Abstract
BACKGROUND/OBJECTIVES
Nutrition is a determinant factor of health in elderly people. Independent living in elderly people can be maintained or enhanced by improvement of nutritional behavior. Hence, the present study was conducted to determine the impact of Health Belief Model (HBM)-based intervention on the nutritional behavior of elderly women.
SUBJECTS/METHODS
Cluster-random sampling was used to assess the sample of this clinical trial study. The participants of this study attended a 12-week nutrition education program consisting of two (2) sessions per week. There was also a follow-up for another three (3) months. Smart PLS 3.5 and SPSS 19 were used for structural equation modeling, determination of model fitness, and hypotheses testing.
RESULTS
The findings indicate that intervention had a significant effect on knowledge improvement as well as the behavior of elderly women. The model explained 5 to 70% of the variance in nutritional behavior. In addition, nutritional behavior was positively affected by the HBM constructs comprised of perceived susceptibility, self-efficacy, perceived benefits, and barriers after the intervention program.
CONCLUSION
The results of this study show that HBM-based educational intervention has a significant effect in improving nutritional knowledge and behavior among elderly women.
Keywords: Nutritional behavior, elderly women, Health Belief Model
INTRODUCTION
There has been rapid growth in the elderly population due to reductions in fertility and mortality rates, increased life expectancy, and improvements in the health system [1]. Iran is no exception to this issue [2]. This fast growth in the elderly has created significant challenges, particularly in relation to health [3]. As the proportion of older people increases, their health status becomes a concern [4] Aging brings about an uneven increase in common illnesses such as degenerative disorders, stroke, cancer, dementia, and related disabilities [2]. As such, most patients admitted to hospital wards are older adults, and two-thirds of them have two or more chronic conditions [5]. Therefore, prevention of chronic conditions in the elderly is very vital to public health [6]. Nutrition is considered as an influential factor on health status of the elderly [7]. Improvement of nutritional behavior can help maintain independent living in the elderly and prevent age-related conditions [8].
Educational intervention has been shown to induce changes in the nutritional behavior of the elderly [9]. Numerous studies have investigated the efficacy of educational models such as the Health Belief Model (HBM), theory of planned behavior, and social cognitive theory on the nutritional behavior of the aged [10]. The most frequently used model for investigating behavioral changes and preventing diseases in the elderly is the HBM method [11]. Furthermore, the HBM has been shown to be an important instrument for assessing an individual's health perception [12]. The HBM contains different constructs, including perceived susceptibility, perceived severity, perceived benefits, perceived barriers, and perceived self-efficacy, and focuses on the cognitive aspects of an individual's belief such as perception, knowledge, and decisions [13]. The HBM asserts that elderly individuals should understand their elevated risk for potential severe health problems in order to induce a positive response [14]. Perceived barriers and benefits are the most influential variables of the HBM for predicting and explaining health-related behaviors [15]. Those who perceive more benefits than barriers are more probably to take action. In addition, self-efficacy plays a positive role in altering behavior of the elderly [12,14,16].
At the moment, little information is available on the nutritional status of older people. The majority of previous studies were conducted in aging centers or hospitals [17,18,19], and a limited number involved community-dwelling older adults. As such, this study aimed to determine the effectiveness of intervention in improving the nutritional behavior of the elderly in Urmia City based on the HBM. This study attempted to prove three hypotheses:
1: Nutritional knowledge obtained by elderly women will significantly influence constructs of the HBM after 3 and 6 months of intervention.
2: In elderly women, nutritional knowledge will considerably induce alteration of nutritional behavior after 3 and 6 months of intervention.
3: The HBM constructs will significantly alter nutritional behavior of the elderly women after 3 and 6 months of intervention.
SUBJECTS AND METHODS
Subjects
The participants of this study were community-dwelling elderly women aged 60 years and above residing in the North West of Iran (Urmia). Cluster-random sampling was carried out to choose a representative sample for the purpose of this study. First, Urmia was divided into four areas: west, east, north, and south. Thereafter, one health center from all available ones in each area was randomly selected. Two hundred out of 800 total recruited elderly women met the study inclusion criteria comprising a minimum of 5-year Urmia residency, being independent in daily activities, and without diabetes and food regimen.
