Abstract
This study investigates the effect of a new Chinese massage technique named “press-extension” on degenerative lumbar with disc herniation and facet joint dislocation, and provides a biomechanical explanation of this massage technique. Self-developed biomechanical software was used to establish a normal L1–S1 lumbar 3D FE model, which integrated the spine CT and MRI data-based anatomical structure. Then graphic technique is utilized to build a degenerative lumbar FE model with disc herniation and facet joint dislocation. According to the actual press-extension experiments, mechanic parameters are collected to set boundary condition for FE analysis. The result demonstrated that press-extension techniques bring the annuli fibrosi obvious induction effect, making the central nucleus pulposus forward close, increasing the pressure in front part. Study concludes that finite element modelling for lumbar spine is suitable for the analysis of press-extension technique impact on lumbar intervertebral disc biomechanics, to provide the basis for the disease mechanism of intervertebral disc herniation using press-extension technique.
Keywords: Biomechanics, Massage technique, Intervertebral disc, Facet joint dislocation
1. Introduction
Lumber disc herniation is an important cause of lower back pains. Relevant research indicates that it is generally induced by the degenerated deformation of a disc due to too much labour or spine abnormality. The number of patients with intervertebral disc herniation is increasing. The lumbar discs in the spine make up a structure with a complex shape, which is the hinge and basis of spine activities. They can transfer labour loads, balance the body, stabilize the spine and absorb vibration (Lee and Teo, 2004). All the functions depend on the intact disc. In pathological cases such as disc herniation caused by too much load on the spine, anatomical morphology and biomechanical properties of the spine will have a series of changes.
At present, there are several types of therapy for disc herniation. Patients with heavy symptoms generally undergo surgery, which will change the biomechanical characteristics of lumbar after operation. These changes will affect the following therapy and recovery.
Recently, there is a growing tendency for disc herniation with non-operation therapies. Chinese massage, usually named “Tuina” in China, is commonly used in China (Zhang et al., 2015, Yang et al., 2014, Hou et al., 2015). Our treatment group proposed new kind of massage technique named “press-extension”, based on improvement of traditional extension massage technique for many years. However, the mechanism of this massage therapy for lumber disc herniation, e.g., the effectiveness and safety of press-extension Tuina, is not clear. Special biomechanical analysis in both lumbar disc herniation and changes of the disc stress–strain distribution states by this treatment is needed.
At present, there are two methods of biomechanical analysis in the lumbar. One is by experimentation and the other is creating a computational model. In vitro experiments conducted using fresh human specimens have inherent limitations (Mehta and Tewari, 2015). For example, human spinal specimens are difficult to get, often with poor bone quality thus not representing the conditions of a living individual. Moreover, there is always the risk of being infected by a virus. Thus, there is need for further models to be used in the field of spinal research. In the analyses of bone joints such as spines, which have complicated shape, load and boundary conditions, finite element (FE) methods can be a useful tool. Using special software, it allows the modelling of complex structures, and demonstrated detailed biomechanical characteristics of lumbar and provides intrinsic parameters (stress, strain, strain energy, etc.).
There were many research studies using FE modelling to investigate the spine biomechanics (Park et al., 2013, Dreischarf et al., 2014, Allison et al., 2015). Most of previous FE spine models mainly focused on spine bone, intervertebral disc and ligament, neglecting surrounding muscles, while the massage technique acts directly on the skin and muscles, which play the role of force transmission and diffusion. Besides, most lumbar disc degeneration models only considerate only changes of disc biomechanical properties (Park et al., 2013), ignoring related changes on the disc morphology, as well as facet joint dislocation in many cases.
In this study, we established a detailed FE model of complete normal lumbar integrated with surrounding muscles, and utilized graphics technique to build a degenerative lumbar model with disc herniation as well as facet joint dislocation, and then did biomechanical analysis on the press-extension massage technique for lumbar disc herniation. We believed that better understanding of the biomechanical characteristics of surgical procedures will ultimately lead to better diagnoses and treatments on intervertebral disc herniation.
