Abstract
Objective: Pathogen distribution characteristics of nephrology patients with urinary tract infections are studied, and drug resistance of nephrology and urinary tract infection disease are analyzed, so as to provide sufficient evidence for treatment of patients. Methods: Conduct randomized control study of 3500 cases of nephrology patients with urinary tract infections treated in different hospitals from December 2013 to December 2015, isolate pathogens in patients’ urine samples, perform identification and drug sensitive test and then conduct detailed analysis of drug resistance of pathogens. Results: Through isolation of pathogens, it can be found that all pathogens include Escherichia coli, Gram-positive cocci, gram-negative bacteria, fungi, Acinetobacter baumannii, Enterococcus faecalis, and urinary Enterococcus. Among them, proportion of E. coli is the largest. Patients have relatively high drug resistance to ceftriaxone, gentamicin, ciprofloxacin and cotrimoxazole. Conclusion: For nephrology patients with urinary tract infection, the main pathogen is E. coli, which has had some drug resistance. Drug resistance detection of pathogen should be strengthened in clinics, so as to provide strong guidance for clinical treatment and promote effective treatment of patients.
Keywords: Nephrology, Urinary tract infection, Pathogen, Distribution characteristic, Drug resistance
1. Introduction
Nephrology disease is kidney based disease of many patients. Nephrology diseases mainly include acute nephritis, chronic kidney disease and urinary tract infections. Nephrology disease can lead to decline in patients’ own immune system, resulting in poor application condition of patients and serious infections. Urinary tract infection is a common infection of nephrology disease, which causes a very serious impact on health of patients with nephrology disease. Therefore, analysis of pathogen distribution of nephrology patients with urinary tract infection should be strengthened, so as to realize diagnosis and treatment of urinary tract infection, and effectively improve treatment of urinary tract infections, which can promote effective recovery of nephrology patients with urinary tract infection. The pathogens under microscope is shown in Fig. 1.
Figure 1.
Pathogens under microscope.
2. Materials and methods
2.1. General information
The 3500 cases of nephrology patients admitted in different hospitals during December 2013–December 2015 were studied, and pathogen characteristics of urinary tract infection patients were studied. All samples of pathogens were provided by Clinical Laboratory Center of Ministry of Health.
2.2. Select appropriate instruments and reagents
Automated microbial analyzer produced in France was adopted for sample analysis, to be equipped with the appropriate bacterial identification and drug sensitive identification card.
2.3. Conduct drug sensitive test
Conduct drug sensitive test of samples in accordance with corresponding steps, with operation methods following corresponding operating instructions, and determine based on low drug sensitivity results of CLSI-S20 monitoring standards. The drug sensitive test is shown in Fig. 2.
Figure 2.

Drug sensitive test.
3. Results
3.1. Pathogen distribution of urinary tract infection patients
Among nephrology patients, a total of 3500 pathogens, 750 Gram-negative bacteria, 1060 Escherichia coli, 770 Klebsiella pneumoniae, 650 Gram-positive bacteria and 270 Acinetobacter baumannii were isolated.
3.2. Discussion of drug resistance of pathogens
E. coli, a common pathogen of sample pathogen of urinary tract infection patients, can have some resistance to drugs such as ceftriaxone, cefazolin, gentamicin and ciprofloxacin. E. coli is a common type of pathogen. Effective study of drug resistance of E. coli can strengthen clinical treatment of nephrology patients with urinary tract infection, and then improve clinical outcomes of patients, which is in favor of patients’ body health. The E. coli under microscope is shown in Fig. 3.
Figure 3.
Escherichia coli under microscope.
Enterococcus faecalis have strong drug resistance to tetracycline, erythromycin. Enterococcus faecium can have relatively strong resistance to penicillin, erythromycin and ciprofloxacin. E. faecalis and Staphylococcus epidermidis have relatively sensitive drug resistance. Hospitalized nephrology patients, especially during hospitalization after dialysis, will have serious infections, which is mainly respiratory tract infection, followed by urinary tract infection. During urinary tract infection, due to relatively complex physiological structure, the majority is caused by parasitic flora in intestinal tract, of which E. coli occupies absolute advantage. In the course of the study, among isolated pathogens, E. coli, ceftriaxone resistance rate is relatively high, which is relatively sensitive to ceftazidime of third-generation cephalosporin, with relatively strong resistance. E. coli can produce corresponding drug resistance to quinolone. In recent years, clinical application of fluoroquinolones has been continuously strengthened; then, bacterial resistance to these drugs has gradually strengthened, and different resistance strains can exhibit cross-resistance for different varieties.
