Abstract
Purpose
To assess the long-term visual acuity (VA) outcome after congenital cataract surgery at Imam Hossein Medical Center (Tertiary Referral Center) (2004–2014).
Methods
In this descriptive study, records of 120 patients with a history of congenital cataract surgery were studied. Those with traumatic, metabolic cataract, aged <5 years at the last visit who were not able to respond VA testing accurately and follow-up < 6 months were excluded. Cases with incomplete files were recalled and reexamined. Finally, the records of 42 patients (71 eyes) were included.
Results
In this study, 20 males and 22 females with a mean age of 11.80 ± 6 years at their last visit were studied. Bilateral and unilateral cataract was seen in 69% and 31% of cases, respectively. Posterior and anterior subcapsular opacity was the most common (53.70%) and rarest (1.90%) type of congenital cataract, respectively. The mean age at the time of operation and surgical interval was 65 ± 66.6 (range: 1–200) and 12.9 ± 23.5 (range: 0–96) months, respectively. The most common method of refractive error correction was pseudophakia plus glasses (56.3%) with the mean best corrected visual acuity (BCVA) of 0.29 ± 0.28 LogMAR., The mean BCVA was 0.7 ± 0.53 LogMAR for aphakic patients correcting by glasses. In our study, amblyopia (56%), glaucoma (23.90%), and posterior capsular opacity (16.40%) were observed during their follow-ups on an average of 76 ± 65 months (median: 60, range: 6–240). Unilateral cataract, aphakia, nystagmus, female gender, and strabismus were risk factors of VA loss.
Conclusion
Based on our results, 56% of cases showed amblyopia. It could be due to late operation (especially in unilateral cases), longer surgical interval between two eyes, and no compliance of amblyopia therapy. Early detection through screening may reduce the rate of amblyopia. Refractive errors, visual acuity, amblyopia, glaucoma, posterior capsular opacity, and compliance of amblyopia therapy should be checked regularly at follow-up visits.
Keywords: Congenital cataract surgery, Best corrected visual acuity (BCVA), Complications
Introduction
Visual system is developed in children as long as sharp, clear and focused images are formed on the retina of both eyes. Otherwise, amblyopia is observed. Therefore, early detection and surgery as well as follow-up visits have significant roles in the restoration of a child's vision in the case of congenital cataract with significant media opacity.1
There are 200,000 children around the world and 133,000 in developing countries that suffer from blindness due to congenital cataract.2 In general, the prevalence of congenital cataract as the most common preventable cause of blindness in childhood has been reported from 1 to 15 per 10,000 children, while it is from 1 to 3 per 10,000 births in developing countries.3, 4
Unfortunately, in many cases, even after early surgery, long-term follow-up (at least up to the age of 10) is not properly instituted, and varying degrees of amblyopia have been reported despite wearing appropriate eye glasses, contact lenses, or implantation of intra ocular lenses (IOL).5
In Birch et al.’s study, the best corrected visual acuity (BCVA) after congenital cataract surgery was 0.60 LogMAR (20/80 Snellen equivalent) or better only in 53% of children with the age range of 3–7 years old, which is not considered an acceptable outcome.5 Tomkins et al. reported BCVA from light perception to 0.20 LogMAR (20/32 Snellen equivalent) with better visual results by early surgery.2 Abdelmoaty et al. studied the records of 100 operated congenital cataract children and found BCVA of 0.30 LogMAR (20/40 Snellen equivalent) in bilateral cases with the mean age of 8.90 ± 8.70 months and 1.00 LogMAR (20/200 Snellen equivalent) in unilateral cases with the mean age of 5.75 ± 4.61 months at the time of their surgery.6 Late surgery and unilateral cataract have been reported as risk factors of lower post-operative visual acuity, and posterior capsular opacity, glaucoma, and amblyopia have been found as the most common post-operative long-term complications according to different studies.6, 7, 8
The aim of this study was to determine the long-term visual outcomes and complications after congenital cataract surgery at Imam Hossein Medical Center, Tehran, Iran during 2004–2014.
