Abstract
Objective
Treatment programs for intimate partner violence (IPV) evidence high rates of noncompliance, which is associated with repeat offending. Problematic alcohol use is reported in approximately half of all partner violent offenders and represents a strong risk factor for treatment noncompliance. However, previous research with IPV offenders mandated to treatment has not evaluated methods to mitigate the effects of alcohol misuse on treatment compliance.
Method
In the current study, 60 male IPV offenders (25 binge drinkers) were randomly assigned to a single-session brief motivational interview (BMI) or control intervention prior to treatment commencement. Treatment compliance data were collected six months later.
Results
Findings indicated that binge drinkers had lower treatment compliance than non- binge drinking participants, and that binge drinking BMI participants attended more treatment sessions and evidenced lower dropout rates than binge drinking control participants.
Conclusions
Findings highlight the importance of individualized treatment planning for IPV offenders in order to maximize available resources while accommodating the needs of males at greatest risk for noncompliance and continued violence.
Keywords: Partner violence, binge drinking, treatment compliance, motivational interviewing
Treatment programs for perpetrators of intimate partner violence (IPV) are plagued by high rates of attrition, poor treatment compliance, and high rates of IPV-related as well as general criminal recidivism (for a comprehensive review, see Smedslund, Dalsbø, Steiro, Winsvold, & Clench-Aas, 2011). Cadsky and colleagues (1996) found that fewer than half of men referred to treatment attended the first session and that approximately 25% completed all treatment requirements. Evidence suggests that attrition from IPV treatment programs and a general pattern of noncompliance are predictive of IPV and other criminal recidivism (Babcock & Steiner, 1999; Gondolf, 2000) and underlie the general lack of evidence of these programs' effectiveness (Babcock, Green, & Robie, 2004; Eckhardt et al., 2013; Feder & Wilson, 2005). An improved understanding of the factors that place offenders at risk for noncompliance may aid in developing more effective IPV treatment approaches. In the present study, we examined binge drinking as a risk factor for treatment noncompliance, and evaluated whether a single session motivational interview administered in advance of IPV treatment would improve outcomes for binge drinkers relative to non-binge drinkers at follow-up.
Factors associated with poor treatment compliance and high attrition have been evaluated extensively in the literature. In a systematic review, Daly and Pelowski (2000) found that substance use problems were associated with elevated rates of treatment attrition among IPV perpetrators. Problematic alcohol use, as indicated by quantity/frequency of use and presence of clinically significant symptomatology, predict treatment noncompliance and IPV recidivism (e.g., Cadsky et al., 1996; Hamberger & Hastings, 1989). In a recent meta-analytic review of 15 studies, Oliver and colleagues (2011) found a small, significant association between problematic alcohol use and treatment attrition among IPV perpetrators (rw = .12, 95% CI = .07 - .10).
The association between alcohol problems and treatment noncompliance is particularly concerning in light of the elevated rate of alcohol use among IPV offenders. Approximately 50% of IPV perpetrators engaged in treatment report concurrent alcoholic tendencies or alcohol use disorders (e.g., Gondolf, 1999; Stuart, Moore, Kahler, & Ramsey, 2003). Despite this association, few treatment approaches systematically address or integrate substance use problems into IPV-related intervention programming, with the standard of care typically involving a mandate for offenders to attend separate substance abuse and IPV abatement programs when problematic substance use is present (Babcock et al., 2004). Such referrals to separate treatments are particularly ineffective (Schumacher et al., 2003), intimating the need for integrated techniques that may mitigate the effects of alcohol problems on treatment compliance among IPV offenders (Easton, Mandel, Hunkele, Nich, Rounsaville, & Carroll, 2007). Substance involved clients identify a lack of perceived benefits from treatment and past failures as obstacles to successful treatment completion (Cunningham et al., 1993), suggesting that interventions designed to increase self-efficacy and improve motivation to change may be particularly beneficial for IPV clients with co-occurring substance use issues.