E. faecalis, one of the most common Gram-positive coccus in urinary tract infection, is with relatively strong drug resistance to erythromycin and tetracycline. Therefore, in treatment of infection caused by E. faecalis, erythromycin and tetracycline should be avoided for treatment. Nitrofurantoin and stubborn miso also have good sensitivity to urinary tract infections caused by E. faecalis. E. faecalis can produce natural resistance to a variety of antibiotics, and emergence of vancomycin strains also provides some guidance for clinical treatment and laboratories. Infection caused by E. faecalis has clinically shown a significant upward trend in recent years. During clinical medicine testing and treatment, bacteriological examination and drug sensitivity test should be strengthened, so that such pathogen phenomenon can be effectively controlled and then infections can be effectively controlled (Chen et al., 2014). The E. faecalis under microscope is shown in Fig. 4.
Figure 4.
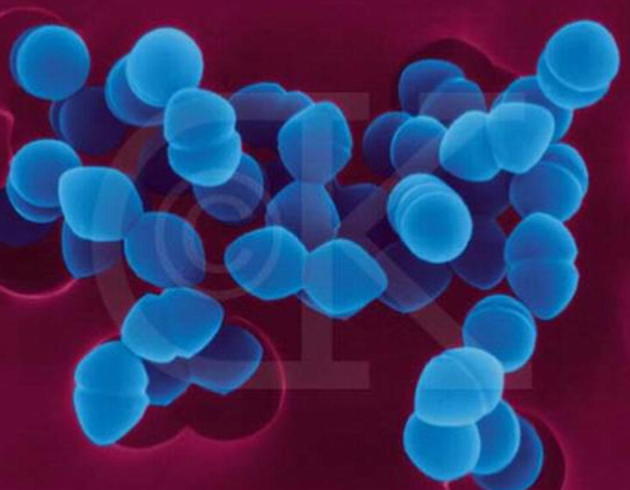
Enterococcus faecalis under microscope.
After nephrology patients have urinary tract infections, major disease pathogens feature E. coli and K. pneumoniae of Grand negative bacteria. Such pathogens have a strong resistance for cephalosporin and penicillin drugs, which brings some difficulties for treatment work. However, this pathogen has no drug resistance to amikacin and cefoxitin, and clinical resistance is relatively low. Amikacin drugs have relatively strong renal toxicity, which will increase renal impairment of renal tubular patient in the use process (Wang, 2014). Therefore, during treatment of nephrology urinary tract infection, treatment method should be carefully selected so as to improve safety of treatment work. Although imipenem is with a certain security in treatment of patients with urinary tract infection, price of this drug is actually relatively high, which will cause serious economic pressure for some patients with financial difficulties and thus is unacceptable. Therefore, based on overall consideration of a number of factors, piperacillin and nitrofurantoin should be selected so as to effectively treat urinary tract infection patients (Liu, 2014). Meanwhile, in the clinical treatment of urinary tract infections, aseptic technique should also be strengthened, and improper operation should be avoided to effectively evade urinary tract infections caused by non-standard operation (Yu et al., 2015), which can effectively reduce incidence of urinary tract infection and thus effectively improve treatment efficiency and quality of life of patients. At this stage, clinical use of antimicrobial agents has been strengthened in clinics, which results in constant change in pathogen variety and drug resistance of urinary tract infection patients. In response to this phenomenon, emphasis on pathogen detection and research in clinics should be strengthened, effective diagnosis and treatment of suspected cases of urinary tract infection should be done, urine culture and sensitivity test should be actively performed, and a relatively safe and effective antimicrobial agent should be selected based on patient pathogen detection result and drug resistance result, so as to improve clinical outcomes and promote early recovery of patients (Qin et al., 2015).
