Abstract
Background:
Electroconvulsive therapy (ECT) is one of the available and the most effective therapies for the treatment of resistant depression. Considering the crucial role of seizure duration on therapeutic response in patients treated with ECT, this study aimed to compare the effect of ketamine and sodium thiopental anesthesia during ECT for treatment of patients with drug-resistant major depression (DRMD).
Materials and Methods:
In a double-blind randomized clinical trial, 160 patients with DRMD were selected consequently and were assigned randomly into two groups including ketamine 0.8 mg/kg and sodium thiopental 1.5 mg/kg. The seizure duration, recovery time, and the side effects of anesthesia were evaluated after 1-h after anesthesia. Data of recovery time and complication collected in 2nd, 4th, 6th, and 8th ECT. Depression was assessed by Hamilton depression scale.
Results:
The results indicated that ketamine and sodium thiopental had a significant effect on the reduction of depression scores in patients with DRMD (P < 0.05). Complications such as a headache, nausea, pain at the injection site, short-term delirium, and long-term delirium were higher in ketamine group (P > 0.05). But ketamine was more effective in improvement of depression score and increasing systolic and diastolic blood pressure (P < 0.05). The mean of seizure duration showed a decreasing trend and was significant between two study groups (P < 0.05).
Conclusion:
Anesthesia induced by ketamine during ECT therapy increased blood pressure and seizure duration. Therefore, due to lower medical complication and attack rate of seizure, ketamine is an appropriate option for anesthesia with ECT in patients with DRMD.
Keywords: Anesthesia, Depression, Ketamine, Sodium thiopental
INTRODUCTION
Depression is a chronic and recurrent disorder and up to 16% of adult population experience at least one period of depression through their life.[1,2] Due to the high prevalence of depression in adolescents,[3] the World Health Organization has predicted that by 2020 depression will become the second major disease in the world.[4] Therefore, the discovery and the development of more effective therapies is of significant importance for alleviating this problem. Despite the recognition of different types of treatment for depression, a group of patients does not respond to the treatment that is called drug-resistant major depression (DRMD). Electroconvulsive therapy (ECT) is one of the oldest therapies available for the treatment of resistant depression and is still the most effective (at a rate of 50–70%) method.[5] Performing ECT without anesthesia could have several side effects such as a headache, confusion, delirium, fracture of vertebrae and ribs, muscle pain, nausea, vomiting, and memory loss.[6,7] Intravenous anesthetics applied for this purpose include methohexital, propofol, midazolam, remifentanil, lidocaine, sodium thiopental, and ketamine. Considering the crucial role of seizure duration on therapeutic response in patients treated with ECT, drugs such as ketamine, sodium thiopental that has more and better impact on increasing the seizure duration are of more attention and usage.[8,9] However, there is a controversy in finding of the positive effects of anesthetic drugs, especially sodium thiopental and ketamine. In addition, more conducted studies have a retrospective design or prospective studies with low sample size. Therefore, the aim of the current study was to compare the effect of anesthesia with ketamine or sodium thiopental during ECT in patients with DRMD.
MATERIALS AND METHODS
A single-blind simple randomized clinical trial were enrolled 160 patients with DRMD, who is referring to Psychiatric Center of Amir Kabir Hospital, Arak, Iran. Patients who were between 20 and 60-year-old, affecting to DRMD according to Diagnostic and Statistical Manual of Mental Disorders-text revised-DSM-IV-TR diagnostic criteria with confirmation of psychiatrist, and without any contraindications for ECT included to the study. Moreover, patients who are affect to any type of cardiovascular and cerebrovascular disease, high intracranial pressure, respiratory tract diseases, serious bone fractures, glaucoma, high intraocular pressure, uncontrolled hypertension, arterial aneurysm or cerebrovascular malformation, previous history of epilepsy, alcohol, and drug abuse with history of sensitivity to anesthetic agents, pregnancy, other psychiatric disorders, dementia were excluded. In addition, study subjects did not performing ECT in the last 3 months. The demographic information and past medical history was registered. In addition, hemodynamic parameters were measured before and after ECT and were recorded in the patients’ checklist. All patients were nil per os (NPO) for at least 6–8 h before ECT After recruitment of patients and taking informed consent, random allocation applied by block randomization method. Group A received ketamine 0.8 mg/kg and Group B received sodium thiopental 1–1.5 mg/kg intravenously before ECT and were anesthetized. Then ECT was performed for 30–90 s 3 times a week. Ultimately, 8 sessions of ECT was performed. After finishing ECT sessions, the patient's recovery time and postanesthesia complications were checked and recorded in the 1st h by an anesthesiologist after 2nd, 4th, 6th, and 8th sessions of ECT.
