Abstract
Purpose
To determine pachymetric, aberrometric, and topometric indices in patients with definite and subclinical keratoconus and the validity of these indices in the diagnosis of keratoconus.
Methods
We evaluated 262 keratoconic and 97 healthy eyes in this study. Pentacam HR examination was performed for all participants, and the data of all pachymetric, aberrometric, and topometric indices was extracted for the study population.
Results
The average of all evaluated pachymetric and topometric indices and the 3rd and 5th order vertical coma aberrations showed a significant difference between the study groups (p < 0.001). Belin/Ambrosio Deviation Display (BAD_D), Index of Vertical Asymmetry (IVA), Index of Surface Variance (ISV), and 5th order vertical coma aberration were identified as the best diagnostic criteria for the diagnosis of subclinical keratoconus (R2 = 0.65, p <0.001), and BAD_D, mean keratometry and 3rd order vertical coma aberration were identified as the best diagnostic criteria for the diagnosis of definite keratoconus (R2 = 0.91, p <0.001). The sensitivity and specificity of the above-mentioned models were 83.6% and 96.9%, and 97.9% and 96.9%, respectively.
Conclusion
Simultaneous evaluation of BAD_D, 5th order vertical coma aberration, IVA, and ISV, especially when the pattern of the corneal curvature is normal, can detect subclinical keratoconus with high sensitivity and specificity. As for definite keratoconus, each of the BAD_D, mean keratometry, and 3rd order vertical coma aberration indices has a desirable diagnostic validity. However, the aforementioned indices do not negate the importance of widely recognized and acceptable indices like keratometry and central corneal thickness.
Introduction
Keratoconus often starts to develop at the age of puberty as a corneal ectatic disorder.1 It is a progressive condition with a heavy burden for patients as a result of aggravation in the third decade of life.2 Corneal cross-linking has made it possible to arrest keratoconus, especially in the early stages.3 Therefore, early diagnosis is of vital importance.
A diagnosis of keratoconus is most commonly made through slit lamp examination, corneal topography, and measurement of visual acuity and refraction. Since slit lamp examination is unable to show the signs of keratoconus in the early stages and visual acuity may not be affected, corneal topography is the only reliable criterion.4, 5 Recent advances in corneal imaging and the possibility of the assessment of the corneal surface with the help of anterior/posterior elevation measurements have provided ophthalmologists with valuable information.6, 7 Pentacam employs the Scheimpflug imaging technique to present the corneal topographic indices with an acceptable accuracy and repeatability.8 There is desirable variety in the output data of this device which can benefit ophthalmologists in various ways. Keratoconus diagnostic indices and some pachymetric indices are among the indices measured by Pentacam which were evaluated in this study in order to facilitate the diagnosis of this condition. In addition to the changes of these indices in patients with definite keratoconus, we investigated their use in detecting the cases of subclinical keratoconus and presented some cut-off points, which are clinically important.
Methods
In this cross-sectional study, we evaluated keratoconus patients who were visited in the keratoconus clinic of Noor Eye Hospital in the second half of 2012 and received Pentacam HR examination. Keratoconus diagnosis had been confirmed by thorough clinical examination and corneal topography. The control group was selected from among the candidates of refractive surgery who did not have a history of ocular surgery and their corneal topography (with Pentacam) was normal. Due to the high number of the people in the control group, one month in the six-month period of the study was randomly selected, and all eligible individuals in that month were included in the control group. The data of the right eye of the participants (case/control) whose family name started with a letter in the first half of the alphabet and the left eye of the rest of participants was used for analysis.
The data of the pachymetric, topometric, and aberrometric indices, which are shown in Table 1, was extracted from the Pentacam software. Based on the criteria developed by McMahon et al9 the severity of keratoconus was categorized from subclinical to severe. The average of the evaluated indices in the control, subclinical, and definite groups was compared using ANCOVA, and the effects of age and sex were controlled. A stepwise logistic regression model was used to control the effect of age and sex and to determine the effective indices in detecting the cases of subclinical and definite keratoconus. The diagnostic specificity and sensitivity of these indices, in comparison with clinical examination and McMahon criteria, were evaluated and compared with Receiver Operating Curve (ROC), and cut-off points were presented.
Table 1.
