Abstract
♦ Introduction:
This study was carried out to examine whether or not elderly patients on peritoneal dialysis (PD) had an increased risk of peritonitis.
♦ Methods:
This was a retrospective cohort study based on data from the French Language Peritoneal Dialysis Registry. We analyzed 8,396 incident patients starting PD between January 2003 and December 2010. The end of the observation period was 31 December 2012. Patients were separated into 2 age groups: up to 75 and over of 75 years old.
♦ Results:
Among 8,396 patients starting dialysis there were 3,173 patients older than 75. When using a Cox model, no association was found between age greater than 75 years and increased risk of peritonitis (hazard ratio [HR]: 0.97 [0.88 – 1.07]). Diabetes (HR: 1.14 [1.01 – 1.28] and continuous ambulatory PD (HR: 1.13 [1.04 – 1.23]) were significantly associated with a higher risk of peritoneal infection whereas nurse-assisted PD was associated with a lower risk of peritonitis (HR: 0.85 [0.78 – 0.94]. In the analysis restricted to the 3,840 self-care PD patients, there was no association between age older than 75 years and risk of peritonitis.
♦ Conclusion:
The risk of peritonitis is not increased in elderly patients on PD in a country where assisted PD is available.
Keywords: Peritoneal dialysis, peritonitis, elderly
An important proportion of subjects starting dialysis are older patients (1,2). In addition, as life expectancy on dialysis is improving and because elderly patients have a lower priority access to the waiting list for renal transplantation, the number of elderly patients on renal replacement therapy is increasing (3,4). One report from the Renal Epidemiology and Information Network (REIN) registry showed that peritoneal dialysis (PD) seemed to be the preferred dialysis modality for elderly patients starting renal replacement therapy (5). At the same time, compared with hemodialysis, PD was associated with a higher risk of mortality in the elderly population in France (6). It is possible that these elderly patients were overexposed to the complications of PD, which may have affected the outcome on dialysis. Visual deficiency, functional impairment, and cognitive dysfunction are common problems in elderly patients and may increase the risk of peritoneal infection linked to errors occurring during manipulation of the device. In addition, diverticulosis, which is more frequent in elderly patients, could increase the risk of enteric peritonitis. Peritoneal infection affects patient survival on dialysis as well as quality of life under treatment. In most of the studies already published, older age was not associated with a higher risk of peritoneal infection (7,8,9). However, these results must be confirmed in a country where disabilities, comorbidities, and functional impairment do not represent contraindications for PD.
This study was carried out to evaluate whether or not elderly patients treated with PD had a higher risk of peritoneal infection.
Study Population and Methods
Study Population
This was a retrospective study using data from the French Peritoneal Dialysis Registry (RDPLF). All adults (older than 18 years) starting PD in France between 1 January 2003 and 31 December 2010 were included. The end of the observation period was 31 December 2012. We excluded patients who had had primary PD failure, defined as PD duration of less than 2 days, and patients previously treated with PD. We also excluded patients treated with hemodialysis for more than 3 months before PD initiation, considering them not to be incident dialysis patients. A subset of self-care PD patients was extracted from the dataset.
Definition of the Events
We examined the occurrence of peritoneal infection during PD. The time from PD start and the first peritonitis were calculated. The number of peritoneal infections during PD was determined for each patient. In addition, the number of peritonitis episodes due to Staphylococcus epidermidis was evaluated, S. epidermidis peritonitis being considered an indicator of peritonitis linked to errors in manipulation of the equipment.
Definition of the Variables
The main objective of the study was to assess whether elderly patients had a greater risk of peritonitis than other patients. Several definitions of elderly population have been used in the nephrology literature. Here, the elderly population was arbitrarily defined by an age greater than 75 years, corresponding to the criteria used in 2 previous studies from France (6,10). Others covariates were gender, comorbidities, diabetes mellitus, underlying nephropathy, PD modality 3 months after dialysis start (automated PD or continuous ambulatory PD [CAPD]), assisted PD (family assistance, nurse assistance), starting PD after transplantation failure, center size, and center category. For center size evaluation, we calculated the number of incident PD patients per center and per year of participation during the study period. Centers were divided into 4 groups (non-profit center, community center, academic hospital, and private hospital). To assess patients' comorbidities we extracted the Charlson comorbidity score (CCI) from the database. In an attempt to evaluate the role of comorbidities independently of patient age, we calculated a modified CCI by subtracting the age sub-score. The causes of transfer to hemodialysis and the causes of the first peritonitis episode were also extracted. The cause of peritonitis is a declarative covariate recorded in the registry.
Statistical Analysis
Continuous variables were recorded as the median value, with the first and third quartile; categorical variables were recorded as frequencies and percentage. To avoid multiple testing issues, no statistical tests were performed for the group description. A Cox model was used for the time-to-event analysis. The event of interest was the occurrence of the first peritonitis episode. Only 95% confidence intervals (CIs) were used for statistical inference and to represent the uncertainty of both hazard ratios (HRs).
