Abstract
A new Web-based self-management intervention was developed for persons with spinal cord injury who use intermittent urinary catheters. Included are a description of the components, examples from the educational book, and multiple screen shots of the online urinary diary.
Keywords: Self-management, spinal cord injury, Internet, intervention research
Spinal cord injury (SCI) affects the bladder’s storage and emptying, often contributing to persistent urinary retention (National Spinal Cord Injury Statistical Center, 2014). Intermittent catheterization (IC), by which the bladder is drained several times a day, is the preferred bladder management method (Cottenden et al., 2013). While the exact frequency of IC is individualized, people with full retention are ordinarily taught to catheterize four to five times a day or every four to six hours (Cottenden et al., 2013). Learning to manage this procedure takes time, with rehabilitation lengths of stay shorter in recent years (Christopher & Dana Reeve Foundation, 2015; National Spinal Cord Injury Statistical Center, 2014), individuals with SCI must develop skill in the method at the same time they are adjusting to this major life-changing event.
Research reports suggest there are many problems associated with living with IC that can influence the acceptance and continued use of it, including managing the frequency and technique of the procedure (Logan, Shaw, Webber, Samuel, & Broome, 2008; Shaw, Logan, Webber, Broome, & Samuel, 2008; van Achterberg, Holleman, Cobussen-Boekhorst, Arts, & Heesakkers, 2008), impact on sex (Shaw et al., 2008), inconvenience of catheterizing (Wilde, Brasch, & Zhang, 2011), urinary tract infection (Wilde et al., 2011; Woodbury, Hayes, & Askes, 2008), urine leakage, inaccessible bathrooms, and a lack of optimal catheter supplies (Al-Jadid, Al-Asmari, & Al-Moutaery, 2004; Wilde et al., 2011). Thus, managing IC issues can be a daily struggle (Kelly, Spencer, & Barrett, 2014; Logan et al., 2008; Shaw et al., 2008).
Moreover, not being well prepared to incorporate catheterizing into everyday life can lead to the use of a long-term indwelling urinary catheter or non-adherence to optimal IC frequency, which can adversely affect the bladder and kidneys (El-Masri, Chong, Kyriakider, & Wang, 2011). People with SCI, who are often injured while young, need to learn to live with IC as a part of their normal routines. Bladder self-management is integral to engaging in and maintaining social and employment opportunities. Restriction in travel due to urine leakage can interfere with quality of life (Brillhart, 2004) and full employment. Sadly, about 65% of adults with SCI are not employed (Wehman, 2010). Therefore, people using IC need excellent self-management skills, such as learning how to 1) adhere to their IC regime; 2) self-monitor fluid intake to prevent leakage while maintain optimal hydration; 3) notice early symptoms of UTI; 4) perform IC in a variety of situations with good technique; 5) choose most advantageous catheters, supplies, and lubrication; and 6) adapt to social needs (Wilde et al., 2011).
Web-based interventions, which are currently expanding, are likely to continue to be developed and disseminated after testing and proven feasible. All activities in this study were approved by our university department for the protection of human subjects. The sample was diverse by race and ethnicity, and was composed of almost equal numbers of males and females, ranging in age from 22 to 79 years (M = 44, SD = 13.1, Md = 47). The research findings will be reported elsewhere in two other articles related to 1) the development of the web-based intervention (under peer review), and 2) testing its feasibility/usability, with a full description of the sample and procedures (in progress, not submitted yet).
Purpose
A new Web-based intervention for people using intermittent urinary catheterization to empty the bladder periodically throughout the day is a part of a single-group trial funded by the National Institutes of Research/National Institute of Nursing Research to evaluate feasibility of a new web-based approach in 34 individuals with SCI who use IC. This report is expected to provide urological practitioners with information about IC self-management using web-based materials and processes, including use of the tables and figures. However, the authors maintain copyright of the figures and tables, and therefore, the content should not be modified or used without permission of the first author.