Hamilton depression rating scale (HDRS-17 items) was used for depression assessment. The scores of this scale ranged from 0 to 52.[10,11] Acquiring scores between 0 and 7 classified as normal and subjects who give scores 20 or higher than categorized as depression and higher scores had been showed the severity of depressive symptoms are moderate, severe, or very severe.[12] Validity and reliability of this scale was reported between 0.91 and 0.94[13] and 0.74,[14] respectively. HDRS was used before the onset of trial and after the end of sessions 2, 4, 6, and 8 ECT. Participants filled the informed consent and ethics committee of Arak University of medical sciences approved the trial protocol. Moreover, this trial is registered in Iranian register clinical trial center by IRCT2015013012642N13 number. Chi-square test, trend test, and analysis of variance for repeated measure were used for statistical analysis. Data analyzed in SPSS (IBM Corp, Armonk, NY) software and a significant level considered in 0.05.
RESULTS
The mean and standard deviation of systolic and diastolic blood pressure was 120.6 ± 13.7 and 75.2 ± 8.9 mm/g, respectively. 53.5% (86/160) of participants were female, and this rate was equal in two groups (P > 0.05). In addition, no difference observed in age groups, education level, gender, blood pressure, history of previous ECT, duration of current major depression, age of onset major depression, cigar smoking, and birth in rural area at baseline measurement [Table 1].
Table 1.
The baseline measurement of two studied groups based on demographic and depression characteristics
| Variables | Ketamine | Sodium thiopental | P |
|---|---|---|---|
| Age groups | |||
| 20-29 | 23 (29.5) | 21 (28) | 0.425 |
| 30-39 | 28 (35.9) | 19 (25.3) | |
| 40-49 | 14 (17.9) | 18 (24) | |
| 50-59 | 13 (16.7) | 17 (22.7) | |
| Female sex | 43 (53.8) | 43 (53.8) | 0.563 |
| Education level | |||
| Under diploma | 32 (40) | 35 (43.8) | 0.743 |
| Diploma | 28 (35) | 21 (26.2) | |
| College | 20 (25) | 24 (30) | |
| Lived in rural area | 18 (23.1) | 17 (21.2) | 0.466 |
| Cigar smoking | 20 (25) | 27 (33.8) | 0.271 |
| Age of onset major depression | |||
| Lower 20 | 17 (21.8) | 16 (20) | 0.969 |
| 20-29 | 29 (37.2) | 31 (38.8) | |
| 30-39 | 20 (25.6) | 19 (23.8) | |
| 40 and higher | 15 (15.4) | 14 (17.5) | |
| Duration of current major depression | |||
| Lower 2 years | 23 (28.8) | 25 (31.2) | 0.879 |
| 2-2.9 | 15 (18.8) | 18 (22.5) | |
| 3-3.9 | 18 (22.5) | 16 (20) | |
| 4 and higher | 24 (30) | 21 (26.2) | |
| No history of the previous ECT | 62 (77.5) | 50 (62.5) | 0.116 |
| Diastolic blood pressure | 75.8±9.1 | 74.6±8.7 | 0.374 |
| Systolic blood pressure | 121.6±14.6 | 119.6±12.8 | 0.400 |
ECT: Electroconvulsive therapy
As showed in Table 2, there was a significant difference in side effects of ECT including to a headache, nausea, and fear with the illusion of awakenings between groups in most of the sessions (P < 0.05). Pain in the injection site and short-term delirium were not significantly different between groups at all sessions (P > 0.05). In addition, long-term delirium was not significantly different in most of the sessions (except in 6th sessions) (P > 0.05). Moreover, the findings depicted in Table 3 showed that the systolic and diastolic blood pressure have statistically significant difference in all sessions between ketamine and sodium thiopental after ECT, but there was not observe significant trend in each medication. Both medications had a significant impact on the amount of electrical energy usage and seizure duration overall. The difference in energy usage and seizure duration was not significant between two medication (P > 0.05) except in session 4 for seizure duration (P = 0.002). Moreover, the overall trend of energy usage and seizure duration was significant in two groups (P < 0.05). There was an increasing significant trend in energy usage and a decreasing trend in seizure duration in both medications. However, the complication is lower in sodium thiopental group than ketamine group.
