Abstract
Objectives.
Conservation of Resources (COR) theory postulates that individuals utilize various resources to manage stressful circumstances. Children employ many resources to cope with the problems of parents who suffer from disabilities, cognitive impairment, and functional limitations. This phenomenon is rarely explored among middle-aged offspring and their aging parents.
Method.
Drawing from the Family Exchanges Study, we focus on a sample (N = 308) of middle-aged adults (mean age = 51) whose only living parent was their mother. We use multiple regression to examine maternal support and self-reported health as moderators of maternal problems on offspring depressive symptoms.
Results.
Participants whose mothers had few problems generally reported low levels of depressive symptoms. When mothers had high problems, results indicate a negative association between depressive symptoms and physical health. When maternal problems were high, the amount of support offspring receive from their mother had a negative association with offspring depressive symptoms. When mothers had low problems, receiving more maternal support was associated with lower depressive symptoms and receiving low support was associated with increased depressive symptoms.
Discussion.
Middle-aged offspring use both personal and family-based resources to buffer the psychological ramifications of their mother’s problems. Our results provide a unique extension of COR theory.
Key Words: Depression, Family, Personal relationships, Widowhood.
Through the theoretical lens of Conservation of Resources (COR) theory (Hobfoll, 1989), we examine differential resources that moderate the effects of maternal problems on middle-aged offspring depressive symptoms. COR suggests that individuals retain and conserve a variety of resources that help them meet various challenges and stressors. Although COR has been tested within the context of adult offspring who serve as caregivers for their aging parents (Lin, Chen, & Li, 2013), this theory is seldom applied to a non-caregiver sample. A wide range of literature highlights the reciprocal relationship between the physical and mental health of aging parents and their middle-aged offspring (Low et al., 2012; Riffin, Suitor, Reid, & Pillemer, 2012; Timko et al., 2009). This body of research maintains a focus on major life events such as a dementia diagnosis, psychiatric condition, or chronic illness. Yet, older adults experience other problems including relationship turmoil, non-chronic health issues, minor injuries, financial setbacks, emotional struggles, or victimization from crimes or abuse. Such problems have been widely explored in child development research (Boyd & Waanders, 2013; Letourneau et al., 2011) but have rarely been considered within the context of older parents and middle-aged offspring. In this study, we utilize COR theory to explore the differential impact of mother’s problems on the depressive symptoms of their middle-aged offspring.
Effects of Parental Problems on Grown Offspring
Middle-aged adults will likely find themselves providing financial, practical, or emotional assistance to their aging parents; others may become the primary caregivers for parents and find themselves increasingly vulnerable to feelings of burden and depression (Amirkhanyan & Wolf, 2006; Lin et al., 2013). Research on offspring who serve as caregivers for their chronically ill parents highlights the relationship between parent and child health. Kim, Wellisch, and Spillers (2008) found that for daughters who serve as caregivers for a mother with cancer, mother’s distress played a significant role in daughter’s quality of life. Daughters of breast cancer patients also report an increased sense of vulnerability as a result of their mother’s cancer diagnosis (Raveis & Pretter, 2005). Furthermore, having unhealthy parents can undermine the mental and physical health of grown offspring; this is particularly true for middle-aged adults with a sole-surviving mother (Marks, Bumpass, & Jun, 2004).
For children who do not serve as caregivers, the reciprocal relationship between parent’s chronic mental illness and offspring well-being is also well established. Low and colleagues (2012) found that maternal mood/anxiety disorders are associated with diagnosed psychiatric disorders among offspring; young adults with depressed parents are more likely to be diagnosed with depression and are likely to display severe depressive symptoms. Similarly, research by Timko et al. (2009) indicates the relationship between depression and other impairments—such as physical dysfunction, pain, disability, and negative events—is stronger for adults with depressed parents than non-depressed parents. Although Timko and colleagues highlight both genetic components and the burden associated with having a chronically depressed parent in adulthood, the age of this sample was relatively young (mean age = 34) in comparison to age ranges typically thought to encompass midlife. Thus, the generalizability of these findings is limited to younger adults.