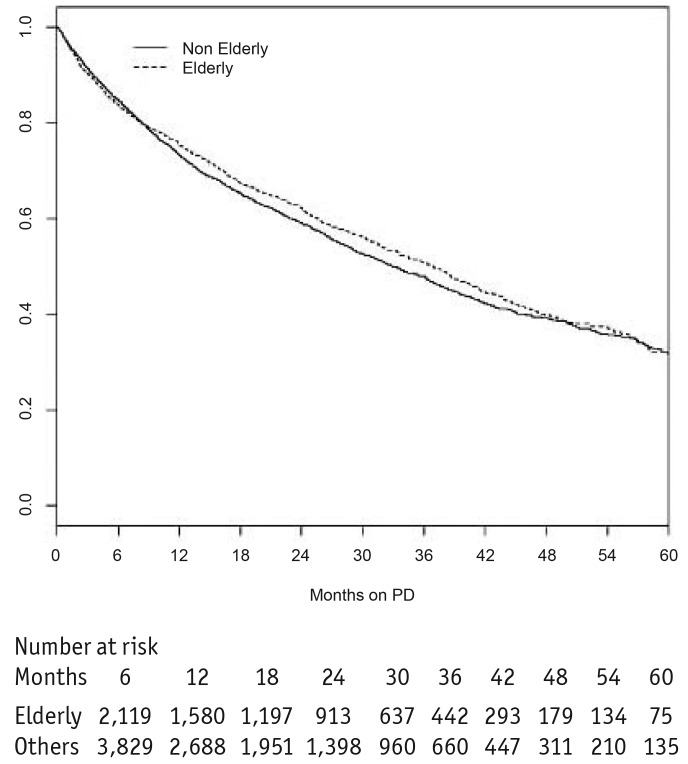
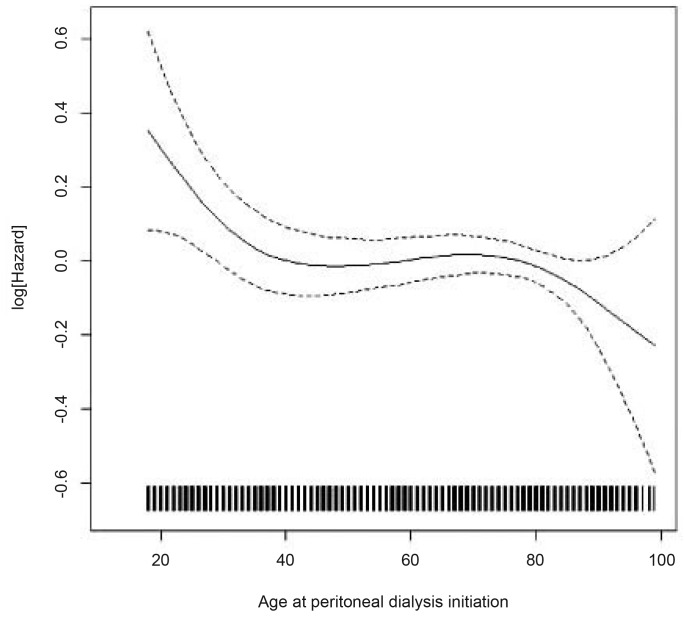
A Kaplan-Meier curve of survival free of peritonitis was drawn for the elderly and patients younger than 75 (Figure 1). We explored the relationship between variables and the time to first peritoneal infection episode using a bivariate Cox regression model. Regression spline was used to explore the functional form of the relationship between patient age and the risk of peritonitis (Figure 2). Proportional hazard assumptions were tested with Schoenfeld residual plots. Multivariate analysis was performed with a Cox regression model. Patient age (older or younger than 75 years) was entered in the model based on a priori consideration. Covariates were included in the multivariate analysis when they were associated with peritonitis risk in the bivariate analysis. The interaction between patient age and assisted PD was tested in the multivariate analysis with a Cox model.
Figure 1 —
Survival free of peritonitis (Kaplan-Meier survival curve). PD = peritoneal dialysis.
Figure 2 —
Relation between patient age and peritonitis risk (smoothing penalized spline).
Missing Data
Five percent of the data were missing for the CCI. We, therefore performed 5 sets of imputation for the missing CCI values. The set of imputed CCI values was chosen based on a graphic representation of the imputed value and the observed value. Modified CCI was calculated using the imputed CCI value.
Statistical analyses were done using R 2.15.1 (R Foundation for Statistical Computing), including the package survival, and MICE (multiple imputation by chained equations).
The RDPLF has the approval of the French national ethics committee, Commission nationale de l'informatique et des libertés. This study took place within the framework of this authorization.