Although we are aware of no research examining the efficacy of interventions that may reduce the effects of alcohol use on IPV-related treatment compliance, brief motivational interviewing (BMI) was developed to engage clients with substance use disorders and has been validated as a method to improve treatment compliance and outcomes across various clinical samples (for a review, see Lundahl, Kunz, Brownell, Tollefson, & Burke, 2010). BMI is, by definition, a client-centered approach that is designed to aid clients in resolving ambivalence and evoking their own, internal motivations to change problem behaviors through encouraging client autonomy and collaboration with treatment providers (Miller & Rollnick, 2002). The critical content of BMI is delivered in one or two sessions and may be adapted to the presenting problem. Several studies have examined the effects of BMI on treatment compliance within IPV samples and the initial findings suggest generally positive effects (e.g., Musser, Semiatin, Taft, & Murphy, 2008; Woodin & O'Leary, 2010). For example, Taft and colleagues (2001) reported that among a sample of 189 offenders, males in a treatment with regular BMI supplements attended more sessions and evidenced higher treatment completion rates than males who underwent a standard treatment regimen. More recently, Crane and Eckhardt (2013) found that a single session BMI improved overall treatment compliance but failed to significantly increase session attendance or reduce recidivism among a sample of 82 male offenders. Thus, while disparate literatures suggest that BMI may result in higher treatment compliance among substance abusers or IPV offenders, none of the previous investigations have evaluated the effects of BMI on treatment compliance among the large, high risk subset of IPV males who report alcohol misuse.
The current analyses aimed to address this critical and neglected issue by examining if the positive effects of MI on treatment compliance detected among IPV perpetrators in general are also observable among IPV offenders with problematic drinking. We randomly assigned recently adjudicated male IPV offenders to either a single BMI session or a control group to determine the relative effects of pretreatment BMI on treatment compliance among offenders with and without a history of binge drinking. Based upon theory and research previously described, we expected to find an interaction between treatment condition and binge drinking with stronger effects of MI among binge drinkers than non-binge drinkers, such that 1) poorer session attendance and 2) higher dropout rates would be observed among binge drinkers in the control condition relative to all other groups.
Method
Participants
The current sample was part of a larger study designed to evaluate the validity of motivational interviewing as a treatment adjunct among partner violent offenders (Crane & Eckhardt, 2013). The current analyses involved 60 IPV offenders who were at least 18 years old, had been adjudicated for an IPV offense within 2 weeks, had no active protection orders, and were mandated to attend an IPV treatment program. Men in the current sample were, on average, 33.1 (SD = 11.0) years of age and reported 1.6 (SD = 1.9) prior arrests, relationships of 8.1 (SD = 8.3) years, Caucasian (50.0%) or African American (48.3%) ethnicity, and limited education with 44 (73.3%) participants reporting a high school diploma or less. Forty-seven (78.3%) participants were parents. Consistent with previous research (e.g., Stuart et al., 2003), 25 (41.7%) participants reported problematic alcohol use in the form of binge drinking, and 21 (35.0%) participants reported the use of illicit substances.
Procedures and Measures
All study procedures were approved by the appropriate institutional review board. Participants were recruited, provided written informed consent, and completed active involvement in the current study during their first probation appointment. Participants first completed a self-report assessment battery including 1) a sociodemographic questionnaire (i.e. age, number of prior arrests), 2) the Dyadic Adjustment Scale – 4 (DAS-4; Sabourin, Valois, Lussier, 2005), a brief and reliable (α = .81-.92) measure of relationship satisfaction with response options ranging from “never” or “extremely unhappy” to “always” or “extremely happy”, 3) the Safe At Home Scale (SAH; Begun et al., 2003), a reliable (α = .67 - .87; Eckhardt & Utschig, 2007) 35-item IPV specific readiness to change abusive behavior measure, 4) the Drug Use Disorder Identification Test (DUDIT; Berman et al., 2005), a 4-item measure used here to assess the presence or absence of self-reported illicit substance use, and 5) the Alcohol Use Disorder Identification Test (AUDIT; Saunders et al., 1993), an alcohol use inventory used in the current investigation to assess the presence of binge drinking at least once a month. Binge drinking, consuming five or more drinks in a drinking episode, is considered a superior predictor of alcohol problems and violent behavior than frequency of use (see Leonard, 2005).