Instruments
Data were collected using a researcher-made questionnaire divided into four sections, including demographic characteristics, nutritional knowledge, HBM constructs, and nutritional behavior. Subjects' knowledge of healthy nutrition was measured based on six items. The HBM constructs consisted of perceived susceptibility (four items), perceived severity (five items), perceived benefits (five items), perceived barrier (five items), and perceived self-efficacy (four items). A 5-point Likert scale, ranging from 0 to 5, was utilized to measure the HBM constructs. In addition, 21 items were used to assess respondents' eating behaviors related to food groups comprising meat and its products, fruits, vegetables, dairy products, drinks, and oils.
To evaluate the validity of the content, the questionnaire was sent to a panel of 10 academic members consisting of experts in the fields of gerontology, epidemiology, nutrition, and health education. The reliability of the knowledge (r = 0.98) and behavior (r = 0.87) sections of the questionnaire were calculated using Spearman's correlation coefficient. Cronbach's alpha test was used to determine the reliability of the HBM constructs of the questionnaire (r = 0.86).
An ethical approval letter was obtained from the Ethics Committee of Urmia Medical Sciences University (P6/92/4/47647) as well as Universiti Putra Malaysia [UPM/TNCPI/RMC/1.4.18.1(JKEUPM)/F1]. All eligible subjects signed the informed consent form after being informed of the procedure, potential benefits, and drawbacks of the study.
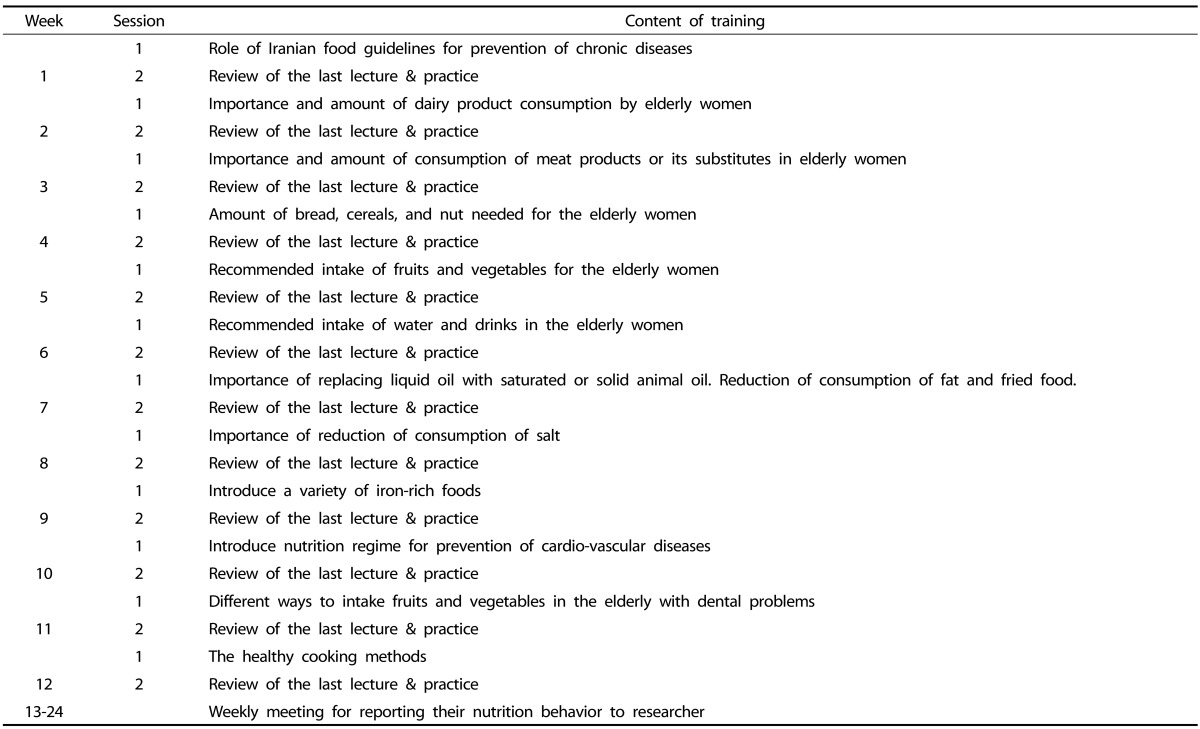
Data were collected at health centers before and after 3 and 6 months of intervention through a face-to-face interview technique. Questions were read aloud by trained and qualified assessors to elderly women, and answers were carefully recorded and written on the questionnaires. After familiarization with the procedure, the subjects participated in the nutrition education program for two sessions per week for 12 consecutive weeks. Each educational session lasted an average of 120 min (Table 1). Educational brochures were also given to the participants to review the presented nutritional information. The contact number of the researcher was provided at the end of the information sheet for any questions related to the research.
