Abstract
Objectives
Diagnosis and clinical presentation of pediatric laryngopharyngeal reflux (LPR) is still controversial. The aims of this work were to study the possibility of performing 24-hour oropharyngeal pH monitoring for children in the outpatient clinic setup and to explore the results of this test in correlation to airway-related problems.
Methods
In this descriptive qualitative study, 26 children suffering from airway-related problems were included. Oropharyngeal 24-hour pH monitoring was performed for all subjects in the outpatient clinic setting. The distribution of airway diagnoses among the study group was studied versus the results of the pH monitoring.
Results
There were 16 males and 10 females participated in the study with a mean age of 6.88 (SD, ±5.77) years. Thirty-five percent of the patients were under the age of 3 years (range, 11 months to 3 years). Eight-five percent of the patients tolerated the pH probe insertion and completed 24-hour of pH recording. Laryngomalacia and subglottic stenosis (SGS) were more frequently reported in the positive LPR patients (77%).
Conclusion
Oropharyngeal 24-hour pH monitoring can be conducted for children in the outpatient setup even in young age children below 3 years old. Among the positive LPR group, SGS and laryngomalacia were the most commonly reported airway findings.
Keywords: Laryngopharyngeal Reflux, Airway Obstruction, Pediatrics
INTRODUCTION
Pediatric laryngopharyngeal reflux (LPR) is a common pediatric disorder that has gained increasing recognition over the past few years. Laryngeal tissue irritation and laryngeal symptoms occur when the gastric contents go up beyond the upper esophageal sphincter into the oropharynx inducing LPR disease [1]. Many otolaryngological conditions have been reported to be associated with LPR [2,3]. However, a cause-effect relationship is yet to be proved [1].
Chronic LPR may be associated with some complications especially in the pediatric population. Pediatric LPR is thought to be related to many respiratory and airway-related problems including refractory asthma, recurrent bronchitis, laryngomalacia, and subglottic stenosis [4].
Subglottic stenosis is the most studied reflux-related airway problem and it is generally believed that LPR is one of the causative factors of this condition. However, those studies are based on animal models that weaken the evidence that links those two pediatric conditions together [5-7].
There is a lot of controversy related to the proper diagnosis of LPR. Up till now, there is no ideal test that can be considered for LPR detection. Many methods are used in both adults and children for LPR diagnosis including pH monitoring, upper gastro-intestinal endoscopy, esophageal manometry, esophageal biopsy, and intramural impedance. However, the results of these tests are not reproducible in patients with pediatric LPR. Dual probe 24-hour pH monitoring is thought for many years to be the gold standard test for diagnosing LPR. It is, however, an invasive test of low sensitivity, with an incidence of false-negative results reaching as high as 50% [8-11].
The Dx-pH measurement system (Dx-pH, Respiratory Technology Corp., San Diego, CA, USA) is a minimally invasive and relatively new device that has been reported to be sensitive in detection of acidic reflux events in the posterior oropharynx [12]. The device uses a thin transnasal catheter (probe) that ends with a pH sensor capable of detection both liquid and aerosolized form of acid. The probe can be easily introduced in the nose and attached to a wireless transmitter at its external end. The tip of the probe has the shape of a tear drop with a flashing red light that helps in determining the proper placement of the catheter in the oropharynx and contains the pH sensor [12].
In the few studies that included oropharyngeal pH monitoring in children, insertion of the probe was performed under general anesthesia [13]. The aims of this study were to explore the possibility of conducting and inserting oropharyngeal pH probe for children in the outpatient clinic setup and to explore the results of this test in correlation to common airway-related diagnoses in this age group.
MATERIALS AND METHODS
This is a descriptive qualitative study that has been approved by the Institutional Review Board at College of Medicine, King Saud University. Informed consent was obtained from the parents of all subjects participated in the study. All patients included in this study were referred from the pediatric airway clinic for LPR assessment and 24-hour pH monitoring. Male and female children having airway-related problems were included in the study while those with chronic nasal obstruction, nasogastric tube feeding, or on acid suppression therapy were excluded. Patients underwent clinical evaluation at the reflux clinic including history taking, laryngoscopic examination, and 24-hour oropharyngeal pH monitoring.
