Abstract
Lipomatous hypertrophy of the interatrial septum (LHIS) is an uncommon cause of superior vena cava syndrome (SVCS). Fibrosing mediastinal lymphadenopathy is another cause of SVCS. We present a 65-year-old female patient with a history of tuberculosis (TB) and the coexistence of LHIS and fibrosing mediastinitis due to TB of the lung. Fibrosing or sclerosing mediastinitis is a rare entity with few cases published in the western literature. She presented with mild symptomatology of SVCS and she underwent on transthoracic and transesophageal echocardiography, computed tomography scan, magnetic resonance imaging, and venography. Due to the development of an abundant collateral venous system seen on venography and her negation for any treatment, she did not undergo yet on any intervention. To our knowledge, this is the first case reported in the international bibliography in which LHIS and sclerosing lymphadenopathy are simultaneously diagnosed in the same patient.
Keywords: Fibrosing mediastinal lymphadenopathy, Lipomatous hypertrophy of the interatrial septum, Superior vena cava syndrome, Tuberculosis
INTRODUCTION
Lipomatous hypertrophy of the interatrial septum (LHIS) is defined as a noncapsulated, circumscribed fatty mass, 2 cm thick of the atrial septum.[1] LHIS is uncommon, but due to technology is more frequently recognized. In several clinical studies no typical symptoms of LHIS are described. This cardiac lesion can cause right atrial obstruction, superior vena cava syndrome (SVCS), intractable supraventricular arrhythmias, or sudden cardiac death.[1] It was first described by Prior in 1964 in five patients at postmortem examination.[1,2] Although many theories have been suggested, etiology of LHIS is still unknown.[3,4] Fibrosing mediastinal lymphadenopathy due to tuberculosis (TB) is a rare cause of SVCS.[5]
CASE REPORT
We present a 65-year-old female with a history of a treated TB and mild symptomatology of SVCS. She underwent on transthoracic and transesophageal echocardiography (TEE) and then in computed tomography (CT) scan and venography. In transthoracic and TEE as well as in CT scan was seen an LHIS [Figure 1a and b]. This lesions, as above mentioned, are usually clinically silent and discovered incidentally at echocardiography or intraoperatively. It may cause SVCS or supraventricular arrhythmias. Our patient had an obstructed SVC but the reason of this, was the fibrosing mediastinal lymphadenopathy due to TB. This woman developed a chronic obstruction of the SVC as a complication of mediastinal and lung TB. However, she developed, as a complication, an obstruction of the SVC that became chronic due to a late diagnosis. The fibrosing mediastinitis is well shown in CT scan [Figure 2a] and then the cavography [Figure 2b] showed a severe and extensive obstruction of the SVC at the level of junction of the left and right innominate vein, before the composition of the SVC. There is not any reason to treat the LHIS because our patient had normal sinus rhythm, and she has never experienced any palpitation or syncoptic episode. The second finding, the scherosing mediastinitis which obstructs the SVC could be treated. We had the dilemma between affront or not affront this lesion. Due to patient negation for any treatment and the mild symptomatology as well as the existence of an abundant collateral venous system seen on venography, it has been decided to not perform any intervention. According the international bibliography the endovascular therapy is of primary selected way of treatment with the implantation in situ a stent.[5]
Figure 1.
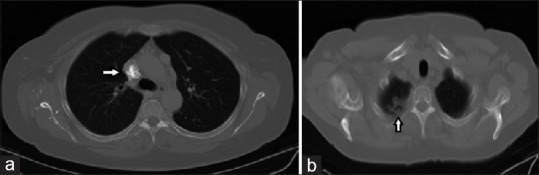
Thoracic computed tomography scan. (a) A heavily calcified mass with almost 4 cm diameter, at the level of the conjunction of the anonymous veins, compressing the superior vena cava (arrow). Multiple small vessels in the anterior mediastinum. No ascending aorta involvement is noticed. (b) Upper pulmonary field level; fibrosis of the right upper pulmonary lobe (arrow)
Figure 2.
