Abstract
Objectives:
To determine the epidemiology of non- transported emergency medical services (EMS) calls within the EMS system at Riyadh, Saudi Arabia, to identify factors that contributes to non-transport of patients by EMS provider, and to recommend suggestions for reduction in number of non-transported calls.
Methods:
Retrospective analysis of 1390 patient care reports (PCR) of non-transported cases responded to, and documented by the Saudi Red Crescent Authority (SRCA) emergency medical technicians (EMTs). All PCRs of non-transported cases from 10 EMS stations, in 3 consecutive months were examined. The SRCA EMTs management in Riyadh allocated all non-transported PCRs for 3 months (March-May 2014). Constructive data that includes patients demographics, scene characteristics, trip and timing information, length of stay, clinical and assessment data, and physician contact, or presence status were extracted from those PCRs.
Results:
Twenty-five percent of calls made during the study period were reported as non-transported calls. Seventy percent of non-transported calls were related to refusal by patient. Approximately 22.4% of non-transported calls were canceled by dispatch. Approximately 50% of non-transported patient were in the young age group (16-30 years). In 26% of non-transported calls, the field time was restricted to 15 minutes.
Conclusion:
More than half of the non-transported emergency calls were reported as refused by patient/relative, while approximately one quarter were reported as cancelled calls.
A large number of emergency medical services (EMS) calls are received and dispatched by the dispatch center of the Saudi EMS system provider, the Saudi Red Crescent Authority (SRCA). Riyadh, the capital city of the Kingdom of Saudi Arabia is home for 5.3 million people.1 At present, 65% of Riyadh population is comprised of citizens, and 35% of the population is comprised of expatriates.2 Non-transported calls affect the quality of the service provided and how efficiently EMS could have been provided, to other urgently needed patients. The non-transported EMS calls carry higher risk of increasing rate of morbidity and consequently litigation and legal action.3-5
The primary objective of this study was to determine the epidemiology of non-transported EMS calls within the EMTs system in Riyadh, Saudi Arabia, to identify factors that contribute to non-transport of patients by the EMTs provider, and to suggest recommendations for reduction in the number of non-transported calls.
Methods
We carried out aretrospective, descriptive document analysis study to scrutinize data in patient care reports (PCR) of non-transported emergency calls documented by responding SRCA EMS obtained from 10 EMS stations in Riyadh, Saudi Arabia for 3 consecutive months. The PCRs were obtained between March and May 2014. Constructive data that includes patients demographics, scene characteristics, trip and timing information, length of stay, clinical and assessment data, and physician contact, or presence status were extracted from those PCRs.
Results
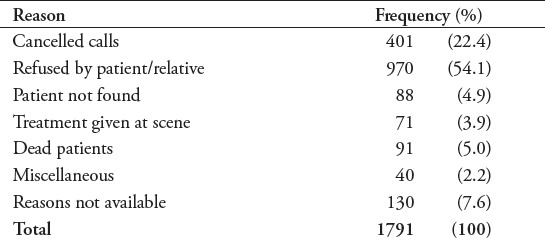
One thousand seven hundred and ninety-one emergency calls were reported as non-transported in the PCR, which accounts for 24.95%, during the study period. From these 1791 non-transported calls, 401 (22.4%) of calls were were cancelled by dispatch before arrival at the scene, for reasons not recorded in the PCR (Table 1). In 91 (5.1%) calls, the patients were found dead on arrival at the scene. The SRCA is not permitted to transport dead patients. Almost all PCRs related to the cancelled calls by dispatch were found 90% incomplete, so these PCRs were not included in the study of different variables. The remaining 1390 (77.6%) non-transported calls were studied for patient demographics and different variables. Table 1 summarizes the categories of non-transported call identified from the PDR.
Table 1.
Categories of the 1791 non-transported calls recorded the Saudi Red Crescent Authority emergency medical services.
Age, gender, and nationality
In this study, we found 50% (698) of non-transported patients ranging from 16-50 years of age with a peak between 16-30 years (30.9%) (n=430 patients), followed by patients >50 years, which accounts for 24.2% (n=336) patients. In a significant numbers of PCR the age of the patient is not mentioned (21.8%; n=303). The male to female ratio was 2:1 where males account for 722 (51.9%), and females patient account for 325 (23.4%). In a significant number of cases, the gender was not listed (n=343; (24.7%).
Call time and response time
In 1187 cases (85.4%), the call time was recorded in the PCR. Six hundred and nineteen (44.5%) of the non-transported patients made emergency calls during the day time (from 0600 hours to 1800 hours), while 568 (40.9%) of patients made their emergency calls during the night time (from 1800 hours to 0600 hours). In 203 (14.6%) cases, the call time could not be obtained from the PCR. In 80.9% of calls (n=1126), the response was within 25 minutes, and most of these calls (65.8%, n=915) were responded to within the first 15 minutes. The response time was limited to half an hour in 82.9% (n=1154) of calls. The average response time was lower at locations near to the dispatching SRCA centers; it was as low as 5 minutes.
Figure 2 summarizes the chief complaints by patient among non-transported calls recorded by the SRCA emergency medical services.
