Abstract
Purpose
The study compared ocular biometry values using applanation and immersion techniques to determine the most applicable method for our tertiary training centre where personnel with different levels of experience and expertise in biometry take measurements used in calculation of required intraocular lens before cataract surgery.
Methods
The study was a prospective cross-sectional comparative study of different techniques of ocular biometry from diagnostic equipment (biometry probe 10 MHz Sonomed® A-scan (PACSCAN 300A, USA). Measurement variables were obtained among children and adults undergoing cataract surgery. Scleral (Prager) shell was used for the immersion technique followed by the contact technique by the same examiner.
Results
The biometry values of 92 eyes of 92 adult were taken. Their ages ranged from 18 to 95 years with a mean of 64.7 (SD ± 12.9) years. There were 55 (59.8%) males and 37 (40.2%) females, with a male to female ratio of 1.5:1.
Average axial length (22.0–24.4 mm) eyes were the most common eyes measured in 75 (81.5%) of the cases. The means of the axial lengths biometry values with immersion and contact technique were 23.66(±1.36) and 23.46 mm (±1.46); the axial length differences was 0.2 ± 0.26 mm (range 0.0–0.94 mm) and statistically significant (95% CI of the Difference 0.15 to 0.26, p = 0.000). The Standard deviation SD (mm) of Individual Eye Axial Length showed a mean of 0.03 ± 0.04 (0.0–0.3) mm for immersion and for contact technique 0.14 ± 0.12(0.0–0.6)mm.
Conclusion
There was a significant difference in ocular biometry measurement with the contact and immersion ultrasound techniques. The immersion technique had better repeatability, thus it is ideal in a training hospital setting in a typical in sub-Saharan Africa who have limited resources to employ a dedicated person to do biometry; and where the different operators of A-scan machines have different levels of experience and expertise.
Keywords: Ocular biometry, Applanation, Immersion, Techniques, Adults, Training
Introduction
Ocular biometric (axial length, anterior chamber depth and lens thickness) values are measured in everyday ophthalmological practice. This is mostly indicated in the pre-operative evaluation of cataract surgery.
Modern cataract surgery is considered a form of refractive surgery, aimed not only to restore visual clarity, but to provide excellent vision in refractive terms as well even when no intraocular lens (IOL) is implanted. When prescribed, an IOL is given to achieve a certain refractive status for the eye unlike what was obtainable in the past when refractive errors were corrected only after the surgery. This is made possible because of the development of modern, accurate diagnostic and surgical techniques.
The critical step in ocular biometry to attain the desired post-operative refractive outcome requires standardization of techniques to ensure accurate measurements important in providing correct calculation of required IOL power for cataract surgery.1, 2
A-scan ultrasound is the traditional technique for measuring anterior chamber depth, axial length and lens thickness. It involves passing an ultrasonic beam via a transducer through the eye, and as this is returned after hitting intraocular structures a trace of ocular spikes is displayed on the monitor from the cornea to the orbital fat.3
Biometry values can be obtained either by contact (applanation), immersion or optical methods. The contact/applanation technique is a widely used method which requires placing an ultrasound probe on the central cornea; this slightly indents the surface leading to various degrees of corneal compressions which may introduce errors into the values.4
The immersion A-scan biometry uses a saline filled scleral (Prager) shell between the probe and the eye; it is relatively observer independent. The optical method is a non-contact technique by partial coherence interferometry (PCI) that is highly reproducible, observer-independent and therefore potentially more accurate.5 The immersion and optical methods give comparative results.6 However, the main disadvantage of the optical method is its inability to obtain axial length measurements in approximately 8–17% of eyes, such as those with dense cataract, posterior sub-capsular cataracts, vision worse than 6/60, nystagmus, unstable lids etc., in which cases, another method of biometry is needed.7, 8, 9 Unfortunately, many cataracts in our population are already dense at the time of surgery making the optical method not widely applicable in our environment.
