Abstract
Objectives:
To evaluate the effect of preoperative statin therapy on the incidence of postoperative infection.
Methods:
This systematic review of the literature was carried out in August 2015. Studies were retrieved via PubMed, Embase, and the Cochrane Library (1980 to 2015), and the reference files were limited to English-language articles. We used a standardized protocol, and a meta-analysis was performed for data abstraction.
Results:
Five studies comprising 1,362 patients qualified for the analysis. The incidence of postoperative infections in the statin group (1.1%) was not significantly lower than that in the placebo group (2.4%), with a risk ratio (RR) of 0.56 (95% confidence interval [CI] 0.24-1.33, p=0.19). Patients of 3 studies underwent cardiac surgery. The aggregated results of these studies failed to show significant differences in postoperative infection when a fixed effects model was used (RR: 0.39; 95% CI: 0.08-1.97, p=0.26].
Conclusions:
We failed to find sufficient evidence to support the association between statin use and postoperative infectious complications. The absence of any evidence for a beneficial effect in available randomized trials reduces the likelihood of a causal effect as reported in observational studies.
The 3-hydroxy-3-methylglutaryl-coenzyme A reductase inhibitors (or statins) have pleiotropic properties; thus, the use of perioperative statin treatment to improve outcomes during and after surgery has become popular.1-5 Although treatment with perioperative statins in cardiac and noncardiac surgery significantly reduced the risk of myocardial infarction and atrial fibrillation and decreased the mean duration of hospitalization5,6 whether statins are effective in preventing postoperative infectious complications remains controversial. A meta-analysis evaluated whether the potential of statins to lower the risk of infections was causal, which failed to support the hypothesis.7 However, the analysis never included the studies evaluating the association between preoperative statin use and the risk of postoperative infectious complications. Some studies have reported that preoperative statin therapy significantly reduced postoperative infectious complications.8,9 Contrary to these results, other studies have shown that preoperative statin therapy failed to reduce the risk of infection after surgery.10,11 A previous meta-analysis showed preoperative statin use was associated with a reduced risk of postoperative infectious complications.12 However, this analysis only included cohort studies, which reduced the reliability. Therefore, we conducted a meta-analysis by pooling together all available randomized trials with similar study designs to evaluate the clinical efficacy of preprocedural statin therapy on preventing infectious complications after surgery. In the present study, we analyzed 5 randomized trials and evaluated the relationships between preprocedural statins and postoperative infections.
Methods
A systematic review of the literature was undertaken in August 2015. All analyses were based on previous published studies, thus, no ethical approval and patient consent are required.
Selection criteria
Studies were included in our analysis if they met the following criteria: (i) written in English; (ii) had a statin therapy group and a simultaneous placebo control group, (iii) and statin therapy was initiated before surgery. Studies not meeting these criteria, non-clinical trials, and studies without data for retrieval were excluded from the analysis.
Search source and strategy
We performed a search via PubMed, Embase, and the Cochrane Library using the following keywords: (‘hydroxymethylglutaryl coenzyme a reductase inhibitor’ OR statin OR ‘anticholesteremic agents’ OR simvastatin OR rosuvastatin OR pravastatin OR atorvastatin OR fluvastatin OR cerivastatin OR pitavastatin OR lovastatin) AND (‘surgical approach’ OR surg* OR operat*) AND (infect* OR sepsis OR bacter* OR pneumonia) AND (random* OR blind* OR placebo OR ‘meta analysis’). The references of relevant trials and reviews were identified and trials were searched manually. We also checked the citations of existing reviews and all studies identified by using these methods. Missing information were obtained by contacting the corresponding authors of the studies.
Quality assessment and data management
We assessed the quality of the included studies based on a well-established, validated scale developed by Jadad et al.13 The range of possible scores was 0 to 5. According to the inclusion criteria, 2 authors independently and blindly selected the studies. They subsequently assessed trial quality independently and extracted data on study design, subject characteristics at baseline, and incidence of postoperative infectious complications using a standardized protocol and reporting form. Any disagreement was resolved by consensus.
Statistical analysis
REVMAN 5.1 software developed by the Cochrane Collaboration was used for meta-analysis. The incidences of postoperative infections were expressed as risk ratio (RR) with 95% confidence interval (CI) for each study. Heterogeneity between selected articles was tested using the Chi-squared and I2 tests. The 2-tailed significance level was set at 0.05. If no significant difference existed among the results, the fixed effects model was applied. If a significant difference was observed among the results, the random effects model was applied and subgroup analysis were used to deal with heterogeneity. The measure of number needed to treat (NNT) was used to assess the effectiveness of statin treatment.