Methods
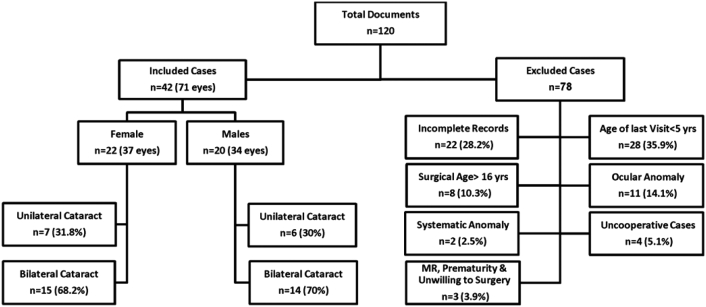
In this descriptive study, the records of 120 children who had a history of congenital cataract surgery up to 16 years old during the past 10 years were reviewed. The patients who had lens opacities (>1 mm centrally or opacities that interfere with dilated pupil funduscopic examination9) up to age one year were included. Children with mental retardation, less than 5 years at the last visit that were not able to respond VA testing, traumatic/metabolic/radiation/medications and other types of cataract, ptosis, uncooperative children, combined congenital glaucoma and cataract, and a follow-up of less than 6 months were excluded. According to our inclusion and exclusion criteria, children with lens opacity diagnosed in the first year of life and who were operated before age of 16 years were included. In case of incomplete documents, the parents were asked to bring their child for further examination, if it was not possible the incomplete files were excluded. Finally, the data of 71 eyes (42 cases) were completed as illustrates on Fig. 1. The study was approved by the Ethics Committee of the Ophthalmic Research of the Imam Hossein Medical Center, Tehran, Iran.
Fig. 1.
Flowchart of our study procedure. MR: mental retardation; yrs: years; n: number.
According to patient documents, data including age, sex, laterality, type of cataract, age of operation, surgical interval between the 2 eyes, accompanying baseline strabismus (>±10pd), different stages of surgical technique (aspiration, posterior capsulectomy and anterior vitrectomy), with or without IOL implantation were recorded.
After cataract surgery, in all cases, refractive error was measured using retinoscope (HEINE BETA 200; US). VA was estimated according to the age of our cases during their follow-up visits by red reflex assessment, CSM test, and Snellen E-test at a 6-m distance through their appropriate glasses. Only BCVA of ≥ 5 years were included in this study. Stereoacuity was also tested using Titmus Stereoacuity test. Slit-lamp examination was performed to rule out any abnormality of cornea, pupil, anterior chamber, and other anterior segment components. Intra ocular pressure (IOP) was measured using applanation Goldmann tonometry or Tonopen (Reichert TONO-PEN AVIA® Tonometer, Richert Inc. Depew, NY, USA). Funduscopic examination was performed using indirect ophthalmoscope (HEINE OMEGA® 500, Germany) through dilated pupil 45 min after instillation of Tropicamide 1%.
Functional amblyopia was considered if BCVA of each eye was 0.30 LogMAR (20/40 Snellen equivalent) or worse, or there was a difference of two LogMAR lines between two eyes. Posterior capsular opacity (PCO) was indicated if any central whitening and/or wrinkling of the posterior capsular lens was found in slit-lamp examination, post-operatively. Glaucoma was considered if (IOP) was measured more than 20 mmHg under general anesthesia using TONO-PEN or Perkins in younger children or by applanation tonometry in older cases in addition to signs of optic neuropathy.10 Optic disc appearance and cup/disc ratio were checked by funduscopic examinations. Microphthalmia was considered as axial length less than 17 mm up in the first year of age.11 Parental cooperation was defined according to their compliance for at least 50% of recommended patching hours by asking them at follow-up visits.12 Partial compliance was considered if parents did not have compliance more than 50% of a day in all periodic follow-ups.
In all cases who had IOL implantation, the IOL was inserted into the posterior chamber or the capsular bag during the primary operation in 38 cases or secondary operation in 12 cases. Furthermore, A-scan ultrasound technique was applied regarding ocular axial length measurements for implanted population. Immediate post-operative hyperopic refraction was considered for IOL power calculation up to age 2 or 3 based on handheld keratometry and biometry under general anesthesia before cataract surgery. IOL power calculation in older children who cooperated with these tests before surgery, have planned for emmetropia with no anisometropia (less than 3D) compared to their fellow eyes' refraction.