Whenever the optical method fails, if the immersion ultrasound was adopted as the second-line investigation, the outcomes could be improved from 82.5% within ±1 D of target10 to between 85.7 and 94.3%.8, 11, 12 In many parts of United Kingdom (UK), comparatively, other than the optical method (61% in UK), the contact method is often employed compared to immersion being used in only 1 out of 178 eye departments13 even though the accuracy of immersion ultrasound is generally better.14
The Royal College of Ophthalmologists Cataract Surgery Guidelines state 'what matters most in biometry is achieving excellent results' which can be presented in terms of the percentage of eyes within 0.5 or 1.0 Dioptre (D) of the target refraction found to be achievable in 85% of cases.10, 15
Axial length (AL) is the most important factor in IOL calculation. A 1-mm error in AL measurement results in a refractive error of approximately 2.35 D error of IOL power in an average eye of 23.5 mm and may translate to an error of 3.75D in a 20 mm eye and much more in the very short eye.16
Errors in predicted refraction after implantation of an intraocular lens (IOL) of calculated power is the sum of the random error in the measurement of the axial length(54%), the measurement of the corneal power (8%), and the estimation of the pseudophakic anterior chamber depth (ACD) (38%).17
The applanation or contact biometry was however the commonly performed method in our centre in the past, being a training centre, different personnel are involved in operation of the A-scan ultrasound machine. There had been the need to frequently repeat biometric measurements, and the need for another operator to repeat measurements because of inconsistencies in the axial length values obtained and refractive surprises from incorrect intra-ocular lens power.
There was therefore a need to compare the contact applanation method with the immersion technique using the available (Sonomed®) ultrasound machine in our hospital. It has both contact/applanation and immersion capabilities. It can be used in conditions like mature cataracts, posterior sub-capsular cataracts, vitreous haemorrhage, maculopathy, or retinal detachment where optical biometry cannot be performed accurately.18
Methods
The study was a prospective cross-sectional comparative study of measurement variables obtained by different techniques from diagnostic equipment. Approval for the study was obtained from the Ethics and Research Committee (ERC/IRB) of Federal Government owned University of Ilorin Teaching Hospital where the research was carried out. Consecutive patients attending the out-patient clinic were included in the study over a 6month period in 2013. Patients with presence of any corneal pathology, ocular developmental anomaly, ocular tumours and non-consenting individuals were excluded from the study.
In one eye of the subjects, measurements of anterior chamber depth (ACD), lens thickness, axial length (AL) and its standard deviation were determined with A-scan (Sonomed®, PACSCAN 300A, USA) machine. It has a 10 MHz A-scan biometry probe for both contact and immersion techniques.
Measurements were taken using immersion A-scan biometry first followed by the contact A-scan biometry by the same examiner. For immersion A-scan; a scleral (Prager) immersion shell was used. The chamber was filled with normal saline connected by the silicone tube to a 5 ml syringe. Automated sequences of five reliable readings were taken according to the pre-set amplitude and timing criteria for the ultrasound reflections with one application of the shell and probe; for contact A-scan, the probe was placed gently over the cornea and an automated sequence of five reliable readings with characteristic peaks was taken according to the pre-set amplitude and timing criteria for ultrasound reflections. The spikes and corresponding gates produced in all instances were carefully evaluated and unreliable readings discarded before the mean value was recorded. For each eye, five axial length readings were taken by the machine to give an average reading with a standard deviation displayed.
The data was analysed with SPSS-17 (Inc. SPSS Chicago, IL) statistical package for social sciences. Student t-test was used to compare the means of the measurement values from the two techniques. A two-tailed p value of less than 0.05 was considered significant (0.95 level of confidence).
Results
The biometry values of 92 eyes of 92 adults were taken. Their ages ranged from 18 to 95 years with a mean of 64.7 (SD ± 12.9) years. There were 55 (59.8%) males and 37 (40.2%) females, with a male to female ratio of 1.5:1.
Average axial length (22.0–24.4 mm) eyes were the most common eyes measured in 75 (81.5%) of the cases. The means of the biometry values with immersion and contact technique were axial lengths 23.66(±1.36) and 23.46 mm (±1.46), anterior chamber depths 3.19 and 3.29 mm, and lens thickness 3.87 and 3.51 mm respectively (Table 1).
Table 1.
