Abstract
Context:
Electrical cardioversion is a short painful procedure to regain normal sinus rhythm requiring anaesthesia for haemodynamic stability, sedation, analgesia and early recovery.
Aims:
To compare propofol and etomidate as sedatives during cardioversion.
Settings and Design:
Single centred, prospective and randomized single blind study comprising 60 patients.
Subjects and Methods:
Patients more than 18 years, American Society of Anesthesiologists I/II/III grades undergoing elective cardioversion, randomly divided to receive propofol 1 mg/kg intravenous (IV) bolus followed by 0.5 mg/kg (Group P, n = 30) or etomidate (Group E, n = 30) 0.1 mg/kg followed by 0.05 mg/kg. All patients received IV fentanyl (1 μg/kg) before procedure. Heart rate, blood pressure (BP) (systolic BP [SBP], diastolic BP [DBP], mean arterial pressure), respiratory rate, Aldrete recovery score (ARS) and Ramsay sedation score (RSS) were assessed at 1, 2, 5, 10, 15, 20 and 30 min post cardioversion. Incidence of hypotension, respiratory depression and side effects were compared.
Statistical analysis used:
Student's unpaired t-test, Chi-square test and Mann–Whitney test. P < 0.05 was taken as significant.
Results:
Group P showed significant fall in SBP, DBP, and mean BP at 2 min after cardioversion. Hypotension (33.3% Group P vs. 16.65% Group E) occurred more with propofol (P < 0.05). Group E showed better ARS at 1, 2, 5, 10, 15 and 20 min. Time required to attain RSS = 2 (659.1 s Group P and 435.7 s Group E) indicated longer recovery with propofol. Left atrial size (35.5-42.5 mm) did not affect success rate of cardioversion (80% Group P vs. 83.3% Group E). Incidence of myoclonus (Group E 26.67% vs. Group P 0%) showed significant difference.
Conclusions:
Etomidate/fentanyl is superior over propofol/fentanyl during cardioversion for quick recovery and haemodynamic stability.
Keywords: Cardioversion, Etomidate, Propofol
INTRODUCTION
Cardioversion is a procedure to convert supraventricular tachyarrhythmia (atrial fibrillation being most common) into a normal sinus rhythm, using electric current or drugs. Cardioversion may be performed as an emergency procedure if hemodynamic instability occurs but it may also be done electively. Electrical cardioversion (EC) is a low risk, painful procedure[1] requiring anaesthesia to provide haemodynamic stability (these patients often have a borderline haemodynamics), early recovery without complications. At the same time, success of the procedure should not be affected either.[2,3,4] No standard anaesthetic technique has been described for EC and it requires further clinical research because though etomidate provides hemodynamic stability, even single dose adrenal suppression caused by it still remains a concern[5,6] while use of propofol is associated with hypotension and pain during injection. To our knowledge, this is the first study in Indian population comparing propofol and etomidate during elective cardioversion in terms of effectiveness, safety, complications and to determine whether propofol can be safely used without compromising haemodynamics during cardioversion.
SUBJECTS AND METHODS
After obtaining institutional ethics committee approval and written informed consent from each patient, this prospective, randomized, single blind study included 60 patients of more than 18 years age, belonging to American Society of Anesthesiologists (ASA) I/II/III grade with ejection fraction more than 35% and undergoing elective EC. Pregnant patients and emergency cardioversion were excluded from this study. Post BMV patients in atrial fibrillation formed majority of cases in this study apart from haemodynamically stable supraventricular and monomorphic ventricular tachycardia. Sample size was calculated considering mean change in blood pressure (BP) as primary end point and type 1 error 5% and 80% power. So total 60 patients incorporated in the study and were distributed randomly into two groups each consisting equal number of patients (n = 30) to receive propofol (Group P) or etomidate (Group E) during cardioversion. Computer generated randomization table equally divided patients into two groups by sealed envelope technique.