Statistical analysis
To describe data, mean, standard deviation, median, range, frequency, and percentage were used.
Normal distribution of data was checked by Kolmogorov–Smirnov test and Q–Q plot. Spearman correlation was used to obtain the relation between variables. Generalized Estimating Equations (GEEs) were used to consider the correlation in bilateral cases when comparing the groups. All statistical analysis was performed by SPSS software (IBM SPSS Statistics, Version 22.0. Armonk, NY: IBM Corp). p-value less than 0.05 was considered statistically significant.
Results
In this study, data of 71 eyes (42 patients) with a history of congenital cataract surgery were analyzed. Of these, 20 children were male and 22 were female with the mean age of 11.80 ± 6 years (5–26 years) at their last visit. There was no case with a history of exposure to X-ray during the fetal period, being in incubator, and also having epilepsy during childhood. Among 42 cases, one child had a history of mother's smoking, one was premature, and two had a history of cataract in their family. There was no post-operative report of anterior capsular opacity or phimosis, but there were two patients with anterior pupillary membrane formation which was removed by surgery.
As Table 1 shows, 29 (69%) and 13 (31%) children had bilateral and unilateral congenital cataract, respectively. The median age of cataract operation and interval between two eyes were 3 years and 3 months, respectively. Patients were followed for an average of 76 ± 65 months (median: 60, range: 6–240).
Table 1.
Demographic data of our patients.
| Parameters | Value | |
|---|---|---|
| Age at the last visit (years) | Mean ± SD | 11.8 ± 6 |
| Median (range) | 11 (5–26) | |
| Sex (%) | Male | 20 (47.6%) |
| Female | 22 (52.4%) | |
| Nystagmus | No | 36 (85.7%) |
| Yes | 6 (14.2%) | |
| Microphthalmia | No | 63 (88.7%) |
| Yes | 8 (11.3%) | |
| Laterality | OD | 10 (23.8%) |
| OS | 3 (7.1%) | |
| OU | 29 (69.0%) | |
| Strabismus | No | 22 (52.3%) |
| Yes | 20 (47.6%) | |
| Age of surgery (months) | Mean ± SD | 65 ± 66.6 |
| Median (range) | 37 (1–200) | |
| ≤3 | 15 (21.1%) | |
| >3 | 56 (78.9%) | |
| ≤6 | 21 (29.6%) | |
| >6 | 50 (70.4%) | |
| ≤12 | 30 (42.3%) | |
| >12 | 41 (57.7%) | |
| Surgical Interval (months) | Mean ± SD | 12.9 ± 23.5 |
| Median (range) | 3 (0–96) | |
| Follow Up (months) | Mean ± SD | 76 ± 65 |
| Median (range) | 60 (6–240) |
OD: oculus dexter; OS: oculus sinister; OU: oculus uterque; SD: standard deviation.
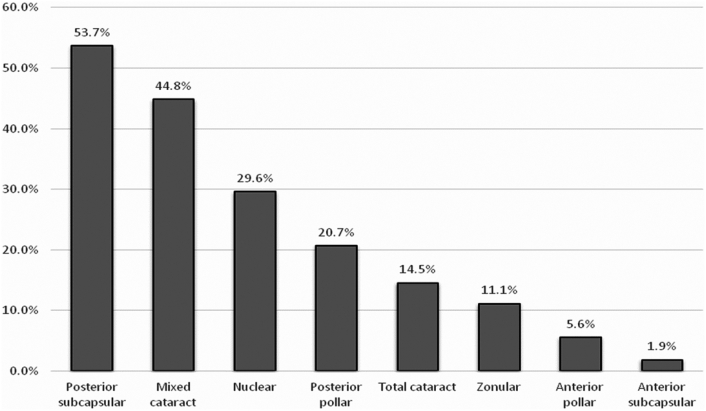
Fig. 2 illustrates the prevalence of different types of congenital cataract in our participants. In our study, posterior and anterior subcapsular cataracts were the most common and the least prevalent type of congenital cataracts, respectively.
Fig. 2.
Different types of cataract. Mixed cataract: two or more types of cataract.