Descriptive table of the biometry readings with immersion & contact biometry techniques.
| Minimum | Maximum | Mean | Std. deviation | |
|---|---|---|---|---|
| Axial length by immersion | 21.82 | 32.43 | 23.66 | 1.46 |
| Axial length by contact | 21.03 | 31.89 | 23.46 | 1.46 |
| Anterior chamber depth immersion | 1.97 | 5.57 | 3.19 | 0.63 |
| Anterior chamber depth contact | 2.41 | 5.20 | 3.29 | 0.51 |
| Lens thickness immersion | 0.00 | 5.69 | 3.87 | 0.99 |
| Lens thickness contact | 0.00 | 5.72 | 3.51 | 0.90 |
| Differences in axial length between immersion and contact A-scan | −0.47 | 0.94 | 0.21 | 0.26 |
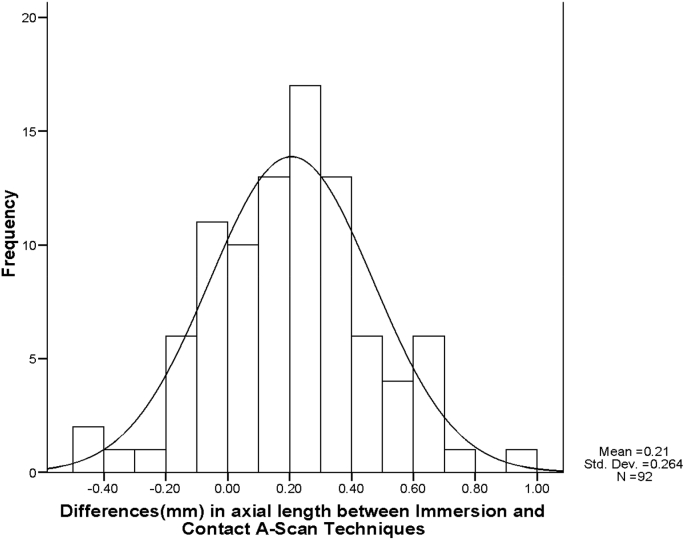
There was a statistically significant high linear correlation (correlation 0.984, R-Square 0.968, p = 0.000) in the axial length measurement by the two techniques, however, the correlation for lens thickness was fair, marginal for anterior chamber depth. The mean of the axial length differences was statistically significant (95% CI of the Difference 0.15–0.26, p = 0.000); it was 0.2 ± 0.26 mm (range 0.0–0.94 mm), this difference was within 0.2 mm in 49(53.3%) of the eyes and greater than 0.2 mm in 43(46.7%) of the eyes, the distribution of the difference in axial length between the immersion and contact is shown in Fig. 1.
Fig. 1.
Differences in axial length between immersion and contact A-scan techniques.
Five axial length readings were taken in each eye by the machine to give an average reading with a standard deviation (SD). A high significance p value of 0.20 (greater than 0.05) by Kolmogorov-Smirnov, test of Normality indicates a normal distribution of the data Table 2.
Table 2.
Correlation and differences in measurements obtained by immersion and contact techniques of ocular biometry.
| Biometry parameters | Paired samples correlations |
Paired sample differences (T-Test) |
|||||
|---|---|---|---|---|---|---|---|
| Correlation | R-Square | Mean | SD | 95% CI of the difference |
p-Value | ||
| Lower | Upper | ||||||
| Axial length immersion-axial length contact | 0.984 | 0.968 | 0.21 | 0.26 | 0.15 | 0.26 | 0.000 |
| Anterior chamber depth immersion – Anterior chamber depth Contact | 0.552 | 0.305 | −0.11 | 0.55 | −0.22 | −0.01 | 0.071 |
| Lens thickness immersion – Lens thickness contact | 0.610 | 0.373 | 0.36 | 0.83 | 0.19 | 0.53 | 0.000 |
SD – Standard deviation, CI – Confidence interval.
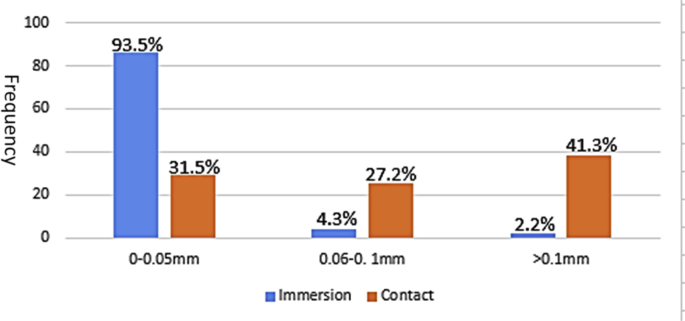
The Standard deviation SD (mm) of Individual Eye Axial Length Showed a mean of 0.03 ± 0.04 (0.0–0.3) mm for immersion and for contact technique 0.14 ± 0.12(0.0–0.6)mm. There was a statistically significant difference of the SD of the individual readings of immersion and contact technique of biometry, the SD of the two techniques were poorly correlated (correlation, 0.038, R-square 0.01, 95% Confidence Interval of −0.08 to −8.02, and p = 0.000). Whereas the SD was 0–0.05 mm in 86 (93.5%) eyes measured by immersion, it was so in only 29 (31.5%) of eyes by contact technique which also recorded a difference greater than 0.1 mm in 38 (41.3%) compared to 2 (2.2%) by immersion technique. The relatively wide dispersion of the Standard Deviation of axial length values using the contact technique is displayed in (Fig. 2).