After confirming adequate starvation, patients were monitored with cardioscope (electrocardiography [ECG]), digital pulse oximeter (SpO2), and noninvasive BP. Supplementary oxygen by nasal prongs was provided to every patient. All the emergency endotracheal intubation equipment and cardiorespiratory drugs were kept ready for resuscitation. In an effort to abolish pain during intravenous (IV) administration of both drugs, all patients received a slow IV injection of 2% injection lignocaine (0.5 mg/kg) 1 min before giving propofol or etomidate. All patients received injection fentanyl (1 μg/kg) IV for analgesia. Group P received propofol (1 mg/kg IV bolus followed by 0.5 mg/kg) and Group E received etomidate, (0.1 mg/kg IV followed by 0.05 mg/kg) to achieve adequate level of sedation (no respose to verbal commands and loss of eyelid reflex) with spontaneous breathing. Haemodynamic variables (heart rate [HR], BP [systolic BP [SBP], diastolic DP [DBP] and mean arterial pressure [MAP]], SpO2, respiratory rate [RR]) and Aldrete recovery score (ARS)[7] were assessed at 1 min, 2 min, 5 min, 10 min, 15 min, 20 min and 30 min post cardioversion. Incidence of hypotension, respiratory depression, nausea, vomiting and myoclonus were compared. In addition to this, time taken to regain consciousness, follow simple commands (corresponding to Ramsay sedation score[8] [RSS = 2] denoting recovery; was also compared. We defined hypotension as more than 20% fall in SBP and respiratory depression was considered when RR <8/min or apnea >10 s occurred.
All patients were monitored and post anaesthesia discharge score (PADS)[7] at 4 h was compared.
Statistical analysis
All raw data were analyzed using IBM SPSS software, United States, Predictive analytics software and solutions (SPSS 16). Descriptive analysis for numerical data consists of mean with standard deviation for various parameters. Categorical data (e.g., sex distribution, ASA status) were analyzed using Pearson's Chi-square test with Yate's correction. Parametrical numerical data between groups were analyzed using Student's t-test. Mann–Whitney U-test was applied for comparing different scores in both groups. P < 0.05 was considered as statistically significant. All analyses were two-tailed.
RESULTS
Patients in both groups were comparable with respect to demographic data such as age, gender, weight and ASA grade [Table 1].
Table 1.
Demographic characteristics
| Parameter | Group P (n=30) | Group E (n=30) | P |
|---|---|---|---|
| Age (years) | 38.233±11.190 | 38.800±11.186 | 0.845 |
| Weight (kg) | 50.967±10.912 | 50.967±12.488 | 1 |
| Gender (male/female) (%) | 12 (40)/18 (60) | 13 (43.3)/17 (56.7) | 0.816 |
| ASA (II/III) | 26/4 | 24/6 | 0.793 |
ASA: American Society of Anesthesiologists
Heart rate decreased in both groups after cardioversion at all time intervals but the difference was insignificant. SBP decreased at all time intervals but significant difference was observed at 2 min (95.33 ± 12.04 Group P vs. 106.13 ± 15.27 mmHg Group E; P = 0.004) and 5 min (98.30 ± 11.64 Group P vs. 105.43 ± 13.81 mmHg Group E; P = 0.035). DBP (Group P 62.87 ± 9.68 vs. Group E 68.90 ± 11.54 mmHg; P = 0.032) and MAP (Group P 74.13 ± 10.06 vs. Group E 81.23 ± 12.21 mmHg; P = 0.017) at 2 min showed significant fall in Group P; although clinically insignificant [Figure 1–4]. Oxygen saturation (SpO2) was comparable in both groups at all times.
Figure 1.
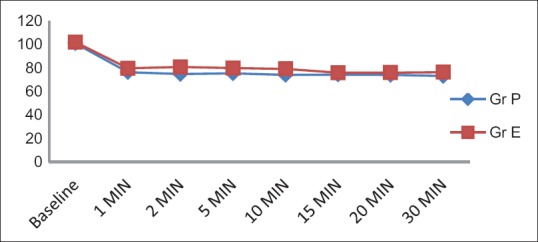
Comparison of heart rate (no difference noted)
Figure 4.