Intervention Website
The intervention website includes content on a number of pages: a Home Page, Continence Product Advisor, Commercial Products, Educational Materials, Personal Data, Forum, Contact Us, Help, and Logout. The Home Page is a welcome/introductory page with links across the top menu bar to the other pages. The Continence Product Advisor introduces study participants to a website that is a collaboration between the International Consultation on Incontinence (ICI) and the International Continence Society (ICS) (http://www.continenceproductadvisor.org/) that describes continence products and how they are used. With permission from these website developers, we made a table with links to the sections related to IC products to help people navigate this site. In the Commercial Products section, we provided links to a number of common IC-related products about which people might not have been known, such as catheters attached to a bag for use when going out of the home, and special adaptive aids, like a knee spreader for women and penis holder for men to help with hand dexterity.
The Educational Materials page is linked to the Educational Booklet, which is a 23-page illustrated booklet created by the first author based on a previous self-management program for indwelling catheter users (Wilde et al., 2013, 2015; Wilde & Brasch, 2008). The content was modified using literature and information obtained in the research team’s qualitative study about issues and concerns in IC users (Wilde et al., 2011). After an introduction and description of basic IC self-management (see Table 1), specific topics follow:
Table 1.
Basic Intermittent Catheter Self-Management
| • Stay aware. Using an intermittent catheter requires that you stay aware of your body and how you feel. |
| • Drink more water than any other beverage! Limit coffee, and consider substituting tea and decaffeinated beverages. |
| • Balance fluids with cathing volumes. You may find it helpful to do a two to three-day intake and output diary to know how much you are drinking. While it will vary by individual, drinking more than about 2 liters could cause over-distention of the bladder, but it depends on the type of fluids. Over-distention is a major contributor to urinary tract infection (UTI). You do not need to focus on the amount taken each day as long as your volumes for catheterization do not go over 500 mL. If your volumes are consistently over 500 mL, then you should either drink less or catheterize more frequently. |
| • Pay attention to the color of your urine. It should be light yellow to yellow all day long. The color of urine can be a quick way to know whether you are drinking enough or too much during the day. If the urine color changes, notice if you are doing something different, such as drinking more caffeinated beverages or taking a diuretic medicine or water pill, such as furosemide (Lasix®) or chlorothiazide sodium (Diuril®). |
| • Notice how often you are catheterizing. Most people need to do this four to five times a day, approximately every four to six hours. If you do not do it often enough, you are more susceptible to UTIs or leakage of urine. You should have less than 500 cc. in each catheterization. |
| • Pay attention to how fluids affect your activities, the time between intermittent catheterization (IC), and how the amount and what you drank contribute to urine leakage and accidents. |
| • Consider other catheters. You can try other types of catheters if you wish. Not one catheter will work with all people. Contact your physician after you have considered options. |
| • Prepare for getting out. You may need to learn different positions for cathing or where the bathrooms are. You might need to assemble your own IC kit. |
| • Ask for help. If you need assistance with IC or bathroom access, ask for help. |
Source: Copyright © Mary H. Wilde et al. Used with permission. Content should not be modified or used without permission of the first author.
Balance fluids with activities – optimal fluid intake.
Balance fluids with activities – promote best IC interval.
Negotiate and select catheters and supplies.
Choose best positions for catheterization.
Learn about travel and bathroom issues.
Prevent leaking.
Recognize early symptoms of UTI.
Seek social support.
Make adjustments for sexual activity.
Work with caregivers.
Prevent autonomic dysreflexia.
Manage painful catheterizations.
Decrease caffeine.
Am I dehydrated? (Urine Color Chart).