Results
Identification and characteristics of eligible studies
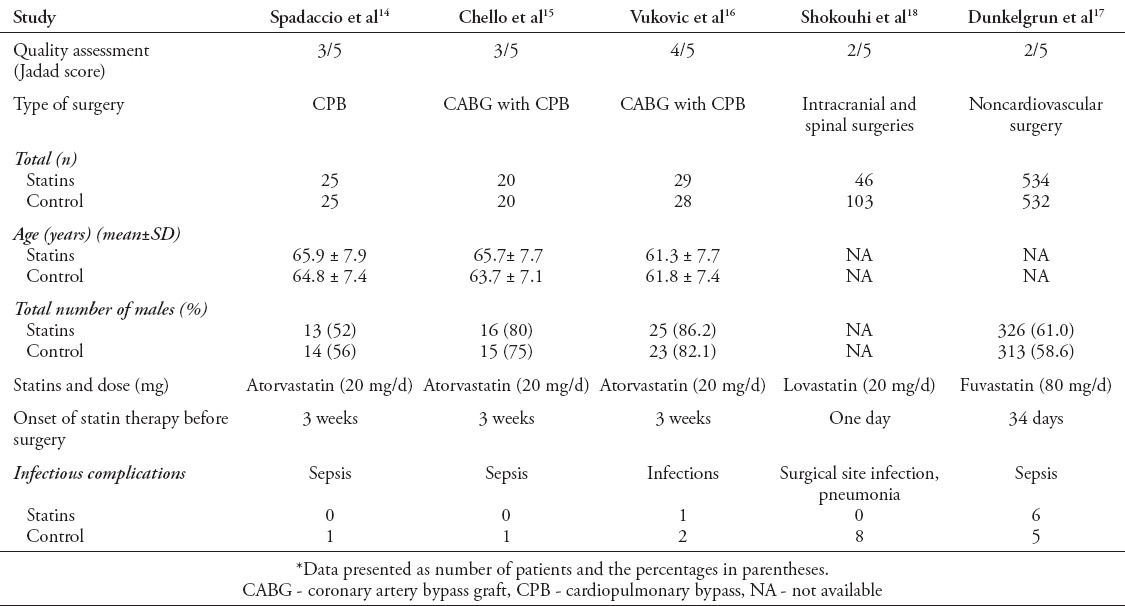
The initial search using the electronic search strategy and the manual search yielded 491 studies. We reviewed the studies to determine whether they met the criteria for inclusion. After independent evaluation by 2 authors, only 5 trials met the inclusion criteria. We included 5 studies in the analysis (Figure 1).14-18 Quality assessment, subject characteristics (such as age, gender, statins, and dose), and other treatment data of the included studies are presented in Table 1. Three studies were of fairly good quality (Jadad score 3/5). In total, 1362 patients were enrolled from 5 trials. Among these patients, 654 received statins and 708 received placebos.
Figure 1.
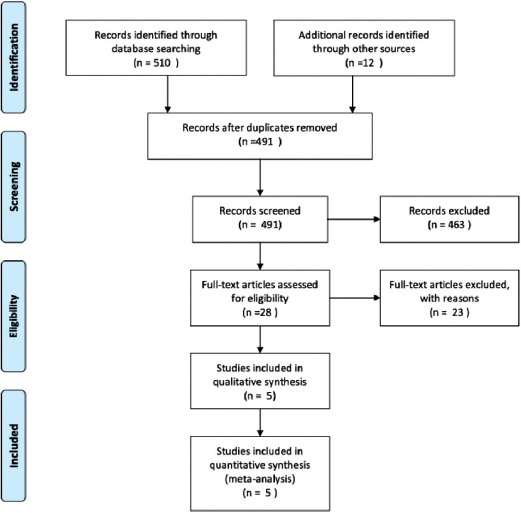
Flow diagram depicting the selection of studies included in the meta-analysis.
Table 1.
Characteristics of the 5 randomized clinical studies included in the present meta-analysis.
Main analysis
No heterogeneity was found in the incidence of postoperative infections from 5 studies (x2 = 2.81; p=0.59; I2 = 0%). A fixed effects model was used. The total incidence of postoperative infections in the statin group (1.1%) was not significantly lower than that in the placebo group (2.4%; RR, 0.56; 95% CI, 0.24-1.33; p=0.19) (Figure 2). However, our analysis demonstrated a trend toward statistical significant for this association.