Description of Pentacam indices.
| TP | Minimum corneal thickness | CKI | Central keratoconus index |
| AP | Corneal thickness at apex | Rmin | Minimum sagittal curvature |
| RPIavg | Average pachymetric progression index | ACD | Anterior chamber depth |
| RPImax | Maximum pachymetric progression index | ACv | Anterior chamber volume |
| RPImin | Minimum pachymetric progression index | CV | Corneal volume |
| ARTmax | Maximum Ambrosio relational thickness | AE | Maximum anterior elevation in 5 mm zone above the best fit sphere |
| ARTavg | Average Ambrosio relational thickness | PE | Maximum posterior elevation in 5 mm zone above the best fit sphere |
| BAD_D | Belin/Ambrosio enhanced ectasia total deviation value | AEdif | Difference of maximum–minimum anterior elevation above/below the best fit sphere |
| MEAN keratometry | PEdif | Difference of maximum–minimum posterior elevation above/below the best fit sphere | |
| Maximum keratometry front | CKI | Central keratoconus index | |
| IVA | Index of vertical asymmetry | Rmin | Minimum sagittal curvature |
| ISV | Index of surface variance | ACD | Anterior Chamber Depth |
| IHD | Index of height decentration | KI | keratoconus index |
| IHA | Index of height asymmetry | Corneal and total values of higher order aberrations and all Zernike indices | |
Results
We selected 226 keratoconus patients from the list of the patients visited in the keratoconus clinic and 100 healthy controls who were candidates of refractive surgery with no previous history of ocular surgery and no abnormal topographic pattern. The mean age of the participants was 32.02 ± 10.15 and 29.64 ± 7.45 years for cases and controls, respectively. The male to female ratio was 54/46 in the case group and 38/62 in the control group. Of keratoconus patients, 14.1% (63 eyes) were categorized as suspicious, 51.7% (231 eyes) as mild, 14.5% (65 eyes) as moderate, and 19.7% (88 eyes) as severe keratoconus. The data of both eyes was evaluated in 27 individuals, one eye with the diagnosis of keratoconus and the other eye as suspicious for keratoconus. The mean and SD topographic indices in the study groups, after adjusting for the effect of age and sex, are presented in Table 2. The variables that are presented in Table 2 showed significant differences between normal and keratoconic cases in univariate logistic regression models.
Table 2.
Pentacam indices among normal, subclinical keratoconus, and definite keratoconus corneas.
| Controls | Subclinical keratoconus | Definite keratoconus |
Subclinical vs. controls |
Definite vs. controls |
|||
|---|---|---|---|---|---|---|---|
| Mild | Moderate | Severe | p value | p value | |||
| Mean K | 43.8 ± 1.4 | 43.1 ± 1.2 | 46.1 ± 2.0 | 50.6 ± 2.3 | 53.4 ± 5.9 | 0.443 | <0.001 |
| AEmax | 8.70 ± 4.6 | 12.39 ± 8.0 | 26.95 ± 12.8 | 41.93 ± 15.5 | 54.42 ± 22.2 | 0.346 | <0.001 |
| PEmax | 14.60 ± 6.0 | 24.02 ± 12.8 | 48.72 ± 19.5 | 72.87 ± 23.7 | 93.94 ± 29.1 | 0.012 | <0.001 |
| Topometric indices | |||||||