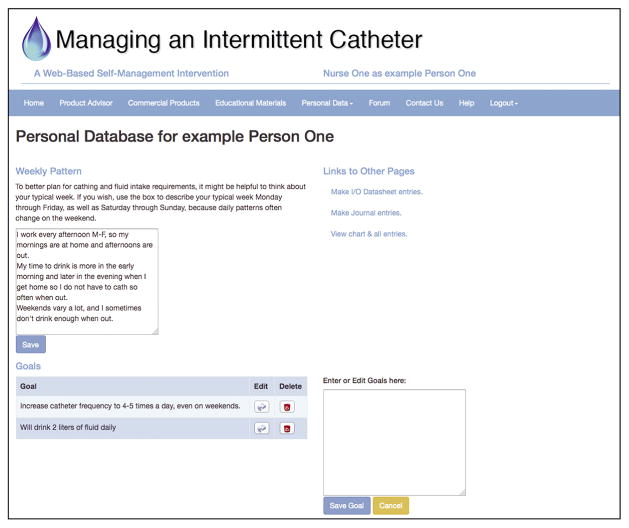
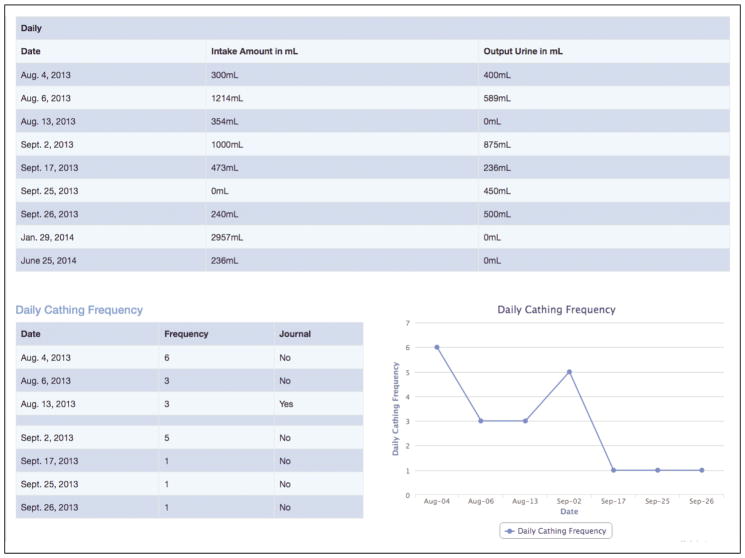
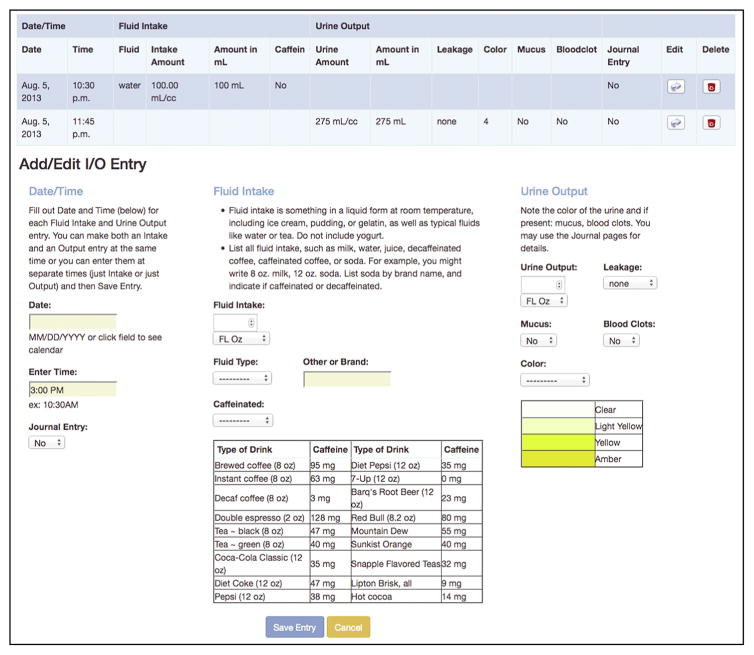
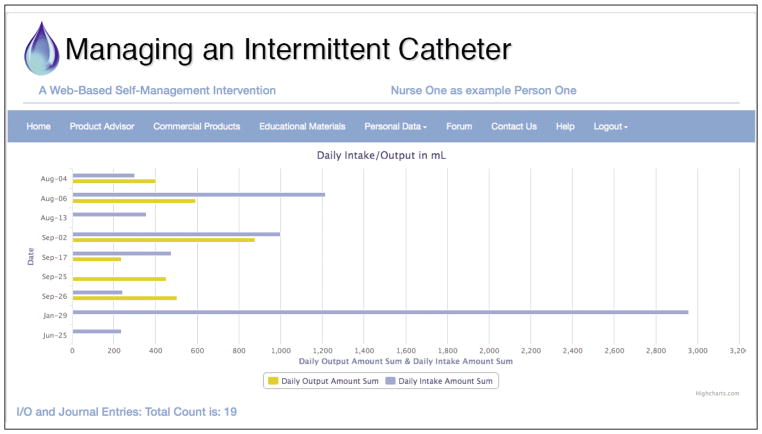
The Personal Data page (viewed only by the study participant and the study nurses) is the most interactive section of the intervention website and involves links to four webpages: goals and catheterization frequency, intake and output (I&O) entries, journal, and an overview with summary tables and graphs (see Figures 1 to 5). The goals and catheterization frequency (see Figure 1) has a textbox for writing, revising, and deleting goals, and places to select a date and frequency of catheterization for that date. The I&O entries (see Figure 2) include options for entering volumes and characteristics. For fluid intake, options are mL/cc, ounces, cup, pint, or quart; type of fluids (such as water, milk, juice, beer, soda); and if the fluid was caffeinated or not (with a table listing the amount of caffeine). For urine output, the amounts are in mL/cc or ounces, and characteristics can be selected, such as mucus, blood clots, or urine color (using a simplified color chart with options that include clear, light yellow, yellow, and amber). Leakage can be monitored as none, small, medium, or large amounts. Amounts for both I&O are automatically calculated to mL, and thus, are not dependent on the metric used for data entry.
