Abstract
Introduction:
European system for cardiac operative risk evaluation (EuroSCORE) is a valuable tool in control of the quality of cardiac surgery. However, the validity of the risk score for the individual patient may be questioned. The present study was carried out to investigate whether the continued fall in short-term mortality reflects an actual improvement in late mortality, and subsequently, to investigate EuroSCORE as predictor of 1-year mortality.
Methods:
A population-based cohort study of 25,602 patients from a 12-year period from three public university hospitals undergoing coronary artery bypass grafting (CABG) or valve surgery. Analysis was carried out based on EuroSCORE, age and co-morbidity factors (residual EuroSCORE).
Results:
During the period the average age increased from 65.1 ± 10.0 years to 68.9 ± 10.7 years (P < 0.001, one-way ANOVA), and the number of females increased from 26.0% to 28.2% (P = 0.0012, Chi-square test). The total EuroSCORE increased from 4.67 to 5.68 while the residual EuroSCORE decreased from 2.64 to 1.83. Thirty-day mortality decreased from 4.07% in 1999–2000 to 2.44% in 2011–2012 (P = 0.0056; Chi-square test), while 1-year mortality was unchanged (6.50% in 1999–2000 vs. 6.25% in 2011–2012 [P = 0.8086; Chi-square test]).
Discussion:
The study demonstrates that both co-morbidity and age has a great impact on 30-day mortality. However, with time the impact of co-morbidity seems less. Thus, age is more important than co-morbidity in late mortality. The various developments in short and long-term mortality are not readily explained.
Conclusion:
Although 30-day mortality of CABG and valve surgery patients has decreased during the 12-year period, the 1-year mortality remains the same.
Keywords: Cardiac surgery, Coronary artery bypass grafting, European system for cardiac operative risk evaluation, Risk factor
INTRODUCTION
Cardiac surgery has always been associated with a higher perioperative risk than most other kinds of surgery. Crude mortality rates have been used as an indicator of quality of care, but their value is limited without knowledge of the patients’ risk profile. To compensate and adjust, a number of risk evaluation systems has been proposed and used during the last decades.[1,2,3,4,5,6] Of six different scoring systems, European system for cardiac operative risk evaluation (EuroSCORE) yields the highest predictive value of a population.[7] Although developed for in-hospital and 30-day mortality, the EuroSCORE has also proven to have some value in predicting long-term mortality of valve surgery.[8]
The EuroSCORE has been widely used not only for risk prediction, but also for the assessment of the quality of cardiac surgery. However, the original logistic EuroSCORE overestimates the hospital mortality[9,10,11] and in most centers the difference between actual mortality and predicted mortality has increased to 50–100%. Therefore, the EuroSCORE was updated in 2012.[12]
Without doubt, the EuroSCORE has been a valuable tool in control of the quality of surgery. None the less, the validity of the risk score for the individual patient may be questioned. The continued fall in short-term mortality achieved over the last decades furthermore calls for investigation of the score as a tool in the assessment of the patients’ long-term survival. The present study was carried out to see whether the continued fall in short-term mortality reflects an actual improvement in 1-year mortality, and subsequently, to investigate EuroSCORE as predictor of 1-year mortality.
METHODS - DESIGN AND SETTING
We conducted this population-based cohort study from three public university hospitals, which provide cardiothoracic surgery for all inhabitants of hospitals uptake area, a mixed rural-urban population, which again covers a little more than 60% of the Danish population. The patients were identified in the Western Denmark Heart Registry (WDHR).[13] WDHR is a collaborative initiative between Western Denmark's three major cardiac centers and contains information from January 1, 1999 on all invasive cardiac procedures: Coronary angiography, percutaneous coronary intervention, and all types of adult cardiac surgery. The registry holds extensive mandatory and prospectively registered information on patient and procedural characteristics. Due to the unique Central Personal Registry number assigned to each Danish citizen at birth and to residents on immigration, it is possible to make accurate linkage of all registries at an individual level. Thus, the outcome all-cause death was studied through linkage to the Danish Civil Registration System.[14] The Danish National Health Service provides tax-funded medical care for all Danish residents. The study was approved by the Danish Data Protection Agency (record number: 2013-1-16-02-17-13).