Results
Patient Characteristics
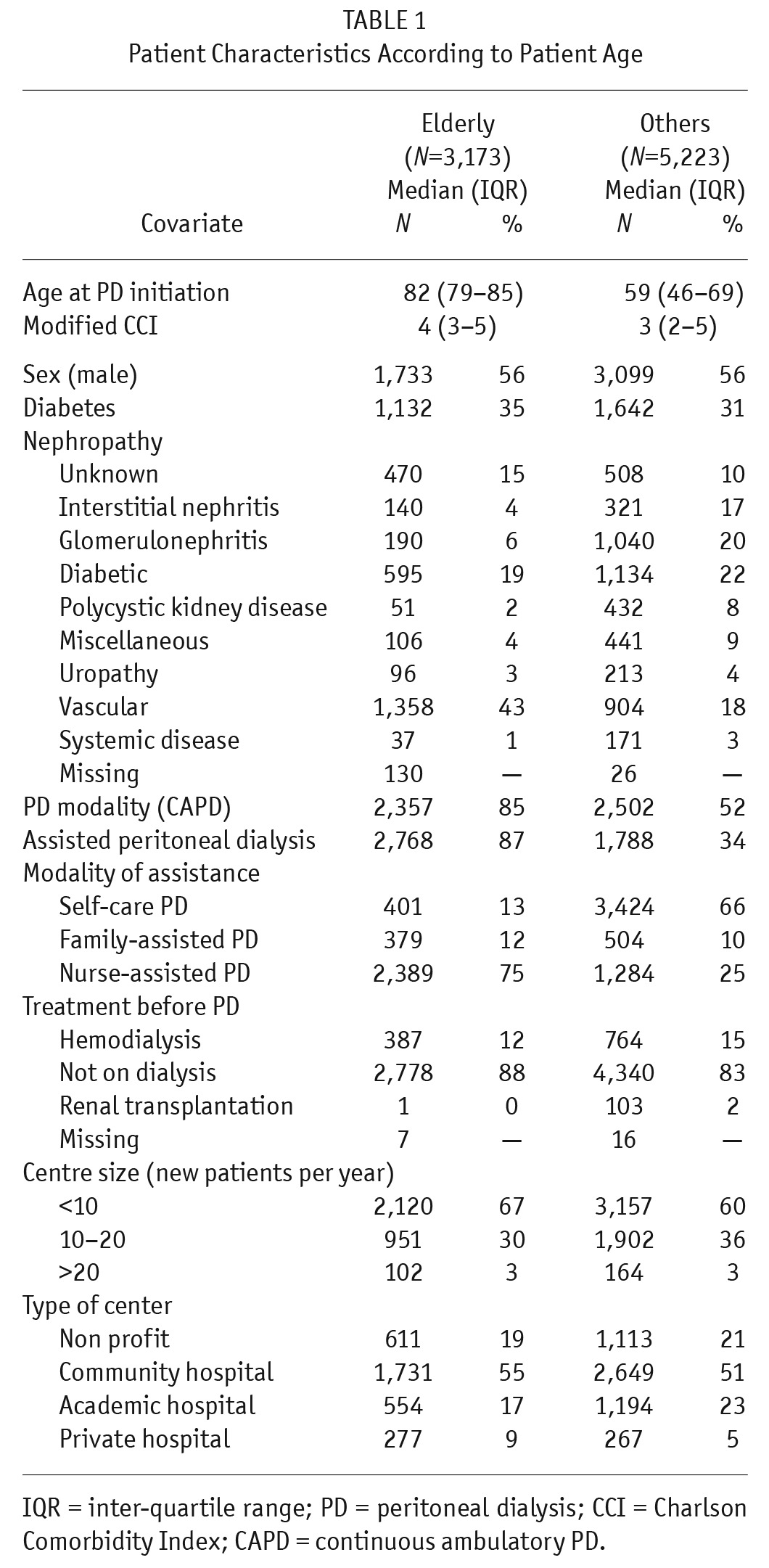
Of the 8,396 patients included in the study, 3,173 were older than 75 years. The median ages at dialysis initiation were respectively 82 and 59 years for the elderly group and the other patients. Elderly patients had a higher modified Charlson score than the other patients. Elderly patients were more frequently treated using CAPD and assisted PD than patients under 75. Detailed information about patient characteristics by dialysis initiation is provided in Table 1. Among the 8,396 patients there were 3,840 self-care PD patients. The 2-year actuarial patient survival was 36% (95% CI: 34 – 38) for the elderly patients and 70% (95% CI: 68 – 71) for the other patients. The 2-year technique survival of the elderly patients was 73% (95% CI: 0.71 – 0.75) compared with 59% (95% CI: 0.58 – 0.61) for the younger patients.
TABLE 1.
