The Editor,
A 70-year-old male patient with chronic obstructive pulmonary disease was operated for off-pump coronary artery bypass grafting surgery. Patient had oral cuffed endotracheal tube (ET) size 8 mm. After the surgery, soft nasogastric tube-size 14 Fr gauge without guide wire was inserted nasally before shifting patient to Intensive Care Unit (ICU). The passage of the tube was smooth, and its gastric placement was confirmed by epigastric auscultation. In ICU, chest X-ray was done before giving any medication through a feeding tube as per the institute's protocol. It revealed course of a nasogastric tube into right lower lobe bronchus [Figure 1]. The tube was removed, and no other pulmonary complications were observed.
Figure 1.
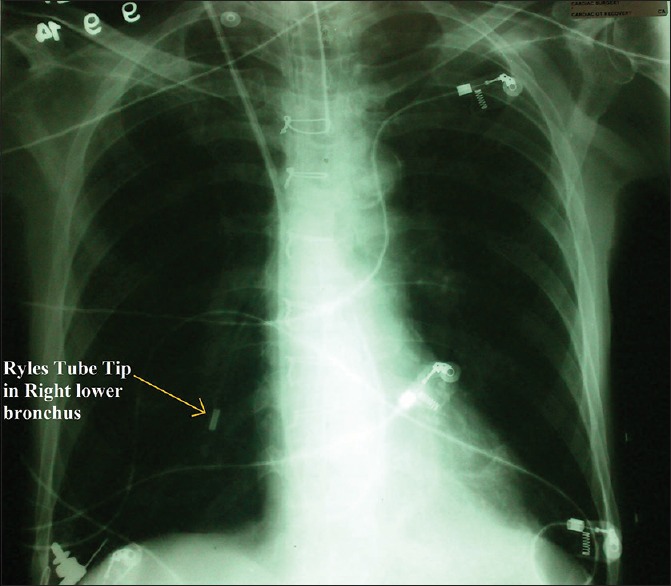
Chest X-ray showing nasogastric tube entering right lower lobe bronchus
The insertion of nasogastric tube insertion has been considered as being easy and mostly uneventful procedure. 2% incidence of tracheopulmonary complications from nasogastric tube insertion has been reported.[1] Malpositioned nasogastric tube causing complications such as pneumothorax, pleural effusion, retropharyngeal abscess and lung abscess have all been reported in the literature.[1,2] Such patients may not have symptoms suggestive of the malpositioning. Abnormal position was recognized only after chest X-ray or after enteral feeding through nasogastric gastric tube (NGT) had started with resulting pulmonary complications. Malposition of NGT can be missed or misinterpreted on chest X-ray.[1,2]
Air insufflation and epigastric auscultation are commonly used sign of gastric placement. However, good thoracoabdominal sound transmission may cause misinterpretation even with tracheobronchial misplacement of NGT. 20% false gastric confirmation by auscultation has been reported by Benya et al.[3] Laryngoscope can be used to direct the NGT while inserting. Compact, disposable colorimetric end-tidal CO2 detector has been used to confirm tube position with 100% specificity and a 100% sensitivity rate among 53 insertions.[4] Small-diameter (5-6 mm) upper gastrointestinal tract video flexible endoscopes can be used for guidewire placement over which feeding tube is rolled over. This can be used in the complicated or difficult or prior failed attempts.[5]
Failure to identify a malpositioned NGT may lead to fatal pulmonary complications. Hence, it is essential to confirm radiographically before starting enteral feeding or medications. Mostly narrow lumen tubes with stiff inner guide wire have been reported in the malposition complication.[6] In the present case, we had a malposition of large bore 14 French gauge nasogastric tube without guide wire. Inadequately inflated ETT cuff may have been the reason for the passage of NGT in trachea as cuff pressure was not monitored. While inserting NGT, confirm cuff of ETT adequately inflated and NGT can be directed to esophagus under direct laryngoscopic vision with the help of Magill's forcep (Manufacturer - Anaesthetics). After placing NGT, epigastric auscultation can mislead about the positioning as, in this case. However, checking for the air coming out of the outer end of NGT and confirming it by seeing air bubbles with every expiration of the patient when outer end of NGT is placed below the water level, can be proposed as a method to identify the tracheal malposition of NGT. Chest X-ray can confirm the position of NGT. Complication in the present case was avoided as no feeding or medication was given through the tube. This case emphasizes the significance of making clinicians aware about the potential morbidity and mortality associated with such a simple procedure.
REFERENCES
- 1.Rassias AJ, Ball PA, Corwin HL. A prospective study of tracheopulmonary complications associated with the placement of narrow-bore enteral feeding tubes. Crit Care. 1998;2:25–28. doi: 10.1186/cc120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roubenoff R, Ravich WJ. Pneumothorax due to nasogastric feeding tubes. Report of four cases, review of the literature, and recommendations for prevention. Arch Intern Med. 1989;149:184–8. doi: 10.1001/archinte.149.1.184. [DOI] [PubMed] [Google Scholar]
- 3.Benya R, Langer S, Mobarhan S. Flexible nasogastric feeding tube tip malposition immediately after placement. JPEN J Parenter Enteral Nutr. 1990;14:108–9. doi: 10.1177/0148607190014001108. [DOI] [PubMed] [Google Scholar]
- 4.Araujo-Preza CE, Melhado ME, Gutierrez FJ, Maniatis T, Castellano MA. Use of capnometry to verify feeding tube placement. Crit Care Med. 2002;30:2255–9. doi: 10.1097/00003246-200210000-00013. [DOI] [PubMed] [Google Scholar]
- 5.Pillai JB, Vegas A, Brister S. Thoracic complications of nasogastric tube: Review of safe practice. Interact Cardiovasc Thorac Surg. 2005;4:429–33. doi: 10.1510/icvts.2005.109488. [DOI] [PubMed] [Google Scholar]
- 6.Takwoingi YM. Inadvertent insertion of a nasogastric tube into both main bronchi of an awake patient: A case report. Cases J. 2009;2:6914. doi: 10.1186/1757-1626-2-6914. [DOI] [PMC free article] [PubMed] [Google Scholar]


