Abstract
Objective:
To study the distribution of weight for age standard score (Z score) in pediatric cardiac surgery and its effect on in-hospital mortality.
Introduction:
WHO recommends Standard Score (Z score) to quantify and describe anthropometric data. The distribution of weight for age Z score and its effect on mortality in congenital heart surgery has not been studied.
Methods:
All patients of younger than 5 years who underwent cardiac surgery from July 2007 to June 2013, under single surgical unit at our institute were enrolled. Z score for weight for age was calculated. Patients were classified according to Z score and mortality across the classes was compared. Discrimination and calibration of the for Z score model was assessed. Improvement in predictability of mortality after addition of Z score to Aristotle Comprehensive Complexity (ACC) score was analyzed.
Results:
The median Z score was -3.2 (Interquartile range -4.24 to -1.91] with weight (mean±SD) of 8.4 ± 3.38 kg. Overall mortality was 11.5%. 71% and 52.59% of patients had Z score < -2 and < -3 respectively. Lower Z score classes were associated with progressively increasing mortality. Z score as continuous variable was associated with O.R. of 0.622 (95% CI- 0.527 to 0.733, P < 0.0001) for in-hospital mortality and remained significant predictor even after adjusting for age, gender, bypass duration and ACC score. Addition of Z score to ACC score improved its predictability for in-hosptial mortality (δC - 0.0661 [95% CI - 0.017 to 0.0595, P = 0.0169], IDI- 3.83% [95% CI - 0.017 to 0.0595, P = 0.00042]).
Conclusion:
Z scores were lower in our cohort and were associated with in-hospital mortality. Addition of Z score to ACC score significantly improves predictive ability for in-hospital mortality.
Keywords: Aristotle comprehensive complexity score, Congenital heart surgery, Weight-for-age, Z score
INTRODUCTION
Low body weight, which is prevalent in congenital heart disease (CHD) patients, has been associated with worse outcomes after pediatric cardiac surgery.[1,2,3] Low body weight can either be low absolute weight which is adequate for age or low weight-for-age. Low weight-for-age, a manifestation of malnutrition, is important in developing countries where patients present late. Nutritional deficiency, recurrent infections, etc., contribute to malnutrition.[2,4] Though the effect of low body weight has been analyzed in CHD population, the effect of low weight-for-age has not been studied.
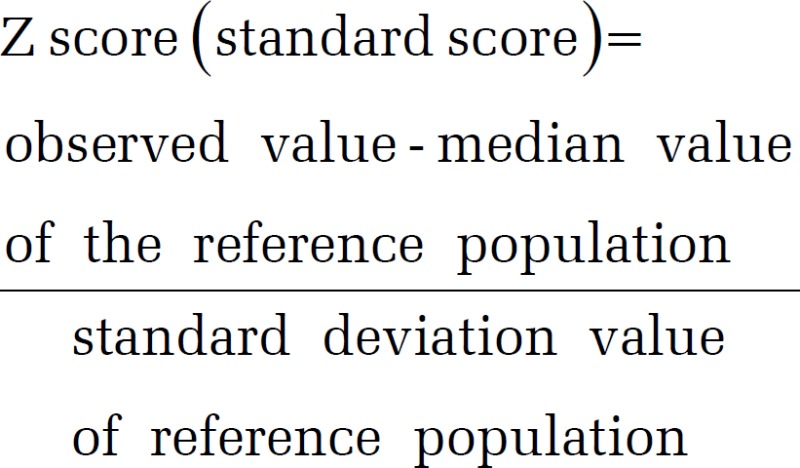
WHO recommends the use of Z (standard) score to describe weight-for-age. The Z score system expresses weight-for-age as the number of standard deviations or Z score below or above the reference mean or median value. Thus, a Z score of −2, indicates weight-for-age which is 2 standard deviations below the reference mean and corresponds to 2.3rd percentile.[5]
Z scores (in contrast to percentiles) can quantify extreme values, are gender-independent, and allows comparison across age-groups and populations.[5,6,7] WHO recommends using -2 Z (2.3rd percentile) scores for diagnosis of underweight and -3 Z (0.1 percentile) for the diagnosis of severe underweight.[5]
Aristotle comprehensive complexity (ACC) score predicts outcome after pediatric cardiac surgeries and has been validated in multiple populations.[8,9,10] It takes into account procedure-related and procedure-independent factors. Body weight of <2.5 kg is taken as a procedure independent complexity factor and scored accordingly. Thus, ACC score takes into account the absolute weight of 2.5 kg as a cutoff and fails to consider weight-for-age.[8] In Indian population ACC score has been found to have less than acceptable discrimination.[9,11]
This study was conducted to study the distribution of weight-for-age Z score (hereafter mentioned as Z score), its association to mortality and improvement of ACC model with addition of Z score to predict mortality, in Indian cardiac surgical population below 5 years.