Table 2.
Comparing the rate of complication including headache, nausea, pain in injection site, fear with illusion of awakenings, short and long-term delirium after ECT between two groups
| Complication | Session | Ketamine | Sodium thiopental | P |
|---|---|---|---|---|
| Headache | 1 | 51 (63.8) | 37 (46.2) | 0.019 |
| 2 | 54 (67.5) | 38 (47.5) | 0.008 | |
| 4 | 51 (63.8) | 36 (45) | 0.013 | |
| 6 | 48 (60) | 32 (40) | 0.009 | |
| 8 | 49 (61.2) | 29 (36.2) | 0.001 | |
| Trend test | ||||
| Nausea | 1 | 37 (46.2) | 25 (31.2) | 0.037 |
| 2 | 32 (40) | 24 (30) | 0.123 | |
| 4 | 29 (36.2) | 16 (20) | 0.017 | |
| 6 | 26 (32.5) | 11 (13.8) | 0.004 | |
| 8 | 29 (36.2) | 12 (15) | 0.002 | |
| Pain in injection site | 1 | 11 (13) | 5 (6.2) | 0.093 |
| 2 | 5 (6.2) | 5 (6.2) | 0.627 | |
| 4 | 4 (5) | 2 (2.5) | 0.341 | |
| 6 | 5 (6.2) | 1 (1.2) | 0.105 | |
| 8 | 5 (6.2) | 1 (1.2) | 0.105 | |
| Fear with illusion of awakenings | 1 | 48 (60) | 33 (41.2) | 0.013 |
| 2 | 42 (52.5) | 32 (40) | 0.077 | |
| 4 | 32 (40) | 18 (22.5) | 0.013 | |
| 6 | 32 (40) | 18 (22.5) | 0.013 | |
| 8 | 31 (38.8) | 14 (17.5) | 0.002 | |
| Short-term delirium | 1 | 69 (86.2) | 66 (82.5) | 0.332 |
| 2 | 74 (88.8) | 66 (82.5) | 0.184 | |
| 4 | 68 (85) | 66 (82.5) | 0.415 | |
| 6 | 64 (80) | 68 (85) | 0.267 | |
| 8 | 66 (82.5) | 66 (82.5) | 0.582 | |
| Long-term delirium | 1 | 52 (65) | 49 (61.2) | 0.372 |
| 2 | 50 (62.5) | 46 (57.5) | 0.314 | |
| 4 | 48 (60) | 40 (50) | 0.133 | |
| 6 | 51 (63.8) | 37 (46.2) | 0.019 | |
| 8 | 49 (61.2) | 38 (47.5) | 0.056 |
ECT: Electroconvulsive therapy
Table 3.