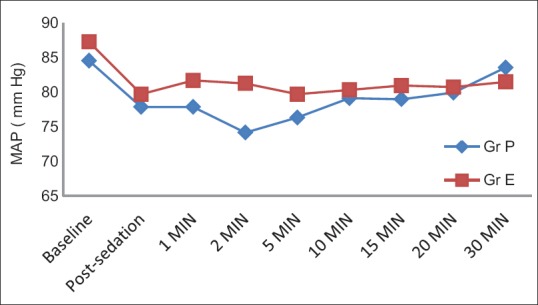
Comparison of mean blood pressure (P = 0.017 at 2 min)
Figure 2.
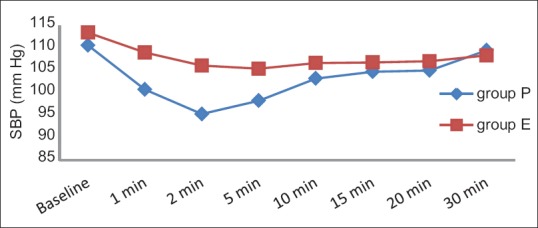
Comparison of systolic blood pressure (P = 0.004 at 2 min; P = 0.035 at 5 min)
Figure 3.
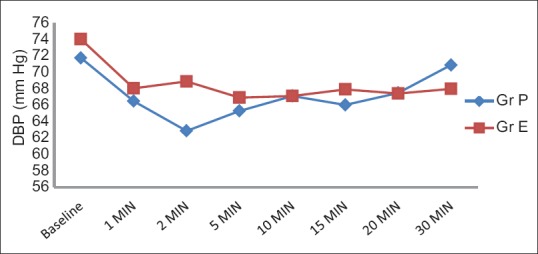
Comparison of diastolic blood pressure (P = 0.032 at 2 min)
Ramsay sedation score was higher in Group E at 1 and 2 min after cardioversion (P = 0.04 at 1 min) but thereafter Group P showed higher RSS at all times denoting early onset and brief duration of etomidate. Time required to achieve RSS = 2 was higher in Group P (659.1 + 150.7 vs. 435.7 + 148.06 seconds, P < 0.001) denoting early recovery with etomidate. ARS showed significant difference at all times; suggesting better recovery profile with etomidate (although clinically insignificant) [Figure 5 and 6].
Figure 5.
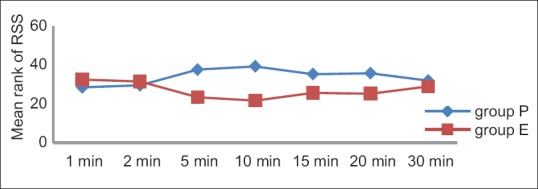
Comparison of Ramsay sedation score (P < 0.05 at 1, 5, 10, 15, 20 min denoting profound sedation with propofol)
Figure 6.
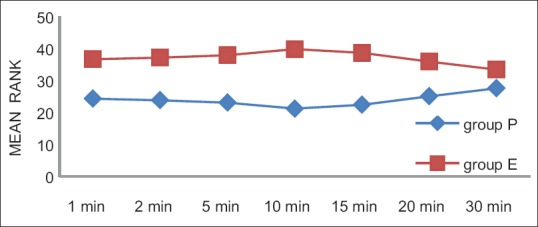
Comparison of Aldrete recovery score (etomidate showing better recovery at all times)
Incidence of hypotension and respiratory depression was higher in Group P (33.3% vs. 16.6%, P = 0.233; 20% vs. 0%, P = 0.024 respectively). None of the patient in Group P had myoclonus (26.6% vs. 0%, P = 0.004). Mean left atrial (LA) size in Group P and E was 35.967 ± 8.74 mm and 42.633 ± 9.40 mm respectively (P = 0.006) but still success rate of cardioversion was comparable in both groups (80% vs. 83.35%; P = 0.739) (Chi-square test).