Fig. 2.
Range of standard deviation (mm) between five axial length readings taken for each eye by immersion and contact A-scan ultrasound techniques.
Discussion
Ocular biometry is basic to cataract surgery, the commonest surgery carried out in Ophthalmology. Precise measurement of ocular biometry values, especially axial length measurement is central to the accurate calculation of intra-ocular lens (IOL) power inserted at surgery. It is not unusual for different categories of staff to be involved in this important measurement.13 This necessitates the use of the least operator dependent technique which is the optical method by partial coherence laser interferometry whose reading is set to conform to that of immersion technique.16 Unfortunately, its limitations in not being widely available nor applicable to our population on account of its higher cost relative to the ultrasound technique; and the limit of its applicability in view of the usually dense cataract that we mostly deal with, makes the ultrasonography method appropriate in our setting.
In this study, the immersion technique gave longer axial length measurement compared to the contact method. In the immersion technique, measurements are performed through a water bath. This prevents direct contact of the A-scan probe with the cornea thus avoiding corneal compression. The shell also stabilizes the globe, keeps the eyelids open, and allows proper alignment of the probe to the visual axis. The shorter biometric values found with the contact method can be explained by corneal compression resulting in decreased anterior chamber depth and off-axis measurements.19
Statistically significant differences (p = 0.000) were found in the mean values obtained using both techniques in measurement (the mean difference in measured axial length with immersion and contact was 0.21 mm).
The difference of the mean axial length showed longer readings by immersion technique by an average of 0.21 ± 0.26 mm (0–0.94 mm). This may have implications for the choice of IOL power18 as the most common indication for ocular biometry is to calculate IOL power that will result in the target post-operative refraction. The clinical significance of the difference for the average length eye may therefore be a refractive error of about 0–3 Dioptres.
This is similar to other reports of 0.24 mm by Shammas20 and 0.26 mm (SD 0.3) by Kronbauer et al.21 Similar significant differences in the two techniques in measuring ocular biometry especially, axial length measurement was reported by other authors22, 23, 24 who showed that with the contact method, a difference up to 0.47 mm occurred among various examiners, resulting in an unsystematic difference between both techniques of about 18% greater intra-ocular lens calculation errors with the contact technique.
The greater accuracy was attributed to the greater sensitivity of the immersion technique to probe displacement and absence of corneal compression.25 This difference is said to be due to pressure exerted on the eye by the ultrasound probe which results in corneal indentation and shortening of axial length unlike in the immersion technique where, the ultrasound probe is inserted into a shell in which a coupling fluid is introduced to prevent direct contact with the cornea thus preventing compression.26
Henessy et al27 however reported on 36 eyes, and found longer axial length measurement of 0.03 mm by contact method, and also suggested that repeating measurement made contact ultrasound biometry comparable to that of immersion with no clinically significant difference in mean axial length measurements.
A better repeatability with the immersion technique was demonstrated in this study. The differences (the standard deviation) between the five readings taken for each eye demonstrates the dispersion of the readings by the different techniques; The standard deviation of five repeated axial length measurements was found to be between 0 and 0.05 mm in 86 (93.5%) and greater than 0.1 mm in 2 (2.2%) eyes measured by immersion, compared to 29(31.5%) and 38 (41.3%) of eyes by contact technique respectively-(Fig. 2).
The dispersion using contact methods translates to less repeatability of the technique and the need to delete more measurement values, do more repeat examination and the need to have more people to cross check the measurements making it a longer technique and least reassuring to the operator of the machine and the cataract surgeon especially so in a training centre where different operators exist.