The exploration into mother’s problems and child well-being is also truncated by an emphasis on early child development or adolescents. Much of this research focuses on the developmental hurdles of children with depressed mothers (Boyd & Waanders, 2013; Dodge, 1990; Goodman & Gotlib, 1999; Kohl, Kagotho, & Dixon, 2011; Markowitz, 2008; Murray et al., 1999). Other studies have explored the increased risk factors that children face when their mothers are victims of intimate partner violence (Letourneau et al., 2011), drug dependent (Steinhausen, Mas, Ledermann, & Metzke, 2006), socioeconomically disadvantaged (Bradley & Corwyn, 2002; McLoyd, 1998), homeless (Meadows-Oliver, 2009), or incarcerated (Dallaire, 2007; Myers, Smarsh, Amlund-Hagen, & Kennon, 1999). These studies provide insight into how life circumstances, problems, and negative events can severely affect child development as well as the mother–child relationship as a whole. Despite evidence that suggests age differences in problem-solving strategies (Blanchard-Fields, Stein, & Watson, 2004), little is known about how offspring cope with the problems of their parents during later stages of development.
Conservation of Resources and Mother–Child Bonds
This study explores the sustaining and protective power of different resources that moderate the relationship between mother’s problems and depressive symptoms of middle-aged offspring. We analyze this phenomenon within the theoretical context of COR theory. COR suggests that individuals build and maintain resources to help meet challenges and cope with stressors (Hobfoll, 1989). Although often used to understand burnout and stress processes in organizational settings (Seiger & Wiese, 2009), we seek to examine this theory within the context of mother–child relationships. COR has guided previous research on children who serve as caregivers for their aging parents (Lin et al., 2013). Lin and colleagues identify several resources including parent–child relationship satisfaction and social support from others that serve as a buffer between caregiver burden and caregiver depressive symptoms. Other literature has identified psychosocial moderators of the effects of transitioning into the caregiving role and caregiver well-being (Marks, Lambert, Jun, & Song, 2008). In a similar fashion, we apply COR to a non-caregiver sample of middle-aged adults to understand personal and relational moderators of mother’s problems on offspring depressive symptoms.
Mothers are a logical focus for the study of parent problems and adult–offspring depressive symptoms due to gender differences in mortality rates as well as the distinctive nature of the mother–child relationship. According to the National Vital Statistics Reports (Hoyert & Xu, 2012), the life expectancy for women is nearly 5 years longer than that of men. These differences in longevity indicate that midlife adults are three times more likely to have a sole-surviving mother than a sole-surviving father (Marks et al, 2004). In addition to population-based statistical trends, evidence suggests that mother’s relationships with their children are unique from and more intensive than father’s relationships with their children (Burholt & Wenger, 1998; Rossi & Rossi, 1991). The highly probable role transition of becoming a widowed mother also shifts the mother–child relationship as well as family obligation (Rossi & Rossi, 1990). Thus, examining middle-aged offspring with a sole-surviving mother is a logical starting point for this investigation into mother’s problems.
COR suggests that individuals maintain resources to help meet various challenges; we tested this theory within the challenging context of having a sole-surviving mother with life problems. Although a sample of non-caregivers is certainly not prone to the same stressors or burden as primary caregivers, we predicted that the amount of support participants received from their mothers would moderate the association between mother’s problems and offspring depressive symptoms. Specifically, we hypothesized that participants who reported having a mother with higher levels of problems would report more depressive symptoms if they also reported receiving low levels of support from their mother. In addition, we view self-reported physical health as a personal resource that has potential to moderate the relationship between mother’s problems and offspring depressive symptoms. We hypothesized that having low physical health would be associated with an exacerbation of depressive symptoms within the context of having a mother with many life problems.