Table 2 shows various techniques of cataract surgery as well as post-operative optical correction. Combined lens aspiration (90.1%), posterior capsulectomy (94.4%), and anterior vitrectomy (91.5%) were the most common surgical procedure. IOL was implanted in 76% of children with mean age of 9.1 ± 4.8 (range: 2–24) years at primary surgery and 24% with mean age of 4.3 ± 2.1 years (range: 2–7.75) at secondary operation. Post-operatively, in cases with PCO (n = 11, 16.40%), posterior capsulotomy was performed in significant PCOs by neodymium-doped yttrium aluminium garnet (Nd:YAG laser, n = 2) or surgery (n = 1). The combination of IOL implantation and glasses was the most common method used for correcting refractive errors in 56.30% of cases. Although amblyopia therapy was recommended in all cases, only 21.7% followed their patching orders, completely and regularly.
Table 2.
Surgical and optical managements of congenital cataract in our participants.
| Parameters | Value | ||
|---|---|---|---|
| Lensectomy | No | 7 (9.9%) | |
| Yes | 64 (90.1%) | ||
| Aspiration | No | 65 (91.5%) | |
| Yes | 6 (8.5%) | ||
| Plus P. capsulectomy | No | 4 (5.6%) | |
| Yes | 67 (94.4%) | ||
| Plus Ant. Vitx | No | 6 (8.5%) | |
| Yes | 65 (91.5%) | ||
| IOL | No | 21 (29.6%) | |
| Yes | 50 (70.4%) | ||
| Primary | 38 (76.0%) | ||
| Secondary | 12 (24.0%) | ||
| Refractive Correction | Glasses | 17 (23.9%) | |
| C.Lens | 4 (5.6%) | ||
| IOL | 10 (14.1%) | ||
| IOL plus Glasses | 40 (56.3%) | ||
| Amblyopia | No | 31 (43.7%) | |
| Yes | 40 (56.3%) | ||
| Compliance of amblyopia therapy | No | 20 (49.3%) | |
| Partial | 12 (29.0%) | ||
| Yes | 2 (21.7%) |
ECCE: extra capsular cataract extraction; P: posterior; Ant: anterior; Vitx: vitrectomy.
IOL: intra ocular lens; C.Lens: contact lens; Phaco: phacoemulsification; ASP: aspiration.
Table 3 shows that maximum value of 0.0 LogMAR BCVA (equal to 20/20) was achieved after IOL implantation. Peripheral stereopsis (100–3000 s of arc) was also observed in 23 children.
Table 3.
Visual and refractive outcomes of our participants.
| Parameters | p | ||||
|---|---|---|---|---|---|
| BCVA (LogMAR) | Total | Mean ± SD | 0.46 ± 0.43 | ||
| Median (range) | 0.3 (0–1.8) | ||||
| Correction | Glasses | Mean ± SD | 0.7 ± 0.53 | 0.190b | |
| Median (range) | 0.6 (0.1–1.7) | ||||
| C.Lens | Mean ± SD | 0.7 ± 0 | |||
| Median (range) | 0.7 (0.7–0.7) | ||||
| IOL | Mean ± SD | 0.29 ± 0.28 | |||
| Median (range) | 0.26 (0–1) | ||||
| IOL + Glasses | Mean ± SD | 0.37 ± 0.39 | |||
| Median (range) | 0.22 (0–1.8) | ||||
| SE (D) | IOL | No | Mean ± SD | 11.76 ± 3.54 | <0.001a |
| Median (range) | 11.13 (6.75–20) | ||||
| Yes | Mean ± SD | −1.55 ± 1.91 | |||
| Median (range) | −1 (−6.5 to 1.25) | ||||
| Stereopsis (sec/arc) | No | 19 (45.2%) | |||
| Yes | 23 (54.8%) | ||||
| Value | Mean ± SD | 681 ± 960 | |||
| Median (range) | 400 (30–3000) |
BCVA: best corrected visual acuity; LogMAR: logarithm minimum angle of resolution; C.Lens: contact lens; IOL: intra ocular lens; Sph: spherical; SE: spherical equivalent; sec: second.
Based on Mann–Whitney test.
Based on Kruskal–Wallis test.