Participants were then randomly assigned to a control condition in which they completed additional unrelated measures, or to the BMI condition in which they participated in a single motivational interview session for IPV perpetration (Murphy & Eckhardt, 2005). Administration procedures and interview content is detailed elsewhere (Crane & Eckhardt, 2013). This study was conducted prior to the publication of the most recent edition of Miller and Rollnick's (2012) Motivational Interviewing text. Briefly, sessions began with the use of open ended questions and reflection to elicit ambivalence as well as expand upon change talk that was detected during the completion of the SAH inventory and a brief relationship description provided by the participant. Content of all BMI sessions was driven by interactions with the participant in the spirit of MI and focused on the identified change goal of nonviolent behavior within the context of intimate relationships. Thus, the content of each session varied considerably and alcohol use behavior was discussed only when identified as problematic by the participant. When indicated by participant preparedness, the clinician attempted to work with participants to generate a plan of action, including behavioral change and available resources (e.g., family members, a treatment facility) that could result in nonviolent relationship conditions with current or future partners.
BMI sessions were conducted by a clinician trained in MI techniques. Eight sessions (16.7%) were transcribed and an experienced MI-oriented clinician reviewed both audio recordings and transcripts using the Motivational Interviewing Treatment Integrity (MITI) Code system, version 3.1.1 (Moyers, Martin, Manuel, Miller, & Ernst, 2010). The MITI system provides codes for five global scales to indicate MI adherence (empathy, collaboration, evocation, autonomy/support, and direction) that are scored on a scale from 1 (low) to 5 (high). Specific behaviors are also counted, but were not the focus of this initial investigation into the effects of BMI on the relationship between problematic alcohol use and treatment compliance among IPV offenders. MITI competency is defined as an average of four on the global ratings (Moyers et al., 2010). Review of randomly sampled 20-minute segments of each tape concluded that the clinician had a mean adherence of 4.60 across the global scales, indicating acceptable proficiency in MI adherence. Participants then underwent debriefing and were compensated. Treatment compliance data, including the number of sessions attended and enrollment status (active or dropped out), were collected from probation records six months later. The number of sessions attended is the most representative measure of treatment dosage from a methodological standpoint (Daly, Power, & Gondolf, 2001).
Data Analytic Strategy
To examine the relationship between treatment condition, alcohol binge drinking, and number of treatment sessions attended, a linear regression was conducted controlling for age, readiness to change, relationship satisfaction, drug use, and prior arrests. Inspection of the number of sessions attended revealed minor skewness (skewness value = 1.097), therefore the model was estimated using robust standard errors (MLR estimation in MPLUS 7.11; Muthen & Muthen, 2013). To examine the relationships between treatment condition, alcohol binge drinking, and dropout rates, a logistic regression was conducted controlling for age, readiness to change, relationship satisfaction, drug use, and prior arrests. For both analyses, missing data were handled using full-information maximum likelihood estimation (FIML). See Table 1 for a summary of overall means, standard deviations, and bivariate correlations.
Table 1. Summary of means, standard deviations, and bivariate correlations.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | M | SD | |
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||||
| 1. # Sessions | -- | 11.092 | 9.610 | ||||||||
| 2. Dropout | -.602** | -- | 0.328 | 0.473 | |||||||
| 3. Age | .136 | -.265* | -- | 33.067 | 11.044 | ||||||
| 4. Drug Use | -.138 | .189 | .002 | -- | 0.350 | 0.481 | |||||
| 5. Readiness | .278* | -.133 | .413** | .010 | -- | 22.545 | 12.793 | ||||
| 6. Satisfaction | .338* | -.155 | -.085 | -.166 | -.243 | -- | 4.183 | 1.244 | |||
| 7. Prior Arrests | .161 | .024 | .145 | .116 | .089 | .180 | -- | 1.567 | 1.854 | ||
| 8. Binge Drinking | -.138 | .185 | .016 | .159 | .050 | -.105 | .236 | -- | 0.417 | 0.497 | |
| 9. Condition | .157 | -.232 | .027 | .360** | .023 | .002 | .061 | .323 | -- | 0.517 | 0.504 |
Note: Dropout (0=no, 1=yes); Readiness = Safe at Home Scale readiness to change total score; Satisfaction = Dyadic Adjustment Scale-4 relationship satisfaction total score; Binge (0=no, 1=yes); Condition (0=control condition, 1=treatment condition).
p < .01,
p < .05.