2. Materials and methods
2.1. Hardware and software
Hardware employed was a standard desktop computer with Intel Pentium Core 2 Duo processor running at 2 × 2.83 GHz and 4 GB RAM, and an NVIDIA GeForce GTX 465 Graphics card. A specially designed modelling system – E-3D Biomedical Modeler (http://www.e-feature.net/content/fea) was employed to build a finite element model. ANSYS 12 was used as the finite element computation software.
2.2. Development of the FE model of the healthy lumbar spine
A young man with no history of present and past disc disease was selected as normal subject, with scan range of lumbar spine from L1 to S1. The CT slice images had a slice thickness of 0.8 mm, and the MRI slice images had a slice thickness of 1.5 mm. This study was approved by the Ethics Committee for the Protection of Human Subjects at Zhejiang Provincial Hospital of Traditional Chinese Medicine in accordance with the tenets of the Declaration of Helsinki, and informed consent was obtained from all participating individuals.
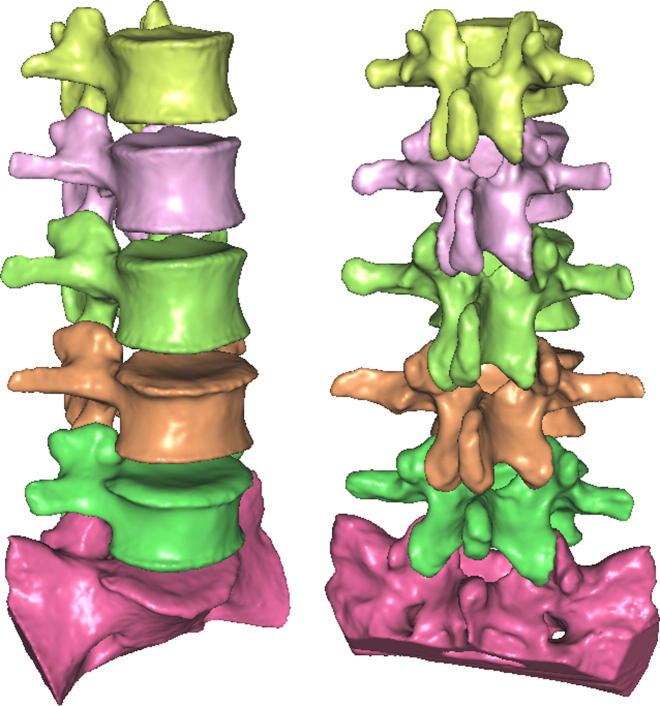
The scan images were exported to the E-3D Biomedical Modeler system in DICOM 3.0 format. Then, each vertebra region (L1–S1) was extracted from CT data by some semi-automatic segmentation tools, and corresponding 3D solid model was reconstructed precisely, such as in Fig 1, including the separation surfaces between cortical and trabecular regions. It should be noted that we ranged the thickness of cortical bone of 0.5–2.5 mm, taking consideration of the fact that CT tends to overestimate the thickness of cortical bone in this work (Silva et al., 1994). Then, these bony regions discretized to volumetric mesh elements of high quality.
Figure 1.
Accurate 3D reconstruction of the complete lumber vertebra (L1–S1).
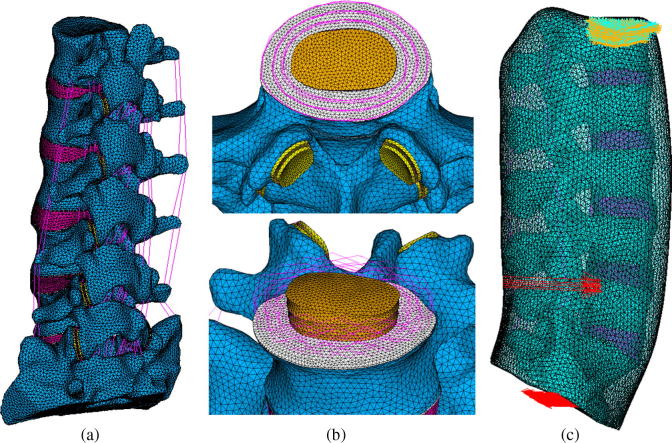
Each intervertebral disc was extracted from MRI data, and modelled as a central nucleus surrounded by an annular ground substance reinforced by fibres acting at approximately ±30° from the transverse plane, as shown in Fig2(b). The upper and lower surfaces of each disc were covered with the end plate of 0.6 mm. The fibres were modelled using a rebar definition. The nucleus was modelled as an incompressible fluid whose volume was approximately 48% of the entire disc volume.
