McDonald CR, Hagler DJ, Jr, Ahmadi ME, Tecoma E, Iragui V, Gharapetian L, Dale AM, Halgren E. Regional neocortical thinning in mesial temporal lobe epilepsy. Epilepsia. 2008;49:794–803. doi: 10.1111/j.1528-1167.2008.01539.x. [DOI] [PubMed] [Google Scholar]
- Meletti S, Benuzzi F, Rubboli G, Cantalupo G, Stanzani Maserati M, Nichelli P, Tassinari CA. Impaired facial emotion recognition in early-onset right mesial temporal lobe epilepsy. Neurology. 2003;60:426–431. doi: 10.1212/wnl.60.3.426. [DOI] [PubMed] [Google Scholar]
- Meletti S, Benuzzi F, Cantalupo G, Rubboli G, Tassinari CA, Nichelli P. Facial emotion recognition impairment in chronic temporal lobe epilepsy. Epilepsia. 2009;50:1547–1559. doi: 10.1111/j.1528-1167.2008.01978.x. [DOI] [PubMed] [Google Scholar]
- Miao X, Wu X, Li R, Chen K, Yao L. Altered connectivity pattern of hubs in default-mode network with Alzheimer’s disease: an Granger causality modeling approach. PLoS ONE. 2011;6:e25546. doi: 10.1371/journal.pone.0025546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller JM, Kustra RP, Vuong A, Hammer AE, Messenheimer JA. Depressive symptoms in epilepsy: prevalence, impact, aetiology, biological correlates and effect of treatment with antiepileptic drugs. Drugs. 2008;68:1493–1509. doi: 10.2165/00003495-200868110-00003. [DOI] [PubMed] [Google Scholar]
- Nadkarni S, Arnedo V, Devinsky O. Psychosis in epilepsy patients. Epilepsia. 2007;48(Suppl 9):17–19. doi: 10.1111/j.1528-1167.2007.01394.x. [DOI] [PubMed] [Google Scholar]
- Ozkara C, Aronica E. Hippocampal sclerosis. Handb Clin Neurol. 2012;108:621–639. doi: 10.1016/B978-0-444-52899-5.00019-8. [DOI] [PubMed] [Google Scholar]
- Petersen SE, Posner MI. The attention system of the human brain: 20 years after. Annu Rev Neurosci. 2012;35:73–89. doi: 10.1146/annurev-neuro-062111-150525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pitkänen A, Tuunanen J, Kälviäinen R, Partanen K, Salmenperä T. Amygdala damage in experimental and human temporal lobe epilepsy. Epilepsy Res. 1998;32:233–253. doi: 10.1016/s0920-1211(98)00055-2. [DOI] [PubMed] [Google Scholar]
- Pittau F, Grova C, Moeller F, Dubeau F, Gotman J. Patterns of altered functional connectivity in mesial temporal lobe epilepsy. Epilepsia. 2012;53:1013–1023. doi: 10.1111/j.1528-1167.2012.03464.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price CJ, Warburton EA, Moore CJ, Frackowiak RS, Friston KJ. Dynamic diaschisis: anatomically remote and context-sensitive human brain lesions. J Cogn Neurosci. 2001;13:419–429. doi: 10.1162/08989290152001853. [DOI] [PubMed] [Google Scholar]
- Protzner AB, McAndrews MP. Network alterations supporting word retrieval in patients with medial temporal lobe epilepsy. J Cogn Neurosci. 2011;23:2605–2619. doi: 10.1162/jocn.2010.21599. [DOI] [PubMed] [Google Scholar]
- Richardson EJ, Griffith HR, Martin RC, Paige AL, Stewart CC, Jones J, Hermann BP, Seidenberg M. Structural and functional neuroimaging correlates of depression in temporal lobe epilepsy. Epilepsy Behav. 2007;10:242–249. doi: 10.1016/j.yebeh.2006.11.013. [DOI] [PubMed] [Google Scholar]