Table 1. Content of nutrition program for the elderly women over 3 months.
***Ministry of Health and Medical Education of Iran, 2014
Data analysis
Data were analyzed using the Statistical Package for the Social Sciences version 19 (SPSS® IBM, New York, U.S.A) and Partial Least Square (PLS). The significance level was set at 0.05. Descriptive statistics were used to report the means (m) ± standard deviations (SD) of baseline scores of the variables. Smart PLS was applied for testing the model fitness and hypotheses. The analytical method of PLS is a relatively new method in regression analysis [20]. PLS is a useful soft modeling approach to SEM, when there is a limited sample size or the data distribution is skewed [21]. Similar to structural equation modeling, PLS has two sub-models. The structural model specifies relationships between the latent variables while the measurement model specifies relationships between latent variables and their indices. Furthermore, it is possible to determine the standard regression coefficients for the paths by Smart PLS modeling. The fit indices in Smart PLS equal to or greater than 0.50 are acceptable [22]. The dependent variables scores at baseline were compared by one way ANOVA to detect any significant differences. All data were normally distributed using the Shapiro-Wilk test, Skewness, kurtosis, and histogram.
Adherence rate
The adherence rate for all subjects was calculated by the following formula:
(Sessions attended/total number of sessions) × 100.
The compliance rate of the intervention groups was 86%. This high adherence rate might be related to regular contact and reminding of the subjects to join the intervention sessions. Another reason may be associated with the social aspect of this program and the subjects' satisfaction with the nutrition education.
RESULTS
Baseline scores
Table 2 shows the baseline scores for knowledge, behavior, and belief of the participants. As depicted in this Table, there were no significant differences in scores of the dependent variables among the subjects from the four areas of Urmia.
Table 2. Baseline scores for knowledge, behavior, and belief of the participants.
Outcomes of intervention
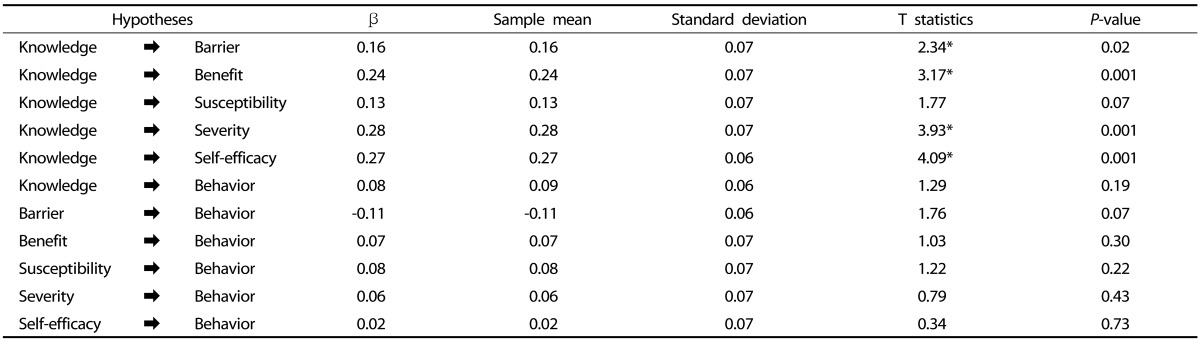
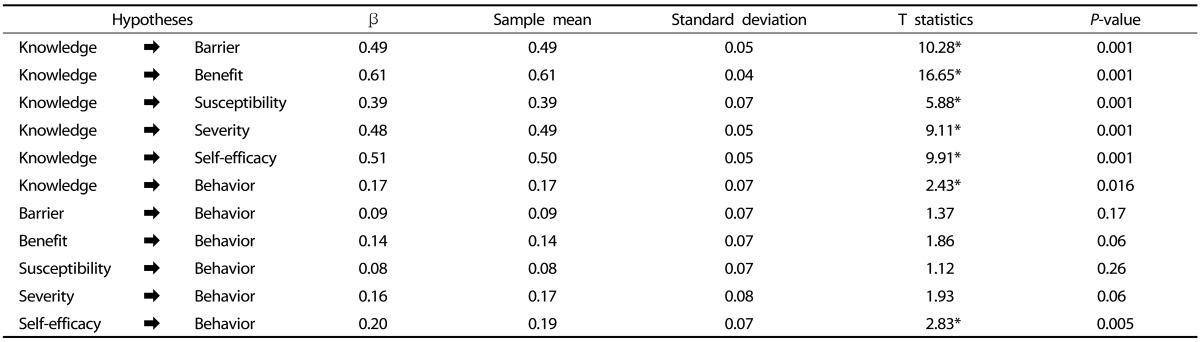
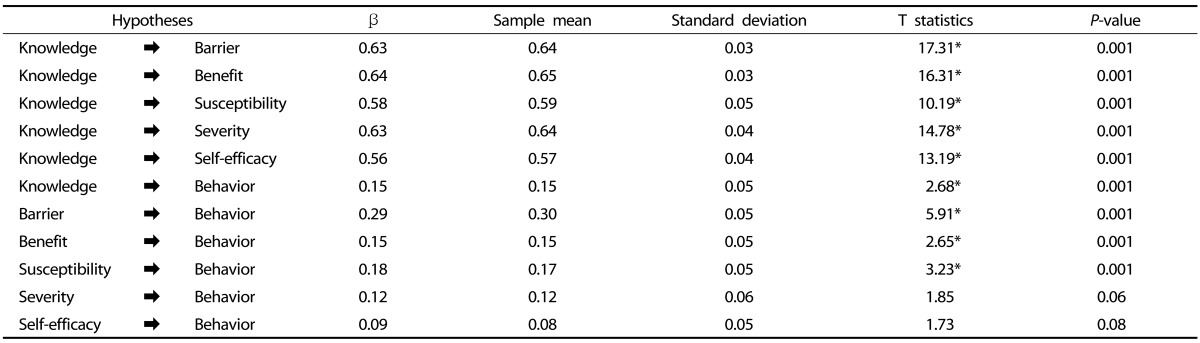
Tables 3, 4, and 5 present the path analysis for testing the hypotheses in the form of path coefficients at baseline and 3 or 6 months after intervention.
Table 3. Path coefficients of the study variables before intervention.
*The criterion for factor confirmation is a higher value of T than ± 1.96.
Table 4. Path coefficients of the study variables after 3 months of intervention.
*The criterion for factor confirmation is a higher value of T than ± 1.96.
Table 5. Path coefficients of the study variables after 6 months of intervention.
*The criterion for factor confirmation is a higher value of T than ± 1.96.