Figure 2.
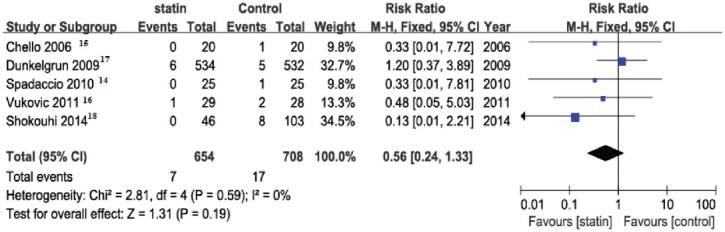
Analysis of controlled studies of statin versus control in patients undergoing surgery. Outcome: incidence of postoperative infections, 95% CI - 95% confidence interval, M-H - Mantel-Haenszel, df - degrees of freedom
Subgroup analysis
Table 2 shows the results of subgroup analysis stratified by surgery and statins design. Patients of 3 studies underwent cardiac surgery.14-16 The aggregated results of these studies failed to show a significant difference in postoperative infections using a fixed effects model (RR: 0.39, 95% CI: 0.08-1.97, p=0.26). Patients of 2 studies underwent noncardiovascular surgery.17,18 The total incidence of postoperative infections in the statin group was not significantly lower than in the placebo group (RR: 0.65, 95% CI: 0.23-1.79, p=0.40). Patients of 3 studies received atorvastatin treatment before surgery.14-16 The use of statins in the preoperative period was not associated with a lower incidence of postoperative infections (RR: 0.39, 95% CI: 0.08-1.97, p=0.26) (Figure 3).
Table 2.
Results of stratified analyses of infection-associated incidence in patients undergoing surgery and statins.
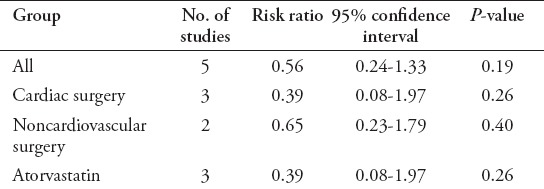
Figure 3.
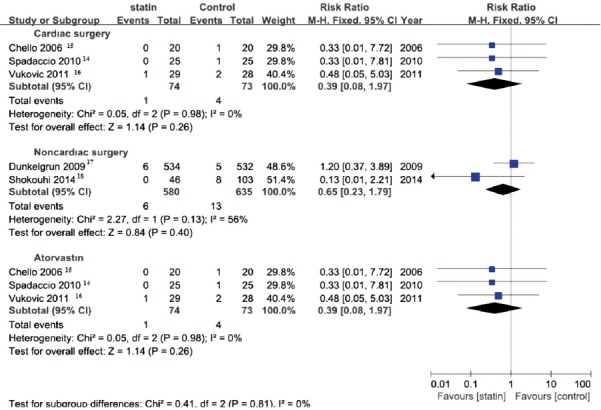
Subgroup analysis of controlled studies of statin versus control in patients undergoing surgery. Outcome: incidence of postoperative infections, 95% CI - 95% confidence interval, M-H - Mantel-Haenszel, df - degrees of freedom.
Publication bias
We performed a funnel plot for postoperative infections, which included 5 randomized control trials (RCTs).14-18 However, the limiting RCTs make it difficult to interpret the result of publication bias (Figure 4).
Figure 4.
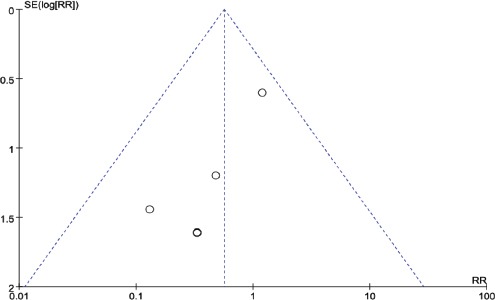
Funnel plot of SE (log risk ratio) by risk ratio to evaluate publication bias for effect of treatment.
Number needed to treat
Since statistical analysis failed to prove a benefit for statin treatment, the NNT was not assessed.
Discussion
In the present meta-analysis, we failed to obtain adequate evidence to support the association between statin use and postoperative infectious complications. However, the pooled effect estimate of 0.56 and the trend toward statistical significance for this association indicated the need for further investigation.