| ISV | 19 ± 7 | 28 ± 13 | 62 ± 24 | 96 ± 23 | 133 ± 34 | 0.002 | <0.001 |
| IVA | 0.10 ± 0.0 | 0.28 ± 0.2 | 0.69 ± 0.3 | 0.97 ± 0.4 | 1.25 ± 0.5 | <0.001 | <0.001 |
| KI | 1.02 ± 0.02 | 1.05 ± 0.05 | 1.15 ± 0.10 | 1.25 ± 0.10 | 1.36 ± 0.17 | <0.001 | <0.001 |
| CKI | 1.00 ± 0.00 | 1.00 ± 0.01 | 1.03 ± 0.03 | 1.07 ± 0.04 | 1.12 ± 0.06 | <0.001 | <0.001 |
| IHA | 3.39 ± 2.80 | 7.04 ± 6.08 | 20.90 ± 15.08 | 25.24 ± 15.96 | 35.10 ± 24.54 | 0.131 | <0.001 |
| IHD | 0.006 ± 0.003 | 0.017 ± 0.012 | 0.051 ± 0.027 | 0.080 ± 0.034 | 0.122 ± 0.049 | <0.001 | <0.001 |
| Rmin | 7.49 ± 0.25 | 7.47 ± 0.20 | 6.59 ± 0.32 | 5.83 ± 0.12 | 5.13 ± 0.44 | 0.331 | <0.001 |
| Pachymetric indices | |||||||
| TP | 537 ± 31 | 499 ± 32 | 473 ± 38 | 439 ± 40 | 415 ± 58 | <0.001 | <0.001 |
| RPIavg | 0.99 ± 0.14 | 1.23 ± 0.34 | 1.80 ± 0.52 | 2.50 ± 0.55 | 3.39 ± 1.24 | <0.001 | <0.001 |
| RPImax | 1.23 ± 0.20 | 1.71 ± 0.48 | 2.55 ± 0.86 | 3.35 ± 0.80 | 4.67 ± 2.00 | <0.001 | <0.001 |
| ARTavg | 555 ± 94 | 435 ± 124 | 282 ± 93 | 185 ± 51 | 140 ± 69 | <0.001 | <0.001 |
| ARTmax | 449 ± 82 | 319 ± 107 | 202 ± 67 | 139 ± 37 | 103 ± 46 | <0.001 | <0.001 |
| BAD_D | 0.96 ± 0.8 | 3.34 ± 2.9 | 6.94 ± 2.9 | 10.77 ± 3.2 | 15.52 ± 6.4 | <0.001 | <0.001 |
| Aberrometric indices | |||||||
| RMS total | 1.70 ± 0.84 | 2.46 ± 1.40 | 6.64 ± 2.95 | 10.10 ± 3.61 | 15.65 ± 5.85 | <0.001 | <0.001 |
| RMS HOA | 0.34 ± 0.08 | 0.66 ± 0.39 | 1.70 ± 0.84 | 2.59 ± 0.97 | 4.01 ± 1.74 | <0.001 | <0.001 |
| 3rd Ver. coma total | −0.05 ± 0.17 | −0.42 ± 0.41 | −1.32 ± 0.90 | −1.98 ± 1.20 | −2.76 ± 2.03 | <0.001 | <0.001 |
| 3rd Ver. coma front | −0.13 ± 0.51 | −1.53 ± 1.41 | −4.68 ± 3.02 | −7.00 ± 4.05 | −9.84 ± 6.5 | <0.001 | <0.001 |
| 3rd Ver. coma back | 0.186 ± 1.07 | −3.50 ± 3.28 | −10.02 ± 6.21 | −14.49 ± 7.93 | −19.91 ± 10.75 | <0.001 | <0.001 |
| 3rd Hor. coma total | 0.000 ± 0.123 | 0.012 ± 0.262 | −0.034 ± 0.631 | 0.022 ± 1.011 | 0.041 ± 1.660 | 0.605 | 0.929 |
| 3rd Hor. coma front | −0.016 ± 0.385 | 0.000 ± 0.889 | −0.124 ± 2.18 | 0.069 ± 3.65 | 0.293 ± 5.64 | 0.837 | 0.934 |
| 3rd Hor. coma back | −0.144 ± 0.580 | −0.332 ± 0.494 | −0.310 ± 5.09 | 0.137 ± 8.57 | 1.517 ± 11.75 | 0.236 | 0.552 |
| 5th Ver. coma total | 0.001 ± 0.027 | 0.032 ± 0.064 | 0.149 ± 0.170 | 0.149 ± 0.293 | 0.219 ± 0.525 | <0.001 | <0.001 |
| 5th Ver. coma front | 0.004 ± 0.068 | 0.152 ± 0.206 | 0.535 ± 0.545 | 0.511 ± 0.958 | 0.718 ± 1.587 | <0.001 | <0.001 |
| 5th Ver. coma back | −0.01 ± 0.34 | 0.68 ± 0.62 | 1.49 ± 1.43 | 1.45 ± 2.20 | 2.05 ± 2.50 | <0.001 | <0.001 |
| 5th Hor. coma total | 0.001 ± 0.024 | 0.002 ± 0.045 | 0.002 ± 0.112 | 0.004 ± 0.203 | −0.020 ± 0.320 | 0.723 | 0.815 |
| 5th Hor. coma front | 0.001 ± 0.053 | 0.009 ± 0.132 | 0.003 ± 0.348 | 0.008 ± 0.682 | −0.083 ± 0.942 | 0.453 | 0.690 |
| 5th Hor. coma back | −0.001 ± 0.36 | 0.035 ± 0.49 | −0.020 ± 1.18 | −0.041 ± 1.80 | −0.355 ± 2.13 | 0.461 | 0.415 |
Mean comparisons were performed while age and sex were controlled in ANCOVA analysis.