Figure 1.
Goals and Catheterization Frequency
Source: Copyright © University of Rochester School of Nursing. Used with permission.
Figure 5.
Daily Amounts in Tables and Line Graphs
Source: Copyright © University of Rochester School of Nursing. Used with permission.
Figure 2.
Intake and Output Entries
Source: Copyright © University of Rochester School of Nursing. Used with permission.
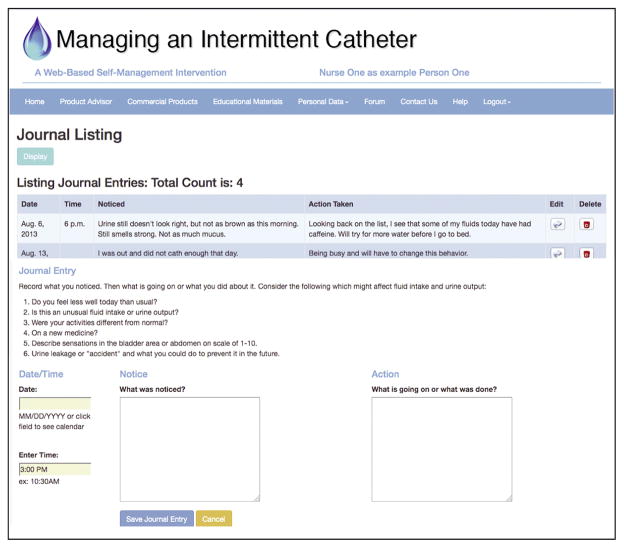
The Journal page (see Figure 3) includes a place for the date, two sections for “what was noticed” and another for “what was going on or done about it,” and questions/statements to facilitate writing journal entries. The prompts are based on questions used in the previous indwelling catheter study by the research team (Wilde & Brasch, 2008), with modifications for IC:
Figure 3.
Journal Page
Source: Copyright © University of Rochester School of Nursing. Used with permission.
Do you feel less well today than usual?
Is this an unusual fluid intake or urine output?
Were your activities different from normal?
On a new medicine?
Describe sensations in the bladder area or abdomen on scale of 1 to 10.
Urine leakage or “accident” and what you could do to prevent it in the future.