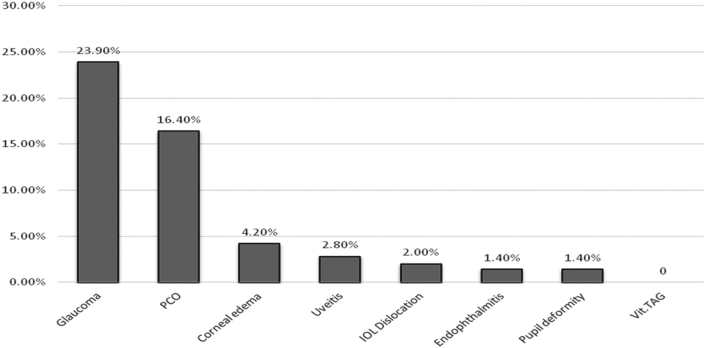
As Fig. 3 shows, glaucoma (23.90%) was the most common long-term surgical complication in this study.
Fig. 3.
Post-operative complications of our participants. PCO: Posterior Capsular Opacity; Vit: vitreous; IOL: Intra Ocular Lens.
According to our results, unilateral cataract (p < 0.001), nystagmus (p = 0.007), female gender (p = 0.007), strabismus (p = 0.009), and all forms of congenital cataract were risk factors of VA loss. Zonular cataract had better visual outcomes (p = 0.048, Table 4).
Table 4.
Risk factors of post-operative best corrected visual acuity.
| Best corrected visual acuity |
||||
|---|---|---|---|---|
| Parameters | Mean ± SD | Median (range) | pa | |
| Sex | Male | 0.31 ± 0.33 | 0.22 (0–1.8) | 0.007 |
| Female | 0.59 ± 0.48 | 0.52 (0–1.7) | ||
| Laterality | OD | 0.94 ± 0.49 | 0.7 (0.22–1.8) | <0.001 |
| OS | 0.93 ± 0.21 | 1 (0.7–1.1) | ||
| OU | 0.35 ± 0.36 | 0.3 (0–1.7) | ||
| Nystagmus | No | 0.42 ± 0.45 | 0.3 (0–1.8) | 0.007 |
| Yes | 0.66 ± 0.22 | 0.7 (0.22–1) | ||
| Strabismus | No | 0.3 ± 0.24 | 0.26 (0–1) | 0.009 |
| Yes | 0.63 ± 0.53 | 0.7 (0–1.8) | ||
| Posterior subcapsular cataract | No | 0.34 ± 0.25 | 0.3 (0–1) | 0.364 |
| Yes | 0.56 ± 0.53 | 0.3 (0.05–1.7) | ||
| Anterior subcapsular cataract | No | 0.44 ± 0.43 | 0.3 (0–1.7) | 0.197 |
| Yes | 1 ± 0.0 | 1 (1–1) | ||
| Zonular cataract | No | 0.49 ± 0.45 | 0.3 (0–1.7) | 0.048 |
| Yes | 0.17 ± 0.13 | 0.16 (0–0.4) | ||
| Nuclear cataract | No | 0.44 ± 0.45 | 0.3 (0–1.8) | 0.962 |
| Yes | 0.48 ± 0.53 | 0.3 (0–1.7) | ||
| Total cataract | No | 0.43 ± 0.41 | 0.3 (0–1.7) | 0.153 |
| Yes | 0.62 ± 0.53 | 0.3 (0.22–1.7) | ||
| Mixed cataract | No | 0.43 ± 0.32 | 0.3 (0–1.2) | 0.780 |
| Yes | 0.53 ± 0.53 | 0.3 (0.05–1.7) | ||
| Compliance | No | 0.45 ± 0.4 | 0.3 (0–1.7) | 0.934 |
| Yes/No | 0.34 ± 0.22 | 0.3 (0–0.9) | ||
| Yes | 0.47 ± 0.49 | 0.3 (0–1.8) | ||
| Age of surgery (months) | ≤3 | 0.56 ± 0.44 | 0.3 (0.1–1.7) | |
| >3 | 0.32 ± 0.29 | 0.25 (0–0.7) | ||
| ≤6 | 0.49 ± 0.41 | 0.3 (0–1.7) | 0.206 | |
| >6 | 0.78 ± 0.60 | 0.7 (0.1–1.7) | ||
| ≤12 | 0.78 ± 0.60 | 0.7 (0.1–1.7) | ||
| >12 | 0.37 ± 0.37 | 0.22 (0–1.8) | ||
| Glaucoma | No | 0.46 ± 0.46 | 0.3 (0–1.8) | 0.984 |
| Yes | 0.44 ± 0.34 | 0.52 (0–1.1) | ||
| PCO | No | 0.42 ± 0.37 | 0.3 (0–1.8) | 0.992 |
| Yes | 0.43 ± 0.49 | 0.3 (0–1.7) | ||
PCO: posterior capsular opacity; IOL: intra ocular lens; SD: standard deviation; OD: oculus dexter; OS: oculus sinister; OU: oculus uterque.