Results
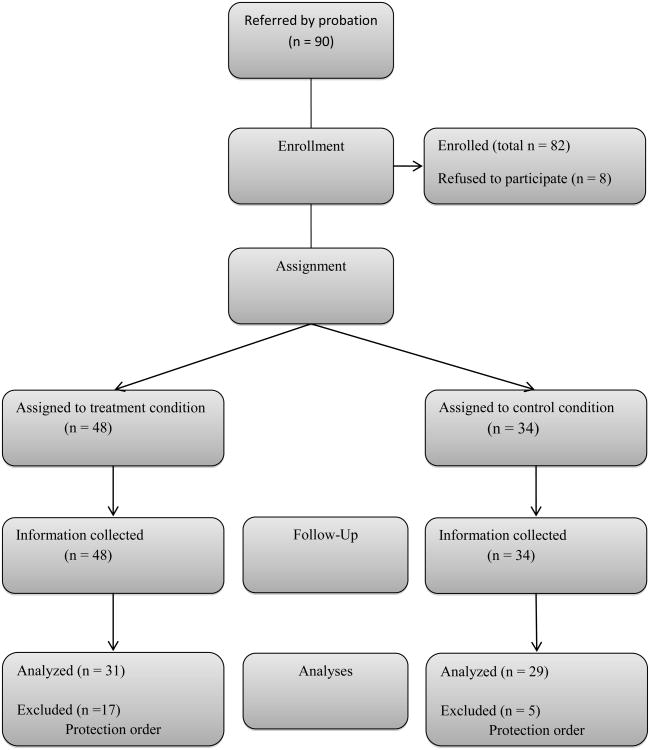
Analyses suggested that the randomization procedure was successful. Thirty-one participants (11 binge drinkers) were randomly assigned to the BMI condition and 29 participants (14 binge drinkers) were randomly assigned to the control condition (Figure 1). There were no significant differences between BMI and control groups on participant education, relationship duration, or self-reported physical and psychological IPV perpetration. Raw descriptive outcome data across treatment condition and binge drinking groups are presented in Table 2.
Figure 1. Flow of Participants through Each Stage of the Study.
Table 2.
Raw means and standard deviations for session attendance as well as percentage of dropout across treatment condition and binge drinking groups.
| Control/No Binging | Control/Binging | Treatment/No Binging | Treatment/Binging | |
|---|---|---|---|---|
|
|
||||
| Average # Sessions | 13.00 (10.86) (n = 15) |
3.44 (5.77) (n = 9) |
11.35 (8.45) (n = 20) |
14.60 (10.08) (n = 10) |
| % Dropout | 26.7 (n = 15) |
66.7 (n = 12) |
25.0 (n = 20) |
18.2 (n = 11) |
Note: n's = number of subjects with data on variable of interest.
Treatment Sessions
To examine hypothesis 1, that binge drinking control participants would attend fewer sessions than binge drinking BMI participants and non binge drinking control participants, we regressed the number of treatment sessions onto treatment condition, binge drinking, and their interaction while controlling for age, readiness to change, relationship satisfaction, illicit drug use, and prior arrests. Results indicated a significant Treatment Condition × Binge Drinking interaction (β = .438, p = .010; See Figure 2 top panel and Table 3 for summary of results). Follow-up analyses indicated that binge drinking BMI participants attended more sessions when compared to binge drinking control participants (estimate = 10.544, p = .002). No significant differences were found between BMI and control conditions among those without episodes of binge drinking (estimate = -.193, p = .943). Furthermore, binge drinking control participants attended significantly fewer sessions than non binge drinking control participants (estimate = -7.588, p = .007). Finally, although binge drinking BMI participants attended an average of three more sessions than non binge drinking BMI participants, this difference was not significant (estimate = 3.148, p = .397).
Figure 2.
