Abstract
35 year old with ruptured lateral wall of Left ventricle (LV) resulting in large pseudo aneurysm contained within the pericardium [Figure 1]. There was free flow of blood between the LV and pseudoaneurysm.He underwent endoventricular patch plasty of the defect after opening the wall of aneurysm [Figure 2].
Keywords: LV Pseudoaneurysm, Recanalised coronary, Transesophageal echo
A 35-year-old man had come to the cardiovascular outpatient department with vague chest discomfort and shortness of breath for 3 months duration. He had a history of severe, sudden onset chest pain 4 months back which settled with sublingual nitrates from a local pharmacy. His history was negative for trauma, previous cardiac surgery/ablation and chronic cardiac ailments. 12-lead ECG showed ST elevation in lateral leads and T-wave inversion in inferior leads. His two-dimensional echo findings were shocking to us. He had a ruptured lateral wall of a left ventricle (LV) resulting in a large pesudoaneurysm.[1] contained within the pericardium [Figure 1]. The neck of the pseudoaneurysm measured around 35 mm and the largest diameter of the aneurysmal cavity measured around 125 mm. Retrospective auscultation of the heart revealed a grade 4/6 holosystolic murmur. There was a free flow of blood between the LV and pseudoaneurysm during the phases of the cardiac cycle. His coronary angiogram was surprisingly normal. He underwent an endoventricular patch plasty.[2,3] of the defect [Figure 2]. He could be weaned from bypass after the institution of intra-aortic balloon pump along with high inotropic support. Myocardial infarction as a result of coronary artery disease is the most common cause of LV pseudoaneurysm. However, our patient had a recanalized normal coronary with LV pseudoaneurysm. Though we did not do an endomyocardial biopsy to rule out other causes, thrombotic occlusion and subsequent spontaneous recanalization of left circumflex artery was felt to be the primary cause of this pseudoaneurysm.[4]
Figure 1.

Mid esophageal four chamber view showing pseudoaneurysm
Figure 2.
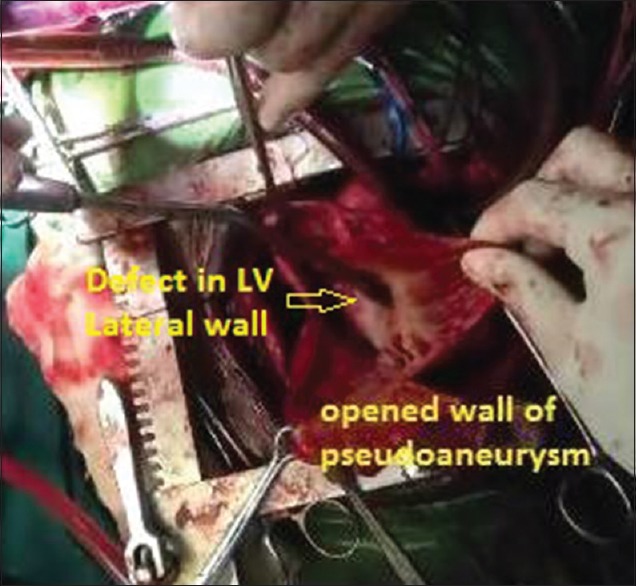
Opened pseudoaneurysmal cavity and the defect in left ventricle lateral wall
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Frances C, Romero A, Grady D. Left ventricular pseudoaneurysm. J Am Coll Cardiol. 1998;32:557–61. doi: 10.1016/s0735-1097(98)00290-3. [DOI] [PubMed] [Google Scholar]
- 2.Prêtre R, Linka A, Jenni R, Turina MI. Surgical treatment of acquired left ventricular pseudoaneurysms. Ann Thorac Surg. 2000;70:553–7. doi: 10.1016/s0003-4975(00)01412-0. [DOI] [PubMed] [Google Scholar]
- 3.Eren E, Bozbuga N, Toker ME, Keles C, Rabus MB, Yildirim O, et al. Surgical treatment of post-infarction left ventricular pseudoaneurysm: A two-decade experience. Tex Heart Inst J. 2007;34:47–51. [PMC free article] [PubMed] [Google Scholar]
- 4.Cho JM, Raffel OC, Stone JR, Kim CJ, Jang IK. Spontaneous recanalization of a coronary artery after thrombotic occlusion: In vivo demonstration with optical coherence tomography. J Am Coll Cardiol. 2010;55:1274. doi: 10.1016/j.jacc.2008.11.071. [DOI] [PubMed] [Google Scholar]