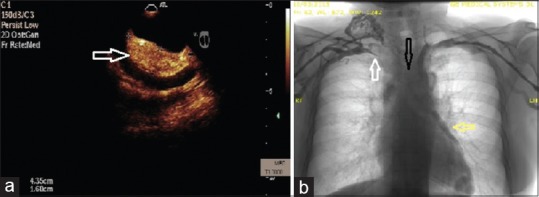
(a) Transesophageal echocardiography, interatrial septal fatty infiltration was demonstrated (arrow). Interatrial septum of 1.6 cm thick (b) beside subtraction venography shows: On the right, progressive stenosis of the right anonymous vein and finally stop before the superior vena cava origin (white arrow) with multiple venous collateral vessels formation. On the left, there is a stop at the distal part of left anonymous vein (black arrow) and presence of enlarged varicose veins at the level of the left heart margin area (yellow arrow)
DISCUSSION
Although LHIS has often been identified incidentally, atrial arrhythmias, including atrial fibrillation, atrial premature complexes, supraventricular tachycardia, ectopic atrial rhythm, and junctional rhythm, have been associated with lipomatous hypertrophy.[1] Intervention is not usually required. Surgical resection has been performed in symptomatic patients with SVC obstruction or with intractable arrhythmias.[1,2,3] It differs from a pure lipoma in that lipomas are true neoplasms and usually occur in a much younger patients. However, surgical treatment is similar for both.[3] CT scan and magnetic resonance imaging can be useful in selected patients with large fatty infiltration or marked hypertrophy of the septum. Lipomatous hypertrophy of the IAS can be surgically excised. The large IAS defect that results after excision of the mass requires closure using a pericardial or a synthetic patch. Recurrence after excision has not been reported, and the long-term prognosis is excellent. Malignant degeneration is a rare occurrence.[3,4] Surgical therapy appears to be reserved to patients with SVC obstruction or any rhythm disturbances.[4] The main problem is differentiating LHIS from a cardiac neoplasm when the lesion is discovered with echocardiography. With improvements in imaging, LHIS should possibly be recognized more frequently. However, surgical resection should only be performed in symptomatic patients.[4]
The second finding was the fibrosing mediastinal lymphadenopathy. The most common etiologies for sclerosing mediastinitis are TB and histoplasmosis.[5] In TB sclerosing mediastinitis, hilar adenopathy or active pulmonary disease are not a common found. Interestingly, of the following vascular structures, such as a pulmonary artery, pulmonary veins, and SVC, the latter is the least frequently compromised.[5]
CONCLUSION
We will suggest considering LHIS as a part of the differential diagnosis for any atrial cardiac tumor. It may be the cause of SVCS, but other causes as mediastinal lymphadenopathy may be responsible. The rich diagnostic armamentarium helps us to take the right decision and to perform the correct intervention.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.O’Connor S, Recavarren R, Nichols LC, Parwani AV. Lipomatous hypertrophy of the interatrial septum: An overview. Arch Pathol Lab Med. 2006;130:397–9. doi: 10.5858/2006-130-397-LHOTIS. [DOI] [PubMed] [Google Scholar]
- 2.Christiansen S, Stypmann J, Baba HA, Hammel D, Scheld HH. Surgical management of extensive lipomatous hypertrophy of the right atrium. Cardiovasc Surg. 2000;8:88–90. doi: 10.1016/s0967-2109(99)00080-0. [DOI] [PubMed] [Google Scholar]
- 3.Moinuddeen K, Marica S, Clausi RL, Zama N. Lipomatous interatrial septal hypertrophy: An unusual cause of intracardiac mass. Eur J Cardiothorac Surg. 2002;22:468–9. doi: 10.1016/s1010-7940(02)00369-x. [DOI] [PubMed] [Google Scholar]
- 4.Verberkmoes NJ, Kats S, Tan-Go I, Schönberger JP. Resection of a lipomatous hypertrophic interatrial septum involving the right ventricle. Interact Cardiovasc Thorac Surg. 2007;6:654–7. doi: 10.1510/icvts.2007.157776. [DOI] [PubMed] [Google Scholar]
- 5.Esquivel L, Diaz-Picado H. Fibrosing TB mediastinitis presenting as a superior vena cava syndrome: A case presentation and echocardiogram correlate. Echocardiography. 2006;23:588–91. doi: 10.1111/j.1540-8175.2006.00265.x. [DOI] [PubMed] [Google Scholar]