Lastly, the Personal Data section includes an Overview page, which is composed of tables and graphs of all cumulative data. These are intake and output in a bar graph (see Figure 4) with a blue color for intake and light yellow for output, showing amounts/day; a table with daily totals of intake and output; and catheterization information with daily amounts in tables and line graphs (see Figure 5) showing patterns and trends. These overview visuals show differences among dates and can depict discrepancies between intake and output. In addition, because this overview displays all entries chronologically, the catheter user or study nurse can more readily see patterns between notes in the journal and the entries for I&O. This level of linking detail is believed to facilitate better self-management skills. For instance one might discover reasons for not adhering to their IC planned frequency on weekends by reviewing how their activity and fluid intake varied during the week as compared with the weekend.
Figure 4.
Intake and Output in a Bar Graph
Source: Copyright © University of Rochester School of Nursing. Used with permission.
Study Nurse Consultations
The study nurse made two phone consultations about a week apart. The first contact was to teach the initial three-day self-monitoring, explaining how to use the online diary formats, including use of the personal database for storing I&O information/graphs and journal notes. The second contact was to discuss the results of the self-monitoring period: reviewing I&O data, graphs, identifying what the person noticed about how intake affected output, activities, urine leakage, and suggesting self-management activities to prevent problems. While the entire educational booklet was reviewed, special emphasis was on issues related to balancing fluids with activity (see Table 2) and adherence to appropriate IC intervals (see Table 3). Participants were informed that they could email the study nurse with questions. The third consultation phone call was made at three months to identify additional issues and to guide the person in further self-management activities.
Table 2.
Balance Fluids with Activity: Optimal Fluid Intake
While you need fluids for health, drinking too much can cause over-distention of the bladder, and this can contribute to urinary tract infection (UTI).
Quote: “As long as the urine looks clear and clean, I’m not worried about it.”
| Paying Attention | Things You Can Do |
|---|---|
| Notice whether you are getting enough fluids – but not too much – throughout the day. Become aware of whether different types of fluids make you need to cath more frequently or with more urgency. 
|
If you find you are not drinking enough, by cathing volume, you can try some of the suggestions below to increase your fluids. If you like the water cold, keep several bottles in the fridge and refill them with fresh water every day. To add flavor to water, try 2 ounces of cranberry or apple juice to 8 to 10 ounces of water. You may also try adding a little lime or lemon juice. Keep fresh glasses of water throughout the house. Secure a jug or bottle of water to your wheelchair. Use a rigid straw so you don’t have to suck hard. You may want to drink around meal times and before bed. Have a caregiver remind you to drink water. |
| Notice changes in color of urine every time you catheterize. | Color should remain light yellow to yellow all day. (See the color chart at the end of the booklet.) If color gets dark or urine has foul smell, increase water. |
| If you are on fluid restriction, make sure you stay within restricted range. | Record fluid intake occasionally to check that you are staying within range. |
| Be aware of changes in daily activities, such as stress, illness, or travel. | Use a journal to increase awareness of how activity affects fluid intake. If you choose to restrict fluids for a while to prevent leakage, it could take up to 24 hours to balance your intake again. Noticing the color and amount in cathing will tell you when you are back on track. |
Source: Copyright © Mary H. Wilde et al. Used with permission. Content should not be modified or used without permission of the first author.
Table 3.
Balance Fluids with Activity: Promote Your Best Intermittent Catheterization (IC) Intervals
IC should be done on the average every four to six hours, and the amount of urine should be less than 500 mL (cc). Cathing too often is irritating to the urethra, but not cathing often enough contributes to a urinary tract infection (UTI).