Based on Mann–Whitney or Kruskal–Wallis test, whenever appropriate. We found no statistical relation between the surgical interval of two eyes and final BCVA (r = −0.166, p = 0.218).
Discussion
In the present study, 71 eyes (42 cases) with a history of congenital cataract surgery were included. Their mean age at the last visit was 11.80 ± 6 years old. Long-term BCVA was 0.29 ± 0.28 LogMAR in cases with IOL, 0.70 ± 0.53 LogMAR in cases corrected with glasses and 0.37 ± 0.39 LogMAR in cases with IOL plus glasses.
Epidemiological characteristics
There were 29 patients (69%) with bilateral and 13 (31%) with unilateral congenital cataract. Lee and Msamati et al. also reported more bilateral cases in their studies.13, 14
Sensory strabismus was presented in 47.60% (n = 20) of our cases, which was in line with the study by Demirkilinc et al. {59.5% of their cases were strabismic after long-term (>1 year) follow-up examinations}.15 In fact, ocular deviation represents our failure to restore good post-operative VA.
The most common type of congenital cataract in our study was PSCO, while in South Korea13 the nuclear cataract was the most common type. Genetic factors or demographic characteristics in each region and society may have an efficient role in this regard.
Surgical factors
The mean age of surgery in our cases was 65 ± 66.60 months (median: 37, range: 1 to 288), while in the studies of the UK,7, 16 China,8 Ethiopia,2 and Kuwait,6 the children were operated at the mean age of 12 months, 8.7 weeks, 5.6 months, 7.21 years, and 12 months, respectively. Our mean age of surgery was closer to the results from Ethiopia than other countries. Based on the above reports, it should be noted that the diagnosis and surgery of congenital cataract were unfortunately more delayed in some developing countries compared to developed countries. The reason could be due to late diagnosis and therefore late surgery, less severity or peripheral lens opacity with acceptable visual acuity, unavailable subspecialty of pediatric ophthalmologist in the rural regions, poor economic status, or a combination of some the above mentioned etiologies.
Better visual acuity was achieved among children who had surgery at less than 6 months (0.49 ± 0.41 LogMAR) compared to older ones (0.78 ± 0.60 LogMAR) in our study. Although this difference was noticeable clinically, it was not statistically significant (Table 4). Studies of Ethiopia,2 Britain,16 and China8 found statistically better visual outcomes in younger surgical ages.
The mean surgical interval of two eyes in this study was 12.9 ± 23.50 months (median: 3, range: 0 to 96), and it was longer compared to Jain et al.'s study16 with the mean surgical interval of 3.80 days. The reason could be due to unequal lens opacities in both eyes or poor socioeconomic status of child's families.
In our study, the common method of congenital cataract surgery was lensectomy combined with posterior capsulectomy and anterior vitrectomy with or without IOL implantation, as others.8, 13
IOL implantation was performed in 50 eyes (70.40%), 38 cases of which (76%) were implanted at the same operation (primary implantation), and 12 cases of which (24%) with secondary implantation due to age limitation (<2 years in bilateral and <1 year for unilateral cases), deep amblyopia secondary to retinopathy of prematurity (ROP), or eccentric fixation (EF), uveitis, glaucoma, fundus lesion, and ocular anomalies like microphthalmia. Magli et al.17 also implanted their cases in primary or secondary operations as well.