MATERIALS AND METHODS
This was a single center, retrospective, observational study. Institutional Ethical Committee approval was obtained. All patients of younger than 5 years who underwent cardiac surgery for CHD, from July 2007 to June 2013, under single surgical unit at our institute were enrolled. Data regarding age, gender, weight, diagnosis, procedure, CPB time were collected from hospital records, and ACC scores were calculated.[8] Patients with incomplete data were excluded.
Z score was calculated for individual patient using WHO Anthro software version 3.2.2, January 2011, (World Health Organization, Geneva, Switzerland) available from http://www.who.int/childgrowth/en. It is developed for monitoring growth in individuals of 0-60 months based on WHO Child Growth Standards (WHO CGS). This represents the optimum growth of babies and is derived from WHO Multicentre Growth Reference Study, which included 8500 children, from 6 countries belonging to different regions including India.
The primary outcome was in-hospital mortality defined as all-cause mortality in same hospital admission as CHD surgery.
Data analysis
Descriptive data are summarized in Table 1. Continuous data are summarized as mean and standard deviation or median with interquartile range (IQR). The cohort was divided into 10 categories on the basis of Z score and mortality in each category was analyzed [Table 2]. Prevalence of underweight (Z <−2) and severely underweight (Z <−3) was noted. Two-sided P ≤ 0.05 was considered significant. Mortality across the categories was compared with Chi-square test. ACC score across categories was compared using analysis of variance. Stepwise logistic regression was to describe the association of Z score (as a continuous variable) to mortality before and after adjusting for the ACC score and other variables. Logistic regression was used to find the effect of increasing Z score (categorical variable) on mortality before and after adjusting for ACC score. The Z score classes were compared against a reference group with Z score >−0.9 and OR were calculated from a binary logistic regression model. Discrimination and calibration of the ACC model were assessed using C statistic and Hosmer–Lemeshow test, respectively. Improvement in C statistic and Reclassification Indices were used to compare the improvement in the predictability of ACC score for mortality with the addition of Z score. Increase in sensitivity and specificity was calculated from Reclassification tables. Reclassification Indices were calculated using improve improveProb function from Hmisc (Harrel Miscellaneous) package (version 3.14-6) authored by Frank E. Harrell Jr. for R for Windows (version 3.1.2) (The R Foundation for Statistical Computing, Vienna, Austria). Statistical analysis was performed with Statistical Package for Social Sciences (SPSS) version 16.0.0 for Windows (SPSS Inc., Chicago, USA).
Table 1.
Descriptive data for whole cohort
| Variable | Minimum | Maximum | Mean | SD |
|---|---|---|---|---|
| Age (months) | 0.33 | 60 | 21.44 | 15.12 |
| Weight (kg) | 1.25 | 31 | 8.4 | 3.38 |
| Z score | −7.1 | 4.08 | −3.06 | 1.67 |
| CPB time (min) | 16 | 276 | 82.2 | 35.66 |
| Variable | Minimum | Maximum | Mean | IQR |
| ACC score | 3 | 14 | 8 | 6-8.25 |
| Z score | −7.1 | 4.08 | −3.2 | −4.24 - −1.91 |
| Variable | Number | Percentage | ||
| Females | 347 | 49.7 | ||
| Deaths | 80 | 11.5 | ||
| Cyanotic CHD | 195 | 28 | ||
| CPB | 609 | 87.5 | ||
| Severe pulmonary hypertension | 282 | 40.5 | ||
IQR: Inter quartile range, CPB: Cardiopulmonary bypass, ACC score: Aristotle comprehensive complexity score, CHD: Congenital heart defects, SD: Standard deviation
Table 2.