Method
Sample and Procedure
This sample is from the Family Exchanges Study (FES; Fingerman, Miller, Birditt, & Zarit, 2009), which sought to understand family relationships of middle-aged adults, their living parents, and their adult children. In 2008, FES recruited a target sample of 845 middle-aged adults who had at least one living adult child and at least one living parent. These participants were identified through lists from Genesys Corporation and random digit dialing from the Philadelphia Primary Metropolitan Statistical Area including urban, rural, and suburban areas in New Jersey and Pennsylvania. Of the eligible participants, 633 (75%) agreed to be interviewed. Participants completed 1-hr long Computer-Assisted Telephone Interviews regarding relationships with their grown offspring and living parents. This article utilizes a subset of 308 participants (157 men and 151 women; mean age = 51) whose only living parent was their mother (Table 1).
Table 1.
Demographic Characteristics of Participants
| Variables | M | SD |
|---|---|---|
| Age | 51.3 | 4.95 |
| Gender (1 = male) | 0.51 | 0.50 |
| Education levelª | 3.19 | 1.12 |
| Number of children | 2.91 | 2.48 |
| Number of siblings | 3.30 | 2.48 |
| Self-reported physical health | 3.40 | 1.09 |
| Depression | 1.49 | 0.70 |
| Proportions | ||
| Marital status | ||
| Married/remarried | 0.68 | |
| Cohabiting | 0.02 | |
| Single/never married | 0.07 | |
| Divorced/separated | 0.20 | |
| Widowed | 0.02 | |
| Ethnicity | ||
| White | 0.58 | |
| African American | 0.36 | |
| Asian | 0.003 | |
| Hispanic | 0.07 | |
| Multicultural | 0.05 | |
Note. ªEducation: 1 = no high school; 2 = high school graduate; 3 = some college; 4 = college graduate; 5 = postgraduate.
Measures
Life problems.
Participants reported life problems they, their mother, and/or offspring have experienced in the past 2 years through a series of yes/no questions. The dimensions tapped were serious health problem or injury, emotional or psychological problem, drinking or drug problem, serious financial problem, the death of someone close to them, victim of a crime, a serious relationship problem, or other problems. We used the sum of mothers’ problems in our analyses. Past research examined childrens’ life problems in this manner (Birditt, Fingerman, & Zarit, 2010; Fingerman, Cheng, Birditt, & Zarit, 2012; Greenfield & Marks, 2006).
Family support.
Family support is a resource that may moderate the relationship between mother’s problems and offspring depressive symptoms. Support received from a mother may buffer the effects of a mother’s problems on her offspring, but support given to a troubled mother may further exacerbate depressive symptoms in offspring. Thus, we chose to measure the amount of support given and received by the participant’s mother. Support was measured using the Intergenerational Support Scale (Fingerman et al., 2009) that measures how frequently family members exchange different types of support including companionship, talking about daily events, giving emotional support, providing practical support, giving advice, and providing financial assistance. Participants rated how frequently they exchanged these six types of support with their mother on an 8-point scale ranging from 1 (less than once a year or not at all) to 8 (daily) (α = 0.79).
Individual resources.
An individual resource that has been utilized to assess COR in previous research is self-reported physical health. Self-reported physical health has also shown a strong association with mental health across the life span (Street, O’Connor, & Robinson, 2007). We measured self-reported physical health by asking participants to rate their own physical health for the past 12 months using a 5-point scale ranging from 1 (poor) to 5 (excellent). This resource stands independently from family resources.
Control variables.
We controlled for several variables associated with depressive symptoms. Keyes and Westerhof (2012) suggest that age is associated with major depressive episodes and mental health in midlife; thus, we controlled for both participant and mother’s age. We also controlled for participant gender because the literature shows significant gender differences in the prevalence of depression disorders in midlife (Cleary, Zaborski, & Ayanian, 2004). We controlled for minority status due to a growing body of research that shows racial differences in family ties and well-being (Cichy, Stawski, & Almeida, 2013). To ensure that results were not confounded by other family members’ problems, we controlled for the mean problems of the participants’ children. Intensity of help that adult offspring provide to an aging parent correlates positively with the number of brothers and negatively with the number of sisters that a middle-aged child has (Tolkacheva, van Groenou, & van Tilburg, 2010). We incorporated a control measure of siblings living geographically close (within 50 miles) to the participant’s mother.
