Abstract
Background
The Injury Severity Score (ISS) is an assessment of anatomical threat to life, but does not correlate with severity perceived by the patient. The purpose of this study was to assess how and why patients assign perceived injury severity.
Methods
One hundred twenty consecutive patients were asked “Would you say your injury is mild, moderate, severe or very severe?” and “Why do you rate your injury that way?” Explanations were categorized and compared by age, perceived injury severity, and injury mechanism. Categories were pain, injury assessment, injury description, and all others. The two age groups used were <55 and ≥55 years old. Perceived injury severity and ISS were given a 1 to 4 value, and a difference score was generated. The data were analyzed with Wilcoxon Rank-Sum, Spearman’s correlation coefficient, and Mantel-Haenszel tests.
Results
The ISS was not significantly correlated with perceived injury severity scores (r2 =0.177, p=0.0535, Spearman’s correlation), and most patients reported a higher injury severity. The difference between perceived severity and ISS was statistically significant (p<0.001, Wilcoxon Rank Sum). Patients with penetrating injuries significantly overestimated their injury severity (p=0.014, Wilcoxon Rank Sum). Patients with mild and moderate injuries gave more assessment explanations, whereas patients with severe or very severe injuries gave more description explanations (p=0.0220, Mantel-Haenszel).
Conclusions
Patients based perceived severity on their injuries, but it did not correlate with ISS, likely because ISS considers injuries graded events, while the patient considers them all or none events.
Keywords: injury severity, patient perception, quality of life
INTRODUCTION
The care of trauma patients has advanced greatly over the last 100 years. Warfare brought many achievements to our modern trauma system. The importance of timely care led to strategically placed hospitals and quicker transport. Anesthesia and antibiotics were discovered, surgical wound repair was advanced, and communication systems progressed. These innovations improved outcomes and saved lives that were previously lost (13-15).
Even with the remarkable strides made in trauma care, survivors do not always recover as expected. Trauma patients still suffer some physical and psychological disabilities from 6 months to 5 years post-injury (2, 4, 6-8, 10-12, 20, 22, 23). What factors determine recovery and whether a patient’s recovery trajectory can be predicted are current areas of active research.
The Injury Severity Score (ISS) is a numerical summary of the trauma patient’s anatomical injuries and acute threat to life. It was designed to predict mortality from trauma and to evaluate the quality of emergency care provided (9). The literature provides conflicting views on the relationship of the ISS to Health Related Quality of Life (HRQoL) and recovery (1, 6, 10, 12). Recent evidence suggests that it is the patient’s perceived injury severity, rather than the ISS, that is related to post-injury HRQoL (1). Interestingly, ISS is not related to patient’s perceived injury severity. To our knowledge, no previous study has explored the reasons behind why patients perceive how severely they are injured.
Elderly patients have poorer outcomes after injury when compared to younger patients. This is in part due to the presence of comorbidities and less physiological reserve, unlike younger patients (17-19, 21). In addition, studies suggest that elderly patients do not experience pain like younger patients, with the elderly having impaired pain perception and reporting less acute pain (3, 5, 16). Perceived injury severity may be influenced by the perception of pain as well as the presence of comorbid diseases.
The purpose of our study was to: 1) explore the relationship between the ISS and the patient’s perceived injury severity score; 2) to investigate how patients assign their injury severity score; 3) to determine if older patients perceive injury differently compared to younger patients; and 4) to explore any differences in perceived injury severity with mechanism of injury. We hypothesized that patients ≥ 55 years-old would underestimate the severity of their injury, and all other aims were exploratory.
PARTICIPANTS AND METHODS
One hundred twenty consecutive trauma patients admitted to a Level I trauma center participated. Patients were excluded if they were in the ICU, non-English speaking, had symptoms of a traumatic brain injury, <18 years-old, or had a history of belligerent behavior towards other hospital staff.
Consent was obtained and patients were asked “Would you say your injury is mild, moderate, severe, or very severe?” and “Why do you rate your injury that way?” Perceived injury severity was reported as 1-4, where 1=mild, 2=moderate, 3=severe, and 4=very severe. The ISS, mechanism of injury, age, and sex were abstracted from the trauma registry. An ISS of <9 defined a mild injury, ISS of 9-15 a moderate injury, 16-25 a severe injury, and an ISS of >25 a very severe injury (1). The ISS was then converted to a 1-4 scale.