During the period from April 1, 1999 to December 31, 2012 a total of 25,635 adult (age ≥ 15 years) cardiac surgical patients with eligible procedures were identified in the WDHD. Included procedures were; on-and off-pump coronary artery bypass grafting (CABG), aortic valve surgery, mitral valve surgery and combinations. All thoracic aortic surgery or other single or combined procedures were a-priori excluded due to the difficulty in comparison of the different types of surgery. Thirty-three patients with invalid civil registration were excluded leaving 25,602 patients for analysis of which 16,424 was standalone CABG, 6,183 valves and 2,995 combinations of CABG and valves. Although the primary cohort was relatively large dividing into years and EuroSCORE would make the differences and variation in comparison between the individual groups relatively great, and hence EuroSCORE was divided into groups (0-2, 3-5, 6-8, 9-11, 12+). Further analysis was based on age groups (15-59, 60-69, 70-74, 75-79, 80-84, 85+) and residual EuroSCORE (EuroSCORE minus age and procedure factors) divided into (0-1, 2-3, 4-5, 6-7, 8+).
RESULTS
Characteristics of age, sex and EuroSCORE parameters are given in Table 1. During the period the average age of the patients at the time of operation increased from 65.1 ± 10.0 years to 68.9 ± 10.7 years (P < 0.001, one-way ANOVA), and the number of females increased from 26.0% to 28.2% (P = 0.0012, Chi-square test). The total EuroSCORE increased statistically significant over time, but when removing the age-, sex- and procedure factors from the EuroSCORE an actual fall was seen in the remaining primary morbidity factors.
Table 1.
Numbers, procedure types together with age, sex and EuroSCORE divided in time periods. Residual EuroSCORE is total EuroSCORE minus age, sex and procedure scores
| Years | Number of patients | Procedure types (%) | Average age | Number of females (%) | EuroSCORE | |||
|---|---|---|---|---|---|---|---|---|
| CABG | Valves | Combination | Total | Residual | ||||
| 1999-2000 | 3269 | 81.3 | 12.5 | 6.2 | 65.1 | 26.0 | 4.67 | 2.64 |
| 2001-2002 | 4291 | 75.2 | 15.5 | 9.3 | 65.8 | 25.8 | 4.75 | 2.42 |
| 2003-2004 | 3929 | 66.4 | 20.7 | 12.9 | 66.6 | 25.2 | 4.93 | 2.26 |
| 2005-2006 | 3655 | 59.3 | 25.1 | 15.6 | 67.6 | 26.0 | 5.65 | 2.20 |
| 2007-2008 | 3331 | 58.5 | 27.3 | 14.2 | 66.9 | 27.1 | 5.70 | 2.22 |
| 2009-2010 | 3235 | 52.1 | 34.8 | 13.1 | 68.0 | 29.1 | 6.46 | 2.52 |
| 2011-2012 | 3892 | 54.7 | 34.5 | 10.8 | 68.9 | 28.2 | 5.68 | 1.83 |
| P | 25,602 | <0.001# | <0.001* | 0.0012# | <0.001* | <0.001* | ||
Statistics: #Chi-square test, *One-way ANOVA. Valves=Aortic valves or mitral valves. CABG: Coronary artery bypass grafting, EuroSCORE: European system for cardiac operative risk evaluation
Mortality is demonstrated in Figure 1. During the observation period, 30-day mortality decreased from 4.07% in 1999–2000 to 2.44% in 2011–2012 (P = 0.0056; Chi-square test). At the same time, the 1-year mortality was unchanged, being 6.50% in 1999–2000 and 6.25% in 2011–2012 (P = 0.8086; Chi-square test). The figure further demonstrates that CABG patients follows the same patterns with decrease in 30-day mortality from 2.9% to 1.7% (P = 0.007; Chi-square test) and 1-year mortality unchanged 4.8% to 4.3% (P = 0.388; Chi-square test).
Figure 1.