Figure 2.
Finite element models of normal lumbar spine. (a) Lumbar model without muscles. (b) Local view of disc and facet joint. (c) Lumbar embedding in muscles and press-extension load conditions.
For each facet joint, the modelling tool first generated two layers of shell elements with thickness of 0.5 mm as the articular cartilage, as shown in Fig2(b); frictionless 3D surface-to-surface soft contact and an initial gap of 0.5 mm were assumed to exist between the superior and inferior articular cartilage (Park et al., 2013).
Several major spine ligaments were incorporated into the model, such as the anterior longitudinal (ALL), posterior longitudinal (PLL), ligamentum flavum (LF), capsular ligaments (CL), interspinal ligament (IS), supraspinal ligament (SS) and transverse ligaments (TL). The ligaments were defined as 3D nonlinear spring elements acting nonlinearly in tension only (Park et al., 2013, Zheng et al., 2012).
The lumbar muscles surrounding the lumbar spine is necessary to investigate the massage technique. Based on anatomical knowledge of lumbar muscles surrounding the lumbar spine, e.g., paraspinal muscles, quadratus lumborum muscle, and psoas major muscle, were generated by interactive graphics modelling function in E-3D software. Fig. 2(c) shows the final lumbar model embedding in muscles.
The complete lumbar model contains 939,532 10-node solid elements, 82,756 6-node 3D shell elements, 896 3D nonlinear spring element, 41,321 surface target elements, and 41,228 surface contact elements. The material and physical properties were adopted from previous validated finite element and experimental studies of lumbar spines (Park et al., 2013, Dreischarf et al., 2014, Allison et al., 2015, Silva et al., 1994).
2.3. Build degenerative lumbar with disc herniation and facet joint dislocation
The FE model of the degenerative lumbar spine was generated based on the developed FE model of the healthy lumbar spine. The degeneration was assumed at the L4–L5 FSU. The changes in geometry and material properties used to simulate the degeneration were adapted from the clinical classification of degeneration of the lumbar spine and the results of the previously published literature (Park et al., 2013, Silva et al., 1994, Zheng et al., 2012).
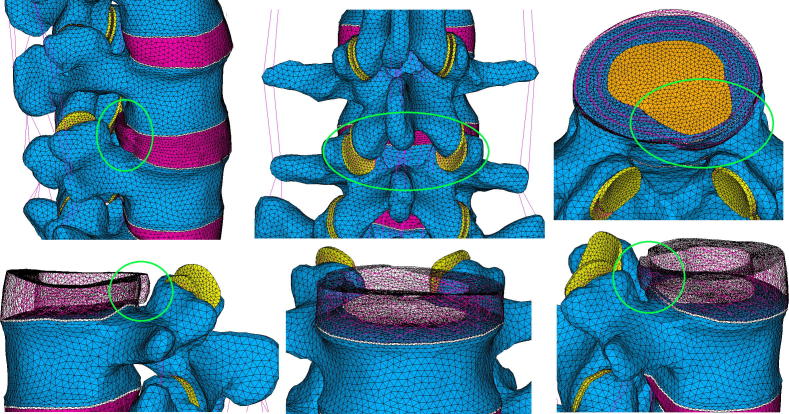
For intervertebral disc of L4–L5, the posterior annulus was weaken with inner annulus fibres tearing, to allow herniation of nuclear material into the outer annular structure as a contained protrusion, and part of the disc pass into the vertebral canal space as an extrusion, such as shown in Fig. 3. The materials of degenerative disc refer to the previous modelling literature (Park et al., 2013, Silva et al., 1994, Zheng et al., 2012).
Figure 3.
Finite element model of degenerative lumbar with disc herniation and staggered facet joint.