Figure 1.
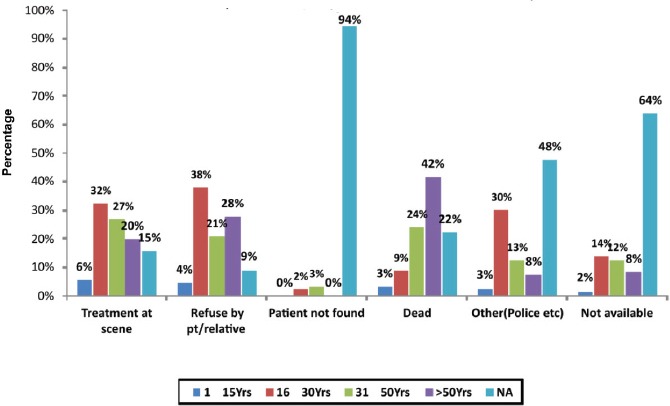
Reason for non-transport in relation to age among non-transported calls recorded by the Saudi Red Crescent Authority emergency medical services. pt - patient, NA - not applicable
Figure 2.
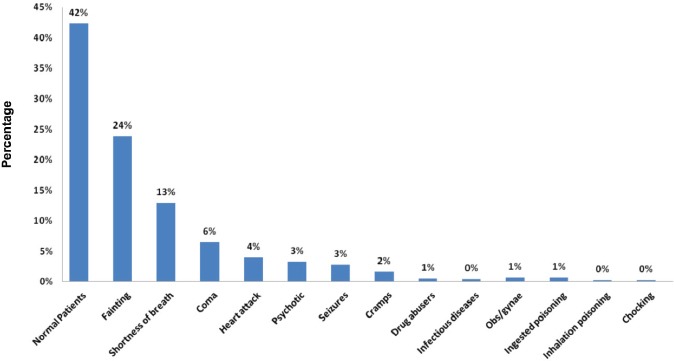
Chief complaints by patient distribution among non-transported calls recorded by the Saudi Red Crescent Authority emergency medical services.
Discussion
There is a lack of this type of study in the Kingdom of Saudi Arabia, which discuss the results in relation to area. However a significant proportion of cancelled calls (22.4%), by dispatch is a concern. This group of cancelled calls is the major contributor of non-transported calls, but nothing is recorded in the PCR. It is important to investigate the reasons for such a high number of cancelled emergency calls. Although there is no obvious reason, these cancelled calls by dispatch might reflect calls that were actually not in need of the ambulance service. The longer the response time, the greater are the chances for the cancellation of calls by patients. Longer waiting times might encourage the patient to use other means of transportation, or it might be that in the course of time they managed to call the family physician at home. In this study, there is a little evidence to relate the cancelled calls with response time of EMS provider as a relatively higher proportion of emergency call were responded to within the first 15 minutes, almost up to 65.8% (n=915). We postulate that if there is any connection between longer response time and call cancellation, it suggests the complete dissatisfaction of clients with the EMS provider. To further explore the reasons for cancelled calls, the EMS provider should follow up on all cancelled calls, which at present is not practiced by SRCA. Refusal by the patient or relative to be transported was another major proportion of patients, accounting for approximately 70% of all non-transported calls. To activate the EMS system, and then refuse to use the ambulance service for transport results in wastage of resources and time, which in turn affects the quality of EMS services to effectively serve other emergency calls. However, we need to consider the cultural factor that the female patient requires a male relative’s permission and company to ride in the ambulance. Another cultural factor could be unwillingness of the female patients to accompany the male EMS crew. This might affect the patient decision when they realize that the EMS crew are all males. A small proportion of non-transported calls (6.3%) is related to the not found category, where the ambulance crew failed to reach the scene or incident site. Although this group of not found patients is small, it has greater impact on patient outcome. As there is no address system available in the Kingdom of Saudi Arabia, the SRCA faces great challenges in reaching patients. The use of a GPS system by the SRCA will help in reducing the ratio of not found patients. Approximately 75% of non-transported patients with trauma were involved in motor vehicle collision. This matches with the age group, with a peak between 16-30 years, as motor vehicle accident young drivers are involved in most of the road side accidents in Riyadh.
Incomplete documentation with poor hand writing by the responding paramedics made it difficult to extract and analyze the data. This can produce errors in the study in term of patterns and follow up for non-transported patients. The SRCA have not yet established electronic reporting system. Such a system will be very effective in filling in sufficient data before submission of the report.
Little research has been published in this regard in Saudi Arabia. In Taiwan, 32% of emergency calls ended in patients not being transported to definitive facility as reported by Chen al el.6 Thirty percent emergency ambulances run as no transport runs resulting because of patients refusals in United States as reported by Hipskind et al7 Deborah Shaw et al,8 reveals that, of those who were not transported either due to patient’s refusal, or by EMS paramedics, almost half of them required further attention within a week, a significant minority required hospital admission and many agreed to be admitted following telephone advice from medical personnel. Dale et al’s9 study showed prior assessment of the call by paramedics to identify the non-urgent calls is helpful to identify the patients who are less likely to need emergency care. For those patients who refused to be transported, alternative methods such as community services, alternative transport, and specific interventions such as community falls programs was suggested by Snooks et al.10 Gardner et al’s,13 study was carried out to find out social and practical points to see if they are able to investigate the group of patients who use the emergency ambulance service without a medical need. This study revealed that 36% of cases were not in need of emergency assistance by EMS.