Statins, which inhibit 3-hydroxy-3-methyl-glutaryl(HMG)-CoA reductase, are the medical treatment of choice for the reduction of high cholesterol levels. Independent of lipid-lowering effects, statins have pleiotropic effects, including decreased inflammation, improved endothelial function, antagonism of platelet function, and antithrombotic properties.19-22 Previous studies1,5,23-25 demonstrated that statins improve outcomes during and after PCI, cardiac surgery, and noncardiac vascular surgery. However, these studies never evaluate the effect of preoperative statin therapy on the incidence of postoperative infection.
The association among statins, infection prevention, and outcomes was biologically plausible. Statins can modulate the function of different immune cells, including T cells, and endothelial cells.26,27 Many cell receptors and cytokines can be reduced by statins, such as MCH-II, P-selectin, and MCP-1.28 In addition, statins exert direct antibacterial and antiviral effects.29,30 Some study suggests a potent antimicrobial activity of statins against both Aggregatibacter actinomycetemcomitans and Porphyromonas gingivalis.31 Statins contribute to macrophage-bactericidal activity against Mycobacterium bovis, Mycobacterium leprae, and Mycobacterium tuberculosis. It is likely that the association of statins with the actual multidrug therapy effectively reduces mycobacterial viability and tissue lesions in leprosy and tuberculosis patients.32
Whether preoperative statin therapy can help to prevent postoperative infection is still debated, with some studies finding a significant reduction in postoperative infections,8,9 and others reporting no effect on infection risk.10,11 A systematic review addressing the role of statins in preventing postoperative infectious complications has been published recently.12 The review showed a significant difference, however, it only included observational and retrospective studies. Observational studies are always at risk of unmeasured confounding. Our review is unique. The strength of our data from randomized controlled trials is the absence of such bias. Infection risk differed depending on the type of surgery. Thus, we investigated the results of subgroup analysis stratified by surgery design. Such investigation yielded a precise estimate of the anti-infective effects of statins. We also investigated the results of subgroup analysis stratified by the design of statins.
Study limitations
Randomized control trials with statins and infections as endpoints are difficult to find. Only 5 randomized clinical trials that included 1362 subjects in total were included in this study. Also, the enrolled studies had a wide-ranging sample size from 40 to 1066. These 2 factors may result in unreliable outcomes. Morever, only one of the trials included infection-related events as a primary outcome measure.18 Most of the included trials failed to describe the type of infection involved.
In conclusion, our findings do not support the hypothesis that statins reduce the risk of postoperative infectious complications. Current cumulative evidence suggests a trend toward statistical significance. More large-scale RCTs are needed to determine all the potential benefits of statins in patients undergoing surgery.
Footnotes
References
- 1.Hao PP, Chen YG, Wang JL, Ji WQ, Xue L, Liu XH, et al. Meta-analysis of the role of high-dose statins administered prior to percutaneous coronary intervention in reducing major adverse cardiac events in patients with coronary artery disease. Clin Exp Pharmacol Physiol. 2010;37:496–500. doi: 10.1111/j.1440-1681.2009.05339.x. [DOI] [PubMed] [Google Scholar]