Also, mean number of shocks required (2.1 + 1.29 vs. 1.9 + 0.88 [P = 0.488]) showed no significant statistical difference.
Post anaesthesia discharge score at 4 h in both groups were comparable (P = 0.72; Mann–Whitney U-test).
None of the patients in the study required resuscitation, inotrops or ventilator support.
DISCUSSION
Cardioversion is a method to restore an abnormal heart rhythm back to normal sinus rhythm using either an electric shock or medications. During electric cardioversion, shock has to be synchronized with the R wave of ECG which avoids the phase of vulnerability of myocardium during cardiac cycle. It is a short, painful procedure[1] requiring sedation, analgesia and early recovery; failing which patient may develop panic attacks and unpleasant memories.[9] Also presence of significant pre-existing cardiac disease as well as involvement of other organ systems makes choice of anaesthetic an important issue before cardioversion. Drugs having a rapid onset and short duration of action with rapid recovery should be selected. At the same time, anaesthetic should not cause hemodynamic disturbances and should be devoid of unwanted side effects without losing airway reflex control. Propofol and etomidate both fulfil majority of these criteria as an ideal anaesthetic agent for cardioversion. Therefore, we decided to compare both these anaesthetics in order to assess their safety and efficacy during cardioversion.
After cardioversion, decreased HR was observed in both groups due to interruption in re-entry circuits after depolarization of a critical mass of myocardium; thus regaining sinus rhythm.[10] We observed greater fall in SBP with propofol at 2 min and 5 min after cardioversion although the degree of fall was clinically insignificant. But then SBP gradually approached towards baseline at 20 and 30 min in both groups. MAP and DBP in propofol group showed statistically significant but clinically insignificant drop at 2 min after cardioversion. Incidence of hypotension in both groups was comparable. Our results were consistent with other similar studies comparing propofol and etomidate.[11,12,13,14] We realized that our doses were rather low and as a result achieved hemodynamic stability in majority of the cases.
Propofol in a dose of 2 mg/kg reduces arterial BP by approximately 40%, mainly due to vasodilatation and potentially enhanced by its direct myocardial depressant effect. Old and sick patients are more prone to profound hypotension when opioid is added.[15] Etomidate neither inhibits sympathetic tone nor impairs myocardial function, even in patients with valvular or ischemic heart disease contributing to stable hemodynamic.[16] But in our study SBP decreased in both groups due to additive effect of fentanyl contributing to deep sedation.
Propofol produced more respiratory events in our study although without any significant effect on SpO2 and none of the patient required intubation. These observations are in concordance to other similar studies.[9,17,18,19]
We found delayed and prolonged sedation with propofol as compared to etomidate but the degree of sedation produced by both drugs was sufficient enough for cardioversion. This can be explained by the fact that the onset time after induction dose of propofol and etomidate is 40 s and 15–30 s, respectively while context sensitive half life for propofol infusion upto 8 hrs is <40 min only.[15]
Aldrete recovery score was significantly better with etomidate at all times after cardioversion denoting faster and clear headed recovery. Time required to achieve RSS = 2 also showed faster recovery with etomidate. Toklu et al.[20] compared recovery time of etomidate-ramifentanyl and propofol-ramifentanyl sedation in patients scheduled for colonoscopy and concluded that etomidate-ramifentanyl administration for sedation and analgesia during colonoscopy resulted in more stable hemodynamic response and shorter recovery and discharge times. An addition of fentanyl to etomidate reduces the required dose of etomidate and allows earlier awakening.[15] Experimental studies have shown conflicting effects on propofol pharmacokinetics when used with fentanyl depending on timing of fentanyl administration before propofol.[15,21] Other similar study found faster recovery with propofol but higher dose of etomidate and absence of fentanyl contributed to this contrary finding.[22] In another study comparing propofol and etomidate, where incremental doses were given but no analgesic agent was given, no difference in recovery times was observed.[17]
We found similar PADS at 4 h after cardioversion suggesting that neither drug delayed discharge of the patients. In another study, there was no residual psychomotor impairment 60 min after anaesthesia in any patient before discharge.[23]
We found only one female patient who developed nausea and vomiting after cardioversion with etomidate that was well controlled with antiemetic. Otherwise none of the patients had nausea and vomiting in our study due to antiemetic effects of propofol itself and low dose of etomidate used in the study. Propofol has anti-emetic properties and studies have shown a lower incidence of postoperative nausea and vomiting (PONV) in patients receiving propofol as induction agent.[24] But it is possible that the number of patients in our study was too few to reliably detect any difference in PONV between the groups. Other studies found more frequent nausea and vomiting during and after anaesthesia in patients who received etomidate.[18,25]
Etomidate is associated with considerably less injection pain in children compared with propofol with added lidocaine.[26] None of our patient experienced pain on injection of either drug because of pretreatment with lignocaine.