Distribution according to Z scores
| Z score | P | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ≤ - 6 | −5 to −5.9 | −4 to −4.9 | −3 to −3.9 | −2 to −2.9 | −1 to −1.9 | 0 to −0.9 | 0 to 0.9 | 1 to 1.9 | 2 to 2.9 | ≥3 | |||||||||||||
| n | Percentage in category | n | Percentage in category | n | Percentage in category | n | Percentage in category | n | Percentage in category | n | Percentage in category | n | Percentage in category | n | Percentage in category | n | Percentage in category | n | Percentage in category | n | Percentage in category | ||
| Total | 18 | 58 | 117 | 173 | 133 | 117 | 51 | 10 | 10 | 4 | 5 | ||||||||||||
| Deaths | 6 | 33.3 | 15 | 25.9 | 17 | 13.4 | 24 | 13.9 | 12 | 9 | 4 | 3.4 | 2 | 3.9 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.0001 |
| Median | IQR | Median | IQR | Median | IQR | Median | IQR | Median | IQR | Median | IQR | Median | IQR | Median | IQR | Median | IQR | Median | IQR | Median | IQR | ||
| ACC score | 8 | 5.8-9 | 8 | 8-11 | 8 | 6.3-8 | 8 | 6.225-8.5 | 8 | 6.3-8.5 | 8 | 6-8 | 8 | 6-8.5 | 6 | 5-8 | 6 | 5-8 | 4 | 3-5 | 6 | 3-8 | |
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||
| 7.839 | 2.4765 | 8.347 | 2.4786 | 7.772 | 2.0025 | 7.697 | 1.9986 | 7.558 | 1.9978 | 6.682 | 1.9001 | 7.475 | 1.8987 | 6.05 | 1.7 | 6.05 | 1.707 | 4 | 1.1547 | 5.6 | 2.51 | 0.00 | |
IQR: Interquartile range, SD: Standard deviation, ACC score: Aristotle comprehensive complexity score
RESULTS
Total of 774 patients underwent cardiac surgery. 78 patients had to be excluded due to incomplete data. A total of 696 patients were included. Descriptive data are summarized in Table 1. On comparing Z score categories mortality increased across groups with lower (more negative) Z scores. The groups were also different among themselves with respect to ACC scores [Table 2]. 71.69% of our cohort were underweight (Z <−2), and 52.58% were severely underweight (Z <−3). Distribution of mortality and OR (with Z >−2 as reference) for mortality are tabulated [Table 3]. Z score (as a continuous variable) was associated with OR of 0.622 (95% confidence interval [CI] – 0.527-0.733; P < 0.0001) for mortality. OR was 0.6 (0.490–0.73; P < 0.0001) after controlling for ACC score, age, cyanotic CHD, pulmonary hypertension, gender, and cardiopulmonary bypass. Lower Z scores had higher OR compared to the reference group, and relationship remained similar even after adjusting for ACC score [Table 4].
Table 3.
Comparison according WHO cut-off for underweight
| Variable | Percentage of mortality | OR | 95% CI | P |
|---|---|---|---|---|
| Normal weight | 3.2 | |||
| Underweight (Z ≤ −2) | 9.0 | 2.99 | 1.09-8.08 | 0.03 |
| Severe underweight (Z ≤ −3) | 16.5 | 5.95 | 2.52-14.04 | <0.0001 |
OR: Odds ratio, CI: Confidence interval
Table 4.
