Abstract
Aims
To report a patient with unrecognized small macular melanoma, who gradually developed neovascular glaucoma that was treated with an Ahmed valve. We presume that tumor cells gained access to the orbit through this aqueous drainage device.
Methods
The medical records pertaining to 5 different centers, the results of imaging studies, the clinical course of the patient and histopathological findings were retrospectively reviewed.
Results
A 61-year-old man presented with a blind and painful proptotic right eye. Retinal hemorrhage had been suspected 3 years earlier and followed accordingly thereafter. Yearly performed MRI studies demonstrated the steady growth of the hemorrhagic lesion/tumor. Meanwhile, he developed neovascular glaucoma first treated unsuccessfully with cyclocryotherapy then with implantation of an Ahmed valve. Right proptosis became evident within a year, and a final MRI study revealed a large retrobulbar mass. Orbital exenteration was performed and histopathological examination showed intraocular and orbital epithelioid cell melanoma. Tumor cells were also found within the reservoir of the Ahmed valve. The patient died of widespread metastases 1 year later.
Conclusions
Ahmed valve implantation in an eye with unsuspected macular choroidal melanoma may ultimately be associated with extraocular extension and orbital tumor formation.
Key Words: Choroidal melanoma, Neovascular glaucoma, Ahmed valve, Orbit, Extraocular extension, Exenteration
Introduction
Extraocular tumor extension is reported to occur in 3-14.6% of eyes enucleated for uveal melanoma [1,2]. Massive orbital invasion is rare and has been diagnosed in 0.5% of patients in a large series [3]. Possible routes of exit include the trabecular meshwork and Schlemm's canal, anterior and posterior ciliary arteries, vortex veins, long and short ciliary nerves and through direct scleral perforation, all of which may occur also with relatively small choroidal melanomas [1,4].
We herein report a patient who developed massive retrobulbar orbital melanoma presumably egressing through an Ahmed valve, originating from an unsuspected macular choroidal melanoma and masked longtime by subretinal hemorrhage, cataract and neovascular glaucoma.
Case Report
In September 2011, a 61-year-old man presented with a blind and painful proptotic right eye. Because he was travelling frequently, all his previous ocular examinations and surgical procedures were performed elsewhere, each at different centers. His complaints with his right eye started 3 years earlier when he experienced acute right upper altitudinal hemianopia, which was attributed to a localized subretinal hemorrhage of unknown origin (fig. 1). Ocular ultrasonography and MRI studies (fig. 2a) were inconclusive, and since a melanocytic lesion could not be definitely ruled out, close follow-up was recommended. In December 2009, another MRI study showed that the size of the lesion was increasing (fig. 2b), although clinically, no change was noted. Eight months later, he suffered a sudden loss of vision in the right eye and received the diagnosis of neovascular glaucoma. After 2 unsuccessful attempts to control the intraocular pressure (IOP) with cyclocryotherapy, an Ahmed valve was implanted to the right eye in August 2010. His right IOP varied between 20-28 mm Hg with the valve in place, but a 360° cyclocryotherapy was again performed in July 2011 for ‘uncontrollable neovascular glaucoma’ while he was in the United States. After this procedure he noticed progressive forward displacement of his right eye.
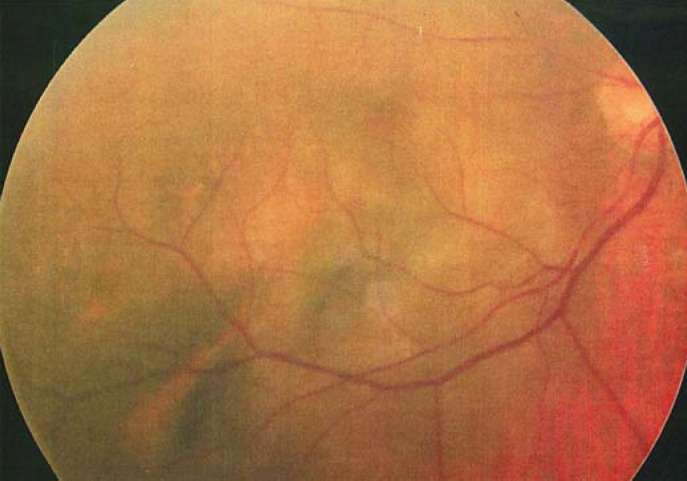
Fig. 1.
Right fundus view when his complaints first started in December 2008. This was also the last time that the right fundus could clearly be visualized.