We found 26.67% incidence of myoclonus with etomidate against none in propofol group (P = 0.004). The incidence of myoclonus is reported to be 60–80% in non premedicated patients after etomidate injection and has been found to be reduced after pre-administration of fentanyl in a dose dependent manner.[27,28]
None of the patients had intra-procedural recall after cardioversion denoting equivalent amnesia produced by both drugs. In their study, Mitterschiffthaler et al.[29] found more incidence of recall with etomidate as compared to propofol but greater dose of the hypnotic agents without analgesia were used. Swann et al.[30] too, found a low incidence of recall during sedation in emergency department.
Another interesting observation was that although etomidate group had significant (P = 0.006) more LA size than propofol group, success rate of cardioversion (80% in Group P vs. 83.3% in Group E) was comparable between both groups suggesting that probably size of left atrium has no impact on outcome of the procedure but still excessively large left atrium might cause failure to cardiovert.[31]
Overall, etomidate when compared to propofol as sedative agent in patients undergoing cardioversion failed to show significant statistical difference in terms of hypotension after cardioversion. However, recovery time was significantly faster with etomidate but this difference may not be clinically relevant. There was no significant difference in the incidence of nausea and vomiting. So the combination of low-dose fentanyl and etomidate may be a good choice for short procedures where rapid recovery is required and can be a good alternative to propofol in short procedural sedation.
LIMITATIONS
Our study was not double blinded. Although both drugs have milky white appearance; because of the specific nature of dosing, we did not think that double blinding could be safely achieved. So likelihood of preconceived notions about the two agents could have resulted in possible bias. Cost of drug is also an important factor and we did not conduct a cost-effectiveness analysis too.
CONCLUSION
Propofol and etomidate both provide excellent conditions, safety profile and quick recovery for EC. We suggest that in old, sick and critically ill patient etomidate should be preferred over propofol to maintain haemodynamic stability and early recovery. But utmost vigilance is required to tackle complications related to airway. We also conclude that probably LA size is not a determinant for success of electric cardioversion.
ACKNOWLEDGEMENT
We would like to acknowledge cooperation and support of Dr. Madhu Garasia (Professor and Head, Department of Anesthesia) and Dr. Prafulla Kerkar (Professor and Head, Department of Cardiology).