At this stage, a certain number of patients are admitted to hospitals every day. The great number of patients will make spread of bacteria between patients more convenient and make patient more easily accessible to polluted air. Some patients have long-term treatment of bed rest, which increases the chances of infection (August et al., 2016). Some older patients with longer hospital stay tend to use many types of antibiotics, which makes drug invasiveness to patients enhanced. Therefore, pathogen detection of urinary tract infection patients should be strengthened in clinics, in order to conduct effective analysis of drug resistance and achieve effective treatment of patients (Cheng, 2015).
3.3. Infection control measures
For reasons of urinary tract infections, appropriate therapeutic measures should be taken for prevention and treatment of urinary tract infection (Wang, 2015). First, intensity of basic nursing care of patients should be strengthened. For different types of diseases, classification diagnosis and treatment should be conducted to avoid phenomenon of cross-infection among patients. During hospitalization, patients’ wards should also be ventilated, clean and tidy, in order to allow timely treatment of patients. Meanwhile, toilet disinfection should be conducted to prevent bacterial attack and reproduction, which can maximally avoid spread of bacteria, and also reduce possibility of infection among patients (Mellotte et al., 2015). In addition, management of hospital treatment work should be strengthened. In the course of treatment for patients, strict management of therapeutic equipment should be done, and aerosol inhalation tubes and injection utensils should be cleaned and disinfected in a timely manner. For patients with poor physical characteristics, necessary management of antimicrobial drugs should also be done. Before use of antibiotics, detection of pathogens should be strengthened and necessary drug trials should be done to avoid infection in patients in course of medication (Li and Qin, 2013).
4. Discussion and conclusion
All in all, pathogen distribution of nephrology patients with urinary tract infections shows certain characteristics. E. coli is one of the most important pathogens. Study of distribution of pathogens and necessary analysis of drug resistance in patients can provide some guidance for clinical treatment work, enable patients to receive effective treatment, and prevent disease progression in patients and thus is with very significant clinical significance.
Footnotes
Peer review under responsibility of King Saud University.
References
- August D.A., Kallogjeri D., Lewison G., Chen X. Nutrition support in surgical oncology. Asian Pac. J. Surg. Oncol. 2016;2:153–162. [Google Scholar]
- Chen Y.F., Zhao F., Mei C.X. Pathogen distribution and drug resistance analysis of nephrology patients with urinary tract infection. Chinese J. Nosocomiol. 2014;11:574–576. [Google Scholar]
- Cheng X.X. Pathogen distribution and drug resistance analysis of 360 cases of nephrology patients with urinary tract infection. Chinese Commun. Doctors. 2015;16:12–15. [Google Scholar]
- Li G.F., Qin Y.H. Pathogen distribution and drug resistance analysis of nephrology patients with urinary tract infection. J. Clin. Exp. Med. 2013;13:718–719. [Google Scholar]
- Liu Z. Pathogen distribution and drug resistance analysis of nephrology patients with urinary tract infection. Guide China Med. 2014;17:125–126. [Google Scholar]
- Mellotte G., Maher V., Devitt P.G., Shin V.Y., Leung C.P. Minimally invasive surgical oncology: state of the art. Asian Pac. J. Surg. Oncol. 2015;1:101–112. [Google Scholar]
- Qin Y.F., Yuan H., Hu F.Q., Gong J.H., Cui L. Pathogen distribution and drug resistance analysis of nephrology patients with urinary tract infection. Chinese J. Nosocomiol. 2015;31:546–548. [Google Scholar]
- Wang X.H. Pathogen distribution and drug resistance analysis of nephrology patients with urinary tract infection. Chinese Foreign Med. Res. 2015;14:125–127. [Google Scholar]
- Wang Y.Q. Pathogen distribution and drug resistance analysis of nephrology patients with urinary tract infection. Qingdao Med. J. 2014;9:295–296. [Google Scholar]
- Yu F., Hou T.Y., Fang X.W., Hu W.X., Qian Y.J., Liu W., Wu Y.H., He W.N., Hao W.K. Pathogen distribution and drug resistance analysis of elderly patients with urinary tract infections in general wards and ICU. Chinese J. Nosocomiol. 2015;23:318–320. [Google Scholar]