The influence of experience of operators especially on the contact technique was emphasised by Kittahaweesin28 who found that the reproducibility of both techniques was similar when performed by an experienced measurer, whereas, the less experienced measurer had greater reproducibility with the immersion technique and suggested that the immersion technique should be considered, particularly for less-experienced operators.28
The better repeatability with the immersion technique maybe due to the fact that the immersion technique is less dependent on patients' cooperation compared to the contact method. The globe is stabilized with the sclera shell preventing globe motility. Some other comparative studies of ultrasound biometry techniques indicate that the contact technique is equivalent to the immersion technique but only when the operator is experienced.27, 28
The good repeatability of the immersion technique is of advantage in a training institution like ours where there are different personnel with varying levels of expertise performing biometry on patients. It eliminates the problem of having to depend on one particular biometry technician as all measurements will be within hundredths of a millimetre of each other.
In conclusion, there was a significant difference in ocular biometry measurement with the contact and immersion ultrasound techniques. The immersion technique had better repeatability, thus it is ideal in a training (teaching) hospital setting in a typical developing country in sub-Saharan Africa who have limited resources to employ a dedicated person to do biometry; and where the different operators of A-scan machines have different levels of experience and expertise. Further study to correlate the visual outcome with the biometry measurement is suggested.
Conflict of interest
The authors do not have any conflict of interest to declare.
Footnotes
Peer review under responsibility of the Iranian Society of Ophthalmology.
References
- 1.Norrby S. Sources of error in intraocular lens power calculation. J Cataract Refract Surg. 2008;34:368–376. doi: 10.1016/j.jcrs.2007.10.031. [DOI] [PubMed] [Google Scholar]
- 2.Hrebcova J., Skorkovska S., Vasku A. Comparison of contact and immersion techniques of ultrasound biometry in terms of target postoperative refraction. Cesk Slov Oftalmol. 2009;65:143–146. [PubMed] [Google Scholar]
- 3.R J., F M. The contact and immersion ultrasound methods compared using the ray tracing method. Optica Applicata. 2010;XL:77–92. [Google Scholar]
- 4.Hoffmann P.C., Hutz W.W., Eckhardt H.B., Heuring A.H. Intraocular lens calculation and ultrasound biometry: immersion and contact procedures. Klin MonblAugenheilkd. 1998;213:161–165. doi: 10.1055/s-2008-1034967. [DOI] [PubMed] [Google Scholar]
- 5.Olsen T. Calculation of intraocular lens power: a review. Acta Ophthalmol Scand. 2007;85:472–485. doi: 10.1111/j.1600-0420.2007.00879.x. [DOI] [PubMed] [Google Scholar]
- 6.Packer M., Fine I.H., Hoffman R.S., Coffman P.G., Brown L.K. Immersion A-scan compared with partial coherence interferometry: outcomes analysis. J Cataract Refract Surg. 2002;28:239–242. doi: 10.1016/s0886-3350(01)01259-7. [DOI] [PubMed] [Google Scholar]
- 7.Hill W., Angeles R., Otani T. Evaluation of a new IOLMaster algorithm to measure axial length. J Cataract Refract Surg. 2008;34:920–924. doi: 10.1016/j.jcrs.2008.02.021. [DOI] [PubMed] [Google Scholar]
- 8.Haigis W., Lege B., Miller N., Schneider B. Comparison of immersion ultrasound biometry and partial coherence interferometry for intraocular lens calculationaccording to Haigis. Graefes Arch Clin Exp Ophthalmol. 2000;238:765–773. doi: 10.1007/s004170000188. [DOI] [PubMed] [Google Scholar]
- 9.Rajan M.S., Keilhorn I., Bell J.A. Partial coherence laser interferometry vs conventional ultrasound biometry in intraocular lens power calculations. Eye(Lond) 2002;16:552–556. doi: 10.1038/sj.eye.6700157. [DOI] [PubMed] [Google Scholar]
- 10.Gale R.P., Saldana M., Johnston R.L., Zuberbuhler B., McKibbin M. Benchmark standards for refractive outcomes after NHS cataract surgery. Eye (Lond) 2009;23:149–152. doi: 10.1038/sj.eye.6702954. [DOI] [PubMed] [Google Scholar]
- 11.Fontes BM, Castro E. Intraocular lens power calculation by measuring axial length with partial optical coherence and ultrasonic biometry. Arq BrasOftalmol; 74:166–170. [DOI] [PubMed]
- 12.Mylonas G, Sacu S, Buehl W, Ritter M, Georgopoulos M, Schmidt-Erfurth U. Performance of three biometry devices in patients with different grades of age-related cataract. Acta Ophthalmol; 89:e237–41. [DOI] [PubMed]
- 13.Gale R.P., Saha N., Johnston R.L. National biometry audit II. Eye (Lond) 2006;20:25–28. doi: 10.1038/sj.eye.6701778. [DOI] [PubMed] [Google Scholar]
- 14.Lee A.C., Qazi M.A., Pepose J.S. Biometry and intraocular lens power calculation. Curr Opin Ophthalmol. 2008;19:13–17. doi: 10.1097/ICU.0b013e3282f1c5ad. [DOI] [PubMed] [Google Scholar]
- 15.Aristodemou P., Knox Cartwright N.E., Sparrow J.M., Johnston R.L. Intraocular lens formula constant optimization and partial coherence interferometry biometry: refractive outcomes in 8108 eyes after cataract surgery. J Cataract RefractSurg. 2011;37:50–62. doi: 10.1016/j.jcrs.2010.07.037. [DOI] [PubMed] [Google Scholar]
- 16.Basic and Clinical Science Course, Section 3: American Academy of Ophthalmology 2011-2012; 211–223.