Logistic regression analysis of Z score for mortality
| Unadjusted for ACC score | Adjusted for ACC score | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | |
| >−0.9 (reference category) | ||||||
| < −6 | 17.000 | 3.063-94.363 | 0.001 | 14.349 | 2.509-82.048 | 0.003 |
| < −5 | 11.860 | 2.584-54.447 | 0.001 | 8.467 | 1.808-39.655 | 0.007 |
| < −4 | 5.255 | 1.177-23.456 | 0.030 | 4.364 | 0.967-19.691 | 0.055 |
| < −3 | 5.477 | 1.258-23.836 | 0.023 | 4.662 | 1.061-20.477 | 0.041 |
| < −2 | 3.372 | 0.733-15.512 | 0.119 | 2.939 | 0.633-13.647 | 0.169 |
| < −1 | 1.204 | 0.215-6.747 | 0.833 | 1.333 | 0.236-7.530 | 0.745 |
| ACC | 1.305 | 1.152-1.477 | 0.000 | |||
OR: Odds ratio, CI: Confidence interval, ACC score: Aristotle comprehensive complexity score
Addition of Z score significantly improved the predictability of mortality by ACC score-difference between C statistic of 0.0661 (95% CI - 0.119–0.120; P = 0.0169) [Figure 1] net reclassification index of 49.5% (95% CI - 0.272–0.718, P = 0.000) and integrated discrimination index of 3.83% (95% CI - 0.017–0.0596, P = 0.00042) [Table 5]. Increase in sensitivity and specificity was 3.4 and 0.44%, respectively.
Figure 1.
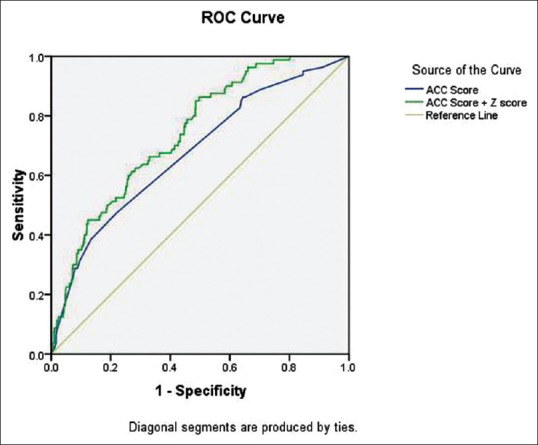
Receiver operating characteristic curve of ACC score and ACC score+Z score model for mortality
Table 5.
Comparison between ACC score and ACC+Z score models
| C statistic | 95% CI | P | H-L test–P | |
|---|---|---|---|---|
| ACC score | 0.676 | 0.640-0.711 | <0.0001 | 0.59 |
| ACC score+Z score | 0.742 | 0.708-0.774 | 0.0269 | 0.269 |
| ACC score versus ACC+Z score | ΔC–0.0661 | 0.0169 | ||
| NRI (continuous)–49.5% | 0.000 | |||
| IDI–3.8 | 0.000 |
NRI: Net Reclassification index, IDI: Integrated discrimination index, ACC score: Aristotle comprehensive complexity score
DISCUSSION
Median Z score in our cohort was −3.2 (IQR - −4.24 to −1.91). 68.82% had Z score <−2 and 52.59% of patients had a Z score <−3. Ramachandran and Gopalan[12] (in rural population) and Khadilkar et al.[13] (in affluent, urban population) studied Z scores according to WHO CGS reference in Indian children. The median Z score was −0.59 and number of underweight patients were 8.5% in Khadilkar et al. and 42.5% in Ramachandran and Gopalan respectively. Thus, compared to general Indian population, our CHD cohort has lower median Z score and higher proportion that are underweight, which is expected.
Vaidyanathan et al. in a study of patients with CHD undergoing interventions at a tertiary center in India noted median Z score of −2.2, 59% underweight and 27.7% severely underweight patients. They used the NCHS/CDC 2000 standard for defining weight-for-age which might have contributed to the variation in results.[14]
Burstein et al. in an analysis of 20992 patients from the STS CHS database described a median Z score of −1.07 (IQR of −2.1 to −0.1) which is much higher than this study.[15]
Other studies in both developing and developed countries describe the similar trend in median Z score and prevalence of underweight.[16,17]
In our cohort, 11.5% of patients had in-hospital mortality. Mortality in normal weight babies (Z < −2) was 3.2%, but increased to 9% in underweight, and 16.5% in severely underweight patients. Compared to normal weight babies, underweight babies had 3 times, and severely underweight babies had 6 times odds of mortality.