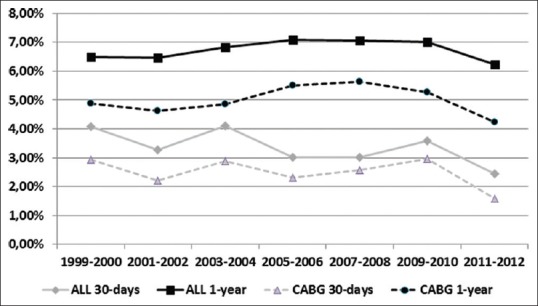
30-day and 1-year mortality of patient cohort (25,602) divided on time periods and type of surgery. Statistical significant change in 30-day mortality (P = 0.0056; Chi-square test). No change in 1-year mortality (P = 0.8086, Chi-square test)
Figures 2–4 shows Kaplan–Meier 1-year survival curves divided on EuroSCORE groups, age and residual EuroSCORE for CABG patients. It demonstrates that the 30-day mortality is highly associated with EuroSCORE group [Figure 2], age group [Figure 3], as well as residual EuroSCORE [Figure 4]. Figure 2 also establishes a statistical significant association between EuroSCORE group and 1-year mortality, seen by both different endpoints and survival curves not running parallel, and further, by mortality rates from 30-day to 1-year being 0.8% in EuroSCORE 0–2 and 9.7% in EuroSCORE 12+. Similarly, when comparing age groups, the mortality was 1.0% in the age group below 60 compared to 9.1% in patients at age 85 and above [Figure 3]. The difference between groups was less pronounced in residual EuroSCORE [Figure 4].
Figure 2.
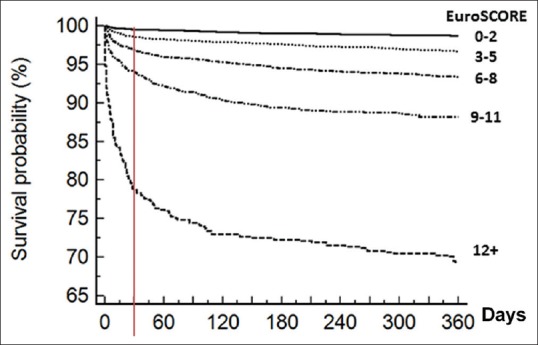
Kaplan–Meier 1-year survival probability curves divided on preoperative European system for cardiac operative risk evaluation (P < 0.0001)
Figure 4.
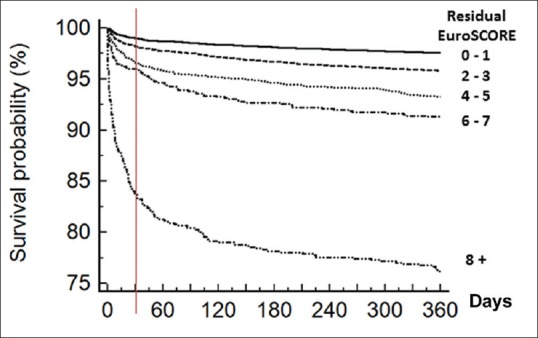
Kaplan–Meier 1-year survival probability curves divided on residual European system for cardiac operative risk evaluation (EuroSCORE) (EuroSCORE sum minus age and procedure score) (P < 0.0001)
Figure 3.
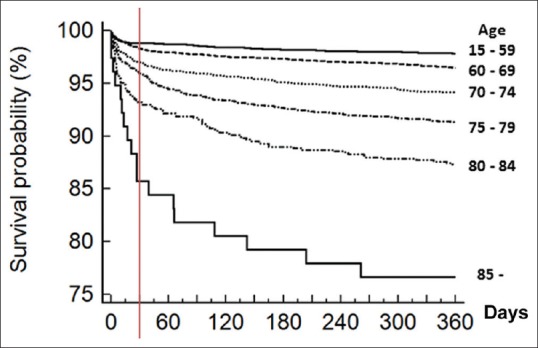
Kaplan–Meier 1-year survival probability curves divided on age groups (P < 0.0001)
DISCUSSION
The study indicates that although 30-day mortality has improved over the last decade, the 1-year mortality seems the same, a little more than 6%. The results of our data are basically guided by CABG, covering more than 62% of procedures together with the, over the years, increased number in valves which again are followed by a higher EuroSCORE. Finally, our data suggest some association between the EuroSCORE and 1-year mortality.