- 17.Olsen T. Sources of error in intraocular lens power calculation. J Cataract Refract Surg. 1992;18:125–129. doi: 10.1016/s0886-3350(13)80917-0. [DOI] [PubMed] [Google Scholar]
- 18.Watson A., Armstrong R. Contact or immersion technique for axial length measurement? Aust N Z J Ophthalmol. 1999;27:49–51. doi: 10.1046/j.1440-1606.1999.00162.x. [DOI] [PubMed] [Google Scholar]
- 19.Abu El Einen K.G., Shalaby M.H., El Shiwy H.T. Immersion B-guided versus contact A-mode biometry for accurate measurement of axial length and intraocular lenspower calculation in siliconized eyes. Retina. 2011;31:262–265. doi: 10.1097/IAE.0b013e3181e17f39. [DOI] [PubMed] [Google Scholar]
- 20.Shammas H.J. A comparison of immersion and contact techniques for axial length measurement. J Am Intraocul Implant Soc. 1984;10:444–447. doi: 10.1016/s0146-2776(84)80044-0. [DOI] [PubMed] [Google Scholar]
- 21.Kronbauer A.L., Kronbauer F.L., Kronbauer C.L. Comparative study of the biometric measurements made by immersion and contact techniques. Arq Bras Oftalmol. 2006;69:875–880. doi: 10.1590/s0004-27492006000600017. [DOI] [PubMed] [Google Scholar]
- 22.Ben-Zion I., Neely D.E., Plager D.A., Ofner S., Sprunger D.T., Roberts G.J. Accuracy of IOL calculations in children: a comparison of immersion versus contact A-scanbiometry. J AAPOS. 2008;12:440–444. doi: 10.1016/j.jaapos.2008.03.016. [DOI] [PubMed] [Google Scholar]
- 23.Hitzenberger C.K., Drexler W., Dolezal C. Measurement of the axial length of cataract eyes by laser Doppler interferometry. Invest Ophthalmol Vis Sci. 1993;34:1886–1893. [PubMed] [Google Scholar]
- 24.Olsen T., Nielsen P.J. Immersion versus contact technique in the measurement of axial length by ultrasound. Acta Ophthalmol (Copenh) 1989;67:101–102. doi: 10.1111/j.1755-3768.1989.tb00732.x. [DOI] [PubMed] [Google Scholar]
- 25.Falhar Martin R.J. The contact and immersin ultrasound methods compared using the ray tracing method. Optica Applicata. 2010;XL:77–92. [Google Scholar]
- 26.Attah H. Ophthalmic ultrasound, a practical guide. 2008. pp. 555–560. [Google Scholar]
- 27.Hennessy M.P., Franzco, Chan D.G. Contact versus immersion biometry of axial length before cataract surgery. J Cataract Refract Surg. 2003;29:2195–2198. doi: 10.1016/s0886-3350(03)00224-4. [DOI] [PubMed] [Google Scholar]
- 28.Kitthaweesin K., Mungsing W. Agreement and reproducibility of contact and immersion techniques for axial length measurement and intraocular lens power calculation. J Med Assoc Thai. 2009;92:1046–1049. [PubMed] [Google Scholar]