Based on grounded theory analysis, explanations for the perceived injury severity rating were examined for the theme of a participant’s statement, and then placed into one of seven categories that were determined after analysis of the first week of responses: pain (degree), assessment of injury (present or possible implications of injury according to the patient), description of injury (statement of the specific physical injury by the patient), impact on future, emotional reactions, medical care needed, and unsure.
This study was approved by the Institutional Review Board at the Medical College of Wisconsin.
Statistical Analysis
Data were analyzed using SAS version 9.2 (The SAS Institute, Cary, NC) and SPSS (Version 19, SPSS, Chicago, IL). Frequency counts and descriptive statistics were used to report demographics, injury characteristics, and explanations of perceived severity ratings. The ISS for each patient was subtracted from their perceived injury severity, which led to values between -3 and +3. This difference in severity was then analyzed using the Wilcoxon Rank-Sum test. The association between perceived injury severity and ISS was analyzed using Spearman’s correlation coefficient. The Wilcoxon Rank-Sum test was used to test the dependence of perceived severity on age and mechanism of injury. The Exact Pearson test was used to test the dependence of the categorical explanations on age and mechanism of injury. The Mantel Haenszel test was used to compare categories of explanations with perceived injury severity.
RESULTS
One hundred twenty consecutive trauma patients completed the questionnaire during the three-month study period, a response rate of 85%. Seventy-three percent of the 120 patients were male. The mean age for patients <55 (n=81) was 35.3 ± 10.6 years, and the mean age for patients ≥55 (n=39) was 68.8 ± 11.3 years [t (df) = 70.6, p=0.000]. Seventy percent of the patients described themselves as Caucasian, 22.5% as African American and 5.8% as Hispanic. 84.2% of the injuries were blunt and 15.8% were penetrating.
The most common mechanisms of injury in both age groups were motor vehicle crashes, falls, and motorcycle crashes (table 1). “Accident” included industrial injuries and a water-ski injury. Gun shot wounds and stab wounds were found only in patients less than 55 years old. Bicycle crashes and motor vehicle vs. pedestrian crashes were more prevalent in patients aged 55 and older.
Table 1.
Frequency and Percent of Mechanism of Injury for all Participants
| ≤55 (n=81) | ≥55 (n=39) | |
|---|---|---|
|
| ||
| Mechanism of Injury | n (%)* | n (%)* |
| Accident | 2 (2) | 2 (5) |
| Animal | 0 (0) | 1 (3) |
| Assault | 2 (2) | 0 (0) |
| Bicycle | 3 (4) | 3 (8) |
| Crush | 2 (2) | 0 (0) |
| Fall | 11 (14) | 13 (33) |
| GSW | 10 (12) | 0 (0) |
| MCC | 19 (23) | 5 (13) |
| Moped | 0 (0) | 1 (3) |
| MPC | 2 (2) | 2 (5) |
| MVC | 21 (26) | 12 (31) |
| SW | 9 (11) | 0 (0) |
Note.
= As percent of age group.
Perceived Injury Severity and ISS
The mean ISS was 10.7 ± 6.3 for patients under 55 years old and 11.7 ± 1.2 for patients aged 55 and older [t (df) =79.6, p=0.398]. Thirty percent of all patients had a mild ISS, 45% had a moderate ISS, 23% had a severe ISS, and 3% had a very severe ISS. Eleven percent of all participants reported a mild perceived injury severity score, 22% reported moderate, 47% reported severe, and 21% reported a very severe perceived injury severity score (figure 1).
Figure 1.