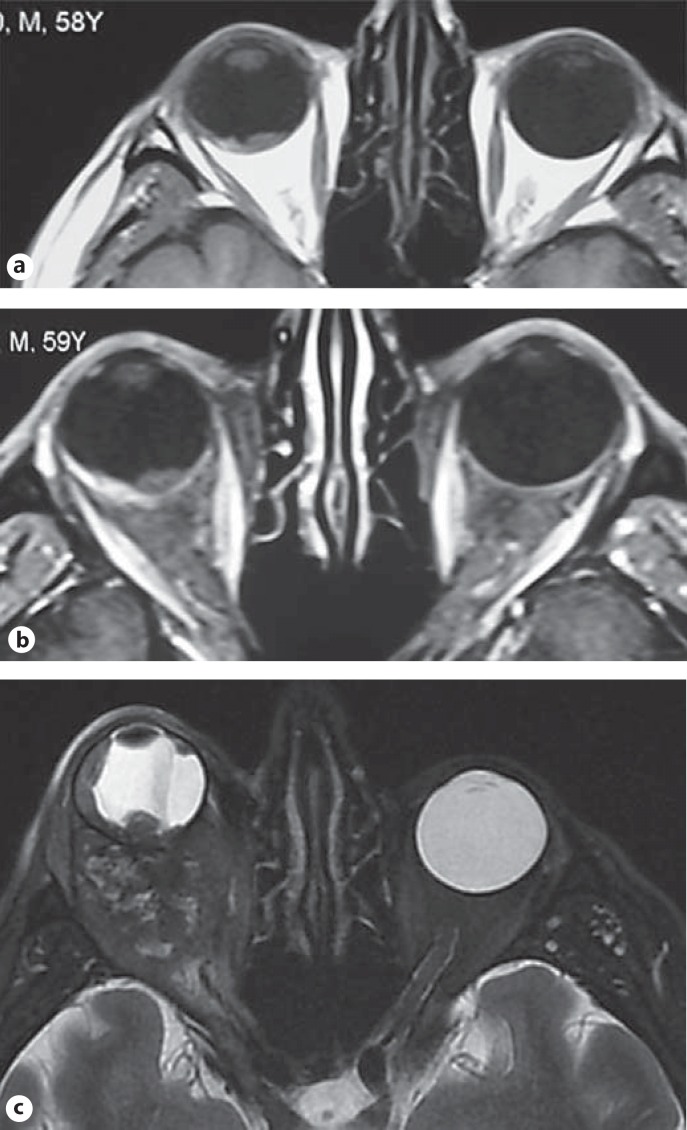
Fig. 2.
Axial orbital MRI studies through the course of the disease. a December 2008 at initial presentation; contrast-enhanced T1W scan shows an intraocular irregular hyperintense and a less hyperintense area side by side probably corresponding to the melanocytic lesion and subretinal hemorrhage, respectively. b December 2009; slight growth of the lesion with persistent subretinal hemorrhage. c September 2011; this T2W image reveals a retrobulbar mass and intraocular anterior progression of the tumor on the temporal side.
On our examination, his vision was no light perception in the right eye and 20/20 in the left eye. He had 5-mm (Hertell) axial proptosis of the right eye with conjunctival hyperemia. The drainage device was visible in the upper temporal subconjunctival space. The anterior chamber was shallow. There were seclusio pupillae, ectropion uveae and diffuse iris neovascularization. The dense cataract and hemorrhage on its anterior surface impeded visualization of the fundus. B-mode ultrasonography demonstrated a hyperechogenic solid mass with 4.7 mm of thickness in the posterior pole with total retinal detachment. The left eye was normal. An orbital MRI study revealed a posteriorly located intraocular mass which extended to the ciliary body as a continuous uveal thickening on the temporal side. There was also a large retrobulbar mass without intracranial extension (fig. 2c). With the suspicion of a choroidal melanoma with extrascleral spread, the right orbit was exenterated (fig. 3a, b). Histopathologically, both intraocular and orbital tumors were composed of epithelioid melanoma cells (fig. 3c). The sclera and the optic nerve head were intact. The reservoir of the Ahmed valve contained tumor cells. The patient then received 50 Gy LINAC-based stereotactic radiosurgery to the orbit but died of widespread systemic metastases 1 year later.