Correction of aphakia and visual outcomes
To correct the residual refractive errors after congenital cataract surgery with IOL implantation (70.40%), the glasses were needed in 40 cases (56.30%). Only 4 of 13 unilateral cataract cases were corrected by contact lenses. It seems some contact lens problems such as infection, loss, and cost made its usage limited, except in some unilateral cases who have been operated in the early infancy period.
The mean BCVA after IOL implantation was 0.29 ± 0.28 LogMAR. Tomkins et al.2 shows the good BCVA after IOL implantation as well (92% of their patients presented final BCVA of 0.20 LogMAR).
In our study, the mean BCVA of bilateral congenital cataract was more than unilateral cases (p < 0.001) as indicated in studies of Chak7 and Abdelmoaty et al.,6 and there was better BCVA in males compared to females (p = 0.007). Eriksen et al.18 reported that males had better prognosis for good BCVA. It may be due to cultural beliefs that sons are going to be responsible for the family in the future; therefore, parents take more care of them.
In the present study, 54.80% of our cases achieved peripheral stereopsis after surgery, which was in line with other studies reporting 0%–91% of increased stereopsis, post-operatively.8, 19
Parental cooperation in amblyopia therapy was evaluated using a questionnaire, and VA improvement during examination can be also considered useful evidence in this regard. Eriksen et al.18 indicated the efficient role of parents in amblyopia therapy, but Ye et al.8 found little effect of the parental cooperation in this regard, similar to ours.
Unilateral cataract, nystagmus, female gender, strabismus, and all types of congenital cataract, except zonular, were considered as the risk factors of our post-operative BCVA. According to other studies, lack of parental compliance for amblyopia therapy,7 longer surgical interval,16 and delayed surgery18 were also reported as the risk factors of the post-operative BCVA.
The mean follow-up of our study was 5 years (6–240 months), which was comparable to other studies.8, 16, 19
Complications
Our long-term complications were PCO (16.40%) and glaucoma (23.90%) as reported in other publications like Astle et al.’s study with 22.70% PCO as a common surgical complication and Abdelmoaty et al.'s, with 4% PCO and 2% glaucoma, postoperatively.6, 19
Limitations of the study
The study design (existing data) was one of our limitations. We tried to overcome it by completing some files through calling and asking some questions and recruitment of some cases for complementary examinations. A small sample size was another limitation of our study. It was due to our limiting inclusion criteria since we wanted to prevent the effect of other factors on final VA to increase internal validity of our study.
In the current study, late diagnosis, late operation, long surgical interval, short-term post-operative follow-up, and some long-term complications are major findings.
Based on our results, 56% of our cases showed post-operative amblyopia. It could be due to late operation (especially in unilateral cases), longer surgical interval between two eyes, and no compliance of amblyopia therapy. Early detection through screening may reduce the rate of amblyopia. All practitioners should check refractive errors, visual acuity, amblyopia, glaucoma, posterior capsular opacity, and compliance of amblyopia therapy in each post-operative visit.
Conflict of interest
The authors have no conflict of interest with the subject matter of this manuscript.
Footnotes
Peer review under responsibility of the Iranian Society of Ophthalmology.