Patient Characteristics According to Patient Age
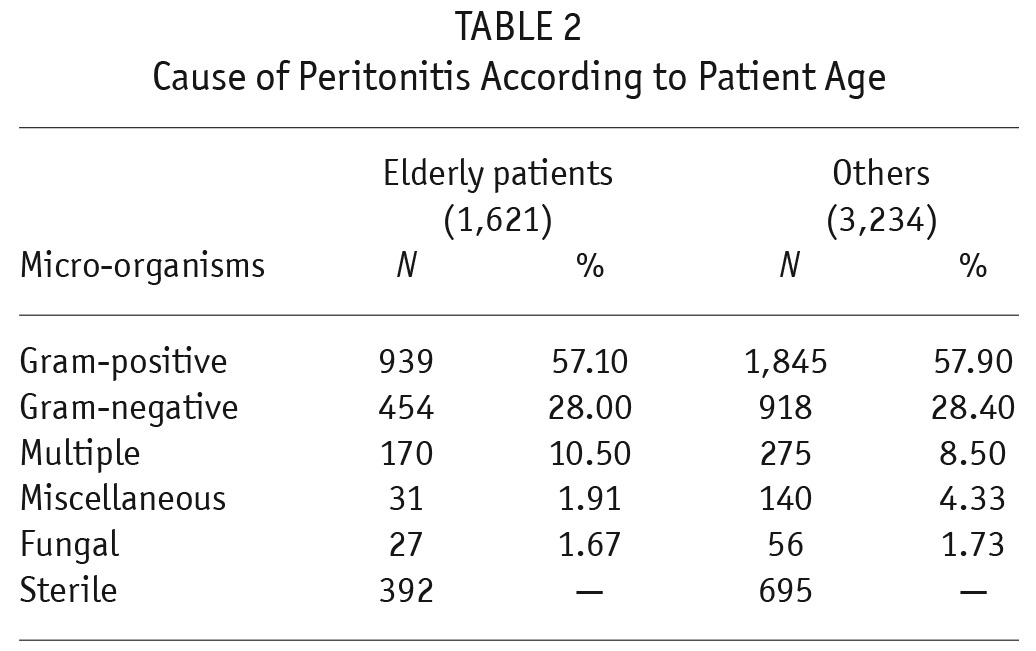
Peritoneal Infection
The median PD duration of the cohort was 12.68 months (interquartile range: 5.15 – 26.15). There were 5,958 peritonitis episodes for a total exposure time of 145,811 months on PD (1/25 patient months). The peritonitis rate was 1/27 patient months and 1/24 patients months for the elderly and younger patients, respectively. The incidence rate ratio of peritonitis was 0.86 (95% CI: 0.81 – 0.91, elderly as reference group). In addition, for infections specifically due to S. epidermidis the incidence ratio was 0.82 (0.69 – 0.98, elderly as reference group). The 2-year actuarial survival free of peritonitis was 62% (95% CI: 60 – 64) and 59% (95% CI: 57 – 61) for the elderly and other patients, respectively. Among the elderly patients, peritonitis was responsible for 109/637 (17%) of transfers to hemodialysis whereas peritonitis was a cause of PD cessation for 333/1,760 (19%) of the younger patients. There was no difference between the 2 groups regarding the causative agent of the peritonitis episode except for peritoneal infection due to the category of miscellaneous microorganisms (Table 2).