KayPentax video laryngeal stroboscopic system (Model 9200C, KayPentax, Montvale, NJ, USA) was used for laryngoscopic examination. The procedure was described in detailed for the parents and if possible for the children. Laryngoscopic examination was conducted using either rigid or flexible fiber-optic nasolaryngoscopy according to the patients’ tolerability. All examinations were recorded and reviewed to the children and their parents.
The diagnosis of LPR in the study groups was carried out using 24-hour oropharyngeal Dx-pH probe system (Respiratory Technology Corp.). The procedure was described in details for the parents and the child if possible. Before the procedure, calibration process according to manufacturer’s instructions was conducted to ensure accurate pH reading. In some patients, especially older and agitated children, nasal decongestant drops along with local anesthetic spray (xylometazoline hydrochloride, 0.05%, with lidocaine hydrochloride, 1%) were applied to the patients’ nostrils either before probe insertion or before fiber-optic nasolaryngoscopy if needed. The probe was then inserted through patient’s nose and advanced slowly to its destination in the back of the oropharynx. The place of the probe in the oropharynx was verified by observing the flashing light at the tip of the probe. The probe with the attached transmitter was then secured to the patient’s face and the transmitter was fixed to the patient’s clothes. In some cases of hyperactive children, and to ensure that the child will not pull the probe out, fingers’ splints were fixed to the child’s hands and fingers. The parents were then given the recording device and were instructed to keep it close to their child (within 5-m distance). During the 24-hour examination the children were encouraged to live a normal everyday life and eat normally. Parents were instructed to press a button on the monitor to indicate the feeding and sleeping periods. Fig. 1 shows one of the patients of the study having the oropharyngeal pH probe in place.
Fig. 1.

One of the patients of the study (11 months old) having the oropharyngeal pH probe in place.
The parents were instructed to keep the device away from water and they were given a diary to record the meal times and recumbent position times. The parents were instructed to write down the time precisely during the 24 hours of recording depending on the digital clock that appears on the recording device display. Following the 24 hours of recording, recorded data was downloaded to software that is provided with the device for data analysis. Thresholds for the detection of acidic reflux were set for 5.5 for the upright position and 5.0 for the supine position. The system automatically generates the Ryan score, which is a composite score, that was calculated based on the given pH thresholds of upright and supine positions. The score incorporates 3 main parameters including number of reflux episodes, duration of longest reflux episode, and percentage of time below the predetermined pH threshold. Scores greater than 9.41 in the upright position and/or 6.80 in the supine position were considered suggestive of LPR. Because no normal values exist for this age group, the adult criteria for diagnosing positive LPR were adopted in this study [12]. Comparative graphs of positive and normal studies are shown in Fig. 2.
Fig. 2.
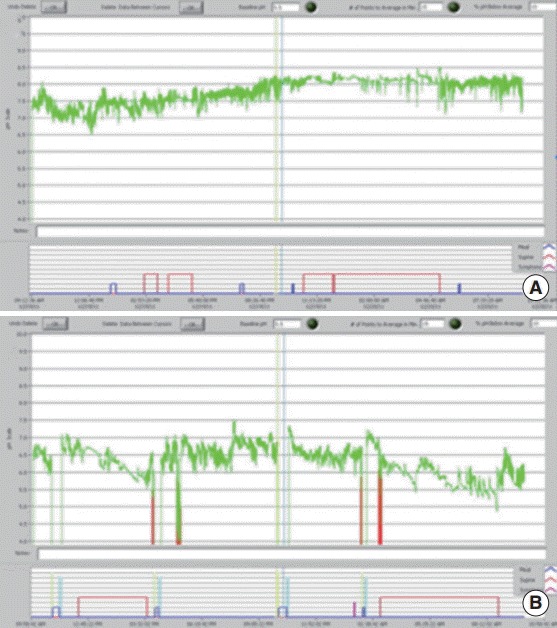
An oropharyngeal pH graph showing of a negative laryngopharyngeal reflux (LPR) study (A), and an oropharyngeal pH graph showing of a positive LPR study (B).