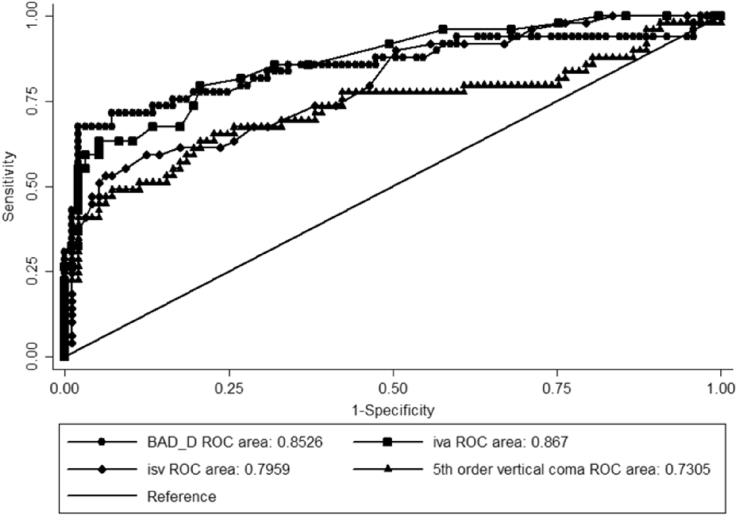
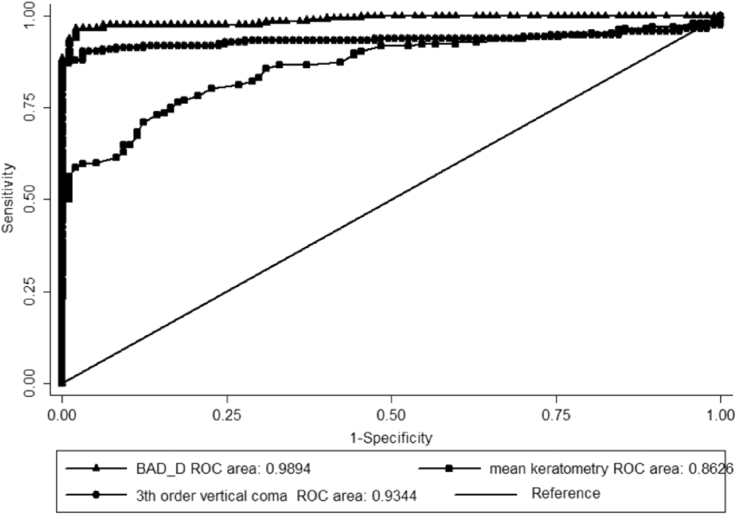
According to the regression model, Belin/Ambrosio Deviation Display (BAD_D), Index of Vertical Asymmetry (IVA), Index of Surface Variance (ISV), and 5th order coma aberration at the front surface of the cornea were the best variables for the diagnosis of subclinical keratoconus, which finally remained in the model (Table 3). Moreover, BAD_D, 3rd order vertical coma aberration, and mean keratometry were appropriate criteria for the diagnosis of definite keratoconus (Table 4). The proposed cut-off points for these indices along with their sensitivity and specificity are presented in Table 5. The area under the ROC for the evaluated variables in the regression models are shown in Fig. 1, Fig. 2.
Table 3.
Logistic regression model of determinant factors for diagnosis of subclinical keratoconus cases.
| Coefficient (SE) | p value | 95% Confidence interval | ||
|---|---|---|---|---|
| BAD_D | 1.35 (0.49) | 0.006 | 0.38 | 2.31 |
| IVA | 33.24 (8.44) | <0.001 | 16.70 | 49.78 |
| ISV | −0.26 (0.08) | 0.002 | −0.42 | −0.09 |
| 5th Order vertical coma aberration of cornea front | 14.35 (4.14) | 0.001 | 6.21 | 22.47 |
Pseudo R2 = 0.65.
Table 4.