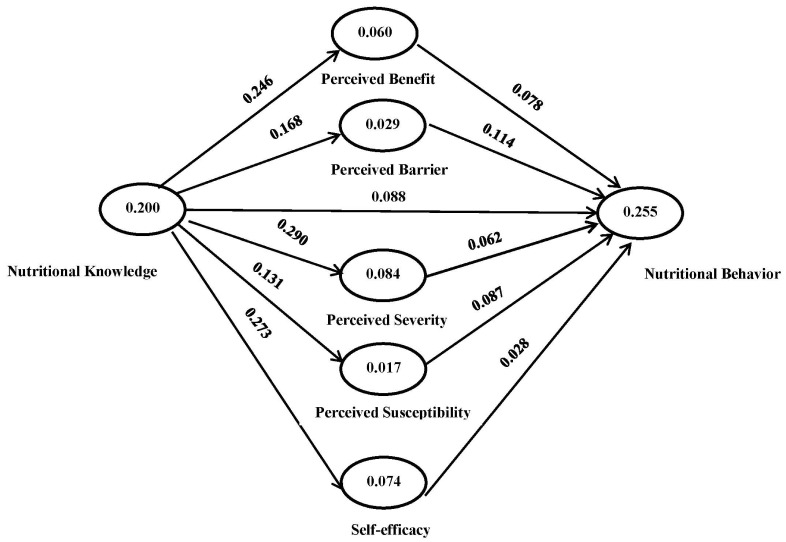
Based on Table 3, an increase in nutritional knowledge influences HBM constructs, consisting of perception of benefits, barrier, severity of disease, and self-efficacy (hypothesis one). However, the second and third hypotheses are not supported by the information in this Table. Fig. 1 shows that the HBM constructs predicts 5.5% (R2 = 0.055) of nutritional behavior changes among elderly women before the intervention.
Fig. 1. Structural model of nutritional behavior for the elderly women before intervention.
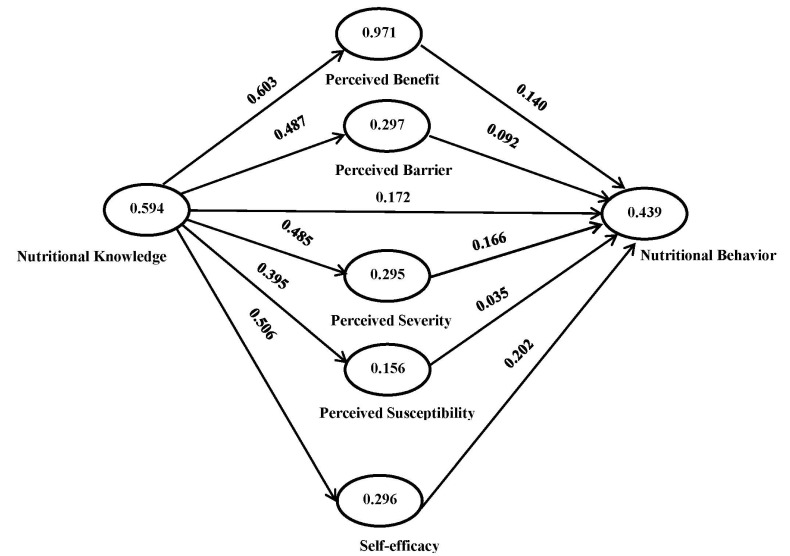
The information in Table 4 supports hypotheses 1 and 2. Furthermore, Table 4 shows that only self-efficacy is effective in improving the nutritional behavior of elderly women. Fig. 2 shows that 43.9% of nutritional behavior can be explained by the HBM constructs after 3 months of intervention (R2 = 0.439).
Fig. 2. Structural model of nutritional behavior for the elderly women 3 months after intervention.
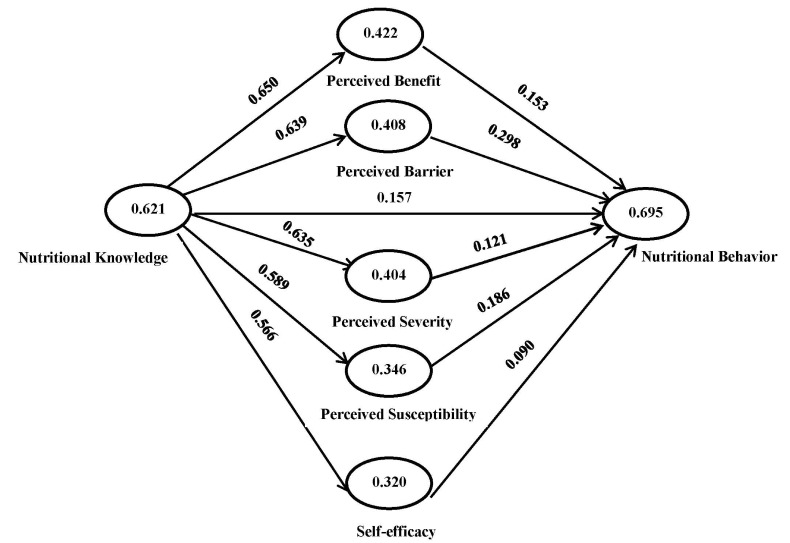
Based on the information in Table 5, hypotheses 1 and 2 are supported after 6 months of intervention. In terms of hypothesis 3, only perceived susceptibility, perception of benefits, and barrier of the model are supported (Table 5). In addition, Fig. 3 indicates that the HBM constructs explain 69.5% of nutritional behavior in elderly women 6 months after intervention (R2 = 0.695).