RESULTS
The study initially included 26 children. However, 4 children (15%) did not complete the 24-hour recording duration either because of pulling out the probe or displacement of the probe from its proper position. Three children were able to pull the probe out while there was 1 case where the probe was displaced up in the nasopharynx. On the other hand, 22 children (85%) completed the 24-hour duration of recording and had the probe in place. The mean age of the study group was 6.88 years (SD, ±5.77) including, 16 males and 10 females. Thirty-five percent of the patients were under the age of 3 years (11 months to 3 years). Table 1 shows demographic data and distribution of clinical presentation among the study group.
Table 1.
Demographic data of the study group (n=26)
| Demographic | No. (%) |
|---|---|
| Age (yr) | |
| ≤3 | 9 (34.6) |
| 4-7 | 6 (23.1) |
| 8-11 | 3 (11.5) |
| 12-16 | 8 (30.8) |
| Sex | |
| Male | 16 (61.5) |
| Female | 10 (38.5) |
| Clinical presentations | |
| Chronic cough | 20 (76.9) |
| Dysphonia | 13 (50.0) |
| Stridor | 15 (57.7) |
| Dyspnea | 18 (69.2) |
| Initial airway diagnosis | |
| Subglottic stenosis | 10 (38.5) |
| Bilateral vocal folds paralysis | 5 (19.2) |
| Laryngomalacia | 6 (23.1) |
| Laryngeal web | 5 (19.2) |
All children included in the study were referred from the pediatric airway clinic with different airway problems including bilateral vocal folds paralysis, laryngomalacia, subglottic stenosis, or laryngeal web. Table 2 shows the distribution of airway-related diagnoses among patients who successfully completed 24-hour of pH recording having the probe in place (total number, 22 patients). Based on the results of the oropharyngeal pH study, out of the 22 patients with successful probe insertion, there were 10 children (45.5%) with positive laryngopharyngeal reflux diagnosis while 12 children (54.5%) had negative results. Seventy-five percent of the patient diagnosed with subglottic stenosis had positive LPR diagnosis while 60% of the patients with laryngomalacia and 20% of the patients with bilateral vocal folds paralysis had positive LPR diagnosis.
Table 2.
Distribution of the airway diagnosis, and LPR diagnosis among the study group with successful pH probe insertion (n=22)
| Diagnosis | No. of children | Positive LPR | Negative LPR |
|---|---|---|---|
| Subglottic stenosis | 8 | 6 (75) | 2 (25) |
| Bilateral vocal folds paralysis | 5 | 1 (20) | 4 (80) |
| Laryngomalacia | 5 | 3 (60) | 2 (40) |
| Laryngeal web | 4 | 0 | 4 (100) |
| Total | 22 | 10 | 12 |
Values are presented as number (%).
LPR, laryngopharyngeal reflux.
Subglottic stenosis and laryngomalacia were the most common airway presentations in the positive LPR group. Patients were referred to the reflux clinic as part of preoperative assessment to rule-out LPR or to control it before surgery especially in cases of subglottic stenosis, bilateral vocal folds paralysis, and laryngeal web while in cases of laryngomalacia, the main reason of referral was to rule-out LPR as an etiological factor. The anticipated airway surgeries included airway reconstruction as cricotracheal resection for subglottic stenosis, partial arytenoidectomy in bilateral vocal folds paralysis, and glottis web excision. In cases of subglottic stenosis, based on Myer-Cotton classification [14]. the grade of stenosis ranged from II–III. On the other hand, children presented with laryngomalacia were between the ages of 1–2.5 years old and the severity of laryngomalacia ranged from mild to moderate based on the clinical presentation. Unfortunately, there was no sleep study conducted for patients in this study to document obstructive sleep apnea and its degree. There was no multiple airway anomalies or major comorbidity reported in the study group. Fifteen patients (68%) were tracheostomized because of their airway problems. Among those tracheostomized patients there were 8 patients (36%) with subglottic stenosis, 5 patients (23%) with bilateral vocal folds paralysis, and 2 patients (9%) with glottis web. Most of the children had reflux related symptoms including chronic cough, dysphonia, and asthmatic attacks. There were other presentations related to primary airway problems including stridor and dyspnea.