Comparing the rate of complication including systolic and diastolic blood pressure, the rate of used energy and seizer duration after ECT between two groups
| Session | Ketamine | Sodium thiopental | P |
|---|---|---|---|
| Systolic blood pressure | |||
| 1 | 184.4±26.1 | 168.3±19.2 | <0.001 |
| 2 | 189.5±26.3 | 171.2±19.1 | <0.001 |
| 4 | 185.7±20.7 | 169.1±22.1 | <0.001 |
| 6 | 189.1±22.1 | 170±20.9 | <0.001 |
| 8 | 187.2±20 | 171±17.7 | <0.001 |
| Repeated measure P value | 0.416 | 0.834 | |
| Diastolic blood pressure | |||
| 1 | 99.5±16.4 | 91.1±16.2 | 0.001 |
| 2 | 99.9±13.1 | 91.6±14.2 | <0.001 |
| 4 | 100.1±12.2 | 92±15.6 | <0.001 |
| 6 | 100.1±13.5 | 90.4±14.1 | <0.001 |
| 8 | 99.9±13.3 | 92.2±16 | 0.001 |
| Repeated measure P value | 0.846 | 0.790 | |
| Duration of seizure | |||
| 1 | 37.9±10.2 | 35.2±12.4 | 0.141 |
| 2 | 36.2±10.8 | 34.9±8.8 | 0.393 |
| 4 | 35.7±8.6 | 31.8±7.2 | 0.002 |
| 6 | 35.4±10.3 | 33.6±9.6 | 0.262 |
| 8 | 34.8±7.9 | 29.8±7.3 | 0.057 |
| Repeated measure P value | 0.023 | 0.020 | |
| Used energy | |||
| 1 | 43±8.8 | 42.2±9.4 | 0.591 |
| 2 | 44.9±8.2 | 45.1±8.6 | 0.844 |
| 4 | 49.7±10.1 | 50.6±11 | 0.627 |
| 6 | 52.2±12.4 | 55.5±13.8 | 0.113 |
| 8 | 53.4±11.8 | 56±14.6 | 0.219 |
| Repeated measure P value | <0.001 | <0.001 |
ECT: Electroconvulsive therapy
According to the Table 4, the Mauchly's test of sphericity was significant, and the HDSR score was showed a significant decreasing trend in both groups that indicates the good effect of medications. (P < 0.001) Also, this trend was significantly different between two groups (P = 0.049) [Figure 1]. In the other hand, the effect of ketamine was more rapid in the recovery from major depression. Nevertheless, the difference in mean depression score in each session was not significant except in session 8 (P = 0.2).
Table 4.
Comparing the mean±SD of HDRS score between ketamine and sodium thiopental groups after ECT
| Session | Ketamine | Sodium thiopental | P* |
|---|---|---|---|
| HDRS score | |||
| 1 | 29.82±7.3 | 28.86±7.6 | 0.442 |
| 2 | 29.34±7.45 | 21.89±6.8 | 0.279 |
| 4 | 15.43±6.16 | 17.73±8.33 | 0.061 |
| 6 | 12.06±6.41 | 13.44±8.48 | 0.270 |
| 8 | 8.32±5.17 | 10.53±7.87 | 0.047 |
*T-test. SD: Standard deviation, HDRS: Hamilton depression rating scale, ECT: Electroconvulsive therapy
Figure 1.
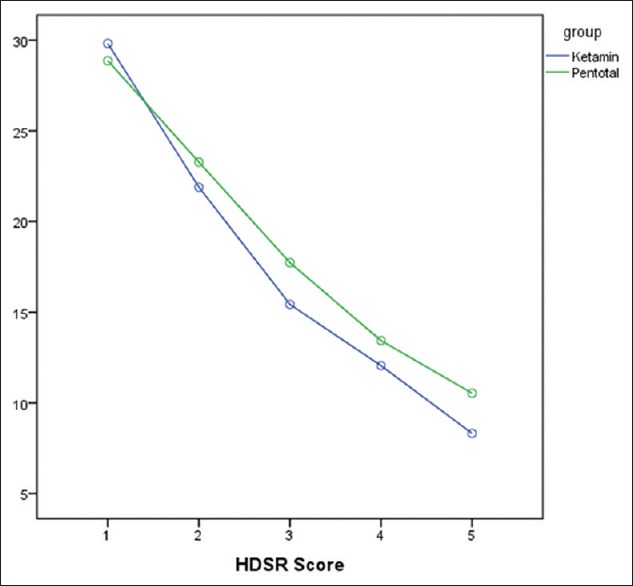
The trend of decreasing in Hamilton depression rating scale score between ketamine and sodium thiopental groups after electroconvulsive therapy
DISCUSSION
The findings in our study showed that the depression score have been decreased after every ECT session in two anesthetic agents. Although the side effects were more common in ketamine group but the groups were not significantly different based on pain in injection site, short- and long-term delirium, duration of seizure, and usage of energy. Ketamine was more effective in decreasing the depression score and increasing systolic and diastolic blood pressure than sodium thiopental. In addition, both groups had significant decreasing trend on seizure duration at different sessions. Nevertheless, the seizure duration was higher in ketamine group. Barkhori et al. showed that ketamine had significant effect in seizure duration, decrease in depression score, and rapid effect in comparison to sodium thiopental,[15] which is consistent with our study. The same results were obtained in Ibrahim et al. study.[16] In addition, different studies have demonstrated the rapid impact of ketamine on reduction of depression scores.[17,18,19,20,21] Yaraghi et al. reported that ketamine will increase blood pressure, seizure duration, and recovery time significantly compared to sodium thiopental.