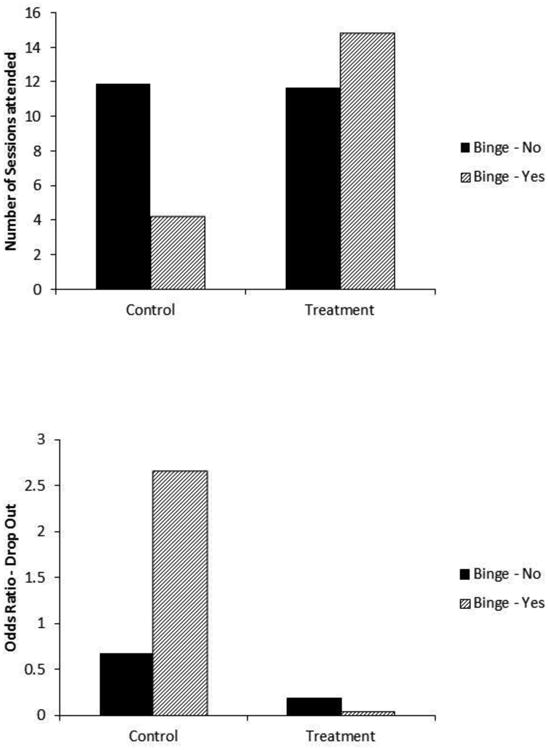
Binge use × Treatment Condition interaction for number of sessions attended (top panel) and dropout odds ratios (bottom panel).
Table 3.
Summary of unstandardized estimates and standard errors for Number of Sessions attended and Dropout.
| # of Sessions Attended | Dropped Out of Treatmenta | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Estimate | SE | p-value | Estimate | SE | p-value | |
| Age | -.013 | .120 | .912 | -.079 | .040 | .049 |
| Drug Use | -1.786 | 2.609 | .494 | 1.661 | .955 | .082 |
| Readiness | .212 | .076 | .005 | -.014 | .031 | .656 |
| Satisfaction | 2.982 | .842 | .000 | -.415 | .286 | .146 |
| Prior Arrests | .087 | .766 | .910 | .359 | .222 | .106 |
| Binge | -7.588 | 2.824 | .007 | 1.381 | .988 | .162 |
| Condition | -.193 | 2.717 | .943 | -1.285 | 1.087 | .237 |
| Binge × Condition | 10.737 | 4.178 | .010 | -2.745 | 1.561 | .079 |
Unstandardized estimates are logits from a logistic regression (dropout; 0=no, 1=yes)
Note: Readiness = Safe at Home Scale readiness to change total score; Satisfaction = Dyadic Adjustment Scale-4 relationship satisfaction total score; Binge (0=no, 1=yes); Condition (0=control condition, 1=treatment condition).
Dropout Rates
To examine hypothesis 2, that binge drinking control participants would be more likely to drop out of treatment than binge drinking BMI participants or non binge drinking control participants, treatment dropout (0=no, 1=yes) was regressed onto treatment condition, binge drinking, and the interaction while controlling for age, readiness to change, relationship satisfaction, illicit drug use, and prior arrests. Results indicated a marginally significant Treatment Condition × Binge Drinking interaction (p = .079; See Figure 2 bottom panel and Table 3 for summary of results). Follow-up analyses indicated that binge drinking control participants (odds ratio = 2.656, p= .184) were at a significantly greater risk of dropping out of treatment when compared to binge drinking BMI participants (odds ratio = .047, p = .012; logit difference = -4.029, p = .007). No significant differences were found between the control (odds ratio = .668, p = .574) and treatment conditions (odds ratio = .185, p = .016) among those without episodes of binge drinking (logit difference = -1.285, p = .237). Dropout rates between the binge drinking and the non-binge drinking groups did not differ within either the control (logit difference = -1.381, p = .162) or the BMI (logit difference = 1.364, p = .267) condition.
Discussion
The current study is the first to evaluate the utility of implementing brief motivational interviewing to improve treatment compliance among partner violent offenders who report binge drinking and, therefore, represent a group at particularly elevated risk of treatment dropout. Results showed that BMI improved outcomes, using both attendance and dropout as indicators of treatment compliance, among only those participants who endorsed binge drinking. Specifically, binge drinking BMI participants attended more sessions than binge drinking control participants and BMI was protective against treatment dropout among binge drinkers.