DISCUSSION
Although LPR is a common problem in pediatric population, there is much controversy still surrounds pediatric LPR. The diagnostic criteria of defining LPR in pediatrics have not been yet identified. Some investigators consider the occurrence of any pharyngeal reflux episodes is enough for diagnosing positive LPR [11,15,16]. Others consider the total amount of acid exposure time expressed as percentage of time below the baseline pH of the 24-hour period as a suitable diagnostic criterion [17].
Although widely used, double probe 24-hour pH monitoring does have limitations. For example, the probe does not detect nonacidic or gaseous reflux. Furthermore, having double probe is considered to some-extent an invasive technique, and not well tolerated by children. Especially it was proved that almost 50% of LPR patients had normal esophageal acidification [18]. In this study, a less invasive technique for pH monitoring (oropharyngeal pH-Dx system) has been used to assess the oropharyngeal pH with a single probe that is capable of detecting even the gaseous acidic reflux. Few studies have used this new technique in children for diagnosis of LPR. Some of them described the technique of probe insertion that was under general anesthesia because of difficulty of insertion of the probe while the child is awake [13,19]. In this study, the pH probe has been inserted for all children in the outpatient clinic using the technique described in the methodology above. Despite few cases in which there was some resistance in probe insertion associated with mild epistaxis, most of children in this study (85%) tolerated the probe well with few incidents of probe pull out and displacement (15%). The main age group of patients included in this study was under the age of 3 years (35%). These results confirm the possibility of performing this kind of procedure in the outpatient setup for young age children with no reported major complications.
Because of the lack of normative data for LPR in pediatric population, the adult criteria for diagnosis of LPR was adopted in this study as described in the methodology section. All patients in this study were suffering from airway-related problems including laryngomalacia, subglottic stenosis, bilateral vocal folds paralysis, and laryngeal web. Most of those children have been referred to the reflux clinic to rule-out LPR before airway reconstructive surgery. It has been reported that there is a significant association between LPR and wound healing in airway reconstruction surgery [20]. Also, it was found that there is a significant association between LPR and laryngomalacia [21,22]. A recent meta-analysis showed that 65% of patients with severe laryngomalacia had reflux [23]. Also, it has been reported that one-third to two-thirds of children diagnosed with subglottic stenosis have reflux [24-28]. These results match the findings in this study, as 77% of the patients who have been diagnosed with subglottic stenosis and laryngomalacia had positive LPR results. These results signify the association between LPR and both subglottic stenosis and laryngomalacia. One of the main limitations of this study is the absence of a control group, which is mainly related to the difficulty in obtaining ethical approval for a relatively invasive technique in pediatric population. However, this could be one of the potential future research areas in this field to establish normative pharyngeal pH data in children through comparing their oropharyngeal pH monitoring results with other objective diagnostic testing of LPR.
In conclusion, eighty-five percent of the study subjects tolerated the pH probe insertion and successfully completed 24 hours of recording. These results prove the possibility of conducting oropharyngeal pH monitoring in children with good tolerability even in children below the age of 3 years old. Utilizing this pH-monitoring test, LPR was found to be more frequent in children diagnosed with subglottic stenosis and laryngomalacia. The results of this study support the proposed association between LPR and these two airway-related problems.
Acknowledgments
This project was full financially supported by King Saud University, through Vice Deanship of Research Chairs, Research Chairs Program, Research Chair of Voice, Swallowing, and Communication Disorders.