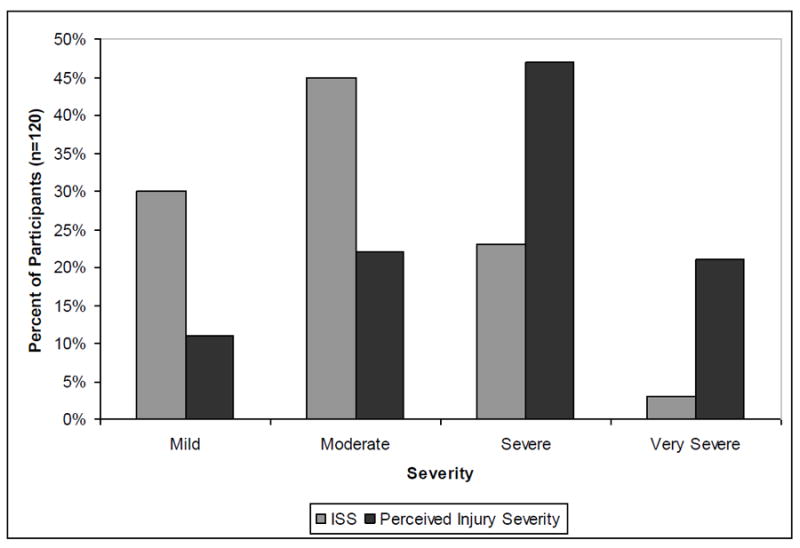
Percent of Participants per Perceived Injury Severity Score and ISS Severity Level.
Shows percent of patients (n=120) that had an ISS of mild, moderate, severe, or very severe, as compared to the percent of patients reporting a severity in one of those four levels.
In patients less than 55, 13.6% reported a mild injury, 19.8% reported moderate, 46.9% reported severe, and 19.8% reported a very severe injury. In patients ≥55, 5.1% reported a mild injury, 25.6% reported a moderate injury, 43.6% reported a severe injury, and 25.6% reported a very severe injury. There was not a significant difference in perceived injury severity for patients <55 versus participants ≥55 years old [Wilcoxon Rank-Sum (df) = 1, p=0.7856]. Frequency statistics show that patients <55 reported severe injuries most often, whereas patients ≥55 reported severe most often, but had more moderate and very severe perceived injury severities, as well as fewer mild perceived injury ratings (figure 2).
Figure 2.
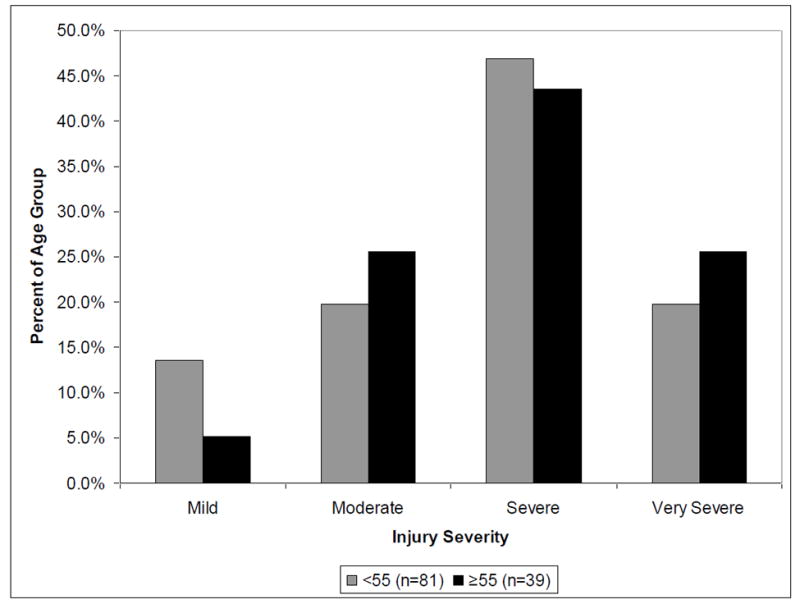
Percent of Perceived Injury Severity Scores per Age Group (<55 and ≥55 years old).
Percent of patients per each age group that reported a perceived injury severity rating of that degree (mild, moderate, severe, and very severe).
Sixty-eight percent of patients reported an injury severity greater than the ISS, 20.8% of all patients reported a perceived injury severity equal to the ISS, and 11.7% reported an injury severity less than their ISS. There was a significant difference between the perceived injury severity and the ISS (Wilcoxon Rank-Sum, p<0.001). Furthermore, there was not a significant correlation between ISS and perceived severity [Spearman’s correlation coefficient (df) = 6, r2=0.17670, p=0.0535]. Patients with penetrating injuries were more likely to overestimate their injury severity [Wilcoxon Rank-Sum (df) = 1, p=0.0139, table 2].
Table 2. Frequency and Percent of Blunt and Penetrating Injuries by Perceived Injury Severity Score.