- Riederer F, Lanzenberger R, Kaya M, Prayer D, Serles W, Baumgartner C. Network atrophy in temporal lobe epilepsy: a voxel-based morphometry study. Neurology. 2008;71:419–425. doi: 10.1212/01.wnl.0000324264.96100.e0. [DOI] [PubMed] [Google Scholar]
- Riley JD, Moore S, Cramer SC, Lin JJ. Caudate atrophy and impaired frontostriatal connections are linked to executive dysfunction in temporal lobe epilepsy. Epilepsy Behav. 2011;21:80–87. doi: 10.1016/j.yebeh.2011.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadaghiani S, Scheeringa R, Lehongre K, Morillon B, Giraud AL, Kleinschmidt A. Intrinsic connectivity networks, alpha oscillations, and tonic alertness: a simultaneous electroencephalography/functional magnetic resonance imaging study. J Neurosci. 2010;30:10243–10250. doi: 10.1523/JNEUROSCI.1004-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salzberg M, Taher T, Davie M, Carne R, Hicks RJ, Cook M, Murphy M, Vinton A, O’Brien TJ. Depression in temporal lobe epilepsy surgery patients: an FDG-PET study. Epilepsia. 2006;47:2125–2130. doi: 10.1111/j.1528-1167.2006.00860.x. [DOI] [PubMed] [Google Scholar]
- Schacher M, Haemmerle B, Woermann FG, Okujava M, Huber D, Grunwald T, Kramer G, Jokeit H. Amygdala fMRI lateralizes temporal lobe epilepsy. Neurology. 2006a;66:81–87. doi: 10.1212/01.wnl.0000191303.91188.00. [DOI] [PubMed] [Google Scholar]
- Schacher M, Winkler R, Grunwald T, Kraemer G, Kurthen M, Reed V, Jokeit H. Mesial temporal lobe epilepsy impairs advanced social cognition. Epilepsia. 2006b;47:2141–2146. doi: 10.1111/j.1528-1167.2006.00857.x. [DOI] [PubMed] [Google Scholar]
- Seeley WW, Menon V, Schatzberg AF, Keller J, Glover GH, Kenna H, Reiss AL, Greicius MD. Dissociable intrinsic connectivity networks for salience processing and executive control. J Neurosci. 2007;27:2349–2356. doi: 10.1523/JNEUROSCI.5587-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seidenberg M, Kelly KG, Parrish J, Geary E, Dow C, Rutecki P, Hermann B. Ipsilateral and contralateral MRI volumetric abnormalities in chronic unilateral temporal lobe epilepsy and their clinical correlates. Epilepsia. 2005;46:420–430. doi: 10.1111/j.0013-9580.2005.27004.x. [DOI] [PubMed] [Google Scholar]
- Shamim S, Hasler G, Liew C, Sato S, Theodore WH. Temporal lobe epilepsy, depression, and hippocampal volume. Epilepsia. 2009;50:1067–1071. doi: 10.1111/j.1528-1167.2008.01883.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheline YI, Price JL, Yan Z, Mintun MA. Resting-state functional MRI in depression unmasks increased connectivity between networks via the dorsal nexus. Proc Natl Acad Sci USA. 2010;107:11020–11025. doi: 10.1073/pnas.1000446107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spencer SS. Neural networks in human epilepsy: evidence of and implications for treatment. Epilepsia. 2002;43:219–227. doi: 10.1046/j.1528-1157.2002.26901.x. [DOI] [PubMed] [Google Scholar]
- Spencer S, Spencer D. Entorhinal-hippocampal interactions in medial temporal lobe epilepsy. Epilepsia. 1994;35:721–727. doi: 10.1111/j.1528-1157.1994.tb02502.x. [DOI] [PubMed] [Google Scholar]
- Sporns O, Zwi JD. The small world of the cerebral cortex. Neuroinformatics. 2004;2:145–162. doi: 10.1385/NI:2:2:145. [DOI] [PubMed] [Google Scholar]