TABLE 2.
Cause of Peritonitis According to Patient Age
Risk of Peritonitis
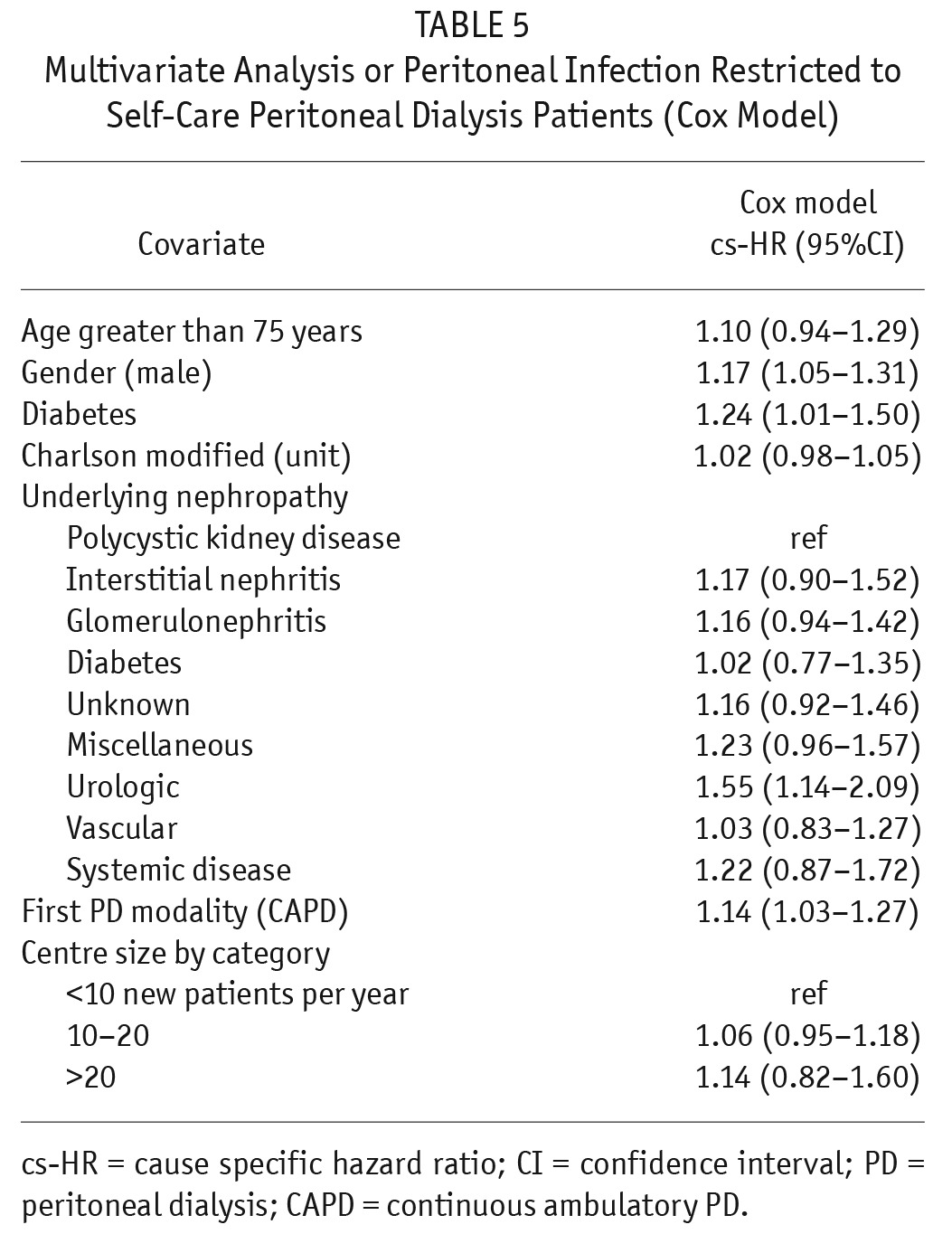
The Cox regression model showed that nurse-assisted PD was associated with a lower risk of peritoneal infection (Table 3). Nurse-assisted PD had a protective effect for elderly patients but had no significant effect on the peritonitis risk for younger patients (data not shown). Male patients, diabetic patients, and CAPD were associated with an increased risk of peritonitis. There was a significant relationship between patient age and assisted PD. In the multivariate analysis, there was no significant relationship between age greater than 75 years and peritonitis risk (Table 4). In the multivariate analysis restricted to the non-assisted PD patients, there was no significant association between age over 75 and risk of peritoneal infection (Table 5). Figure 2 represents the relationship between patient age and peritonitis risk.
TABLE 3.
Association Between Each Covariate and Peritonitis (Bivariate Analysis with Cox Model)
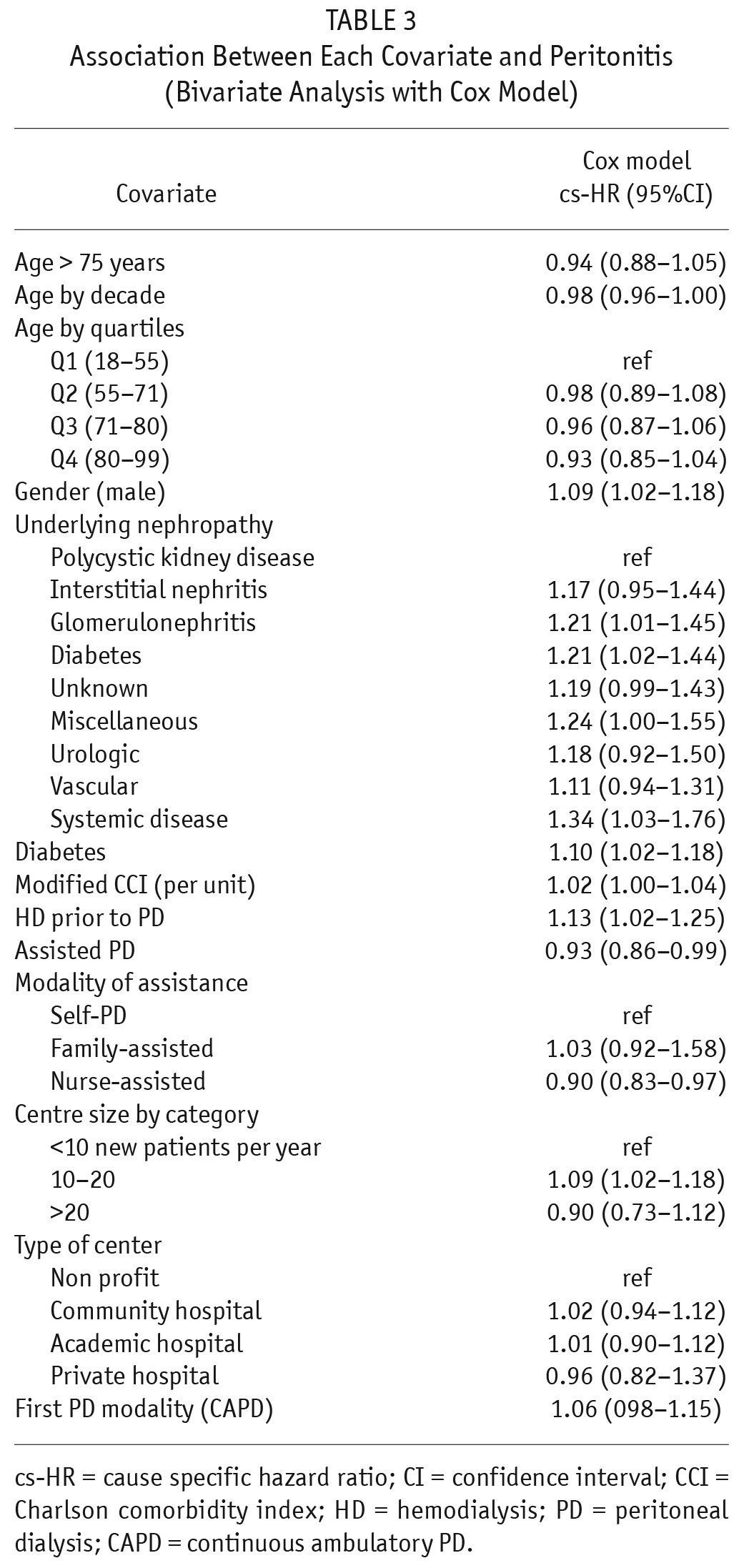
TABLE 4.