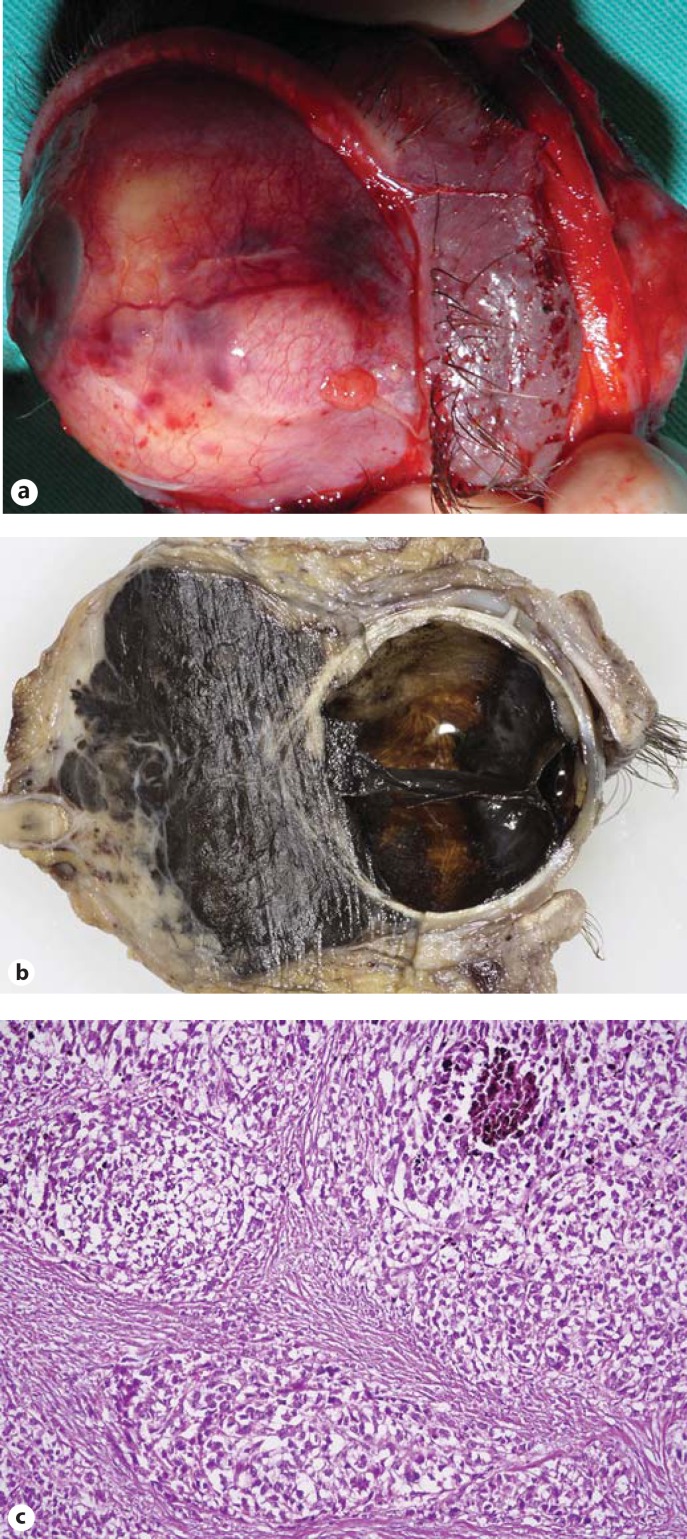
Fig. 3.
Exenteration specimen. a Gross view showing the subconjunctival Ahmed reservoir. b Sagittal cut demonstrates total retinal detachment, anterior advancement of the tumor and the massive retrobulbar tumor. c Histopathological analysis of the orbital part of the tumor reveals large epithelioid cells (HE, original magnification ×80).
Discussion
Secondary elevation of IOP may be encountered in 3-57% of eyes harboring uveal melanoma in general, and a breakdown of cases shows that 2% of choroidal melanomas, 7% of iris melanomas and 17% of ciliary body melanomas may be associated with secondary glaucoma [5,6]. The underlying mechanisms of pressure elevation include tumor invasion of aqueous drainage channels, tumor-induced neovascular glaucoma, elevated episcleral venous pressure as the result of extraocular tumor extension and severe inflammation caused by tumor necrosis [6,7]. The latter is often associated with uveitis, scleritis, retinal detachment and iris neovascularization [8]. Of interest is the fact that an untreated small- to medium-sized posterior uveal melanoma perhaps adopting several of these mechanisms had ultimately led to intractable glaucoma in the right eye of our patient.
Intraocular surgical procedures in eyes with untreated uveal melanomas have always raised concerns. Although rare, extraocular tumor extension was documented following vitrectomy, fine needle aspiration and open biopsies [9]. Moreover, a recent study demonstrated extraocular tumor dissemination in 5 patients with unrecognized malignant nonteratoid medulloepithelioma, ciliochoroidal melanoma and diffuse iris melanoma who also had aqueous tube shunt implantation [6]. The authors of that study concluded that aqueous tube shunts could have served as access routes to extraocular structures particularly for untreated anterior segment tumors [6]. There are conflicting outcome reports on the use of aqueous shunt devices and filtration surgery in eyes with previously treated uveal melanomas. One study found that the Baerveldt shunt was effective in lowering the IOP in 86% of 31 eyes with anterior uveal melanoma which had secondary glaucoma due to previous treatment with proton beam radiotherapy [5]. None of these patients developed extraocular tumor extension or metastases [5]. In contrast, two studies reporting on two patients previously treated with plaque brachytherapy for ciliary body melanomas casted doubt on the safety of drainage surgery if secondary glaucoma is to be managed [10,11]. One patient had orbital recurrence 11 years after Baerveldt tube shunt implantation, and the other patient developed extraocular spread 5 years after trabeculectomy [10,11].