During the period, the average age of the patients increased with almost 4 years, the number of females increased slightly, and the fraction of procedures other than CABG increased. As a consequence, the overall EuroSCORE has increased almost one point during the period. However, the impact of age, sex and procedure type seems more or less counterbalanced by a lower morbidity as the residual EuroSCORE has gone down almost one point. The 40% reduction in 30-day mortality during the 12-year period is in agreement with the findings, which lead to development of EuroSCORE II12 and is most likely part of the general improvement in surgical expertise and techniques, handling of cardiac physiology, blood transfusion practices and advances in mechanical ventilation, which has taken place in almost all centers, also illustrated by the overestimation of the EuroSCORE seen in the late zeroes.[9,10,11]
The lack of improvement in 1-year mortality is interesting. During the period, the overall EuroSCORE of CABG patients has increased from 4.20 to 4.37. However, at the same time, the residual EuroSCORE has declined from 2.68 to 1.88, which indicates that in CABG patients the long-term mortality is more dependent on high age than morbidity factors. This is further supported by the fact that the three Kaplan-Meier plots are running almost parallel after approximately 150 days after surgery.
Our data support that the EuroSCORE is valuable in prediction and estimation of long-term mortality.[8,15,16] A high EuroSCORE, in our material set to ≥12 has higher 1-year mortality, being almost three times higher compared to EuroSCORE 9–11 (31.0% vs. 11.8%). Furthermore, as the fraction of patients with EuroSCORE higher than 12 has been almost constant since 2005, this may partly explain the constant 1-year mortality.
Our study demonstrates that age is more important in late mortality than co-morbidity. It is clear that both factors are important for 30-day mortality but our data also demonstrate that co-morbidity has much less impact on mortality 3 months postsurgery [Figure 4].
LIMITATION OF THE STUDY
The various developments of 30-day mortality and 1-year mortality suggest that inborn determinant elements of cardiac disease, co-morbidity, and to a lesser extent surgical complications have a greater impact on 30-day mortality than on 1-year survival. Hence, an improvement in 30-day mortality does not necessarily reflect improved outcome.
Further, the increased age of patients during the time period may certainly account for slightly higher 1-year mortality but only to a lesser degree. The increased number of females, who in general lives longer, may to some extend counterweigh the increased age in the cohort.
Finally, the important factors for survival after cardiac disease are the postoperative rehabilitation, recovery and medical treatment, but as we have no systematic registered data regarding the postoperative regimens, this is a relative limitation to our study.
CONCLUSION
Although 30-day mortality of CABG and valve surgery patients has decreased during a 12-year period, the 1-year mortality remains the same. The various developments in short- and long-term mortality are not readily explained, but overall age seems to grow increasingly more important than morbidity factors in CABG patients in the time after surgery. A large study evaluating causes of death is needed to further explain our findings.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Parsonnet V, Dean D, Bernstein AD. A method of uniform stratification of risk for evaluating the results of surgery in acquired adult heart disease. Circulation. 1989;79(6 Pt 2):I3–12. [PubMed] [Google Scholar]
- 2.Higgins TL, Estafanous FG, Loop FD, Beck GJ, Blum JM, Paranandi L. Stratification of morbidity and mortality outcome by preoperative risk factors in coronary artery bypass patients. A clinical severity score. JAMA. 1992;267:2344–8. [PubMed] [Google Scholar]