Comparison of reported perceived injury severity scores by mechanism of injury (blunt or penetrating).
| Blunt (n=101) | Penetrating (n=19) | |
|---|---|---|
|
| ||
| Perceived Injury Severity | n (%)* | n (%)* |
| Mild | 12 (11.9) | 1 (5.3) |
| Moderate | 23 (22.8) | 3 (15.8) |
| Severe | 47 (46.5) | 9 (47.4) |
| Very Severe | 19 (18.8) | 6 (31.6) |
Note.
= As a percent of mechanism of injury group.
Penetrating injury patients significantly overestimated their injury severity (p=0.0139, Wilcoxon Rank-Sum).
Explanations for Perceived Injury Severity
Patients’ explanations fit into seven categories. The first category was pain, which was based on the degree of pain patients felt. The second category was assessment of injury, which encompassed interpretations of the injury severity or consequences the traumatic event could have had on their mortality in the acute setting (i.e. “Because it could have been life threatening,” or “Because I can’t walk.”). The third category was description of injury, which included answers in which patients restated their injuries as they understood them (i.e. “I have 6 broken ribs and a punctured lung.”). The last four categories were emotional reactions to the injury, medical care needed (amount, or of a quality that was extensive or invasive), future implications because of the injury, and unsure.
All patients had the same basic trend for their explanations, in that assessment and description reasons were most frequently cited. Patients <55 responded with assessment of injury responses (40%), then description responses (28%), all others category responses (19%), and pain responses least often (14%). Patients ≥55 gave slightly more description responses (36%), then assessment responses (33%), pain responses (23%), and all others explanations least often (8%). Category explanations did not differ significantly by age [Exact Pearson (df) = 3, p= 0.2377, table 3].
Table 3. Frequency and Percent of Explanations Given for Perceived Injury Severity Score by Age Group.
Shows the count and percent of patients in each age group that respond with answers in each of the four explanation categories.
| <55 (n=81) | ≥55 (n=39) | |
|---|---|---|
|
| ||
| Categories | n (%)* | n (%)* |
| Pain | 11 (14) | 9 (23) |
| Assessment | 32 (40) | 13 (33) |
| Description | 23 (28) | 14 (36) |
| All Others | 15 (19) | 3 (8) |
Note.
= Percent of patients per age group.
Patients with mild injuries most often gave assessment explanations, 62%. Moderate injuries were also most represented in the assessment category (69%). Patients with severe injuries more often gave a description of injury explanation, 43%. Very severe injuries followed severe injuries, having description of injury as the most often explanation (46%). Of all patients with mild injuries, none gave description explanations for their perceived injury severity ratings (Mantel-Haenszel, p=0.0220, figure 3).
Figure 3.
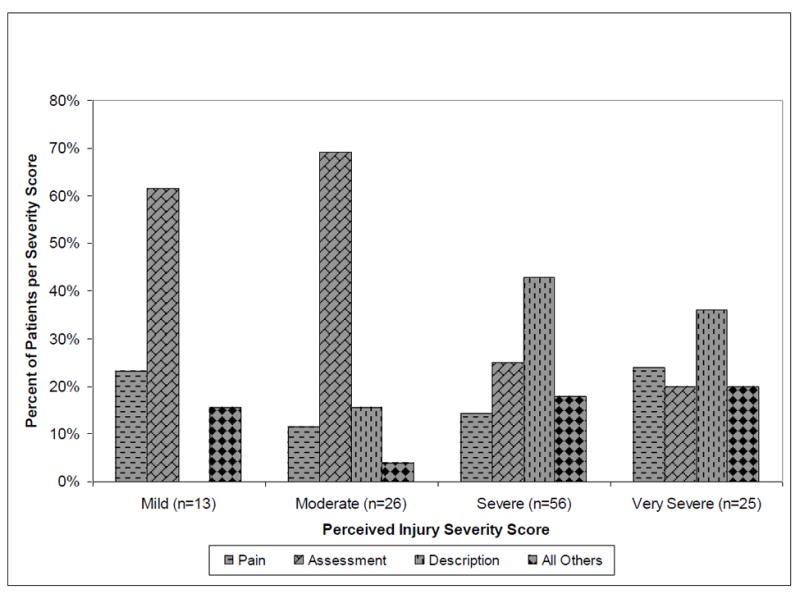
Percent of Patients Responding with Pain, Assessment of Injury, Description of Injury, or Other Explanations per Perceived Injury Severity Score.