Logistic regression model of determinant factors for diagnosis of definite keratoconus cases.
| Coefficient (SE) | p value | 95% Confidence interval | ||
|---|---|---|---|---|
| BAD_D | 2.25 (0.51) | <0.001 | 1.24 | 3.26 |
| Mean keratometry | 0.72 (0.30) | 0.018 | 0.12 | 1.31 |
| 3rd Order vertical coma aberration of cornea front | −2.51 (0.70) | <0.001 | −3.88 | −1.14 |
Pseudo R2 = 0.91.
Table 5.
Cut-off points of Pentacam indices for detection of subclinical and definite keratoconus cases.
| Cut-off | Sensitivity (%) | Specificity (%) | AUC | |
|---|---|---|---|---|
| Definite keratoconus vs. controls | ||||
| BAD_D | ≥2.38 | 96.7 | 94.8 | 0.99 |
| Mean keratometry | ≥44.9 | 80.2 | 77.3 | 0.86 |
| 3rd Order vertical coma aberration of cornea front | ≤−0.798 | 91.3 | 90.72 | 0.93 |
| Total | 97.9 | 96.9 | 0.99 | |
| Suspect keratoconus vs. controls | ||||
| BAD_D | ≥1.54 | 81.1 | 73.2 | 0.86 |
| IVA | ≥0.14 | 82.3 | 73.2 | 0.86 |
| ISV | ≥22 | 74.5 | 61.8 | 0.80 |
| 5th Order vertical coma aberration of cornea front | ≥0.023 | 70.6 | 61.8 | 0.72 |
| Total | 83.6 | 96.9 | 0.96 | |
Fig. 1.
Combined receiver operating curves of Pentacam indices for detecting subclinical keratoconus.
Fig. 2.
Combined receiver operating curves of Pentacam indices for detecting definite keratoconus.
Discussion
Detecting the cases of subclinical keratoconus has always been a challenge for ophthalmologists, especially when the suggestive clinical signs and symptoms to differentiate subclinical keratoconus from the normal corneal are not observed. In these conditions, although topographic indices and the pattern of the corneal curvature can benefit ophthalmologists, their overlap in subclinical and normal cases in indices with low sensitivity and specificity is a problem. In this study, with more focus on subclinical cases, we introduced Pentacam indices which were applicable and had acceptable specificity and sensitivity. A combination of pachymetric, topometric, and aberrometric indices was entered to the regression model to differentiate subclinical and normal cases. If the value(s) of one/some of these indices in one patient is close to the values in subclinical keratoconus patients (available in Table 3), it can help the ophthalmologist with clinical judgment. However, we suggest that attention be paid to all the indices to reduce false negative/positive results. Regarding the cases of definite keratoconus, each of the proposed indices has a high sensitivity and specificity in and of themselves.
Our findings showed that BAD_D was very important in the diagnosis of subclinical and definite keratoconus which is congruent with other studies.10, 11
Ambrosio et al12 emphasized the importance of the relative corneal thickness indices instead of relying on point measurements. They introduced new indices named Maximum Ambrosio Relational Thickness “ARTmax” and Average Ambrosio Relational Thickness “ARTavg” based on the data of Maximum Pachymetric Progression Index “RPImax” and Average Pachymetric Progression Index “RPIavg” and the thinnest point of the cornea which were more accurate in detecting the cases of keratoconus when compared to point measurements. Our findings, in addition to confirming the difference in the values of these indices between the study groups (Table 2), showed that BAD_D with a cut-off point of 1.54 was more effective than ARTmax and ARTavg in detecting the cases of subclinical keratoconus. In line with this finding, a cut-off point of 1.45 was proposed by Ambrosio et al11 which is very close to ours.
The results of different studies suggest that with removing the data of central 3.5 mm height and using enhanced best fit sphere instead of the standard mode in calculating BAD_D, an even more sensitive and specific index is available for detecting the cases of subclinical keratoconus. It shows the reason why this index is more appropriate than anterior/posterior elevation data. The weak point of the elevation data is the way the reference surface is determined to detect the height of the different corneal points while this problem has been well-addressed in enhanced best fit sphere. Ucakhan et al13 considered the corneal surface height as well as the corneal thickness and curvature when analyzing Pentacam data. In particular, while comparing keratoconic patients with normal participants, they found that the difference between maximum and minimum elevations in each anterior or posterior surface had demonstrated the most area under ROC, implying that they are proper discriminating criteria. However, we evaluated more effective variables in addition to the corneal height which were far more sensitive and specific.