References
- 1.World Health Organization Preventing Blindness in Children. 2000. http://www.who.int/ncd/vision2020_actionplan/documents/WHO_PBL_00.77 Available at: Last Accessed July 7, 2011. [Google Scholar]
- 2.Tomkins O., Ben-Zion I., Moore D.B., Helveston E.E. Outcomes of pediatric cataract surgery at a tertiary care center in rural southern Ethiopia. Arch Ophthalmol. 2011;129:1293–1297. doi: 10.1001/archophthalmol.2011.268. [DOI] [PubMed] [Google Scholar]
- 3.Hu D.N. Prevalence and mode of inheritance of major genetic eye diseases in China. J Med Genet. 1987;24:584–588. doi: 10.1136/jmg.24.10.584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lin H., Yang Y., Chen J. Congenital cataract: prevalence and surgery age at Zhongshan Ophthalmic Center (ZOC) PLoS One. 2014;9:e101781. doi: 10.1371/journal.pone.0101781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Birch E.E., Wang J., Felius J., Stager D.R., Jr., Hertle R.W. Fixation control and eye alignment in children treated for dense congenital or developmental cataracts. J AAPOS. 2012;16:156–160. doi: 10.1016/j.jaapos.2011.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abdelmoaty S.M., Behbehani A.H. The outcome of congenital cataract surgery in Kuwait. Saudi J Ophthalmol. 2011;25:295–299. doi: 10.1016/j.sjopt.2011.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chak M., Wade A., Rahi Js. long term visual acuity and its predictors after surgery for congenital cataract. Invest Ophthalmol Vis Sci. 2006;47:4262–4269. doi: 10.1167/iovs.05-1160. [DOI] [PubMed] [Google Scholar]
- 8.Ye H.H., Deng D.M., Qian Y.Y., Lin Z., Chen W.R. Long-term visual outcome of dense bilateral congenital cataract. Chin Med J (Engl) 2007;120:1494–1497. [PubMed] [Google Scholar]
- 9.Ceyhan D., Schnall B.M., Breckenridge A., Fontanarosa J., Lehman S.S., Calhoun J.C. Risk factors for amblyopia in congenital anterior lens opacities. J AAPOS. 2005;9:537–541. doi: 10.1016/j.jaapos.2005.09.001. [DOI] [PubMed] [Google Scholar]
- 10.Skuta G.L., Cantor L.B., Cioffi G.A. 1st ed. American Academy of Ophthalmology; 2013–2014. Basic and Clinical Science Course (BCSC): Section 6: Pediatric Ophthalmology and Strabismus; pp. 233–234. [Google Scholar]
- 11.Leighton D.A., Tomlinson A. Changes in axial length and other dimensions of the eyeball with increasing age. Acta Ophthalmol (Copenh) 1972;50:815–826. doi: 10.1111/j.1755-3768.1972.tb06621.x. [DOI] [PubMed] [Google Scholar]
- 12.Rong X., Ji Y., Fang Y., Jiang Y., Lu Y. Long-term visual outcomes of secondary intraocular lens implantation in children with congenital cataracts. PLoS One. 2015;10:e0134864. doi: 10.1371/journal.pone.0134864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee Y.C., Kim H.S. Clinical symptoms and visual outcome in patients with presumed congenital cataract. J Pediatr Ophthalmol Strabismus. 2000;37:219–224. doi: 10.3928/0191-3913-20000701-09. [DOI] [PubMed] [Google Scholar]
- 14.Msamati B.C., Igbigbi P.S., Batumba N.H. Prevalence of lens opacity at Queen Elizabeth Central Hospital in Blantyre, Malawi. East Afr Med J. 2000;77:583–587. doi: 10.4314/eamj.v77i11.46725. [DOI] [PubMed] [Google Scholar]
- 15.Demirkilinc Biler E., Bozbiyik D.I., Uretmen O., Kose S. Strabismus in infants following congenital cataract surgery. Graefes Arch Clin Exp Ophthalmol. 2015;253(10):1801–1807. doi: 10.1007/s00417-015-2983-5. [DOI] [PubMed] [Google Scholar]
- 16.Jain S., Ashworth J., Biswas S., Lloyd I.C. Duration of form deprivation and visual outcome in infants with bilateral congenital cataracts. J AAPOS. 2010;14:31–34. doi: 10.1016/j.jaapos.2009.11.016. [DOI] [PubMed] [Google Scholar]
- 17.Magli A., Forte R., Rombetto L. Long-term outcome of primary versus secondary intraocular lens implantation after simultaneous removal of bilateral congenital cataract. Graefes Arch Clin Exp Ophthalmol. 2013;251:309–314. doi: 10.1007/s00417-012-1979-7. [DOI] [PubMed] [Google Scholar]
- 18.Eriksen J.R., Bronsard A., Mosha M., Carmichael D., Hall A., Courtright P. Predictors of poor follow-up in children that had cataract surgery. Ophthalmic Epidemiol. 2006;13:237–243. doi: 10.1080/09286580600672213. [DOI] [PubMed] [Google Scholar]
- 19.Astle W.F., Alewenah O., Ingram A.D., Paszuk A. Surgical outcomes of primary foldable intraocular lens implantation in children: understanding posterior opacification and the absence of glaucoma. J Cataract Refract Surg. 2009;35:1216–1222. doi: 10.1016/j.jcrs.2009.02.028. [DOI] [PubMed] [Google Scholar]