Parent–offspring relational quality plays an important role in parent–child support exchanges (Fingerman et al., 2009); thus, we controlled for how important the participant rated their relationship with their mother from 1 (least important) to 6 (most important). Finally, because we specifically wanted to explore the problems of mothers who did not have functional limitations, we controlled for mothers’ restriction of activities of daily living (ADL), which participants indicated through a series of yes/no questions pertaining to mothers’ daily functional limitations.
Outcome.
A depression rating for each participant was established using five items from the Brief Symptom Inventory, a 53-item self-report scale (Derogatis, 2000) that taps depression symptoms commonly observed in everyday settings. Participants rated to what extent they felt lonely, blue, worthless, hopeless about the future, or had no interest in things, using a 5-point scale ranging from 1 (not at all) to 5 (extremely). Individual depressive symptom scores were established by computing the mean score of these five items (α = 0.78). Participants generally reported low levels of depression (M = 1.49, standard deviation [SD] = 0.70).
Analysis Strategy
We conducted multiple linear regression analysis to predict depressive symptoms of middle-aged offspring. Predictors included a combination of offspring (self-reported physical health and relational quality with mother) and mother’s characteristics (mother’s problems and support provided and received by the participant’s mother). We controlled for mother characteristics (age and ADL status), offspring characteristics (gender, age, education, and minority status), and family factors (offspring–mother relational quality, mother’s marital status, problems of the participant’s own children, and the number of siblings living geographically close to the mother). We computed possible interactions between personal resources and mother’s life problems to examine whether these different resources moderate the relationship between mother’s life problems and offspring depressive symptoms.
Results
Mother’s Life Problems
Participants reported several types of problems that their mother experienced in the past 2 years (Table 2). Although the sum of mother’s life problems was generally low (M = 1.90, SD = 1.30), participants reported that their mothers did in fact experience a wide range of problems. The most frequently cited problems were having a health problem/injury as well as experiencing a death of a loved one.
Table 2.
Mother’s Problems Experienced in the Past 2 Years
| Mother’s problemsa | Proportions |
|---|---|
| Divorce/relational problem | 0.06 |
| Victim of a crime | 0.06 |
| Experienced a death | 0.57 |
| Financial problem | 0.13 |
| Drinking/drug problem | 0.02 |
| Emotional/psychological problem | 0.21 |
| Health problem/injury | 0.58 |
| Mean total problems (SD) | 1.90 (1.30) |
Note. a1 = yes.
We found two significant interactions between mother’s problems, personal and family-based resources, and participants’ depressive symptoms (Table 3). For depressive symptoms, significant interactions were found for (a) participant self-reported physical health and mother’s problems and (b) support provided by the mother and mother’s problems. To illustrate these interactions, we followed a standard approach by contrasting groups that are high or low in each of these dimensions by fixing scores at +1 for 1 SD above the mean and at −1 for 1 SD below the mean.
Table 3.
Mother’s Life Problems and Participant Depressive Symptoms
| B | SE | β | |
|---|---|---|---|
| Parameter | |||
| Participant age | .007 | .009 | .053 |
| Participant gender (1 = male) | −.150 | .075 | −.110* |
| Participant educationa | −.050 | .034 | −.084 |
| Participant minority status | .000 | .086 | .000 |
| Participant self-reported physical healthb | −.194 | .036 | −.313*** |
| Participant children’s problems | .047 | .041 | .061 |
| Mother age | .006 | .007 | .064 |
| Siblings living near mother | −.013 | .017 | −.042 |
| Mother ADL status | .171 | .080 | .126* |
| Mother problems | .093 | .031 | .171** |
| Mother support received | .083 | .035 | .177** |
| Mother support provided | −.084 | .034 | −.187** |
| Mother marital status | −.020 | .029 | −.038 |
| Mother–child relational importancec | .046 | .041 | .063 |
| Interactions | |||
| Participant self-reported physical health × mother’s life problems | −.079 | .027 | −.161*** |
| Mother support provided × mother’s life problems | .037 | .018 | .107* |
Notes. N = 308, R 2 = .282. Covariates were mean centered. ADL = activities of daily living.
a1 = no high school; 2 = high school graduate; 3 = some college; 4 = college graduate; 5 = postgraduate.
b1 = poor; 2 = fair; 3 = good; 4 = very good; 5 = excellent.
c1 = less important than that; 2 = among the 20 most important people; 3 = among the 10 most important people; 4 = among the six most important people; 5 = among the three most important people; 6 = the most important person in my life.