Footnotes
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Stavroulaki P. Diagnostic and management problems of laryngopharyngeal reflux disease in children. Int J Pediatr Otorhinolaryngol. 2006 Apr;70(4):579–90. doi: 10.1016/j.ijporl.2005.10.021. [DOI] [PubMed] [Google Scholar]
- 2.Koufman JA. The otolaryngologic manifestations of gastroesophageal reflux disease (GERD): a clinical investigation of 225 patients using ambulatory 24-hour pH monitoring and an experimental investigation of the role of acid and pepsin in the development of laryngeal injury. Laryngoscope. 1991 Apr;101(4 Pt 2 Suppl 53):1–78. doi: 10.1002/lary.1991.101.s53.1. [DOI] [PubMed] [Google Scholar]
- 3.El-Serag HB, Gilger M, Kuebeler M, Rabeneck L. Extraesophageal associations of gastroesophageal reflux disease in children without neurologic defects. Gastroenterology. 2001 Dec;121(6):1294–9. doi: 10.1053/gast.2001.29545. [DOI] [PubMed] [Google Scholar]
- 4.Yellon RF, Parameswaran M, Brandom BW. Decreasing morbidity following laryngotracheal reconstruction in children. Int J Pediatr Otorhinolaryngol. 1997 Aug;41(2):145–54. doi: 10.1016/s0165-5876(97)00067-0. [DOI] [PubMed] [Google Scholar]
- 5.Delahunty JE, Cherry J. Experimentally produced vocal cord granulomas. Laryngoscope. 1968 Nov;78(11):1941–7. doi: 10.1288/00005537-196811000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Little FB, Koufman JA, Kohut RI, Marshall RB. Effect of gastric acid on the pathogenesis of subglottic stenosis. Ann Otol Rhinol Laryngol. 1985 Sep-Oct;94(5 Pt 1):516–9. doi: 10.1177/000348948509400521. [DOI] [PubMed] [Google Scholar]
- 7.Jarmuz T, Roser S, Rivera H, Gal A, Roman J. Transforming growth factor-beta1, myofibroblasts, and tissue remodeling in the pathogenesis of tracheal injury: potential role of gastroesophageal reflux. Ann Otol Rhinol Laryngol. 2004 Jun;113(6):488–97. doi: 10.1177/000348940411300614. [DOI] [PubMed] [Google Scholar]
- 8.Merati AL, Lim HJ, Ulualp SO, Toohill RJ. Meta-analysis of upper probe measurements in normal subjects and patients with laryngopharyngeal reflux. Ann Otol Rhinol Laryngol. 2005 Mar;114(3):177–82. doi: 10.1177/000348940511400302. [DOI] [PubMed] [Google Scholar]
- 9.Vaezi MF, Schroeder PL, Richter JE. Reproducibility of proximal probe pH parameters in 24-hour ambulatory esophageal pH monitoring. Am J Gastroenterol. 1997 May;92(5):825–9. [PubMed] [Google Scholar]
- 10.Beaver ME, Stasney CR, Weitzel E, Stewart MG, Donovan DT, Parke RB, Jr, et al. Diagnosis of laryngopharyngeal reflux disease with digital imaging. Otolaryngol Head Neck Surg. 2003 Jan;128(1):103–8. doi: 10.1067/mhn.2003.10. [DOI] [PubMed] [Google Scholar]
- 11.Wiener GJ, Koufman JA, Wu WC, Cooper JB, Richter JE, Castell DO. Chronic hoarseness secondary to gastroesophageal reflux disease: documentation with 24-h ambulatory pH monitoring. Am J Gastroenterol. 1989 Dec;84(12):1503–8. [PubMed] [Google Scholar]
- 12.Wiener GJ, Tsukashima R, Kelly C, Wolf E, Schmeltzer M, Bankert C, et al. Oropharyngeal pH monitoring for the detection of liquid and aerosolized supraesophageal gastric reflux. J Voice. 2009 Jul;23(4):498–504. doi: 10.1016/j.jvoice.2007.12.005. [DOI] [PubMed] [Google Scholar]
- 13.Andrews TM, Orobello N. Histologic versus pH probe results in pediatric laryngopharyngeal reflux. Int J Pediatr Otorhinolaryngol. 2013 May;77(5):813–6. doi: 10.1016/j.ijporl.2013.02.017. [DOI] [PubMed] [Google Scholar]
- 14.Myer CM, 3rd, O’Connor DM, Cotton RT. Proposed grading system for subglottic stenosis based on endotracheal tube sizes. Ann Otol Rhinol Laryngol. 1994 Apr;103(4 Pt 1):319–23. doi: 10.1177/000348949410300410. [DOI] [PubMed] [Google Scholar]