Compares the percent of explanations given between the four perceived injury severity scores. Assessment of injury explanations were most frequent in mild and moderate perceived injury scores, while description of injury explanations were most frequent in severe and very severe perceived injury scores, a significant difference (Mantel-Haenszel, p=0.0220).
Participants that underestimated injury severity most frequently reported pain explanations (35.7%) and assessment responses (50%). Patients with a perceived injury severity score equal to the ISS reported assessment explanations most often (40%), with description reasons close behind (36%). Participants that overestimated their injury severity reported assessment (34.6%) and description (32.1%) explanations most frequently; they also reported the majority of explanations in the all others category (table 4).
Table 4. Frequency and Percent of Underestimates, Accurate Estimates, and Overestimates per Explanation Category.
Compares categories of explanations to the difference between the perceived injury severity score and the ISS
| Underestimate | Same estimate | Overestimate | |
|---|---|---|---|
|
| |||
| Explanation Category | n (%)* | n (%)* | n (%)* |
| Pain | 5 (35.7) | 3 (12.0) | 12 (14.8) |
| Assessment | 7 (50.0) | 10 (40.0) | 28 (34.6) |
| Description | 2 (14.3) | 9 (36.0) | 26 (32.1) |
| All Others | 0 (0) | 3 (12.0) | 15 (18.5) |
Note.
= As percent of patients per estimation difference (perceived injury severity score – ISS).
perceived injury severity – ISS on a 1-4 scale, where 1=mild and 4=very severe.
Pain was reported most frequently in bicycle crashes (33.3%), falls (30.4%) and gun shot wounds (30.0%). Assessment explanations were reported most frequently in motorcycle crashes (58.3%), stab wounds (55.6%), all others (40.0%), and falls (30.4%). Description explanations were reported most frequently in gun shot wounds (50.0%), motor vehicle crashes (42.4%), all others (33.3%), and falls (26.1%). Category responses were not statistically significant in their associations with mechanism of injury [Exact Pearson (df) = 3, p=0.7923, table 5].
Table 5. Frequency and Percent of Explanation Categories Reported by Mechanism of Injury.
Categories of explanations for perceived injury severity score by mechanism of injury.
| Pain | Assessment | Description | All Others | |
|---|---|---|---|---|
|
| ||||
| Injury Mechanism | n (%)* | n (%)* | n (%)* | n (%)* |
| Bicycle | 2 (33) | 1 (17) | 1 (17) | 2 (33) |
| Fall | 7 (30) | 7 (30) | 6 (26) | 3 (13) |
| GSW | 3 (30) | 1 (10) | 5 (50) | 1 (10) |
| MCC | 2 (8) | 14 (58) | 4 (17) | 4 (17) |
| MVC | 4 (12) | 11 (33) | 14 (42) | 4 (12) |
| SW | 1 (11) | 5 (56) | 2 (22) | 1 (11) |
| All Others | 1 (7) | 6 (40) | 5 (33) | 3 (20) |
Note.
= As percent of Mechanism of Injury Group.
CONCLUSIONS
ISS was shown by multiple statistical methods to lack correlation with perceived injury severity scores reported by the patient, supporting our previous work (1). Results confirmed that patients most often overestimated the severity of their injury, which was statistically significant for patients with penetrating injuries.
Patients based their perceived injury severity on assessments of their injury, descriptions of their injury, or the amount of pain they were in because of their injury. Assessment responses were reported more often with mild and moderate injuries. Patients with severe and very severe injuries gave description explanations most often. The explanations for the perceived severity scores did not differ significantly by age or mechanism of injury. Despite the fact that participants based severity on descriptions of their injury, perceived severity lacked correlation with the ISS, which is also based on injury description. This may be due to the fact that the ISS encompasses categories of severity within each body region, while the patients related their perception as a binary event (injury present or absent).
When comparing the difference between perceived injury severity and the ISS, assessment and description explanations were the most frequent responses. It is surprising that patients who underestimated their injury reported pain explanations more frequently than accurate estimators and over-estimators. Under-estimators also reported more assessment explanations, which is likely because many of these responses were “Because it [their injury] was not life threatening.”
One limitation of our study was sample size. However, we did not come up with new explanation categories after establishing the initial categories using a modification of grounded theory, suggesting saturation. Nonetheless, a larger sample size would allow more quantitative analysis of these qualitative responses.