Our findings support the literature describing deleterious effects of substance use on treatment adherence in suggesting that the high dropout rates and poor general treatment compliance observed within IPV-related intervention programs may be disproportionately due to offenders with comorbid alcohol use issues, even after controlling for illicit drug use (e.g., Daly & Pelowski, 2000). This is not surprising given that problematic alcohol use involves frequent, long periods of alcohol seeking, ingestion, intoxication, and resultant physiological incapacitation that interfere with the ability to fulfill obligations across domains, such as treatment attendance. With comparable precondition readiness to change scores across drinking groups, we can conclude that lower compliance among binge drinking participants was not likely the result of a lower perceived need to change violent behavior.
While the mechanisms of change involved in motivational interviewing are not fully understood (Murphy & Eckhardt, 2005), growing evidence suggests that in-session participant change talk may mediate the relationship between MI consistent therapist behaviors and prosocial behavior change among substance abusers (e.g., Miller et al., 2004; Moyers et al., 2007). Future investigations would need to analyze participant verbalizations to assess a potential mediating role of change talk among partner violent offenders. Furthermore, substance involved clients report that they perceive few prospective benefits from treatment and anticipate many obstacles to successful completion (Cunningham et al., 1993). Consistent with theory, the current BMI session may have boosted participant self-efficacy and helped to identify treatment as a beneficial and attainable option through a systematic focus on identifying client-specific reasons to become nonviolent and developing a plan to achieve that goal (Miller & Rollnick, 2002; Murphy & Eckhardt, 2005). The non-confrontational style of MI may have also reduced participant resistance prior to attending subsequent treatment, which was conceptualized as an instrument to aid in acquiring the necessary skills to prosocially cope with and resolve relationship conflict. Substance use was only discussed within the context of the participant's own goals, suggesting the possibility of indirect BMI effects across behavioral domains. These results offer support for the possibility that the beneficial effects of BMI on treatment outcomes among IPV perpetrators in general, detected across recent studies, may be largely attributable to the subset of offenders with substance use problems for whom these techniques were initially developed (e.g., Connors, Walitzer, & Dermen, 2002; Taft et al., 2001). Additional research is required to confirm these findings and to clarify the mechanisms of change that underlie the effects of BMI on treatment compliance among IPV offenders with alcohol use problems.
It is worth noting that recruitment of the current sample occurred at a probation department, which may have influenced the manner in which participants interacted with study personnel. Researchers clearly identified themselves as university affiliates with no ties to law enforcement and provided reasonable assurances of confidentiality. Further, the current sample only included offenders without active protection orders, which introduce the confound of judicial oversight that may bias treatment compliance outcomes as well as increase the likelihood of being involuntarily removed (i.e. dropout) from treatment as a consequence of contact violations despite intended treatment compliance. Substance use detected within the current sample, however, is consistent with previous research, suggesting that the results may generalize well to comparable samples (Stuart et al., 2003). The current results provide initial evidence into the effects of MI on treatment compliance among IPV offenders who misuse alcohol. Results must be replicated in subsequent, methodologically rigorous investigations utilizing multiple therapists and controlling for therapist effects, multiple coders trained to reliability on the MITI, ongoing monitoring for coding reliability, and concurrent reporting of global scores as well as behavior count data. We also see disproportionately high rates of treatment dropout among ethnic minorities and also that the effects of MI on treatment compliance differ among ethnic groups (Taft et al., 2001). Larger samples are needed to determine if the current effects generalize across ethnic groups.
The current results highlight the importance of individualized treatment planning for IPV offenders. It is clear that substance use problems complicate treatment and, therefore, may require unique engagement and specialized treatment protocols. The current results suggest that MI may be neither necessary nor particularly effective at improving treatment compliance among IPV clients without drinking problems but that MI may significantly improve outcomes among clients who binge drink. Thus, assessing drinking history through self-report, collateral informants, and court or treatment records may indicate a need for MI as one part of an individualized treatment plan that will optimize limited treatment resources to produce the greatest reductions in risk among incoming IPV offenders. The addition of motivational interviewing to treatment plans for alcohol involved IPV offenders is consistent with the nascent literature indicating improved outcomes among integrated IPV-substance use treatment programs relative to standard treatments (Easton et al., 2007).