Besides pachymetric indices, we also considered indices obtained from the corneal curvature. ISV and IVA indices remained in the final model for detecting subclinical cases. Their predictive power in detecting subclinical keratoconus was higher than other known variables like maximum/mean keratometry. According to Table 5, more careful evaluation of the corneal is essential if IVA and ISV are more than 0.14 and 0.22, respectively. The results of the study conducted by Arbelaez et al14 who used an index similar to IVA confirm our findings. As expected, mean keratometry, which is probably the most widely used and common index in primary examination of keratoconic patients, was very effective in detecting the definite cases, and although values more than 47D are considered according to the routine definitions,15 we propose a cut-off point of 45D according to our findings. Of course, it is better to interpret it's values along with the data of corneal thickness, aberrometry indices (esp. 3rd order Coma aberration), and BAD_D.
According to our findings, 5th order vertical coma aberration of the front surface had the highest diagnostic validity for detecting the cases of subclinical keratoconus among all aberration indices of Pentacam, and 3rd order vertical coma aberration was the best index for diagnosing definite keratoconus. Different studies have proposed higher order aberrations for the diagnosis of keratoconus and its grading.16, 17 Gordon-Shaag recommended that aberration indices and vertical asymmetry should be simultaneously assessed, which is similar to our recommendation for subclinical cases.18 Moreover, Gordon-Shaag18 believed that although these indices may not be used in refractive surgery examinations, they should be routinely performed in addition to the assessment of corneal thickness and curvature for detecting subclinical keratoconus or when the odds of post-LASIK ectasia are high.
Many efforts have been made to propose multivariate models and machine learning methods for detecting keratoconus.19, 20 The sample size, methods of the diagnosis and classification of keratoconus, and consideration of the cases of subclinical keratoconus are very important while comparing these studies. Considering all the aforementioned points, the indices which were proposed in the final model of this study could enhance machine-learned diagnostic application of corneal imaging devices. Our study, with special attention to the cases of subclinical keratoconus and considering different aspects of the characteristics of the cornea, proposed effective indices in this regard, which are applicable and can be evaluated simultaneously by the ophthalmologist.
Although we implemented both clinical judgment and topographic evidences to define subclinical keratoconus cases as accurately as possible, it should be kept in mind that McMahon criteria are primarily based on placido-based topography, and this delicate point could somehow be challenging while discussing Pentacam images. This could be mentioned as a limitation of our study and should be interpreted with caution.
Simultaneous evaluation of BAD_D, 5th order vertical coma aberration, IVA, and ISV can help to detect the cases of subclinical keratoconus, especially if the pattern of the corneal surface curvature seems to be normal. It is very interesting that BAD_D shows the changes of the corneal surface far better than mean keratometry, even for detecting the cases of definite keratoconus. Although this finding does not reduce the importance of known indices like keratometry, it highlights the importance of new indices like BAD_D and coma aberration values. The cut-off points proposed in our study have acceptable specificity and sensitivity although further studies in this regard would result in more accurate cut-off values and their repeatability in different age and sex groups.
Footnotes
Peer review under responsibility of the Iranian Society of Ophthalmology.