Wallace et al. concluded that weight-for-age Z score of <−2 was associated with in-hospital mortality of 3.8% (odds ratio 2.73, 95% CI - 1.09–-6.86), increased risk of Fontan failure and longer length of stay independent of other patient characteristics.[18]
In the series by Anderson et al., patients with Z score <−2 had greater risk of serious perioperative infection (40% in <−2.0 compared to 11.9% in >−2) contributing to increased hospital length of stay.[19]
Higher (more positive) Z score was associated with lower probability of mortality, seen by the OR of 0.622. The decreasing trend of mortality remained true across the Z score categories. Patients with Z <−6 had 3.3% mortality, gradually reducing to 0 in Z > 0 [Table 2]. This was associated with a significantly lower ACC score in higher Z score categories, but even after adjusting for the confounding effect of ACC score and other factors on mortality, Z score had an OR of 0.6.
The inverse association between Z score and mortality is also reflected in the increasing odds for mortality with lower Z score categories compared to the reference group [Table 4].
In this cohort, ACC score had a less than acceptable discrimination for mortality. But the addition of Z score significantly improved its prediction of in-hospital mortality.
Significance of the study
This paper discusses the distribution of Z scores in the Indian congenital cardiac surgical population. The association between lower Z score and mortality is proved not only in normal, underweight and severely underweight categories, but also across all Z score categories. Further, congenital heart surgery scoring systems have failed to take into account the effect of weight-for-age on the outcome. We describe the improvement in the performance of ACC score on the addition of Z score in predicting outcome. This is the first published study which describes the effect of weight-for-age on mortality and improvement of ACC model with the weight-for-age Z score.
Limitations of study
Only in-hospital mortality was considered in our study. The effect on long-term mortality after corrective surgery will vary due to the improvement of malnutrition, and increased weight-for-age Z score, postcorrective surgery. WHO Multicentre Growth Reference Study describes the optimum growth of babies and excluded children with CHD.[5] Thus, it tends to over diagnose undernutrition in CHD, especially from developing countries.[20] But it provides an international reference for malnutrition.
The cause of death (cardiac or noncardiac) was not analyzed.
CONCLUSION
Weight-for-age Z score is lower in our cohort. A lower Z score is associated with in-hospital mortality after CHS.
Addition of Z score to ACC score significantly improves predictive ability for in-hospital mortality.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Ades AM, Dominguez TE, Nicolson SC, Gaynor JW, Spray TL, Wernovsky G, et al. Morbidity and mortality after surgery for congenital cardiac disease in the infant born with low weight. Cardiol Young. 2010;20:8–17. doi: 10.1017/S1047951109991909. [DOI] [PubMed] [Google Scholar]
- 2.Bové T, François K, De Groote K, Suys B, De Wolf D, Verhaaren H, et al. Outcome analysis of major cardiac operations in low weight neonates. Ann Thorac Surg. 2004;78:181–7. doi: 10.1016/j.athoracsur.2003.12.066. [DOI] [PubMed] [Google Scholar]
- 3.Pawade A, Waterson K, Laussen P, Karl TR, Mee RB. Cardiopulmonary bypass in neonates weighing less than 2.5 kg: Analysis of the risk factors for early and late mortality. J Card Surg. 1993;8:1–8. doi: 10.1111/j.1540-8191.1993.tb00570.x. [DOI] [PubMed] [Google Scholar]
- 4.Mehmood A, Ismail SR, Kabbani MS, Abu-Sulaiman RM, Najm HK. Outcome of low body weight (<2.2 kg) infants undergoing cardiac surgery. J Saudi Heart Assoc. 2014;26:132–7. doi: 10.1016/j.jsha.2014.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.de Onis M, Blossner M. WHO Global Database on Child Growth and Malnutrition. World Health Organization. 1997. [Last accessed on 2015 Mar 01]. p. 67. Available from: http://www.whqlibdoc.who.int/hq/1997/WHO_NUT_97.4.pdf . [DOI] [PubMed]