Multivariate Analysis of Peritoneal Infection (Cox Model)
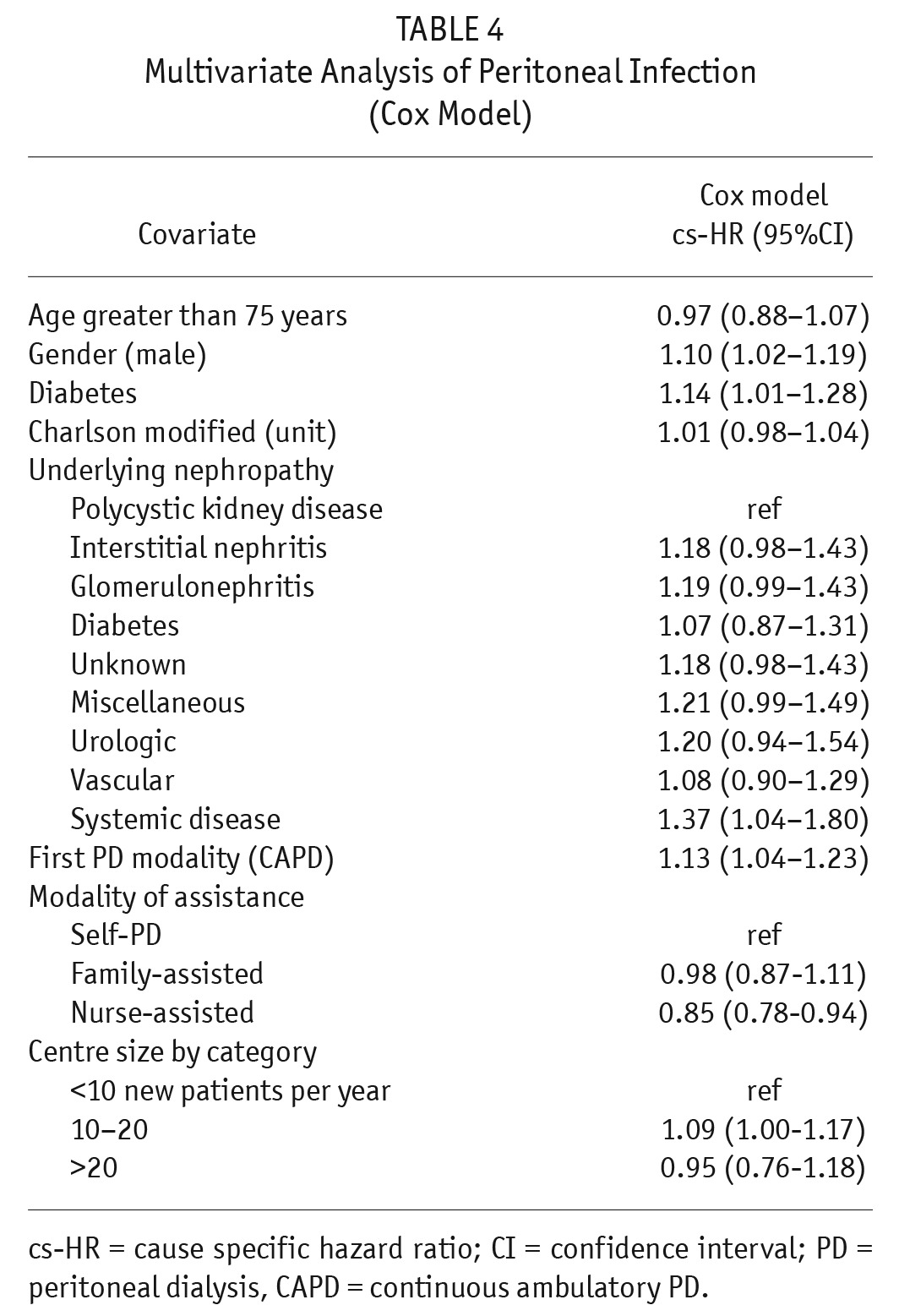
TABLE 5.