Furthermore, it is reported that the facet joint orientation and facet tropism are presented as the potential anatomical predisposing factors for lumbar degenerative changes that may lead in turn to early degeneration and herniation of the corresponding disc or degenerative spondylolisthesis (Kim et al., 2013, Lee et al., 2006, Kunakornsawat et al., 2007, Chadha et al., 2013). For the degenerative model in this study, the staggered facet joint was simulated by reverse rotating the superior and inferior articular cartilage at an angle of 5° in the horizontal direction, and reverse moving the superior and inferior articular cartilage at distance of 5 mm in the vertical direction, such as shown in Fig. 3.
2.4. Validation of lumbar FE model of the healthy lumbar spine
One important step in developing a finite element model (FEM) is to validate the model established with the experimental data. With 10 N m of torque load, Yamamoto et al. (1989) tested the lumbar spine in flexion, extension, lateral bending and rotation, and the average range of motion (ROM) was 38.7°, 25.9°, 8.9°, and 28.8°. Chen et al. (1999) also measured the average ROM of lumbar spine in flexion, extension, lateral bending and rotation, at 44.95° ± 8.34°, 23.74° ± 4.63°, 30.14° ± 5.04°, and 23.27° ± 4.1°. Obviously, it is more suitable to choose the normal physiological lumbar model to compare those experiments.
The nodes of the inferior surface of the L5 vertebral body in normal lumbar model were completely fixed in all directions, and 10 N m of pure moment was applied on the top of the L1 vertebra for 6 loading conditions: flexion, extension, left lateral bending, right bending, left rotation, and right rotation. The simulation result of the ROM of lumbar spine for these loading conditions was as follows: 40.8°, 30.3°, 30.5°, 28.7°, 30.2°, 27.6°. All data of this study were within the standard deviation of the average ROM values reported by previous experimental study.
2.5. Loading and boundary conditions
To simulate the clinically relevant loading scenarios for the press-extension massage technique, the nodes of the upper surface of the L1 vertebral body were completely fixed in all directions, the S1 vertebra was subjected to 30° of post extension, and 300 N pressure was applied on the spot near L4–L5 spinous process with lower-right offset of 5 mm on the skin surface, such as shown in Fig.2(c).
3. Results
Under the loading of the press-extension massage technique, the biomechanics of the degenerative intervertebral disc L4–L5 was carefully analysed and compared.
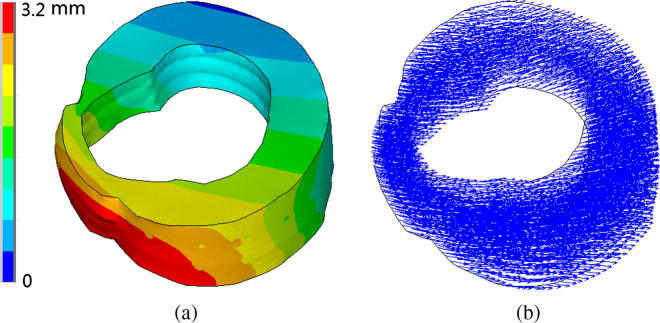
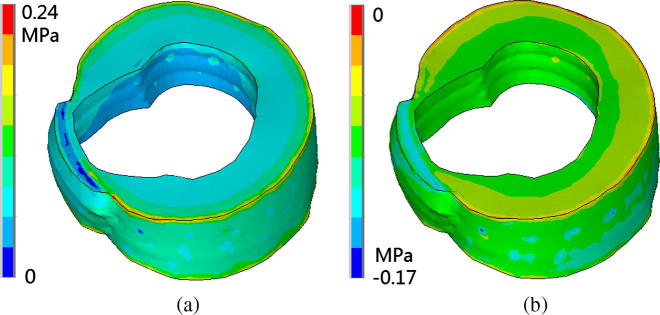
The contour view of the forward displacement of annulus fibrosus in degenerative lumbar is illustrated in Fig. 4, with displacement value pattern and displacement direction vectors. We can see that the displacement of back part is significantly greater than that of the front part, which should has suppression effect on the disc herniation.
Figure 4.
Forward displacement contour of annulus fibrosus in degenerative lumbar. (a) Displacement value pattern. (b) Displacement direction vectors.