Financial support: This project is funded by the Noor Ophthalmology Research Center.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- 1.Ayatollahi H., Rabi Mahboub M.R., Mohammadian N. Ratios of free to total prostate-specific antigen and total prostate specific antigen to protein concentrations in saliva and serum of healthy men. Urol J. 2007;4:238–241. [PubMed] [Google Scholar]
- 2.Rebenitsch R.L., Kymes S.M., Walline J.J. The lifetime economic burden of keratoconus: a decision analysis using a Markov model. Am J Ophthalmol. 2011;151:768–773. doi: 10.1016/j.ajo.2010.10.034. e762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dahl B.J., Spotts E., Truong J.Q. Corneal collagen cross-linking: an introduction and literature review. Optometry. 2012;83:33–42. doi: 10.1016/j.optm.2011.09.011. [DOI] [PubMed] [Google Scholar]
- 4.Randleman J.B., Trattler W.B., Stulting R.D. Validation of the ectasia risk score system for preoperative laser in situ keratomileusis screening. Am J Ophthalmol. 2008;145:813–818. doi: 10.1016/j.ajo.2007.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Binder P.S. Analysis of ectasia after laser in situ keratomileusis: risk factors. J Cataract Refract Surg. 2007;33:1530–1538. doi: 10.1016/j.jcrs.2007.04.043. [DOI] [PubMed] [Google Scholar]
- 6.Belin M.W., Khachikian S.S. An introduction to understanding elevation-based topography: how elevation data are displayed – a review. Clin Exp Ophthalmol. 2009;37:14–29. doi: 10.1111/j.1442-9071.2008.01821.x. [DOI] [PubMed] [Google Scholar]
- 7.Ambrosio R., Jr., Belin M.W. Imaging of the cornea: topography vs tomography. J Refract Surg. 2010;26:847–849. doi: 10.3928/1081597X-20101006-01. [DOI] [PubMed] [Google Scholar]
- 8.Chen D., Lam A.K. Reliability and repeatability of the Pentacam on corneal curvatures. Clin Exp Optom. 2009;92:110–118. doi: 10.1111/j.1444-0938.2008.00336.x. [DOI] [PubMed] [Google Scholar]
- 9.McMahon T.T., Szczotka-Flynn L., Barr J.T. A new method for grading the severity of keratoconus: the Keratoconus Severity Score (KSS) Cornea. 2006;25:794–800. doi: 10.1097/01.ico.0000226359.26678.d1. [DOI] [PubMed] [Google Scholar]
- 10.Correia F.F., Ramos L., Lopes B. Topometric and tomographic indices for the diagnosis of keratoconus. Int J Kerat Ect Cor Dis. 2012;1:92–99. [Google Scholar]
- 11.Ambrósio R., Jr., Faria-Correia F., Ramos I. Enhanced screening for ectasia susceptibility among refractive candidates: the role of corneal tomography and biomechanics. Curr Ophthalmol Rep. 2013;1:28–38. [Google Scholar]
- 12.Ambrosio R., Jr., Caiado A.L., Guerra F.P. Novel pachymetric parameters based on corneal tomography for diagnosing keratoconus. J Refract Surg. 2011;27:753–758. doi: 10.3928/1081597X-20110721-01. [DOI] [PubMed] [Google Scholar]
- 13.Ucakhan O.O., Cetinkor V., Ozkan M. Evaluation of Scheimpflug imaging parameters in subclinical keratoconus, keratoconus, and normal eyes. J Cataract Refract Surg. 2011;37:1116–1124. doi: 10.1016/j.jcrs.2010.12.049. [DOI] [PubMed] [Google Scholar]
- 14.Arbelaez M.C., Versaci F., Vestri G. Use of a support vector machine for keratoconus and subclinical keratoconus detection by topographic and tomographic data. Ophthalmology. 2012;119:2231–2238. doi: 10.1016/j.ophtha.2012.06.005. [DOI] [PubMed] [Google Scholar]
- 15.Rabinowitz Y.S., Rasheed K. KISA% index: a quantitative videokeratography algorithm embodying minimal topographic criteria for diagnosing keratoconus. J Cataract Refract Surg. 1999;25:1327–1335. doi: 10.1016/s0886-3350(99)00195-9. [DOI] [PubMed] [Google Scholar]
- 16.Alio J.L., Shabayek M.H. Corneal higher order aberrations: a method to grade keratoconus. J Refract Surg. 2006;22:539–545. doi: 10.3928/1081-597X-20060601-05. [DOI] [PubMed] [Google Scholar]
- 17.Buhren J., Kuhne C., Kohnen T. Defining subclinical keratoconus using corneal first-surface higher-order aberrations. Am J Ophthalmol. 2007;143:381–389. doi: 10.1016/j.ajo.2006.11.062. [DOI] [PubMed] [Google Scholar]
- 18.Gordon-Shaag A., Millodot M., Ifrah R. Aberrations and topography in normal, keratoconus-suspect, and keratoconic eyes. Optom Vis Sci. 2012;89:411–418. doi: 10.1097/OPX.0b013e318249d727. [DOI] [PubMed] [Google Scholar]
- 19.Twa M.D., Parthasarathy S., Roberts C. Automated decision tree classification of corneal shape. Optom Vis Sci. 2005;82:1038–1046. doi: 10.1097/01.opx.0000192350.01045.6f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Saad A., Gatinel D. Topographic and tomographic properties of forme fruste keratoconus corneas. Invest Ophthalmol Vis Sci. 2010;51:5546–5555. doi: 10.1167/iovs.10-5369. [DOI] [PubMed] [Google Scholar]