Multivariate Analysis or Peritoneal Infection Restricted to Self-Care Peritoneal Dialysis Patients (Cox Model)
Discussion
The results of this report are in line with the findings of our previous study about PD in elderly patients (10). In this new analysis, in an attempt to assess the risk of peritonitis linked to patient age, older individuals were compared with younger ones. There was no relationship between patient age and risk of peritonitis in the Cox model in our study. However, there was a bias due to the association between assisted PD, risk of peritonitis, and age greater than 75. Thus, it cannot be excluded that younger age per se is associated with a greater risk of infection.
There are few large-scale studies regarding the role of patient age on peritonitis risk. Li et al. compared PD outcomes between patients older than 65 years and younger patients (7). There was no significant difference between the 2 groups in peritonitis-free survival. In one study from Canada, age above 70 was not associated with an increased risk of peritonitis (9). In this study, 2 periods of PD initiation were separated (1996 to 2000 and 2001 to 2005). The authors found that older age was associated with a higher risk of infection during the first period but not during the second period of PD initiation. The authors hypothesized that the lack of association between increased age and peritonitis during the recent period could reflect the use of the flush-before-fill technique and of topical antibiotics. The results observed in the second period could also be partially explained by better selection of elderly patients for PD. Recently, Lim et al. found that patients older than 65 years and those 65 and under had similar rates of peritonitis-free survival (11). In this study, however, elderly patients had a higher risk of peritonitis-related and all-cause mortality. In a recent study from Brazil, the only factor associated with death during peritoneal infection was older age (12). This emphasizes the notion that, even if the risk of peritonitis is not higher in the older population, the consequences could be more severe because older subjects have more comorbidities. Colonic diverticular disease, highly prevalent in the older population, may increase peritonitis risk. Surprisingly, there was no difference in the rate of peritoneal infection due to gram-negative microorganisms between elderly and younger patients. Older patients presenting diverticulosis may have been contra-indicated for PD. Nevertheless, it has recently been observed that asymptomatic diverticulosis was not a risk factor for enteric peritonitis in PD patients (13).
It should be noted that more than 85% of the elderly patients in our study were treated with assisted PD, which could cause a co-linearity in the regression modeling. However, when the multivariate analysis was restricted to the subset of individuals on self-care PD, age over 75 was not associated with a higher risk of peritoneal infection. One limitation of our study is that nurse-assisted PD is fully covered by public healthcare insurance in France, and this assistance is therefore widely used by the elderly population. Consequently, the results of our study must be interpreted with caution, especially if applying them to a country where nurse-assisted PD is not available. Indeed, nurse-assisted PD could have a protective effect in elderly patients who have difficulties in manipulating the equipment. One may also argue that self-care elderly patients on PD could have been selected based on their ability to manipulate the catheter connection without the support of a nurse. On the contrary, in 2004, Verger et al. showed that, in patients treated with automated PD, nurse assistance was associated with a higher risk of peritonitis (14). However, when regular nurse visits from the PD center were organized, assisted PD was not associated with a higher risk of peritoneal infection. The differences between our findings and the results of Verger et al. could be explained by the effect of nurse assistance possibly varying from one PD modality to another, as most of the elderly patients included in our study were treated with CAPD. In addition, following the report of Verger et al., and because there were financial incentives to promote PD, more than 50% of PD centers in France had implemented nurse home visits by 2010.
Both diabetes and PD were associated with peritonitis risk in our study. In 2 studies from Australia, increased rate of peritonitis in PD patients was associated with diabetes (15,16). Possible reasons for an association between diabetes and peritonitis may have been visual impairment or immune function of diabetic patients. The role of PD modality on peritonitis risk remains controversial. A meta-analysis concluded that automated PD reduced the peritonitis rate compared with CAPD, whereas in a recent large scale study, PD modality was not associated with a higher peritonitis risk (16,17). It is difficult to draw any conclusion regarding the link between PD modality and peritonitis risk because of the indication bias.
Although it offers advantages in terms of quality of life, PD is underused in elderly patients (18). Our study confirms that, at least in select self-care elderly patients, the risk of peritonitis is similar to the risk observed in younger patients. In addition, our results support the idea that assisted PD may protect non-autonomous elderly patients from peritonitis. Further studies are needed to confirm this finding. We believe, like others, that older age should not be considered a risk factor for peritoneal infection.
Disclosures
The authors have no financial conflicts of interest to declare.
REFERENCES
- 1. USRDS 2008 data report. Available at www.usrds.org/2008/pdf/V2_03_2008.pdf.