Our patient demonstrates the fatal outcome of follow-up at various noncommunicating centers. Unilateral, unexpected neovascular glaucoma, cataract or retinal detachment should always arouse the suspicion of an unrecognized intraocular tumor. Intraocular surgery and tube-shunt implants in particular must be avoided until any malignancy can be safely excluded in these eyes.
Statement of Ethics
Informed consent was obtained from the wife of the patient to utilize all available medical records for publication and other educational purposes.
Disclosure Statement
The authors have no conflicts of interest. The authors did not receive any funding or sponsorship for the preparation of the manuscript.
References
- 1.Coupland SE, Campbell I, Damato B. Routes of extraocular extension of uveal melanoma. Risk factors and influence on survival probability. Ophthalmology. 2008;115:1778–1785. doi: 10.1016/j.ophtha.2008.04.025. [DOI] [PubMed] [Google Scholar]
- 2.Bellmann C, Lumbroso-Le Ruic L, Levy C, et al. Uveal melanoma: management and outcome of patients with extraocular spread. Br J Ophthalmol. 2010;94:569–574. doi: 10.1136/bjo.2009.165423. [DOI] [PubMed] [Google Scholar]
- 3.Shields JA, Shields CL. Massive orbital extension of posterior uveal melanomas. Ophthalmic Plast Reconstr Surg. 1991;7:238–251. doi: 10.1097/00002341-199112000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Wolter JR. Orbital extension of choroidal melanoma: within a long posterior ciliary nerve. Trans Am Ophthalmol Soc. 1983;81:47–63. [PMC free article] [PubMed] [Google Scholar]
- 5.Sharkawi E, Oleszczuk JD, Bergin C, Zografos L. Baerveldt shunt in the treatment of glaucoma secondary to anterior uveal melanoma and proton beam radiotherapy. Br J Ophthalmol. 2012;96:1104–1107. doi: 10.1136/bjophthalmol-2011-301420. [DOI] [PubMed] [Google Scholar]
- 6.Kaliki S, Eagle RC, Grossniklaus HE, Campbell J, Shields CL, Shields JA. Inadvertent implantation of aqueous tube shunts in glaucomatous eyes with unrecognized intraocular neoplasms: report of 5 cases. JAMA Ophthalmology. 2013;131:925–927. doi: 10.1001/jamaophthalmol.2013.828. [DOI] [PubMed] [Google Scholar]
- 7.Shields CL, Shields JA, Shields MB, Augsburger JJ. Prevalence and mechanisms of secondary intraocular pressure elevation in eyes with intraocular tumors. Ophthalmology. 1987;94:839–846. doi: 10.1016/s0161-6420(87)33537-7. [DOI] [PubMed] [Google Scholar]
- 8.el Baba F, Hagler WS, De la Cruz A, Green WR. Choroidal melanoma with pigment dispersion in vitreous and melanomalytic glaucoma. Ophthalmology. 1988;95:370–377. doi: 10.1016/s0161-6420(88)33186-6. [DOI] [PubMed] [Google Scholar]
- 9.Schefler AC, Gologorsky D, Marr BP, Shields CL, Zeolite I, Abramson DH. Extraocular extension of uveal melanoma after fine-needle aspiration, vitrectomy and open biopsy. JAMA Ophthalmology. 2013;131:1220–1224. doi: 10.1001/jamaophthalmol.2013.2506. [DOI] [PubMed] [Google Scholar]
- 10.Sweeney AR, Keene CD, Klesert TR, Jian-Amadi A, Chen PP. Orbital extension of anterior uveal melanoma after Baerveldt tube shunt. Can J Ophthalmol. 2014;49:e133–e135. doi: 10.1016/j.jcjo.2014.08.009. [DOI] [PubMed] [Google Scholar]
- 11.Tay E, Cree IA, Hungerford J, Franks W. Recurrence of treated ciliary body melanoma following trabeculectomy. Clin Exp Ophthalmol. 2009;37:503–507. doi: 10.1111/j.1442-9071.2009.02069.x. [DOI] [PubMed] [Google Scholar]