- 6.Khadilkar V, Khadilkar A. Growth charts: A diagnostic tool. Indian J Endocrinol Metab. 2011;15(Suppl 3):S166–71. doi: 10.4103/2230-8210.84854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Seetharaman N, Chacko T, Shankar S, Mathew A. Measuring malnutrition-The role of Z scores and the composite index of anthropometric failure (CIAF) Indian J Community Med. 2007;32:35. [Google Scholar]
- 8.Lacour-Gayet F, Clarke D, Jacobs J, Comas J, Daebritz S, Daenen W, et al. The Aristotle score: A complexity-adjusted method to evaluate surgical results. Eur J Cardiothorac Surg. 2004;25:911–24. doi: 10.1016/j.ejcts.2004.03.027. [DOI] [PubMed] [Google Scholar]
- 9.Joshi SS, Anthony G, Manasa D, Ashwini T, Jagadeesh AM, Borde DP, et al. Predicting mortality after congenital heart surgeries: Evaluation of the Aristotle and Risk Adjustement in Congenital Heart Surgery-1 risk prediction scoring systems: A retrospective single center analysis of 1150 patients. Ann Card Anaesth. 2014;17:266–70. doi: 10.4103/0971-9784.142057. [DOI] [PubMed] [Google Scholar]
- 10.Bojan M, Gerelli S, Gioanni S, Pouard P, Vouhé P. The Aristotle Comprehensive Complexity score predicts mortality and morbidity after congenital heart surgery. Ann Thorac Surg. 2011;91:1214–21. doi: 10.1016/j.athoracsur.2010.10.071. [DOI] [PubMed] [Google Scholar]
- 11.Hosmer DW, Jr, Lemeshow S, Sturdivant RX. 3rd ed. Hoboken, NJ, USA: John Wiley and Sons, Inc; 2013. The Multiple Logistic Regression Model, in Applied Logistic Regression. doi: 10.1002/9781118548387. [Google Scholar]
- 12.Ramachandran P, Gopalan HS. Assessment of nutritional status in Indian preschool children using WHO 2006 Growth Standards. Indian J Med Res. 2011;134:47–53. [PMC free article] [PubMed] [Google Scholar]
- 13.Khadilkar VV, Khadilkar AV, Chiplonkar SA. Growth performance of affluent Indian preschool children: A comparison with the new WHO growth standard. Indian Pediatr. 2010;47:869–72. doi: 10.1007/s13312-010-0147-6. [DOI] [PubMed] [Google Scholar]
- 14.Vaidyanathan B, Radhakrishnan R, Sarala DA, Sundaram KR, Kumar RK. What determines nutritional recovery in malnourished children after correction of congenital heart defects? Pediatrics. 2009;124:e294–9. doi: 10.1542/peds.2009-0141. [DOI] [PubMed] [Google Scholar]
- 15.Burstein DS, Jacobs JP, Li JS, Sheng S, O’Brien SM, Rossi AF, et al. Care models and associated outcomes in congenital heart surgery. Pediatrics. 2011;127:e1482–9. doi: 10.1542/peds.2010-2796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Monteiro FP, de Araujo TL, Lopes MV, Chaves DB, Beltrão BA, Costa AG. Nutritional status of children with congenital heart disease. Rev Lat Am Enfermagem. 2012;20:1024–32. doi: 10.1590/s0104-11692012000600003. [DOI] [PubMed] [Google Scholar]
- 17.Okoromah CA, Ekure EN, Lesi FE, Okunowo WO, Tijani BO, Okeiyi JC. Prevalence, profile and predictors of malnutrition in children with congenital heart defects: A case-control observational study. Arch Dis Child. 2011;96:354–60. doi: 10.1136/adc.2009.176644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wallace MC, Jaggers J, Li JS, Jacobs ML, Jacobs JP, Benjamin DK, et al. Center variation in patient age and weight at Fontan operation and impact on postoperative outcomes. Ann Thorac Surg. 2011;91:1445–52. doi: 10.1016/j.athoracsur.2010.11.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anderson JB, Kalkwarf HJ, Kehl JE, Eghtesady P, Marino BS. Low weight-for-age z-score and infection risk after the Fontan procedure. Ann Thorac Surg. 2011;91:1460–6. doi: 10.1016/j.athoracsur.2011.01.020. [DOI] [PubMed] [Google Scholar]
- 20.Khadilkar V. The growing controversy about growth charts: WHO or regional? Int J Pediatr Endocrinol 2013. 2013;(Suppl 1):6. [Google Scholar]