Another limitation was the variability of the time of patient interview. Surgical procedures, narcotics, day of admission (weekend or weekday), cognitive status, and patient preference were all factors in how quickly the patient could be interviewed. Time can have an effect on how aware patients are of their injury and change their perceived injury severity over time. However, we tried to approach the patients as close to admission as possible.
Many patients with traumatic injuries still experience a variety of disabilities months and years after the initial injury. Pain, mobility issues, and psychological issues such as anxiety and depression are commonly found complaints (2, 4, 7, 8, 10, 20). The results of this study are an important step in understanding traumatic injury from the patient’s perspective, but more work needs to be done on this subject.
Acknowledgments
The statistical analysis was performed by Jessica Pruszynski, PhD and Dan Eastwood, MS of the Medical College of Wisconsin’s Biostatistics Consulting Service. This service is supported by funds from the Institute for Health and Society, Division of Biostatistics, and by grant 1UL1RR031973 from the Clinical and Translational Science Award (CTSA) program of the National Center for Research Resources, National Institutes of Health.
Thank you to Linda Meurer, MD, MPH and the National Institute on Aging (NIA) T35 Research Training Grant Summer 2010. Thank you to Bonnie Krajcik, Trauma Registrar, Colleen Trevino, RN ACNP, and Edmund Duthie, MD.
Contributor Information
Angie A. Geiger, Email: ageiger@mcw.edu.
Dr. Karen J. Brasel, Email: kbrasel@mcw.edu.
Dr. Terri deRoon-Cassini, Email: tcassini@mcw.edu.
References
- 1.Brasel KJ, deRoon-Cassini T, Bradley CT. Injury Severity and Quality of Life: Whose Perspective is Important? J Trauma. 2010;68:263–268. doi: 10.1097/TA.0b013e3181caa58f. [DOI] [PubMed] [Google Scholar]
- 2.Ponsford J, Hill B, Karamitsios M, Bahar-Fuchs A. Factors Influencing Outcome After Orthopedic Trauma. J Trauma. 2008;64:1001–1009. doi: 10.1097/TA.0b013e31809fec16. [DOI] [PubMed] [Google Scholar]
- 3.Gagliese L. Pain and Aging: The Emergence of a New Subfield of Pain Research. J Pain. 2009;10:343–353. doi: 10.1016/j.jpain.2008.10.013. [DOI] [PubMed] [Google Scholar]
- 4.Lee BO, Chaboyer W, Wallis M. Predictors of Health-Related Quality of Life 3 Months After Traumatic Injury. J Nurs Scholarsh. 2008;40:83–90. doi: 10.1111/j.1547-5069.2008.00210.x. [DOI] [PubMed] [Google Scholar]
- 5.Li SF, Greenwald PW, Gennis P, Bijur PE, Gallagher EJ. Effect of Age on Acute Pain Perception of a Standardized Stimulus in the Emergency Department. Ann Emerg Med. 2001;38:644–647. doi: 10.1067/mem.2001.119849. [DOI] [PubMed] [Google Scholar]
- 6.Halcomb E, Daly J, Davidson P, Elliott D, Griffiths R. Life Beyond Severe Traumatic Injury: An Integrative Review of the Literature. Aust Crit Care. 2005;18:17–24. doi: 10.1016/s1036-7314(05)80020-7. [DOI] [PubMed] [Google Scholar]
- 7.Lundgaard Soberg H, Bautz-Holter E, Roise O, Finset A. Long-Term Multidimensional Functional Consequences of Severe Multiple Injuries Two Years After Trauma: A Prospective Longitudinal Cohort Study. J Trauma. 2007;62:461–470. doi: 10.1097/01.ta.0000222916.30253.ea. [DOI] [PubMed] [Google Scholar]
- 8.Kiely JM, Brasel KJ, Weidner KL, Guse CE, Weigelt JA. Predicting Quality of Life Six Months After Traumatic Injury. J Trauma. 2006;61:791–798. doi: 10.1097/01.ta.0000239360.29852.1d. [DOI] [PubMed] [Google Scholar]