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Clark A, Cotter L. DC cardioversion. Br J Hosp Med. 1991;46:114–5. [PubMed] [Google Scholar]
- 2.Morani G, Bergamini C, Angheben C, Pozzani L, Cicoira M, Tomasi L, et al. General anaesthesia for external electrical cardioversion of atrial fibrillation: Experience of an exclusively cardiological procedural management. Europace. 2010;12:1558–63. doi: 10.1093/europace/euq276. [DOI] [PubMed] [Google Scholar]
- 3.Wood J, Ferguson C. Best evidence topic report. Procedural sedation for cardioversion. Emerg Med J. 2006;23:932–4. doi: 10.1136/emj.2006.043067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hagemeijer F, Van Mechelen R, Smalbraak DW. Fentanyl-etomidate anesthesia for cardioversion. Eur Heart J. 1982;3:155–8. doi: 10.1093/oxfordjournals.eurheartj.a061278. [DOI] [PubMed] [Google Scholar]
- 5.Bruder EA, Ball IM, Ridi S, Pickett W, Hohl C. Single induction dose of etomidate versus other induction agents for endotracheal intubation in critically ill patients. Cochrane Database Syst Rev. 2015;1:CD010225. doi: 10.1002/14651858.CD010225.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chan CM, Mitchell AL, Shorr AF. Etomidate is associated with mortality and adrenal insufficiency in sepsis: A meta-analysis*. Crit Care Med. 2012;40:2945–53. doi: 10.1097/CCM.0b013e31825fec26. [DOI] [PubMed] [Google Scholar]
- 7.Morgan GE, Mikhail M, Murray M. Morgan's Clinical Anaesthesiology. 4th ed. New York: McGraw-Hill Publishers; 2005. Post Anesthesia Care; pp. 1009–10. [Google Scholar]
- 8.Ramsay Sedation Scale. [Last cited on 2004 Nov 16]. Available from: http://www.frca.co.uk/article.aspxarticleid=100192 .
- 9.Kowey PR. The calamity of cardioversion of conscious patients. Am J Cardiol. 1988;61:1106–7. doi: 10.1016/0002-9149(88)90135-x. [DOI] [PubMed] [Google Scholar]
- 10.Zipes DP, Fischer J, King RM, Nicoll A deB, Jolly WW. Termination of ventricular fibrillation in dogs by depolarizing a critical amount of myocardium. Am J Cardiol. 1975;36:37–44. doi: 10.1016/0002-9149(75)90865-6. [DOI] [PubMed] [Google Scholar]
- 11.Miner JR, Danahy M, Moch A, Biros M. Randomized clinical trial of etomidate versus propofol for procedural sedation in the emergency department. Ann Emerg Med. 2007;49:15–22. doi: 10.1016/j.annemergmed.2006.06.042. [DOI] [PubMed] [Google Scholar]
- 12.Kick O, Kessler J, Conradi R, Böhrer H, Motsch J, Martin E, et al. Anesthesia for outpatient cardioversion hypnomidate versus propofol. Anaesthesiology. 1993;70:3A. [Google Scholar]
- 13.Gale DW, Grissom TE, Mirenda JV. Titration of intravenous anesthetics for cardioversion: A comparison of propofol, methohexital, and midazolam. Crit Care Med. 1993;21:1509–13. doi: 10.1097/00003246-199310000-00019. [DOI] [PubMed] [Google Scholar]
- 14.Lechleitner P, Genser N, Mitterschiffthaler G, Dienstl F. Propofol for direct current cardioversion in cardiac risk patients. Eur Heart J. 1991;12:813–7. [PubMed] [Google Scholar]
- 15.Reeves JG, Glass PS, Lubersky DA, McEvoy MD, Ruiz RM. Intravenous anaesthetics. In: Miller RD, editor. Miller's Anaesthesia. USA: Churchill Livingstone Elsevier; 2010. pp. 724-5–748-9. [Google Scholar]
- 16.Forman SA. Clinical and molecular pharmacology of etomidate. Anesthesiology. 2011;114:695–707. doi: 10.1097/ALN.0b013e3181ff72b5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kick O, Böhrer H, Motsch J, Kessler J, Conradi R, Martin E. Etomidate versus propofol for anesthesia in ambulatory cardioversion. Anasthesiol Intensivmed Notfallmed Schmerzther. 1996;31:288–92. doi: 10.1055/s-2007-995922. [DOI] [PubMed] [Google Scholar]