[22] Although, this study is similar to our results but ketamine intervention was related with shorter seizure duration. Nevertheless, another study compared the anesthetic induction effect of thiopental and ketamine in incidence of emergence agitation after pediatric surgery and showed that these two drugs have similar results.[23] However, based on the acquired results some complication such as headache, nausea, and fear with illusion of awakenings was higher in ketamine group. Nevertheless, other side effects were not statistically significant between two groups. Therefore, due to higher impact of ketamine versus sodium thiopental on decreasing of HDRS and recovery of major depression patients, ketamine is more appropriate for anesthesia in ECT in depressive patients which need to anesthesia in ECT. Another study suggested that due to rapid onset and maintenance of improvement after IV ketamine is effective in decreasing suicidality in acutely suicidal depressed patients.[24]
CONCLUSION
Finally, because of more increase in seizure duration in ECT session, we recommend ketamine for inducing anesthesia before ECT in DRMD patients. Also, recommend that future studies compare the effect of ketamine with other anesthetics suitable for ECT in DRMD cases. Because many studies have shown that depressed patients suffer from cognitive deficits, such as impaired memory, it is better that future studies evaluate the effectiveness of ketamine and sodium thiopental on cognitive deficits such as memory impairment.
Financial support and sponsorship
Arak University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, et al. The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289:3095–105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 2.Sadock BJ, Sadock VA, Ruiz P, Kaplan HI. Nine edition. Philadelphia, Lippincott: Williams and walking's publication; 2009. Kaplan and Sadock's Comprehensive Textbook of Psychiatry; pp. 3285–301. [Google Scholar]
- 3.Bayati A, Beigi M, Salehi M. Depression prevalence and related factors in Iranian students. Pak J Biol Sci. 2009;12:1371–5. doi: 10.3923/pjbs.2009.1371.1375. [DOI] [PubMed] [Google Scholar]
- 4.Kenny MA, Williams JM. Treatment-resistant depressed patients show a good response to Mindfulness-based Cognitive Therapy. Behav Res Ther. 2007;45:617–25. doi: 10.1016/j.brat.2006.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reddy PS, Roberts N. Electroconvulsive therapy. Can J Psychiatry. 2015;60:35–6. [Google Scholar]
- 6.McDaniel WW, Sahota AK, Vyas BV, Laguerta N, Hategan L, Oswald J. Ketamine appears associated with better word recall than etomidate after a course of 6 electroconvulsive therapies. J ECT. 2006;22:103–6. doi: 10.1097/00124509-200606000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Folk JW, Kellner CH, Beale MD, Conroy JM, Duc TA. Anesthesia for electroconvulsive therapy: A review. J ECT. 2000;16:157–70. doi: 10.1097/00124509-200006000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Hoyer C, Kranaster L, Janke C, Sartorius A. Impact of the anesthetic agents ketamine, etomidate, thiopental, and propofol on seizure parameters and seizure quality in electroconvulsive therapy: A retrospective study. Eur Arch Psychiatry Clin Neurosci. 2014;264:255–61. doi: 10.1007/s00406-013-0420-5. [DOI] [PubMed] [Google Scholar]
- 9.Abdollahi MH, Izadi A, Hajiesmaeili MR, Ghanizadeh A, Dastjerdi G, Hosseini HA, et al. Effect of etomidate versus thiopental on major depressive disorder in electroconvulsive therapy, a randomized double-blind controlled clinical trial. J ECT. 2012;28:10–3. doi: 10.1097/YCT.0b013e31822a6b8e. [DOI] [PubMed] [Google Scholar]