- 9.Baker SP, O’Neill B, Haddon W, Jr, Long WB. The Injury Severity Score: A Method for Describing Patients with Multiple Injuries and Evaluating Emergency Care. J Trauma. 1974;14:187–196. [PubMed] [Google Scholar]
- 10.Sluys K, Häggmark T, Iselius L. Outcome and Quality of Life 5 Years After Major Trauma. J Trauma. 2005;59:223–232. doi: 10.1097/01.ta.0000173832.01547.cb. [DOI] [PubMed] [Google Scholar]
- 11.Lee BO, Chaboyer W, Wallis M. Illness Representations in Patients with Traumatic Injury: A Longitudinal Study. J Clin Nurs. 2010;19:556–563. doi: 10.1111/j.1365-2702.2009.02972.x. [DOI] [PubMed] [Google Scholar]
- 12.Dimopoulou I, Anthi A, Mastora Z, Theodorakopoulou M, Konstandinidis A, Evangelou E, Mandragos K, Roussos C. Health-Related Quality of Life and Disability in Survivors of Multiple Trauma One Year After Intensive Care Unit Discharge. Am J Phys Med Rehabil. 2004;83:171–176. doi: 10.1097/01.phm.0000107497.77487.c1. [DOI] [PubMed] [Google Scholar]
- 13.Trunkey DD. History and Development of Trauma Care in the United States. Clin Orthop Relat Res. 2000;374:36–46. doi: 10.1097/00003086-200005000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Hoff WS, Schwab CW. Trauma System Development in North America. Clin Orthop Relat Res. 2004;422:17–22. doi: 10.1097/01.blo.0000128292.43913.83. [DOI] [PubMed] [Google Scholar]
- 15.Dutton RP, Stansbury LG, Leone S, Kramer E, Hess JR, Scalea TM. Trauma Mortality in Mature Trauma Systems: Are We Doing Better? An Analysis of Trauma Mortality Patterns, 1997-2008. J Trauma. 2009;69:620–626. doi: 10.1097/TA.0b013e3181bbfe2a. [DOI] [PubMed] [Google Scholar]
- 16.Moore AR, Clinch D. Underlying Mechanisms of Impaired Visceral Pain Perception in Older People. J Am Geriatr Soc. 2004;52:132–136. doi: 10.1111/j.1532-5415.2004.52023.x. [DOI] [PubMed] [Google Scholar]
- 17.Kaarlola A, Tallgren M, Pettilä V. Long-Term Survival, Quality of Life, and Quality-Adjusted Life-Years Among Critically Ill Elderly Patients. Crit Care Med. 2006;34:2120–2126. doi: 10.1097/01.CCM.0000227656.31911.2E. [DOI] [PubMed] [Google Scholar]
- 18.Richmond TS, Kauder D, Strumpf N, Meredith T. Characteristics and Outcomes of Serious Traumatic Injury in Older Adults. J Am Geriatr Soc. 2002;50:215–222. doi: 10.1046/j.1532-5415.2002.50051.x. [DOI] [PubMed] [Google Scholar]
- 19.Cullinane DC, Morris JA. The Impact of Age and Medical Comorbidities on the Outcome Following Severe Trauma. J Intensive Care Med. 1999;14:86–94. [Google Scholar]
- 20.Ringdal M, Plos K, Lundberg D, Johansson L, Bergbom I. Outcome After Injury: Memories, Health-Related Quality of Life, Anxiety, and Symptoms of Depression After Intensive Care. J Trauma. 2009;66:1226–1233. doi: 10.1097/TA.0b013e318181b8e3. [DOI] [PubMed] [Google Scholar]
- 21.Jacobs DG. Special Considerations in Geriatric Injury. Curr Opin Crit Care. 2003;9:535–539. doi: 10.1097/00075198-200312000-00012. [DOI] [PubMed] [Google Scholar]
- 22.Read KM, Kufera JA, Dischinger PC, Kerns TJ, Ho SM, Burgess AR, Burch CA. Life-Altering Outcomes after Lower Extremity Injury Sustained in Motor Vehicle Crashes. J Trauma. 2004;57:815–823. doi: 10.1097/01.ta.0000136289.15303.44. [DOI] [PubMed] [Google Scholar]
- 23.O’Donnell ML, Creamer M, Elliott P, Atkin C, Kossmann T. Determinants of Quality of Life and Role-Related Disability After Injury: Impact of Acute Psychological Responses. J Trauma. 2005;59:1328–1335. doi: 10.1097/01.ta.0000197621.94561.4e. [DOI] [PubMed] [Google Scholar]