- 15.van den Abbeele T, Couloigner V, Faure C, Narcy P. The role of 24 h pH-recording in pediatric otolaryngologic gastro-esophageal reflux disease. Int J Pediatr Otorhinolaryngol. 2003 Dec;67 Suppl 1:S95–100. doi: 10.1016/j.ijporl.2003.08.038. [DOI] [PubMed] [Google Scholar]
- 16.Contencin P, Maurage C, Ployet MJ, Seid AB, Sinaasappel M. Gastroesophageal reflux and ENT disorders in childhood. Int J Pediatr Otorhinolaryngol. 1995 Jun;32 Suppl:S135–44. doi: 10.1016/0165-5876(94)01157-s. [DOI] [PubMed] [Google Scholar]
- 17.Postma GN, Belafsky PC, Aviv JE, Koufman JA. Laryngopharyngeal reflux testing. Ear Nose Throat J. 2002 Sep;81(9 Suppl 2):14–8. [PubMed] [Google Scholar]
- 18.Little JP, Matthews BL, Glock MS, Koufman JA, Reboussin DM, Loughlin CJ, et al. Extraesophageal pediatric reflux: 24-hour double-probe pH monitoring of 222 children. Ann Otol Rhinol Laryngol Suppl. 1997 Jul;169:1–16. [PubMed] [Google Scholar]
- 19.Brigger MT, Sipp JA, Hartnick CJ. Tracheal pH monitoring: a pilot study in tracheostomy dependent children. Int J Pediatr Otorhinolaryngol. 2009 Jul;73(7):999–1001. doi: 10.1016/j.ijporl.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 20.McMurray JS, Gerber M, Stern Y, Walner D, Rudolph C, Willging JP, et al. Role of laryngoscopy, dual pH probe monitoring, and laryngeal mucosal biopsy in the diagnosis of pharyngoesophageal reflux. Ann Otol Rhinol Laryngol. 2001 Apr;110(4):299–304. doi: 10.1177/000348940111000402. [DOI] [PubMed] [Google Scholar]
- 21.Matthews BL, Little JP, Mcguirt WF, Jr, Koufman JA. Reflux in infants with laryngomalacia: results of 24-hour double-probe pH monitoring. Otolaryngol Head Neck Surg. 1999 Jun;120(6):860–4. doi: 10.1016/S0194-5998(99)70327-X. [DOI] [PubMed] [Google Scholar]
- 22.Iyer VK, Pearman K, Raafat F. Laryngeal mucosal histology in laryngomalacia: the evidence for gastro-oesophageal reflux laryngitis. Int J Pediatr Otorhinolaryngol. 1999 Aug;49(3):225–30. doi: 10.1016/s0165-5876(99)00205-0. [DOI] [PubMed] [Google Scholar]
- 23.Hartl TT, Chadha NK. A systematic review of laryngomalacia and acid reflux. Otolaryngol Head Neck Surg. 2012 Oct;147(4):619–26. doi: 10.1177/0194599812452833. [DOI] [PubMed] [Google Scholar]
- 24.Halstead LA. Gastroesophageal reflux: A critical factor in pediatric subglottic stenosis. Otolaryngol Head Neck Surg. 1999 May;120(5):683–8. doi: 10.1053/hn.1999.v120.a91766. [DOI] [PubMed] [Google Scholar]
- 25.Yellon RF, Coticchia J, Dixit S. Esophageal biopsy for the diagnosis of gastroesophageal reflux-associated otolaryngologic problems in children. Am J Med. 2000 Mar;108 Suppl 4a:131S–138S. doi: 10.1016/s0002-9343(99)00352-6. [DOI] [PubMed] [Google Scholar]
- 26.Mitzner R, Brodsky L. Multilevel esophageal biopsy in children with airway manifestations of extraesophageal reflux disease. Ann Otol Rhinol Laryngol. 2007 Aug;116(8):571–5. doi: 10.1177/000348940711600803. [DOI] [PubMed] [Google Scholar]
- 27.Carr MM, Abu-Shamma U, Brodsky LS. Predictive value of laryngeal pseudosulcus for gastroesophageal reflux in pediatric patients. Int J Pediatr Otorhinolaryngol. 2005 Aug;69(8):1109–12. doi: 10.1016/j.ijporl.2005.02.022. [DOI] [PubMed] [Google Scholar]
- 28.Giannoni C, Sulek M, Friedman EM, Duncan NO., 3rd Gastroesophageal reflux association with laryngomalacia: a prospective study. Int J Pediatr Otorhinolaryngol. 1998 Feb;43(1):11–20. doi: 10.1016/s0165-5876(97)00151-1. [DOI] [PubMed] [Google Scholar]