Fig. 3. Structural model of nutritional behavior for the elderly women 6 months after intervention.
DISCUSSION
Health education is a low-cost intervention technique for reducing the incidence, morbidity, and mortality of chronic disorders. Implementation of behavioral change theories into health education is fundamental for achieving desired behavioral changes leading to positive health outcomes [23].
The results of this study indicate that the intervention had direct effects on improving elderly women's knowledge and behavior related to healthy nutrition. Specifically, 5 to 70% of the nutritional behavior of elderly women could be explained by the HBM constructs. These findings are consistent with those who observed significant improvement in the poor nutritional behavior of the elderly [24,25,26]. However, in a similar study using HBM-based intervention for prevention of osteoporosis in menopausal women, Torshizi et al. [27] did not observe a significant difference between the intervention and control groups. This insignificant result may be related to the program duration (2 months), which was not long enough to alter healthy behaviors at a significant level.
On the other hand, the respondents showed poor scores for the HBM constructs at baseline (Table 3), although scores improved significantly after 3 months of intervention (Table 4). In addition, all HBM constructs except for perceived severity and self-efficacy significantly increased after a 3 month follow-up (Table 5). Likewise, Bayat et al. [28] reported a significant positive effect on the HBM constructs after a similar intervention duration. Furthermore, Sharifirad et al. [29], Khabazian & Rezaei [30], and Aghamolayee et al. [31] reported that all HBM constructs were important factors for improvement of health behavior. The lack of change in perceived severity may be related to the current study sample, who were healthy elderly subjects without any chronic conditions. Many previous studies have examined only a limited number of HBM constructs and focused on perceived self-efficacy. For instance, Swaim et al. [32] stated that self-efficacy has a positive effect on calcium intake among menopausal women. Equally, Rejeski et al. [33] in a clinical trial study observed significant improvement of nutritional behavior by increasing self-efficacy in elderly women. However, the present study considered a broad range of HBM constructs in three different occasions. Before the intervention, none of the constructs had a significant effect on the nutritional behavior of elderly women (Fig. 1). However, a 3 month educational program undertaken by elderly women resulted in increased and improved nutritional knowledge. Interestingly, in this stage, only self-efficacy had a positive effect on nutritional behavior (Fig. 2). After 6 months, perceived susceptibility, benefits, and barrier improved nutritional behavior considerably.
The results of this study support the strong effect of educational intervention on improving knowledge, belief, and behavior of elderly women. The HBM serves as an effective framework for modifying educational interventions for promoting preventive behavior in elderly women. Therefore, using a model-based education program and providing required facilities will help to maintain self-dependence in the elderly.
ACKNOWLEDGEMENTS
We would like to express our gratitude to the professors at the Medical Faculty of UPM, Malaysia as well as Tarbiat Modares University, Iran for careful and timely supervision of this project, which is part of a PhD dissertation. We would also like to extend our thanks to the Medical University of Urmia, Iran for their generous cooperation at the time of sampling.