Quote: “I’ve met a lot of people who say, ‘Oh, I don’t want to drink a lot because I’m always worried.’ I do the same thing, but I try to find certain times of the day where I can hydrate my body.”
| Paying Attention | Things You Can Do |
|---|---|
Become aware of your own cathing pattern. Pay careful attention to urine color and how you feel.
|
Pay attention to cathing intervals (times of day and number of hours in between) and amounts for three days to see what your usual pattern is. If you think you might not be adhering to your best intervals, keep track of it for a few days to be sure you are on track. |
| Become aware of reasons for urine “accidents” so you can prevent them in the future. (See page on leakage.) | Consider whether you waited too long and your bladder was too full, you drank too much in a short time, or the bathroom was inaccessible. Sometimes more urine is produced during the night related to your position, the legs being up, and that the kidneys function better when lying down. For women, monthly hormone changes can also affect this. |
| Notice when and what you drink in the evening. | Withhold fluids in the evening to prevent a need to cath at night. However, some people need to wake at night to stay dry. If you avoid caffeine, you are less likely to need to void. (See page on caffeine.) |
Source: Copyright © Mary H. Wilde et al. Used with permission. Content should not be modified or used without permission of the first author.
Peer-Led Online Forum Discussions
Online forums became available when three or four people were enrolled. Topics in the Discussion Forum were open-ended, allowing study participants and peer leaders to start new topics (threads) or post to already developed topics. Peer leaders guided the discussion assisted by the study nurses or principal investigator. A urologist and a urology nurse were available to answer more complex clinical questions, which were then posted by the principal investigator.
Mobile Phone Modification
In addition to our National Institutes of Health funding, we were fortunate to have received a substantial gift for our research from a local donor. The team decided to use these funds to develop a modification in the program for mobile phone use. This decision was based on suggestions from four pretesting study participants who tried out the website in the first six months of the study.
Conclusion
This web-based intervention is the first known of its kind for intermittent catheter users. The intervention included a new and unique web-based interactive urinary diary, which was modified for mobile phone use, three study nurse phone call contacts, and peer-led discussion forums. The intervention will be evaluated for feasibility and usability at the conclusion of the pilot study, which is currently in progress with 30 individuals with SCI. Depending on the feasibility assessment, further research is likely to test the efficacy of the intervention in a larger sample of people using long-term intermittent urinary catheters, with the eventual goal of wide-spread dissemination in a permanent web-site.
Acknowledgments
We gratefully acknowledge our two research consultants on the study, Eun-Ok Im, PhD, RN, and Wonshik Chee, PhD, University of Pennsylvania; and our nurse consultant Karen Genett, MS, RN, who assisted us in recruitment and improvements in the educational materials.
Funding was provided by the National Institute of Nursing Research; National Institutes of Health (U.S.) #R21 NR012763; the University of Rochester, School of Nursing; and the Leary Fund.
Footnotes
Statement of Disclosure: Dr. Wilde is a consultant for NovaBay Pharmaceutical. No other authors have conflicts of interest.
Contributor Information
Mary H. Wilde, Associate Professor, University of Rochester, School of Nursing, Rochester, NY.
Eileen Fairbanks, Project Coordinator, University of Rochester, School of Nursing, Rochester, NY.
Robert Parshall, Senior Analyst/Database and Web Developer, University of Rochester, School of Nursing, Rochester, NY.
Feng Zhang, MS/PhD student, University of Rochester, School of Nursing, Rochester, NY.
Sarah Miner, Doctoral Student, University of Rochester, School of Nursing, Rochester, NY.
Deborah Thayer, Web Developer/Web Designer, University of Rochester, School of Nursing, Rochester, NY.
Brian Harrington, Director of Information Technology Services, University of Rochester, School of Nursing, Rochester, NY.
Judith Brasch, Project Nurse, University of Rochester, School of Nursing, Rochester, NY.
Dan Schneiderman, Senior Analyst/Programmer, University of Rochester, School of Nursing, Rochester, NY.
James M. McMahon, Associate Professor, University of Rochester, School of Nursing, Rochester, NY.
References
- Al-Jadid MS, Al-Asmari AK, Al-Moutaery KR. Quality of life in males with spinal cord injury in Saudi Arabia. Saudi Medical Journal. 2004;25(12):1979–1985. [PubMed] [Google Scholar]
- Brillhart B. Studying the quality of life and life satisfaction among persons with spinal cord injury undergoing urinary management. Rehabilitation Nursing. 2004;29(4):122–126. doi: 10.1002/j.2048-7940.2004.tb00328.x. [DOI] [PubMed] [Google Scholar]
- Christopher & Dana Reeve Foundation. One degree of separation: Paralysis and spinal cord injury in the United States. 2015 Retrieved from http://www.christopherreeve.org/site/c.ddJFKRNoFiG/b.5091685/k.58BD/One_Degree_of_Separation.htm.