Public Health Significance.
Findings strongly suggest that brief motivational interviewing may be a particularly effective adjunctive intervention to increase treatment compliance among partner violent men who engage in binge drinking.
This study highlights the importance of individual assessment and treatment planning to meet the highly variable needs of men seeking treatment for partner violence perpetration.
Acknowledgments
The current study was part of a larger investigation (Crane & Eckhardt, 2013). This research was supported in part by grants from NIAAA (T32-AA007583; K23-AA021768) and the Clifford B. Kinley Trust, Purdue University.
Contributor Information
Cory A. Crane, Department of Psychological Sciences, Purdue University.
Christopher I. Eckhardt, Department of Psychological Sciences, Purdue University
Robert C. Schlauch, Department of Psychology, University of South Florida
References
- Babcock J, Green C, Robie C. Does batterers' treatment work? A meta-analytic review of domestic violence treatment. Clinical Psychology Review. 2004;23:1023–1053. doi: 10.1016/j.cpr.2002.07.001. [DOI] [PubMed] [Google Scholar]
- Berman A, Bergman H, Palmstierna T, Schlyter F. Evaluation of the Drug Use Disorders Identification Test (DUDIT) in criminal justice and detoxification settings and in a Swedish population sample. European Addiction Research. 2005;11:22–31. doi: 10.1159/000081413. [DOI] [PubMed] [Google Scholar]
- Begun A, Murphy C, Bolt D, Weinstein B, Strodthoff T, Short L, Shelley G. Characteristics of the Safe at Home instrument for assessing readiness to change intimate partner violence. Research on Social Work Practice. 2003;13:80–107. [Google Scholar]
- Cadsky O, Hanson RK, Crawford M, Lalonde C. Attrition from a male batterer treatment program: Client-treatment congruence and lifestyle instability. Violence and Victims. 1996;11:51–64. [PubMed] [Google Scholar]
- Connors GJ, Walitzer KS, Dermen KH. Preparing clients for alcoholism treatment: Effects on treatment participation and outcomes. Journal of Consulting and Clinical Psychology. 2002;70:1161–1169. doi: 10.1037//0022-006x.70.5.1161. [DOI] [PubMed] [Google Scholar]
- Crane CA, Eckhardt CI. Evaluation of a single-session brief motivational enhancement intervention for partner abusive men. Journal of Counseling Psychology. 2013;60:180–187. doi: 10.1037/a0032178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham JA, Sobell LC, Sobell MB, Agrawal S, Toneatto T. Barriers to treatment: Why alcohol and drug abusers delay or never seek treatment. Addictive Behaviors. 1993;18:347–353. doi: 10.1016/0306-4603(93)90036-9. [DOI] [PubMed] [Google Scholar]
- Daly JE, Pelowski S. Predictors of dropout among men who batter: A review of studies with implications for research and practice. Violence and Victims. 2000;15:137–160. [PubMed] [Google Scholar]
- Daly JE, Power TG, Gondolf EW. Predictors of batterer program attendance. Journal of Interpersonal Violence. 2001;16(10):971–991. [Google Scholar]
- Easton C, Mandel D, Hunkele K, Nich C, Rounsaville B, Carroll K. A cognitive behavioral therapy for alcohol-dependent domestic violence offenders: An integrated Substance Abuse-Domestic Violence treatment approach (SADV) The American Journal on Addictions. 2007;16:124–31. doi: 10.1080/10550490601077809. [DOI] [PubMed] [Google Scholar]
- Eckhardt CI, Murphy CM, Whitaker DJ, Sprunger J, Dykstra R, Woodard K. The effectiveness of intervention programs for perpetrators and victims of intimate partner violence. Partner Abuse. 2013;4:196–231. [Google Scholar]
- Eckhardt C, Utschig A. Assessing readiness to change among perpetrators of intimate partner violence: Analysis of two self-report measures. Journal of Family Violence. 2007;22:319–330. [Google Scholar]