- Spreng RN, Grady CL. Patterns of brain activity supporting autobiographical memory, prospection, and theory of mind, and their relationship to the default mode network. J Cogn Neurosci. 2010;22:1112–1123. doi: 10.1162/jocn.2009.21282. [DOI] [PubMed] [Google Scholar]
- Stam CJ, Reijneveld JC. Graph theoretical analysis of complex networks in the brain. Nonlinear Biomed Phys. 2007;1:3. doi: 10.1186/1753-4631-1-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stella F, Maciel JA. Attentional disorders in patients with complex partial epilepsy. Arq Neuropsiquiatr. 2003;61:335–338. doi: 10.1590/s0004-282x2003000300003. [DOI] [PubMed] [Google Scholar]
- Tatum WO., IV Mesial temporal lobe epilepsy. J Clin Neurophysiol. 2012;29:356–365. doi: 10.1097/WNP.0b013e31826b3ab7. [DOI] [PubMed] [Google Scholar]
- Tebartz van Elst L, Woermann FG, Lemieux L, Thompson PJ, Trimble MR. Affective aggression in patients with temporal lobe epilepsy: a quantitative MRI study of the amygdala. Brain. 2000;123:234–243. doi: 10.1093/brain/123.2.234. [DOI] [PubMed] [Google Scholar]
- Tebartz Van Elst L, Baeumer D, Lemieux L, Woermann FG, Koepp M, Krishnamoorthy S, Thompson PJ, Ebert D, Trimble MR. Amygdala pathology in psychosis of epilepsy: a magnetic resonance imaging study in patients with temporal lobe epilepsy. Brain. 2002;125:140–149. doi: 10.1093/brain/awf008. [DOI] [PubMed] [Google Scholar]
- Tebartz van Elst L, Groffmann M, Ebert D, Schulze-Bonhage A. Amygdala volume loss in patients with dysphoric disorder of epilepsy. Epilepsy Behav. 2009;16:105–112. doi: 10.1016/j.yebeh.2009.06.009. [DOI] [PubMed] [Google Scholar]
- Téllez-Zenteno JF, Hernández-Ronquillo L. A review of the epidemiology of temporal lobe epilepsy. Epilepsy Res Treat. 2012;2012:630853. doi: 10.1155/2012/630853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomasi D, Volkow ND. Association between functional connectivity hubs and brain networks. Cereb Cortex. 2011;21:2003–2013. doi: 10.1093/cercor/bhq268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaessen MJ, Jansen JF, Vlooswijk MC, Hofman PA, Majoie HJ, Aldenkamp AP, Backes WH. White matter network abnormalities are associated with cognitive decline in chronic epilepsy. Cereb Cortex. 2012;22:2139–2147. doi: 10.1093/cercor/bhr298. [DOI] [PubMed] [Google Scholar]
- van Dellen E, Douw L, Baayen JC, Heimans JJ, Ponten SC, Vandertop WP, Velis DN, Stam CJ, Reijneveld JC. Long-term effects of temporal lobe epilepsy on local neural networks: a graph theoretical analysis of corticography recordings. PLoS ONE. 2009;4:e8081. doi: 10.1371/journal.pone.0008081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Heuvel MP, Hulshoff Pol HE. Exploring the brain network: a review on resting-state fMRI functional connectivity. Eur Neuropsychopharmacol. 2010;20:519–534. doi: 10.1016/j.euroneuro.2010.03.008. [DOI] [PubMed] [Google Scholar]
- van den Heuvel MP, Mandl RC, Kahn RS, Hulshoff Pol HE. Functionally linked resting-state networks reflect the underlying structural connectivity architecture of the human brain. Hum Brain Mapp. 2009;30:3127–3141. doi: 10.1002/hbm.20737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vlooswijk MC, Jansen JF, Jeukens CR, Majoie HJ, Hofman PA, de Krom MC, Aldenkamp AP, Backes WH. Memory processes and prefrontal network dysfunction in cryptogenic epilepsy. Epilepsia. 2011;52:1467–1475. doi: 10.1111/j.1528-1167.2011.03108.x. [DOI] [PubMed] [Google Scholar]