- 2.Das S, Nanda SK, Bisoi AK, Wadhawan AN. Effect of preoperative statin therapy on early postoperative memory impairment after off-pump coronary artery bypass surgery. Ann Card Anaesth. 2016;19:38–44. doi: 10.4103/0971-9784.173018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berwanger O, Le Manach Y, Suzumura EA, Biccard B, Srinathan SK, Szczeklik W, et al. Association between pre-operative statin use and major cardiovascular complications among patients undergoing non-cardiac surgery: the VISION study. Eur Heart J. 2016;37:177–185. doi: 10.1093/eurheartj/ehv456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Youn YN, Park SY, Hwang Y, Joo HC, Yoo KJ. Impact of high-dose statin pretreatment in patients with stable angina during off-pump coronary artery bypass. Korean J Thorac Cardiovasc Surg. 2011;44:208–214. doi: 10.5090/kjtcs.2011.44.3.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sanders RD, Nicholson A, Lewis SR, Smith AF, Alderson P. Perioperative statin therapy for improving outcomes during and after noncardiac vascular surgery. Cochrane Database Syst Rev. 2013;7:CD009971. doi: 10.1002/14651858.CD009971.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dong L, Zhang F, Shu X. Usefulness of statins pretreatment for the prevention of postoperative atrial fibrillation in patients undergoing cardiac surgery. Ann Med. 2011;43:69–74. doi: 10.3109/07853890.2010.541491. [DOI] [PubMed] [Google Scholar]
- 7.van den Hoek HL, Bos WJ, de Boer A, van de Garde EM. Statins and prevention of infections: systematic review and meta-analysis of data from large randomised placebo controlled trials. BMJ. 2011;343:d7281. doi: 10.1136/bmj.d7281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Trezzi M, Blackstone EH, Sun Z, Li L, Sabik JF, 3rd, Lytle BW, et al. Statin therapy is associated with fewer infections after cardiac operations. Ann Thorac Surg. 2013;95:892–900. doi: 10.1016/j.athoracsur.2012.11.071. [DOI] [PubMed] [Google Scholar]
- 9.Hartholt NL, Rettig TC, Schijffelen M, Morshuis WJ, van de Garde EM, Noordzij PG. Preoperative statin therapy and infectious complications in cardiac surgery. Neth Heart J. 2014;22:503–509. doi: 10.1007/s12471-014-0581-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tleyjeh IM, Alasmari FA, Bin Abdulhak AA, Riaz M, Garbati MA, Erwin PJ, et al. Association between preoperative statin therapy and postoperative infectious complications in patients undergoing cardiac surgery: a systematic review and meta-analysis. Infect Control Hosp Epidemiol. 2012;33:1143–1151. doi: 10.1086/668019. [DOI] [PubMed] [Google Scholar]
- 11.Iannuzzi JC, Rickles AS, Kelly KN, Rusheen AE, Dolan JG, Noyes K, et al. Perioperative pleiotropic statin effects in general surgery. Surgery. 2014;155:398–407. doi: 10.1016/j.surg.2013.11.008. [DOI] [PubMed] [Google Scholar]
- 12.Bao-Xin Ma, Hua Li, Jing-Sen Li, Sui-Sheng Wu. Effect of statins on preventing infectious complications after surgery: Systematic review and meta-analysis. J Int Med Res. 2015;43:610–618. doi: 10.1177/0300060515583708. [DOI] [PubMed] [Google Scholar]
- 13.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 14.Spadaccio C, Pollari F, Casacalenda A, Alfano G, Genovese J, Covino E, et al. Atorvastatin increases the number of endothelial progenitor cells after cardiac surgery: a randomized control study. J Cardiovasc Pharmacol. 2010;55:30–38. doi: 10.1097/FJC.0b013e3181c37d4d. [DOI] [PubMed] [Google Scholar]
- 15.Chello M, Patti G, Candura D, Mastrobuoni S, Di Sciascio G, Agro F, et al. Effects of atorvastatin on systemic inflammatory response after coronary bypass surgery. Crit Care Med. 2006;34:660–667. doi: 10.1097/01.CCM.0000201407.89977.EA. [DOI] [PubMed] [Google Scholar]
- 16.Vukovic PM, Maravic-Stojkovic VR, Peric MS, Jovic M, Cirkovic MV, Gradinac S, et al. Steroids and statins: an old and a new anti-inflammatory strategy compared. Perfusion. 2011;26:31–37. doi: 10.1177/0267659110385607. [DOI] [PubMed] [Google Scholar]
- 17.Dunkelgrun M, Boersma E, Schouten O, Koopman-van Gemert AW, van Poorten F, Bax JJ, et al. Bisoprolol and fluvastatin for the reduction of perioperative cardiac mortality and myocardial infarction in intermediate-risk patients undergoing noncardiovascular surgery: a randomized controlled trial (DECREASE-IV) Ann Surg. 2009;249:921–926. doi: 10.1097/SLA.0b013e3181a77d00. [DOI] [PubMed] [Google Scholar]