*p < .05. **p < .01. ***p < .001.
First, we examined the personal resource of self-reported physical health. Significant interactions were found for offspring’s self-reported physical health and mother’s problems (B = −.079, p < . 01; Figure 1). Participants whose mothers had fewer problems generally reported low levels of depressive symptoms. Participants who reported that their mothers had high amounts of problems had higher levels of depressive symptoms when they had low self-reported physical health. Participants who indicated that their mothers had more life problems demonstrated lower levels of depressive symptoms when they had high self-reported physical health.
Figure 1.
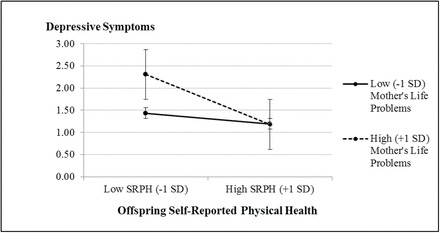
Self-reported physical health and mother’s life problems for participant depressive symptoms.
Next, we explored family support as a resource and found that the association between mother’s life problems and offspring depressive symptoms was moderated by the amount of support that the mother provided to the participant (B = .037, p < .05; Figure 2). For participants whose mothers had low problems, receiving more support from their mother was associated with lower depressive symptoms while receiving low support was associated with increased depressive symptoms. For participants whose mothers had more life problems, the amount of support their mothers provided had a small negative association with offspring depressive symptoms.
Figure 2.
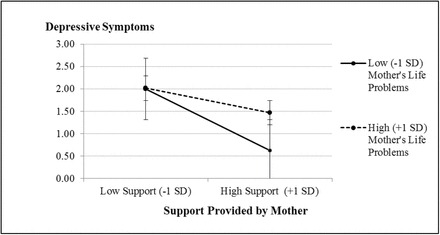
Support provided by the target’s mother and mother’s life problems for participant depressive symptoms.
Post Hoc Analysis
We conducted post hoc analyses in order to examine the stability of our findings. We compared additional models using participants who had both living parents and participants who had only a living father to our original model examining participants with only a living mother. When we ran these models, we saw no interactions and no main effects for offspring depressive symptoms. These results are consistent with the notion that a sole-surviving father is more likely to be remarried and thus is less of a burden to his adult children. It is also possible that having a spouse may reduce the impact of parents’ problems on children. We also ran a correlation to examine the extent to which mother’s problems were associated with ADL status and thus the need for ongoing care. We found a positive yet small correlation r(306) = .18, p < .01, between ADL status and mother’s problems; this confirms that life problems reported are not strongly associated with need for assistance with ADL.
Discussion
Researchers have extensively examined the implications of parent’s chronic health issues on child well-being, but less is known about how aging mother’s life problems relate to the mental health of their middle-aged offspring. Our study provides a critical extension of existing research into this important developmental period that is characterized by combined demands of family, work, and health. Midlife is a time in which coping resources and protective factors are particularly advantageous (Dainese et al., 2011). This study adds to the growing body of research that explores problems experienced among older adults (Tse, Hong, Wang, & Cunningham-Williams, 2012; Waite, Laumann, Das, & Schumm, 2009) and also illuminates how problems influence the parent–child relationship (Fingerman et al., 2012)
We utilized a sample of middle-aged, non-caregiver, offspring with a sole-surviving mother. We assessed several domains of problems that participants indicated their mother had experienced in the past 2 years. Although the problems explored in this study may be temporary in their effects and time limited in comparison to chronic illness or other major life events, they nonetheless occur frequently and have potential to influence the family system (Greenfield & Marks, 2006). When analyzed within the framework of COR theory, both self-reported health and maternal support moderate the relationship between offspring depressive symptoms and the problems experienced by a sole-surviving mother.