- 10.Leentjens AF, Verhey FR, Lousberg R, Spitsbergen H, Wilmink FW. The validity of the Hamilton and Montgomery-Asberg depression rating scales as screening and diagnostic tools for depression in Parkinson's disease. Int J Geriatr Psychiatry. 2000;15:644–9. doi: 10.1002/1099-1166(200007)15:7<644::aid-gps167>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 11.Naarding P, Leentjens AF, van Kooten F, Verhey FR. Disease-specific properties of the Rating Scale for Depression in patients with stroke, Alzheimer's dementia, and Parkinson's disease. J Neuropsychiatry Clin Neurosci. 2002;14:329–34. doi: 10.1176/jnp.14.3.329. [DOI] [PubMed] [Google Scholar]
- 12.Khodai S, Dastgerdi R, Haghighi F, Sadatjoo SA, Keramati A. The effect of cognitive – Behavioral group therapy on depression in patients with cancer. J Birjand Univ Med Sci. 2011;18:183–90. [Google Scholar]
- 13.Reynolds WM, Kobak KA. Reliability and validity of the Hamilton depression inventory: A paper-and-pencil version of the Hamilton depression rating scale clinical interview. Psychol Assess. 1995;7:472–83. [Google Scholar]
- 14.Todorova K, Velikova V. The validity of the Hamilton depression rating scale as a screening and diagnostic instrument for depression in patients with epilepsy. J IMAB. 2012;18:3. [Google Scholar]
- 15.Barkhori A, Haghbin MA, Banazade N, Birjandi B. Comparison of two anesthetic induction methods: Ketamin and thiopental Na for ECT in major depression disorder patients. J Birjand Univ Med Sci. 2014;21:20–6. [Google Scholar]
- 16.Ibrahim L, Diazgranados N, Luckenbaugh DA, Machado-Vieira R, Baumann J, Mallinger AG, et al. Rapid decrease in depressive symptoms with an N-methyl-d-aspartate antagonist in ECT-resistant major depression. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35:1155–9. doi: 10.1016/j.pnpbp.2011.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Murrough JW, Perez AM, Pillemer S, Stern J, Parides MK, aan het Rot M, et al. Rapid and longer-term antidepressant effects of repeated ketamine infusions in treatment-resistant major depression. Biol Psychiatry. 2013;74:250–6. doi: 10.1016/j.biopsych.2012.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.aan het Rot M, Collins KA, Murrough JW, Perez AM, Reich DL, Charney DS, et al. Safety and efficacy of repeated-dose intravenous ketamine for treatment-resistant depression. Biol Psychiatry. 2010;67:139–45. doi: 10.1016/j.biopsych.2009.08.038. [DOI] [PubMed] [Google Scholar]
- 19.Kheirkhah F, Moghadamnia A, Tayebi G, Bijani A, Tayebi P, Salavati A. Effect of ketamine in the treatment of patients with major depressive disorder. J Babol Univ Med Sci. 2010;12:14–20. [Google Scholar]
- 20.Okamoto N, Nakai T, Sakamoto K, Nagafusa Y, Higuchi T, Nishikawa T. Rapid antidepressant effect of ketamine anesthesia during electroconvulsive therapy of treatment-resistant depression: Comparing ketamine and propofol anesthesia. J ECT. 2010;26:223–7. doi: 10.1097/YCT.0b013e3181c3b0aa. [DOI] [PubMed] [Google Scholar]
- 21.Zarate CA, Jr, Singh JB, Carlson PJ, Brutsche NE, Ameli R, Luckenbaugh DA, et al. A randomized trial of an N-methyl-D-aspartate antagonist in treatment-resistant major depression. Arch Gen Psychiatry. 2006;63:856–64. doi: 10.1001/archpsyc.63.8.856. [DOI] [PubMed] [Google Scholar]
- 22.Yaraghi A, Soltani H, Hashemi S, Razavi M, Barakatin M, Solimani B. A comparative study on the effects of thiopental and ketamine, in patients under electroconvulsive therapy. J Shahrekord Univ Med Sci. 2009;10:8–15. [Google Scholar]
- 23.Jung HJ, Kim JB, Im KS, Oh SH, Lee JM. Effect of ketamine versus thiopental sodium anesthetic induction and a small dose of fentanyl on emergence agitation after sevoflurane anesthesia in children undergoing brief ophthalmic surgery. Korean J Anesthesiol. 2010;58:148–52. doi: 10.4097/kjae.2010.58.2.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Price RB, Nock MK, Charney DS, Mathew SJ. Effects of intravenous ketamine on explicit and implicit measures of suicidality in treatment-resistant depression. Biol Psychiatry. 2009;66:522–6. doi: 10.1016/j.biopsych.2009.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]