- 18.Shokouhi S, Alavi Darazam I, Sharifi G, Gachkar L, Amirsardari A, Samadian M. Statins and postoperative infections: a randomized clinical trial. Jundishapur J Microbiol. 2014;7:e9456. doi: 10.5812/jjm.9456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abela GS, Vedre A, Janoudi A, Huang R, Durga S, Tamhane U. Effect of statins on cholesterol crystallization and atherosclerotic plaque stabilization. Am J Cardiol. 2011;107:1710–1717. doi: 10.1016/j.amjcard.2011.02.336. [DOI] [PubMed] [Google Scholar]
- 20.Yaktubay Dondas N, Sucu N, Coskun Yilmaz B, Kaplan HM, Ozeren M, Karaca MK, et al. Molecular mechanism of vasorelaxant and antiatherogenic effects of the statins in the human saphenous vein graft. Eur J Pharmacol. 2011;666:150–157. doi: 10.1016/j.ejphar.2011.05.013. [DOI] [PubMed] [Google Scholar]
- 21.Gismondi RA, Bedirian R, Pozzobon CR, Ladeira MC, Oigman W, Neves MF. Renin-angiotensin system blockade associated with statin improves endothelial function in diabetics. Arq Bras Cardiol. 2015;105:597–605. doi: 10.5935/abc.20150123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li DW, Li JH, Wang YD, Li GR. Atorvastatin protects endothelial colony forming cells against H2O2 induced oxidative damage by regulating the expression of annexin A2. Mol Med Rep. 2015;12:7941–7948. doi: 10.3892/mmr.2015.4440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kuhn EW, Liakopoulos OJ, Stange S, Deppe AC, Slottosch I, Choi YH, et al. Preoperative statin therapy in cardiac surgery: a meta-analysis of 90,000 patients. Eur J Cardiothorac Surg. 2014;45:17–26. doi: 10.1093/ejcts/ezt181. discussion 26. [DOI] [PubMed] [Google Scholar]
- 24.Zhang F, Dong L, Ge J. Effect of statins pretreatment on periprocedural myocardial infarction in patients undergoing percutaneous coronary intervention: a meta-analysis. Ann Med. 2010;42:171–177. doi: 10.3109/07853890903463976. [DOI] [PubMed] [Google Scholar]
- 25.Chen WT, Krishnan GM, Sood N, Kluger J, Coleman CI. Effect of statins on atrial fibrillation after cardiac surgery: a duration- and dose-response meta-analysis. J Thorac Cardiovasc Surg. 2010;140:364–372. doi: 10.1016/j.jtcvs.2010.02.042. [DOI] [PubMed] [Google Scholar]
- 26.Rattazzi M, Faggin E, Buso R, Di Virgilio R, Puato M, Plebani M, et al. Atorvastatin reduces circulating osteoprogenitor cells and T-cell RANKL expression in osteoporotic women: Implications for the bone-vascular axis. Cardiovasc Ther. 2016;34:13–20. doi: 10.1111/1755-5922.12163. [DOI] [PubMed] [Google Scholar]
- 27.Biasucci LM, Biasillo G, Stefanelli A. Inflammatory markers, cholesterol and statins: pathophysiological role and clinical importance. Clin Chem Lab Med. 2010;48:1685–1691. doi: 10.1515/CCLM.2010.277. [DOI] [PubMed] [Google Scholar]
- 28.Nie P, Li D, Hu L, Jin S, Yu Y, Cai Z, et al. Atorvastatin improves plaque stability in ApoE-knockout mice by regulating chemokines and chemokine receptors. PLoS One. 2014;9:e97009. doi: 10.1371/journal.pone.0097009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.López-Cortés LE, Gálvez-Acebal J, Del Toro MD, Velasco C, de Cueto M, Caballero FJ, et al. Effect of statin therapy in the outcome of bloodstream infections due to Staphylococcus aureus: a prospective cohort study. PLoS One. 2013;8:e82958. doi: 10.1371/journal.pone.0082958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Butt AA, Yan P, Bonilla H, Abou-Samra AB, Shaikh OS, Simon TG, et al. Effect of addition of statins to antiviral therapy in hepatitis C virus-infected persons: Results from ERCHIVES. Hepatology. 2015;62:365–374. doi: 10.1002/hep.27835. [DOI] [PubMed] [Google Scholar]
- 31.Emani S, Gunjiganur GV, Mehta DS. Determination of the antibacterial activity of simvastatin against periodontal pathogens, Porphyromonas gingivalis and Aggregatibacter actinomycetemcomitans: An in vitro study. Contemp Clin Dent. 2014;5:377–382. doi: 10.4103/0976-237X.137959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lobato LS, Rosa PS, Ferreira Jda S, Neumann Ada S, da Silva MG, do Nascimento DC, et al. Statins increase rifampin mycobactericidal effect. Antimicrob Agents Chemother. 2014;58:5766–5774. doi: 10.1128/AAC.01826-13. [DOI] [PMC free article] [PubMed] [Google Scholar]