- 2. Kurella M, Covinsky KE, Collins AJ, Chertow GM. Octogenarians and nonagenarians starting dialysis in the United States. Ann Intern Med (2007); 146:177–83. [DOI] [PubMed] [Google Scholar]
- 3. Jassal SV, Trpeski L, Zhu N, Fenton S, Hemmelgarn B. Changes in survival among elderly patients initiating dialysis from 1990 to 1999. CMAJ 2007; 177:1033–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dudley CR, Johnson RJ, Thomas HL, Ravanan R, Ansell D. Factors that influence access to the national renal transplant waiting list. Transplantation 2009; 88:96–102. [DOI] [PubMed] [Google Scholar]
- 5. Couchoud C, Savoye E, Frimat L, Ryckelynck JP, Chalem Y, Verger C, Peritoneal Dialysis Working Group of the French REIN registry Variability in case mix and peritoneal dialysis selection in fifty-nine French districts. Perit Dial Int 2008; 28:509–17. [PubMed] [Google Scholar]
- 6. Couchoud C, Moranne O, Frimat L, Labeeuw M, Allot V, Stengel B. Associations between comorbidities, treatment choice and outcome in the elderly with end-stage renal disease. Nephrol Dial Transplant 2007; 22:3246–54. [DOI] [PubMed] [Google Scholar]
- 7. Li PK, Law MC, Chow KM, Leung CB, Kwan BC, Chung KY, et al. Good patient and technique survival in elderly patients on continuous ambulatory peritoneal dialysis. Perit Dial Int 2007; 27:S196–201. [PubMed] [Google Scholar]
- 8. Szeto CC, Ching-Ha Kwan B, Chow KM. Peritonitis risk for older patients on peritoneal dialysis. Perit Dial Int 2008; 28:457–60. [PubMed] [Google Scholar]
- 9. Nessim SJ, Bargman JM, Austin PC, Story K, Jassal SV. Impact of age on peritonitis risk in peritoneal dialysis patients: an era effect. Clin J Am Soc Nephrol 2009; 4:135–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Castrale C, Evans D, Verger C, Fabre E, Aguilera D, Ryckelynck JP, et al. Peritoneal dialysis in elderly patients. Report from the French Peritoneal Dialysis Registry (RDPLF). Nephrol Dial Transplant 2010; 25:255–62. [DOI] [PubMed] [Google Scholar]
- 11. Lim WH, Dogra GK, McDonald SP, Brown FG, Johnson DW. Compared with younger peritoneal dialysis patients, elderly patients have similar peritonitis-free survival and lower risk of technique failure, but higher risk of peritonitis-related mortality. Perit Dial Int 2011; 31:663–71. [DOI] [PubMed] [Google Scholar]
- 12. de Moraes TP, Olandoski M, Caramori JC, Martin LC, Fernandes N, Divino-Filho JC, et al. Novel predictors of peritonitis-related outcomes in the BRAZPD cohort. Perit Dial Int 2014; 34:179–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Toda S, Ito Y, Suzuki Y, Hiramatsu H, Ozaki T, Tsuboi N, et al. Asymptomatic diverticulosis identified by computed tomography is not a risk factor for enteric peritonitis. Nephrol Dial Transplant 2012; 27:2511–6. [DOI] [PubMed] [Google Scholar]
- 14. Verger C, Duman M, Durand PY, Veniez G, Fabre E, Ryckelynck JP. Influence of autonomy and type of home assistance on the prevention of peritonitis in assisted automated peritoneal dialysis patients. An analysis of data from the French Language Peritoneal Dialysis Registry. Nephrol Dial Transplant 2007; 22:1218–23. [DOI] [PubMed] [Google Scholar]
- 15. Ghali JR, Bannister KM, Brown FG, Rosman JB, Wiggins KJ, Johnson DW, et al. Microbiology and outcomes of peritonitis in Australian peritoneal dialysis patients. Perit Dial Int 2011; 31:651–62. [DOI] [PubMed] [Google Scholar]
- 16. McDonald SP, Collins JF, Rumpsfeld M, Johnson DW. Obesity is a risk factor for peritonitis in the Australian and New Zealand peritoneal dialysis population. Perit Dial Int 2004; 24:340–6. [PubMed] [Google Scholar]
- 17. Rabindranath KS, Adams J, Ali TZ, Daily C, Vale L, Macleod AM. Automated vs continuous ambulatory peritoneal dialysis: a systematic review of randomized controlled trials. Nephrol Dial Transplant 2007; 22:2991–8. [DOI] [PubMed] [Google Scholar]
- 18. Lan PG, Johnson DW, McDonald SP, Boudville N, Borlace M, Badve SV, et al. The association between peritoneal dialysis modality and peritonitis. Clin J Am Soc Nephrol 2014; 9:1091–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Brown EA, Johansson L, Farrington K, Gallagher H, Sensky T, Gordon F, et al. Broadening Options for Long-term Dialysis in the Elderly (BOLDE): differences in quality of life on peritoneal dialysis compared to haemodialysis for older patients. Nephrol Dial Transplant 2010; 25:3755–63. [DOI] [PMC free article] [PubMed] [Google Scholar]