This phenomenon can also be obtained from the analysis of stress. Fig. 5 demonstrated the maximum principal stress of annulus fibrosus in degenerative lumbar, with tensile stress and compressive stress. We can see that the tensile stress of the disc herniation part was small, while the compressive stress was very significant. Combined with the displacement result aforesaid, it is obvious that the annulus fibrosus was under pressure towards the centre part of the disc, which would lead to density increasing in the middle region of the disc.
Figure 5.
Maximum principal stress of annulus fibrosus in degenerative lumbar. (a) Tensile stress. (b) Compressive stress.
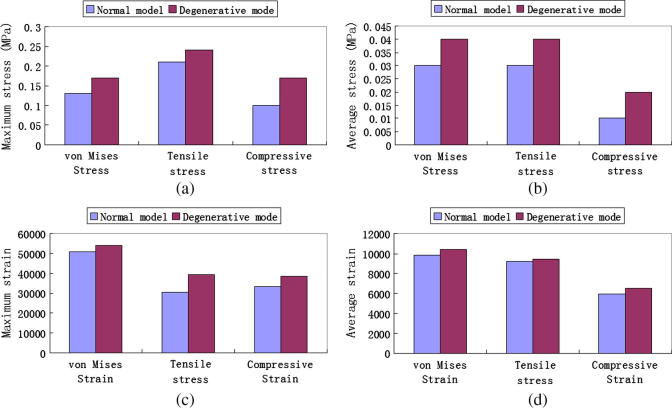
The maximum and average stress and strain values of disc nucleus of L4–L5 are illustrated in Fig. 6, including the normal lumbar and degenerative lumbar. The stress values of degenerative disc nucleus were all larger than those of normal disc nucleus. The maximum compressive stress value increased about 70% compared to the normal disc. The increasing trend was the same for the strain values, although the change was not so obviously.
Figure 6.
Stress and strain of disc nucleus of L4–L5. (a) Maximum stress. (b) Average stress. (c) Maximum strain. (d) Average strain.
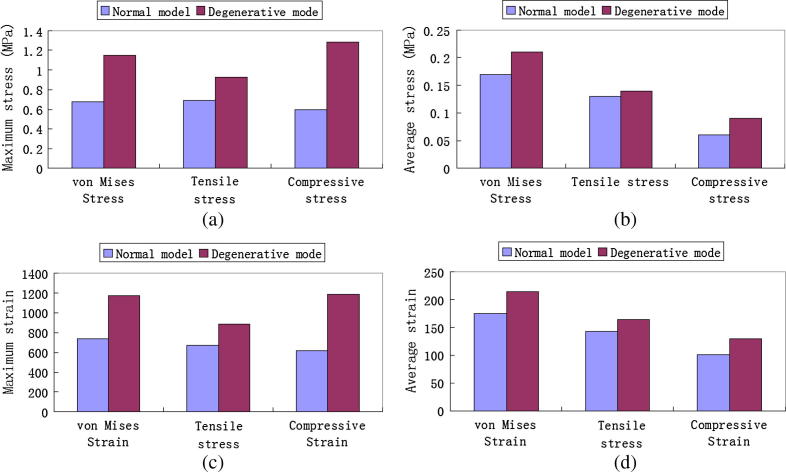
The maximum and average stress and strain values of articular cartilage on facet joint of L4–L5 are illustrated in Fig. 7, including the normal lumbar and degenerative lumbar. The stress values of articular cartilage on staggered facet joint were all larger than those of normal one. The maximum compressive stress value of staggered facet joint increased about 115%. The increasing trend was the same for the strain values, and the maximum compressive strain value also increased about 94% compared to the normal one.
Figure 7.
Stress and strain of articular cartilage on facet joint of L4–L5. (a) Maximum stress. (b) Average stress. (c) Maximum strain. (d) Average strain.
4. Discussion and conclusion
The intervertebral disc consists of endplate, annulus fibre, and nucleus pulposus. The penetration between endplate and the cancellous bone will change feebly if the disc bears an abnormal force and thus can affect the nutrient supply of the annulus fibre, which results in the degeneration of the disc. An annulus fibre with poor nutrient supply is easily ruptured if the stress concentration on this region is high. The nucleus pulposus will dissociate from the disc along the ruptured region. At last, the disc extrudes out (Riches et al., 2002), which leads to lumber disc herniation.