- Voets NL, Beckmann CF, Cole DM, Hong S, Bernasconi A, Bernasconi N. Structural substrates for resting network disruption in temporal lobe epilepsy. Brain. 2012;135:2350–2357. doi: 10.1093/brain/aws137. [DOI] [PubMed] [Google Scholar]
- Wendling F, Badier JM, Chauvel P, Coatrieux JL. A method to quantify invariant information in depth-recorded epileptic seizures. Electroencephalogr Clin Neurophysiol. 1997;102:472–485. doi: 10.1016/s0013-4694(96)96633-3. [DOI] [PubMed] [Google Scholar]
- Wilson SJ, Micallef S, Henderson A, Rayner G, Wrennall JA, Spooner C, Harvey AS. Developmental outcomes of childhood-onset temporal lobe epilepsy: a community-based study. Epilepsia. 2012;53:1587–1596. doi: 10.1111/j.1528-1167.2012.03632.x. [DOI] [PubMed] [Google Scholar]
- Woodward ND, Rogers B, Heckers S. Functional resting-state networks are differentially affected in schizophrenia. Schizophr Res. 2011;130:86–93. doi: 10.1016/j.schres.2011.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong J, Parsons LM, Gao JH, Fox PT. Interregional connectivity to primary motor cortex revealed using MRI resting state images. Hum Brain Mapp. 1999;8:151–156. doi: 10.1002/(SICI)1097-0193(1999)8:2/3<151::AID-HBM13>3.0.CO;2-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Z, Wang H, Zhang Z, Zhong Y, Chen Z, Lu G. Study based on ICA of dorsal attention network in patients with temporal lobe epilepsy. Sheng Wu Yi Xue Gong Cheng Xue Za Zhi. 2010;27:10–15. [PubMed] [Google Scholar]
- Zeber JE, Copeland LA, Amuan M, Cramer JA, Pugh MJ. The role of comorbid psychiatric conditions in health status in epilepsy. Epilepsy Behav. 2007;10:539–546. doi: 10.1016/j.yebeh.2007.02.008. [DOI] [PubMed] [Google Scholar]
- Zhang Z, Lu G, Zhong Y, Tan Q, Liao W, Chen Z, Shi J, Liu Y. Impaired perceptual networks in temporal lobe epilepsy revealed by resting fMRI. J Neurol. 2009a;256:1705–1713. doi: 10.1007/s00415-009-5187-2. [DOI] [PubMed] [Google Scholar]
- Zhang Z, Lu G, Zhong Y, Tan Q, Yang Z, Liao W, Chen Z, Shi J, Liu Y. Impaired attention network in temporal lobe epilepsy: a resting FMRI study. Neurosci Lett. 2009b;458:97–101. doi: 10.1016/j.neulet.2009.04.040. [DOI] [PubMed] [Google Scholar]
- Zhang Z, Lu G, Zhong Y, Tan Q, Chen H, Liao W, Tian L, Li Z, Shi J, Liu Y. fMRI study of mesial temporal lobe epilepsy using amplitude of low-frequency fluctuation analysis. Hum Brain Mapp. 2010a;31:1851–1861. doi: 10.1002/hbm.20982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z, Lu G, Zhong Y, Tan Q, Liao W, Wang Z, Wang Z, Li K, Chen H, Liu Y. Altered spontaneous neuronal activity of the default-mode network in mesial temporal lobe epilepsy. Brain Res. 2010b;1323:152–160. doi: 10.1016/j.brainres.2010.01.042. [DOI] [PubMed] [Google Scholar]
- Zheng J, Qin B, Dang C, Ye W, Chen Z, Yu L. Alertness network in patients with temporal lobe epilepsy: a fMRI study. Epilepsy Res. 2012;100:67–73. doi: 10.1016/j.eplepsyres.2012.01.006. [DOI] [PubMed] [Google Scholar]