- Cottenden A, Bliss D, Buckley B, Fader M, Gartley C, Hayer D, … Wilde MH. Management using continence products. In: Abrams P, Cardozo L, Khoury S, Wein A, editors. Incontinence: 5th International Consultation on Incontinence; The Netherlands: ICUD-EAU Publishers; 2013. [Google Scholar]
- El-Masri YWS, Chong T, Kyriakider AE, Wang D. Long-term follow-up study of outcomes of bladder management in spinal cord injury patients under the care of the Midlands Centre for spinal injuries in Oswestry. Spinal Cord. 2012;50(1):14–21. doi: 10.1038/sc.2011.78. [DOI] [PubMed] [Google Scholar]
- Kelly L, Spencer S, Barrett G. Using intermittent self-catheters: Experiences of people with neurological damage to their spinal cord. Disability and Rehabilitation. 2014;36(3):220–226. doi: 10.3109/09638288.2013.785606. [DOI] [PubMed] [Google Scholar]
- Logan K, Shaw C, Webber I, Samuel S, Broome L. Patients’ experiences of learning clean intermittent self-catheterization: A qualitative study. Journal of Advanced Nursing. 2008;62(1):32–40. doi: 10.1111/j.1365-2648.2007.04536.x. [DOI] [PubMed] [Google Scholar]
- National Spinal Cord Injury Statistical Center. Spinal cord injury facts and figures at a glance. 2014 Retrieved from https://www.nscisc.uab.edu/PublicDocuments/fact_figures_docs/Facts%202014.pdf.
- Shaw C, Logan K, Webber I, Broome L, Samuel S. Effect of clean intermittent self-catheterization on quality of life: A qualitative study. Journal of Advanced Nursing. 2008;61(6):641–650. doi: 10.1111/j.1365-2648.2007.04556.x. [DOI] [PubMed] [Google Scholar]
- van Achterberg T, Holleman G, Cobussen-Boekhorst H, Arts R, Heesakkers J. Adherence to clean intermittent self-catheterization procedures: Determinants explored. Journal of Clinical Nursing. 2008;17(3):394–402. doi: 10.1111/j.1365-2702.2006.01893.x. [DOI] [PubMed] [Google Scholar]
- Wehman P. Employment and return to work for people with significant disabilities: How far have we come? 2010 Retrieved from http://kesslerfoundation.org/media/displaynews.php?id=67&title=8th%20Annual%20Estabrook%20Lecture%20Presented%20by%20Paul%20Wehman,%20PhD.
- Wilde MH, Brasch J. Teaching self-management to long-term urinary catheter users. International Journal of Urological Nursing. 2008;2(2):62–71. [Google Scholar]
- Wilde MH, Brasch J, Zhang Y. A qualitative descriptive study of self-management issues in people with long-term intermittent urinary catheters. Journal of Advanced Nursing. 2011;67(6):1254–1263. doi: 10.1111/j.1365-2648.2010.05583.x. [DOI] [PubMed] [Google Scholar]
- Wilde MH, McMahon JM, McDonald MV, Tang W, Wang W, Brasch J, … Chen DG. Self-management intervention for long-term indwelling urinary catheter users: Randomized clinical trial. Nursing Research. 2015;64(1):24–34. doi: 10.1097/NNR.0000000000000071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilde MH, Zhang F, Fairbanks E, Shah S, McDonald MV, Brasch J. Perceived value of a urinary catheter self-management program in the home. Home Healthcare Nurse. 2013;31(9):465–473. doi: 10.1097/NHH.0b013e3182a89791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodbury MG, Hayes KC, Askes HK. Intermittent catheterization practices following spinal cord injury: A national survey. The Canadian Journal of Urology. 2008;15(3):4065–4071. [PubMed] [Google Scholar]