- 18.Calbet A, Zanca A. A randomized clinical trial of propofol or etomidate for elective electrical cardioversion for atrial fibrillation. Eur J Anaesthesiol. 2010;27:91. [Google Scholar]
- 19.Kalogridaki M, Souvatzis X, Mavrakis HE, Kanoupakis EM, Panteli A, Kasotaki S, et al. Anaesthesia for cardioversion: A prospective randomised comparison of propofol and etomidate combined with fentanyl. Hellenic J Cardiol. 2011;52:483–8. [PubMed] [Google Scholar]
- 20.Toklu S, Iyilikci L, Gonen C, Ciftci L, Gunenc F, Sahin E, et al. Comparison of etomidate-remifentanil and propofol-remifentanil sedation in patients scheduled for colonoscopy. Eur J Anaesthesiol. 2009;26:370–6. doi: 10.1097/EJA.0b013e328318c666. [DOI] [PubMed] [Google Scholar]
- 21.Matot I, Neely CF, Katz RY, Marshall BE. Fentanyl and propofol uptake by the lung: Effect of time between injections. Acta Anaesthesiol Scand. 1994;38:711–5. doi: 10.1111/j.1399-6576.1994.tb03982.x. [DOI] [PubMed] [Google Scholar]
- 22.Herregods LL, Bossuyt GP, De Baerdemaeker LE, Moerman AT, Struys MM, Den Blauwen NM, et al. Ambulatory electrical external cardioversion with propofol or etomidate. J Clin Anesth. 2003;15:91–6. doi: 10.1016/s0952-8180(02)00520-2. [DOI] [PubMed] [Google Scholar]
- 23.Pandey AK, Makhija N, Chauhan S, Das S, Kiran U, Bisoi AK, et al. The effects of etomidate and propofol induction on hemodynamic and endocrine response in patients undergoing coronary artery bypass graft surgery on cardiopulmonary bypass. WJCS. 2012;2:48–53. [Google Scholar]
- 24.Stoelting RK, Hillier SC. Nonbarbiturate intravenous anesthetic drugs. In: Stoelting RK, editor. Pharmacology and Physiology in Anaesthetic Practice. 4th ed. Philadelphia, USA: Lippincott Williams and Wilkins; 2006. pp. 155–67. [Google Scholar]
- 25.Siedy J, Knapik P, Saucha W, Gross M. Comparison of propofol and etomidate anaesthesia for elective electrical cardioversion. Kardiol Pol. 2010;68:1249–55. [PubMed] [Google Scholar]
- 26.Nyman Y, Von Hofsten K, Palm C, Eksborg S, Lönnqvist PA. Etomidate-Lipuro is associated with considerably less injection pain in children compared with propofol with added lidocaine. Br J Anaesth. 2006;97:536–9. doi: 10.1093/bja/ael187. [DOI] [PubMed] [Google Scholar]
- 27.Stockham RJ, Stanley TH, Pace NL, Gillmor S, Groen F, Hilkens P. Fentanyl pretreatment modifies anaesthetic induction with etomidate. Anaesth Intensive Care. 1988;16:171–6. doi: 10.1177/0310057X8801600207. [DOI] [PubMed] [Google Scholar]
- 28.Carlos R, Innerarity S. Effect of premedication on etomidate anaesthesia. Br J Anaesth. 1979;51:1159–62. doi: 10.1093/bja/51.12.1159. [DOI] [PubMed] [Google Scholar]
- 29.Mitterschiffthaler G, Lechleitner P, Hauptlorenz S, Wencker M, Dienstl F. Anesthesia for cardioversion. A comparison of propofol and etomidate. Cah Anesthesiol. 1990;38:159–63. [PubMed] [Google Scholar]
- 30.Swann A, Williams J, Fatovich DM. Recall after procedural sedation in the emergency department. Emerg Med J. 2007;24:322–4. doi: 10.1136/emj.2006.040923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Volgman AS, Soble JS, Neumann A, Mukhtar KN, Iftikhar F, Vallesteros A, et al. Effect of left atrial size on recurrence of atrial fibrillation after electrical cardioversion: Atrial dimension versus volume. Am J Card Imaging. 1996;10:261–5. [PubMed] [Google Scholar]