Self-reported physical health is a personal resource that proved to moderate this relationship. When mother’s life problems were high, participants with lower self-reported physical health indicated more severe depressive symptoms. This was not the case with participants who had high levels of self-reported physical health; those who reported better health had lower levels of depressive symptoms even when their mother experienced more problems. These results are consistent with Grossman’s (1972) concept of Health Capital that positions “good health” as a commodity; in this case, good health may serve as an individual coping resource, whereas offspring in poor health could be more vulnerable to internalizing their mother’s problems. Participants with lower self-reported physical health may feel overwhelmed by the additional demands, perceived or actual, associated with maternal problems. Given the reciprocal nature of parent–child depression (Timko et al., 2009), we expected that parents with fewer problems would have children with lower levels of depressive symptoms. This was true for participants who also had low levels of physical health. Offspring who indicated low levels of physical health had higher levels of depressive symptoms when their mother had more problems. When participants reported high levels of physical health, they had fewer depressive symptoms even when their mother had high levels of problems. In contrast, when mother’s problems were low, offspring reported lower levels of depressive symptoms with only slightly higher levels of depressive symptoms when self-reported health was low.
Consistent with past literature that utilizes COR theory (Seiger & Wiese, 2009), we considered family support as a resource that may buffer the relationship between mother’s problems and offspring depressive symptoms. Specifically, we found a significant interaction between the amount of support provided by the mother and mother’s problems for participant depressive symptoms. When participants reported having a mother with high problems who also provided them with high levels of support, they reported fewer depressive symptoms than when their mother provided them with low levels of support. A similar, yet not as substantial, pattern emerges for participants who reported fewer maternal problems. These results also build off research that has shown the benefits of intergenerational support exchanges (Merz, Consedine, Schulze, & Schuengel, 2009). Past research shows that offspring receive more assistance from parents when they have greater needs (Fingerman et al., 2009); our results show that older parents give support to their offspring despite their own problems.
Although problems experienced by aging mothers are associated with the depressive symptoms of their middle-aged offspring, our results indicate that personal health and family support resources buffer this relationship. This study extends the theoretical framework of COR and addresses the relatively understudied association between depressive symptoms of middle-aged offspring and maternal problems. In effect, these results add to our understanding of the function of differential moderators of parent–child well-being.
Limitations and Future Directions
Several features of the study design, method, and sample limit these results. We only utilize the reports of offspring to gather information about their mothers. Thus, it is possible that mothers experienced more problems than their offspring were aware of. Aging parents may not disclose problems to their children, such as sexual or financial abuse, in an attempt to avoid placing burden on their offspring. Next, the present study only explores two of many potential resources that serve as moderators of maternal problems on offspring depressive symptoms. Although we illuminate the importance of the particular resources of self-reported health and family support, there are many other individual and family resources that have yet to be explored within the context of parent problems. Our study also cannot provide any results about the nature or the impact of paternal problems on offspring depressive symptoms. We could not produce these results due in part to the small sample size of offspring with living fathers and chose to focus on offspring with a sole-surviving mother. Although we controlled for the number of siblings living geographically near the participant’s mother, this cannot be interpreted as a proxy for sibling support; a direct measure of sibling support would have strengthened our results.
Given these limitations, we have several suggestions pertaining to future research concerning the differential impact of parental problems on middle-aged offspring. First, it would be useful to look closer at the specific types of life problems as well as the severity of the problems experienced. We were unable to do this in part because of the relatively low frequency of problems; however, a sample with higher prevalence of problems would allow for a more in-depth understanding of specific problems. The two most common problems reported (experiencing a death and health problem/injury) would be a useful starting point in this exploration. Researchers may also focus on the disclosure patterns of problems, particularly between aging parents and their offspring. By utilizing reports of both aging mothers and middle-aged children, researchers may gain a more accurate measure of mother’s life problems and the extent to which children have an accurate understanding of their mother’s problems. Furthermore, a broader examination of family and individual resources may prove useful to this area of research. A greater understanding of how parent problems in late life affect their adult children would be highly useful to aging families and researchers.