Lumber disc herniation is an important cause of lower back pains. At present, there are several types of therapy for disc herniation (Nicolas, 2006). Patients with heavy symptoms due to degenerative deformation of the lumbar spine, particularly those with extreme discomfort and pains, generally undergo surgery. The operation usually takes decompression therapy of the disc by resecting or dissolving the nucleus pulposus and thus relieves the pain caused by high compression of nucleus pulposus. Currently, chemonucleolysis and resection are two general methods of decompression for the degenerative lumbar disc. The biomechanical characteristics of lumbar will change after operation. These changes will affect the following therapy and recovery.
Recently, there is a growing tendency for disc herniation with non-operation therapies, such as physical exercises, medication therapy, traction therapy, acupuncture and moxibustion therapy. Chinese massage, usually named “Tuina” in China, is an important component of traditional Chinese medicine (TCM), parallel to internal medicine, acupuncture, moxibustion, life cultivation and rehabilitation of Chinese medicine. Massage had been noted in “Yellow Emperor’s Canon of Medicine”, the classic of TCM. It was pointed out that Chinese massage originated and developed in the central region of China. It had the function of unblocking or dredging the meridians and collateral, promoting “qi” to activate blood, and eliminating cold to stop pain.
Our treatment group proposed new kind of massage technique named “press-extension”, based on improvement of traditional extension massage technique for many years. However, the mechanism of this massage therapy for lumber disc herniation, e.g., the effectiveness and safety of press-extension Tuina, is not clear. In this study, we established a detailed FE model of complete normal lumbar integrated with surrounding muscles, and utilized graphics technique to build a degenerative lumbar model with disc herniation (Wilke et al., 2006, Zheng et al., 2012) as well as facet joint dislocation (Kim et al., 2013, Lee et al., 2006, Kunakornsawat et al., 2007, Chadha et al., 2013), and then did biomechanical analysis on the press-extension massage technique for lumbar disc herniation.
According to the simulation results, the stress and strain values of degenerative disc were all larger than those of normal one, with the maximum compressive stress increased about 70%. The stress and values of articular cartilage on staggered facet joint were all larger than those of normal one, the maximum compressive stress value increased about 115%, and the maximum compressive strain value increased about 94%. In addition, the displacement of back disc part near herniation is significantly greater than that of the front part, and the tensile stress of the disc protrusion region was small, while the compressive stress was very significant. These results demonstrated that the massage technique press-extension has the suppression effect on the disc herniation, promoting the protruding portion towards the normal position. This provides us a biomechanical explanation of this massage technique. We believed that better understanding of the biomechanical characteristics of surgical procedures will ultimately lead to better diagnoses and treatments on intervertebral disc herniation.
Acknowledgements
The research was supported by Zhejiang Provincial Natural Science Foundation of China (No. LY13H290010), Public Technology and Social Development Project of Zhejiang Province Science and Technology Department (No. 2014C33G2120093) and the National Natural Science Foundation of China (No. 60903136).
Footnotes
Peer review under responsibility of King Saud University.