Study limitation
The limitation of this study is the expected incompleteness of large number of the collected PCRs resulting in large proportion of missing data. Another challenge comes in the lack of ability to read some of individual hand writing of those reports.
In conclusion, we have some suggestions for reducing the burden of non-transported calls, which in turn will improve the quality and efficiency of the emergency services provided by the SRCA. Emphasis should be made on quality of documentation by responding paramedics. As the majority of PCRs were incomplete. In particular, address and contact numbers, both mobile and land line along with the electronic ID should be made clear so that difficulties in future studies can be avoided and follow up with patients can be made, if needed. In the not found cases, we suggest that the use of mobile applications and GPS system can be effectively utilized to find the location of the patient. Some form of legislation can be introduced to avoid misuse and abuse of the emergency medical services.
Acknowledgements
All the effort of help provided by Dr. Saif Abu Zaid, Mr. Mazen Al Gamdi and Dr. Sameer Smasim from the SRCA to obtain the information is appreciated. Thanks are due to Dr. Mohammed Sami Al Sufi, Prince Sultan Bin Abdulaziz College of Emergency Medical Services, King Saud University for scientific assistance in this project.
Clinical Practice Guidelines.
Clinical Practice Guidelines must include a short abstract. There should be an Introduction section addressing the objective in producing the guideline, what the guideline is about and who will benefit from the guideline. It should describe the population, conditions, health care setting and clinical management/diagnostic test. Authors should adequately describe the methods used to collect and analyze evidence, recommendations and validation. If it is adapted, authors should include the source, how, and why it is adapted? The guidelines should include not more than 50 references, 2-4 illustrations/tables, and an algorithm.
References
- 1.General Authority for Statistics. Population. Statistical Yearbook 47 2011. Central Department of Statistics & Information. [Updated 2016; Accessed 2013 November 15]. Available from URL: http://www.stats.gov.sa/en .
- 2.Wikipedia. Demographics of Saudi Arabia [Internet] Wikipedia, The Free Encyclopedia. [Updated 2016 April 23, 17:36 UTC; Cited 2016 April 26]. Available from: https://en.wikipedia.org/w/index.phptitle=Demographics_of_Saudi_Arabia&oldid=716758776 .
- 3.Zachariah BS, Bryan D, Pepe PE, Griffin M. Follow-up and outcome of patients who decline or are denied transport by EMS. Prehospital and Disaster Medicine. 1992;7:359–364. [Google Scholar]
- 4.American College of Emergency Physicians. Continuous Quality Improvement in EMS. Dallas (TX): ACEP; 1992. pp. 298–230. [Google Scholar]
- 5.Selden BS, Schnitzer PG, Nolan FX. Medicolegal documentation of prehospital triage. Ann Emerg Med. 1990;19:547–551. doi: 10.1016/s0196-0644(05)82187-0. [DOI] [PubMed] [Google Scholar]
- 6.Chen JC, Bullard MJ, Liaw SJ. Ambulance use, misuse and unmet needs in a developing emergency medical services system. Eur J Emerg Med. 1996;3:73–78. doi: 10.1097/00063110-199606000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Hipskind JE, Gren JM, Barr DJ. Patients who refuse transportation by ambulance: a caes series. Prehosp Disaster Med. 1997;12:278–283. [PubMed] [Google Scholar]
- 8.Shaw D, Dyas JV, Middlemass J, Spaight A, Briggs M, Christopher S, et al. Are they really refusing to travel?A qualitative study of prehospital records. BMC Emergency Medicine. 2006;6:8. doi: 10.1186/1471-227X-6-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dale J, Willians S, Foster T, Higgins J, Snooks H, Crouch R, Hartley-Sharpe C, Glucksman E, George S. Safety of telephone consultation for non-serious emergency ambulance service patients. Qual Saf Health Care. 2004;13:363–373. doi: 10.1136/qshc.2003.008003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Snook HA, Dale J, Hartley-Sharpe C, Halter M. On-scene alternatives for emergency ambulance crews attending patients who do not need to ltravel to the accident and emergency department: a review of the literature. Emerg Med J. 2004;21:212–215. doi: 10.1136/emj.2003.005199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fischer AJ, O Halloran P, Littlehohns P, Kennedy A, Butson G. Ambulance economics. J Public Health Med. 2000;22:413–421. doi: 10.1093/pubmed/22.3.413. [DOI] [PubMed] [Google Scholar]
- 12.Gardner GJ. The use and abuse of the emergency ambulance service: some of the factors affecting the decision whether to call an emergency ambulance. Arch Emerg Med. 1990;7:81–89. doi: 10.1136/emj.7.2.81. [DOI] [PMC free article] [PubMed] [Google Scholar]