- Feder L, Wilson D. A meta-analytic review of court-mandated batterer intervention programs: Can courts affect abusers' behavior? Journal of Experimental Criminology. 2005;1:239–262. [Google Scholar]
- Gondolf EW. Characteristics of court-mandated batterers in four cities. Violence Against Women. 1999;5:1277–1293. [Google Scholar]
- Hamberger LK, Hastings JE. Counseling male spouse abusers: Characteristics of treatment completers and dropouts. Violence and Victims. 1989;4:275–286. [PubMed] [Google Scholar]
- Leonard KE. Alcohol and intimate partner violence: when can we say that heavy drinking is a contributing cause of violence? Addiction. 2005;100:422–425. doi: 10.1111/j.1360-0443.2005.00994.x. [DOI] [PubMed] [Google Scholar]
- Lundahl BW, Kunz C, Brownell C, Tollefson D, Burke BL. A meta-analysis of motivational interviewing: Twenty-five years of empirical studies. Research on Social Work Practice. 2010;20:137–160. [Google Scholar]
- Miller W, Rollnick S. Motivational interviewing: Preparing people to change addictive behavior. 2nd. New York: Guilford; 2002. [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Helping people change. 3rd. New York: Guilford Press; 2012. [Google Scholar]
- Moore TM, Stuart GL. Illicit Substance Use and Intimate Partner Violence Among Men in Batterers' Intervention. Psychology of Addictive Behaviors. 2004;18:385–389. doi: 10.1037/0893-164X.18.4.385. [DOI] [PubMed] [Google Scholar]
- Moyers TB, Martin T, Christopher PJ, Houck JM, Tonigan J, Amrhein PC. Client language as a mediator of motivational interviewing efficacy: Where is the evidence? Alcoholism: Clinical and Experimental Research. 2007;31:40–47. doi: 10.1111/j.1530-0277.2007.00492.x. [DOI] [PubMed] [Google Scholar]
- Moyers TB, Martin J, Houck JM, Christopher P, Tonigan JS. From in-session behaviors to drinking outcomes: A causal chain for motivational interviewing. Journal of Consulting and Clinical Psychology. 2009;77:1113–1124. doi: 10.1037/a0017189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moyers TB, Martin T, Manuel J, Miller W, Ernst D. The Motivational Interviewing Treatment Integrity Code: Version 3.1.1. 2010 Available on the World Wide Web at: http://casaa.unm.edu/codinginst.html.
- Murphy C, Eckhardt C. Treating the Abusive Partner: An individualized, cognitive-behavioral approach. New York: Guilford; 2005. [Google Scholar]
- Sabourin S, Valois P, Lussier Y. Development and validation of a brief version of the Dyadic Adjustment Scale with a nonparametric item analysis model. Psychological Assessment. 2005;17:15–27. doi: 10.1037/1040-3590.17.1.15. [DOI] [PubMed] [Google Scholar]
- Saunders J, Aasland O, Babor T, de la Puente J, Grant M. Development of the Alcohol Use Disorders Screening Test (AUDIT). WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Schumacher JA, Fals-Stewart W, Leonard KE. Domestic violence treatment referrals for men seeking alcohol treatment. Journal of Substance Abuse Treatment. 2003;24:279–283. doi: 10.1016/s0740-5472(03)00034-5. [DOI] [PubMed] [Google Scholar]
- Smedslund G, Dalsbo TK, Steiro A, Winsvold A, Clench-Aas J. Cognitive behavioural therapy for men who physically abuse their female partner. Cochrane database of Systematic Reviews. 2011;(2):CD006048. doi: 10.1002/14651858.CD006048.pub2. [DOI] [PubMed] [Google Scholar]
- Stuart GL, Moore TM, Kahler CW, Ramsey SE. Substance abuse and relationship violence among men court-referred to batterers' intervention programs. Substance Abuse. 2003;24:107–122. doi: 10.1080/08897070309511539. [DOI] [PubMed] [Google Scholar]
- Taft C, Murphy C, Elliott J, Morrel T. Attendance enhancing procedures in group counseling for domestic violence abusers. Journal of Counseling Psychology. 2001;48:51–60. [Google Scholar]