References
- 1.McCutcheon M, Pruchno R. Introducing the international spotlight. Gerontologist. 2011;51:423–424. doi: 10.1093/geront/gnr070. [DOI] [PubMed] [Google Scholar]
- 2.Forsyth DR, Chia YC. How should Malaysia respond to its ageing society? Med J Malaysia. 2009;64:46–50. [PubMed] [Google Scholar]
- 3.Thanakwang K, Ingersoll-Dayton B, Soonthorndhada K. The relationships among family, friends, and psychological well-being for Thai elderly. Aging Ment Health. 2012;16:993–1003. doi: 10.1080/13607863.2012.692762. [DOI] [PubMed] [Google Scholar]
- 4.Haron SA, Sharpe DL, Masud J, Abdel-Ghany M. Health divide: economic and demographic factors associated with self-reported health among older Malaysians. J Fam Econ Issues. 2010;31:328–337. [Google Scholar]
- 5.Duque S, Freitas P, Silvestre J, Fernandes L, Pinto M, Sousa A, Batalha V, Campos L. Prognostic factors of elderly patients admitted in a medical intermediate care unit. Eur Geriatr Med. 2011;2:327–331. [Google Scholar]
- 6.Goetzel RZ, Shechter D, Ozminkowski RJ, Stapleton DC, Lapin PJ, McGinnis JM, Gordon CR, Breslow L. Can health promotion programs save medicare money? Clin Interv Aging. 2007;2:117–122. doi: 10.2147/ciia.2007.2.1.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oliveira MR, Fogaça KC, Leandro-Merhi VA. Nutritional status and functional capacity of hospitalized elderly. Nutr J. 2009;8:54. doi: 10.1186/1475-2891-8-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Knoops KT, de Groot LC, Kromhout D, Perrin AE, Moreiras-Varela O, Menotti A, van Staveren WA. Mediterranean diet, lifestyle factors, and 10-year mortality in elderly European men and women: the HALE project. JAMA. 2004;292:1433–1439. doi: 10.1001/jama.292.12.1433. [DOI] [PubMed] [Google Scholar]
- 9.Sahyoun NR, Pratt CA, Anderson A. Evaluation of nutrition education interventions for older adults: a proposed framework. J Am Diet Assoc. 2004;104:58–69. doi: 10.1016/j.jada.2003.10.013. [DOI] [PubMed] [Google Scholar]
- 10.Baranowski T, Cullen KW, Nicklas T, Thompson D, Baranowski J. Are current health behavioral change models helpful in guiding prevention of weight gain efforts? Obes Res. 2003;11:23S–43S. doi: 10.1038/oby.2003.222. [DOI] [PubMed] [Google Scholar]
- 11.Becker MH, Maiman LA, Kirscht JP, Haefner DP, Drachman RH. The Health Belief Model and prediction of dietary compliance: a field experiment. J Health Soc Behav. 1977;18:348–366. [PubMed] [Google Scholar]
- 12.Ceber E, Turk M, Ciceklioglu M. The effects of an educational program on knowledge of breast cancer, early detection practices and health beliefs of nurses and midwives. J Clin Nurs. 2010;19:2363–2371. doi: 10.1111/j.1365-2702.2009.03150.x. [DOI] [PubMed] [Google Scholar]
- 13.Dobe M. Health promotion for prevention and control of noncommunicable diseases: unfinished agenda. Indian J Public Health. 2012;56:180–186. doi: 10.4103/0019-557X.104199. [DOI] [PubMed] [Google Scholar]
- 14.Moore Q, Johnson A. Best Practices for Using Health Education to Change Behavior. Houston (TX): The James A. Baker III Institute for Public Policy of Rice Universit; 2015. [Google Scholar]
- 15.Baghianimoghadam MH, Shogafard G, Sanati HR, Baghianimoghadam B, Mazloomy SS, Askarshahi M. Application of the health belief model in promotion of self-care in heart failure patients. Acta Med Iran. 2013;51:52–58. [PubMed] [Google Scholar]
- 16.Orji R, Vassileva J, Mandryk R. Towards an effective health interventions design: an extension of the health belief model. Online J Public Health Inform. 2012;4:pii: ojphi.v4i3.4321. doi: 10.5210/ojphi.v4i3.4321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saeidlou SN, Merdol TK, Mikaili P, Bektaş Y. Assessment of the nutritional status of elderly people living at nursing homes in Northwest Iran. Int J Acad Res. 2011;3:463–472. [Google Scholar]