References
- Allison L., Clouthier H., Hosseini S., Maquer G., Zysset P.K. Finite element analysis predicts experimental failure patterns in vertebral bodies loaded via intervertebral discs up to large deformation. Med. Eng. Phys. 2015;37:599–604. doi: 10.1016/j.medengphy.2015.03.007. [DOI] [PubMed] [Google Scholar]
- Chadha M., Sharma G., Arora S.S., Kochar V. Association of facet tropism with lumbar disc herniation. Eur. Spine J. 2013;22:1045–1052. doi: 10.1007/s00586-012-2612-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen G., Yu B., Du J., Qu S. A comparative study of three-dimensional movements of lumbar spine in the old and the young people. J. Biomed. Eng. 1999;16:438–440. [PubMed] [Google Scholar]
- Dreischarf M., Zander T., Shirazi-Adl A., Puttlitz C.M., Adam C.J. Comparison of eight published static finite element models of the intact lumbar spine: predictive power of models improves when combined together. J. Biomech. 2014;47:1757–1766. doi: 10.1016/j.jbiomech.2014.04.002. [DOI] [PubMed] [Google Scholar]
- Hou P.W., Fu P.K., Hsu H.C., Hsieh C.L. Traditional Chinese medicine in patients with osteoarthritis of the knee. J. Tradit. Complement. Med. 2015;5:182–196. doi: 10.1016/j.jtcme.2015.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H.J., Chun H.J., Lee H.M., Kang K.T. The biomechanical influence of the facet joint orientation and the facet tropism in the lumbar spine. Spine J. 2013;13:1301–1308. doi: 10.1016/j.spinee.2013.06.025. [DOI] [PubMed] [Google Scholar]
- Kunakornsawat S., Ngamlamaidt K., Tungsiripat R., Prasartritha T. The relationship of facet tropism to lumbar disc herniation. J. Med. Assoc. Thai. 2007;90:1337–1341. [PubMed] [Google Scholar]
- Lee D.Y., Ahn Y., Lee S.H. The influence of facet tropism on herniation of the lumbar disc in adolescents and adults. J. Bone Joint Surg. Br. 2006:520–523. doi: 10.1302/0301-620X.88B4.16996. [DOI] [PubMed] [Google Scholar]
- Lee K.K., Teo E.C. Effects of laminectomy and facetectomy on the stability of the lumbar motion. Med. Eng. Phys. 2004;26:183–192. doi: 10.1016/j.medengphy.2003.11.006. [DOI] [PubMed] [Google Scholar]
- Mehta C.R., Tewari V.K. Biomechanical model to predict loads on lumbar vertebra of a tractor operator. Int. J. Ind. Ergonom. 2015;47:104–116. [Google Scholar]
- Nicolas J.S. Spinal manipulation in patients with disc herniation: a critical review of risk and benefit. Int. J. Osteopath. Med. 2006;9:77–84. [Google Scholar]
- Park W.M., Kim K., Kim Y.H. Effects of degenerated intervertebral discs on intersegmental rotations, intradiscal pressures, and facet joint forces of the whole lumbar spine. Comput. Biol. Med. 2013;43:1234–1240. doi: 10.1016/j.compbiomed.2013.06.011. [DOI] [PubMed] [Google Scholar]
- Riches P.E., Dhillon N., Lotz J., Woods A.W., McNally D.S. The internal mechanics of the intervertebral disc under cyclic loading. J. Biomech. 2002;35:1263–1271. doi: 10.1016/s0021-9290(02)00070-2. [DOI] [PubMed] [Google Scholar]
- Silva M.J., Wang C., Keaveny T.M., Hayes W.C. Direct and computed tomography thickness measurements of the human, lumbar vertebral shell and endplate. Bone. 1994;15:409–414. doi: 10.1016/8756-3282(94)90817-6. [DOI] [PubMed] [Google Scholar]
- Wilke H.J., Rohlmann F., Neidlinger-Wilke C., Werner K., Claes L., Kettler A. Validity and interobserver agreement of a new radiographic grading system for intervertebral disc degeneration: Part I. Lumbar spine. Eur. Spine J. 2006;15:720–730. doi: 10.1007/s00586-005-1029-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamamoto I., Panjabi M.M., Crisco T. Three-dimensional movements of the whole lumbar spine and lumbosacral joint. Spine. 1989;14:1256–1260. doi: 10.1097/00007632-198911000-00020. [DOI] [PubMed] [Google Scholar]
- Yang X., Zhao H., Wang J. Chinese massage (Tuina) for the treatment of essential hypertension: a systematic review and meta-analysis. Complement. Ther. Med. 2014;22:541–548. doi: 10.1016/j.ctim.2014.03.008. [DOI] [PubMed] [Google Scholar]
- Zhang Y., Tang S., Chen G., Liu Y. Chinese massage combined with core stability exercises for nonspecific low back pain: a randomized controlled trial. Complement. Ther. Med. 2015;23:1–6. doi: 10.1016/j.ctim.2014.12.005. [DOI] [PubMed] [Google Scholar]
- Zheng Q., Liao S.H., Wei W., Liu Y.S., Shi S.Y. FEM analysis of complex lumbar spinal stenosis decompression and intervertebral fusion. Chin. J. Biomed. Eng. 2012;31:566–571. [Google Scholar]