- 3.Tuman KJ, McCarthy RJ, March RJ, Najafi H, Ivankovich AD. Morbidity and duration of ICU stay after cardiac surgery. A model for preoperative risk assessment. Chest. 1992;102:36–44. doi: 10.1378/chest.102.1.36. [DOI] [PubMed] [Google Scholar]
- 4.Lovegrove J, Valencia O, Treasure T, Sherlaw-Johnson C, Gallivan S. Monitoring the results of cardiac surgery by variable life-adjusted display. Lancet. 1997;350:1128–30. doi: 10.1016/S0140-6736(97)06507-0. [DOI] [PubMed] [Google Scholar]
- 5.Roques F, Nashef SA, Michel P, Gauducheau E, de Vincentiis C, Baudet E, et al. Risk factors and outcome in European cardiac surgery: Analysis of the EuroSCORE multinational database of 19030 patients. Eur J Cardiothorac Surg. 1999;15:816–22. doi: 10.1016/s1010-7940(99)00106-2. [DOI] [PubMed] [Google Scholar]
- 6.Nashef SA, Roques F, Michel P, Gauducheau E, Lemeshow S, Salamon R. European system for cardiac operative risk evaluation (EuroSCORE) Eur J Cardiothorac Surg. 1999;16:9–13. doi: 10.1016/s1010-7940(99)00134-7. [DOI] [PubMed] [Google Scholar]
- 7.Geissler HJ, Hölzl P, Marohl S, Kuhn-Régnier F, Mehlhorn U, Südkamp M, et al. Risk stratification in heart surgery: Comparison of six score systems. Eur J Cardiothorac Surg. 2000;17:400–6. doi: 10.1016/s1010-7940(00)00385-7. [DOI] [PubMed] [Google Scholar]
- 8.Toumpoulis IK, Anagnostopoulos CE, Toumpoulis SK, DeRose JJ, Jr, Swistel DG. EuroSCORE predicts long-term mortality after heart valve surgery. Ann Thorac Surg. 2005;79:1902–8. doi: 10.1016/j.athoracsur.2004.12.025. [DOI] [PubMed] [Google Scholar]
- 9.Holinski S, Claus B, Christ T, Kasperiunaite R, Konertz W. Overestimation of the operative risk by the EuroSCORE also in high-risk patients undergoing aortic valve replacement with a stentless biological prosthesis. Heart Surg Forum. 2010;13:E13–6. doi: 10.1532/HSF98.20091071. [DOI] [PubMed] [Google Scholar]
- 10.Gummert JF, Funkat A, Osswald B, Beckmann A, Schiller W, Krian A, et al. EuroSCORE overestimates the risk of cardiac surgery: Results from the national registry of the German Society of Thoracic and Cardiovascular Surgery. Clin Res Cardiol. 2009;98:363–9. doi: 10.1007/s00392-009-0010-8. [DOI] [PubMed] [Google Scholar]
- 11.Osswald BR, Gegouskov V, Badowski-Zyla D, Tochtermann U, Thomas G, Hagl S, et al. Overestimation of aortic valve replacement risk by EuroSCORE: Implications for percutaneous valve replacement. Eur Heart J. 2009;30:74–80. doi: 10.1093/eurheartj/ehn523. [DOI] [PubMed] [Google Scholar]
- 12.Nashef SA, Roques F, Sharples LD, Nilsson J, Smith C, Goldstone AR, et al. EuroSCORE II. Eur J Cardiothorac Surg. 2012;41:734–44. doi: 10.1093/ejcts/ezs043. [DOI] [PubMed] [Google Scholar]
- 13.Schmidt M, Maeng M, Jakobsen CJ, Madsen M, Thuesen L, Nielsen PH, et al. Existing data sources for clinical epidemiology: The Western Denmark Heart Registry. Clin Epidemiol. 2010;9;2:137–44. doi: 10.2147/clep.s10190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pedersen CB. The Danish civil registration system. Scand J Public Health. 2011;39(7 Suppl):22–5. doi: 10.1177/1403494810387965. [DOI] [PubMed] [Google Scholar]
- 15.De Maria R, Mazzoni M, Parolini M, Gregori D, Bortone F, Arena V, et al. Predictive value of EuroSCORE on long term outcome in cardiac surgery patients: A single institution study. 2005;91:779–84. doi: 10.1136/hrt.2004.037135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kobayashi KJ, Williams JA, Nwakanma LU, Weiss ES, Gott VL, Baumgartner WA, et al. EuroSCORE predicts short- and mid-term mortality in combined aortic valve replacement and coronary artery bypass patients. J Card Surg. 2009;24:637–43. doi: 10.1111/j.1540-8191.2009.00906.x. [DOI] [PubMed] [Google Scholar]