- 18.Wojszel ZB. Determinants of nutritional status of older people in long-term care settings on the example of the nursing home in Białystok. Adv Med Sci. 2006;51:168–173. [PubMed] [Google Scholar]
- 19.Saletti A, Lindgren EY, Johansson L, Cederholm T. Nutritional status according to mini nutritional assessment in an institutionalized elderly population in Sweden. Gerontology. 2000;46:139–145. doi: 10.1159/000022149. [DOI] [PubMed] [Google Scholar]
- 20.Henseler J, Sarstedt M. Goodness-of-fit indices for partial least squares path modeling. Comput Stat. 2013;28:565–580. [Google Scholar]
- 21.Wong KK. Partial least squares structural equation modeling (PLS-SEM) techniques using SmartPLS. Mark Bull. 2013;24:1–32. [Google Scholar]
- 22.Hulland J. Use of partial least squares (PLS) in strategic management research: a review of four recent studies. Strateg Manage J. 1999;20:195–204. [Google Scholar]
- 23.Champion VL, Skinner CS. The health belief model. In: Glanz K, Rimer BK, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. 4th ed. San Francisco (CA): Jossey-Bass; 2008. pp. 45–65. [Google Scholar]
- 24.Rousset S, Droit-Volet S, Boirie Y. Change in protein intake in elderly French people living at home after a nutritional information program targeting protein consumption. J Am Diet Assoc. 2006;106:253–261. doi: 10.1016/j.jada.2005.10.037. [DOI] [PubMed] [Google Scholar]
- 25.Young K, Bunn F, Trivedi D, Dickinson A. Nutritional education for community dwelling older people: a systematic review of randomised controlled trials. Int J Nurs Stud. 2011;48:751–780. doi: 10.1016/j.ijnurstu.2011.03.007. [DOI] [PubMed] [Google Scholar]
- 26.Kim HS, June KJ, Song R. Effects of nutrition education and exercise programs on perceived dietary behaviors, food intake and serum lipid profiles in elderly Korean women living in residential homes. Asian Nurs Res (Korean Soc Nurs Sci) 2007;1:35–47. doi: 10.1016/S1976-1317(08)60007-9. [DOI] [PubMed] [Google Scholar]
- 27.Torshizi L, Anoosheh M, Ghofranipour F, Ahmadi F, Houshyar-rad A. The effect of education based on Health Belief Model on preventive factors of osteoporosis among postmenopausal women. Iran J Nurs. 2009;22:71–82. [Google Scholar]
- 28.Bayat F, Shojaeezadeh D, Baikpour M, Heshmat R, Baikpour M, Hosseini M. The effects of education based on extended health belief model in type 2 diabetic patients: a randomized controlled trial. J Diabetes Metab Disord. 2013;12:45. doi: 10.1186/2251-6581-12-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sharifirad G, Entezari MH, Kamran A, Azadbakht L. The effectiveness of nutritional education on the knowledge of diabetic patients using the Health Belief Model. J Res Med Sci. 2009;14:1–6. [PMC free article] [PubMed] [Google Scholar]
- 30.Khabazian A, Rezaei N. The effect of education on the nutritional knowledge, attitude and practice in diabetic patients. Tolue Behdasht. 2003;2:57. [Google Scholar]
- 31.Aghamolayee T, Eftekhar H, Mohammad K. The application of Health Belief Model in changing the behavior in diabetic patients. Payesh. 2005;4:263–269. [Google Scholar]
- 32.Swaim RA, Barner JC, Brown CM. The relationship of calcium intake and exercise to osteoporosis health beliefs in postmenopausal women. Res Social Adm Pharm. 2008;4:153–163. doi: 10.1016/j.sapharm.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 33.Rejeski WJ, Brubaker PH, Goff DC, Jr, Bearon LB, McClelland JW, Perri MG, Ambrosius WT. Translating weight loss and physical activity programs into the community to preserve mobility in older, obese adults in poor cardiovascular health. Arch Intern Med. 2011;171:880–886. doi: 10.1001/archinternmed.2010.522. [DOI] [PMC free article] [PubMed] [Google Scholar]