Funding
This work was supported by grant R01 AG027769, “The Family Exchanges Study 2” (principal investigator: K. L. Fingerman, PhD), from National Institute of Aging as well as the MacArthur Network on an Aging Society (John W. Rowe, Network Director). This research also was supported by grant, 5 R24 HD042849, from Population Research Center, awarded to the Population Research Center at The University of Texas at Austin by the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
References
- Amirkhanyan A. A., Wolf D. A. (2006). Parent care and the stress process: Findings from panel data. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 61, S248–S255. doi:10.1093/geronb/61.5.S248 [DOI] [PubMed] [Google Scholar]
- Birditt K. S., Fingerman K. L., Zarit S. H. (2010). Adult children’s problems and successes: Implications for intergenerational ambivalence. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 65B, 145–153. doi:10.1093/geronb/gbp125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanchard-Fields F., Stein R., Watson T. L. (2004). Age differences in emotion-regulation strategies in handling everyday problems. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 59, P261–P269. doi:10.1093/geronb/59.6.P261 [DOI] [PubMed] [Google Scholar]
- Boyd R. C., Waanders C. (2013). Protective factors for depression among African American children of predominantly low-income mothers with depression. Journal of Child and Family Studies, 22, 85–95. doi:10.1007/s10826-012-9588-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley R. H., Corwyn R. F. (2002). Socioeconomic status and child development. Annual Review of Psychology, 53, 371–399. doi:10.1146/annurev.psych.53.100901.135233 [DOI] [PubMed] [Google Scholar]
- Burholt V., Wenger G. C. (1998). Differences over time in older peoples’ relationships with children and siblings. Ageing and Society, 18, 537–562. doi:10.1017/S0144686X98007090 [Google Scholar]
- Cichy K. E., Stawski R. S., Almeida D. M. (2013). A double-edged sword: Race, daily family support exchanges, and daily well-being. Journal of Family Issues. Advanced online publication. doi:10.1177/0192513X13479595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cleary P. D., Zaborski L. B., Ayanian J. Z. (2004). Sex differences in health over the course of mid-life. In Brim O. G., Ryff C. D., Kessler R. C. (Eds.), How healthy are we?: A national study of well-being at midlife (pp. 37–63). Chicago, IL: University of Chicago Press. [Google Scholar]
- Dainese S. M., Allemand M., Ribeiro N., Bayram S., Martin M., Ehlert U. (2011). Protective factors in midlife: How do people stay healthy? GeroPsych: The Journal of Gerontopsychology and Geriatric Psychiatry, 24, 19–29. doi:http://dx.doi.org/10.1024/1662-9647/a000032 [Google Scholar]
- Dallaire D. H. (2007). Children with incarcerated mothers: Developmental outcomes, special challenges and recommendations. Journal of Applied Developmental Psychology, 28, 15–24. doi:10.1016/j.appdev.2006.10.003 [Google Scholar]
- Derogatis L. R. (2000). Brief symptom inventory. In Rush A. J. American Psychiatric Association (Eds.), Handbook of psychiatric measures (pp. 84–86) Washington, DC: American Psychiatric Association. [Google Scholar]
- Dodge K. A. (1990). Developmental psychopathology in children of depressed mothers. Developmental Psychology, 26, 3–6. doi:10.1037/0012-1649.26.1.3 [Google Scholar]
- Fingerman K. L., Cheng Y., Birditt K., Zarit S. H. (2012). Only as happy as the least happy child: Multiple grown children’s problems and successes and middle-aged parents’ well-being. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 67, 184–193. doi:10.1093/geronb/gbr086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fingerman K. L., Miller L. M., Birditt K. S., Zarit S. H. (2009). Giving to the good and the needy: Parental support of grown children. Journal of Marriage and the Family, 71, 1220–1233. doi:10.1111/j.1741-3737.2009.00665.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman S. H., Gotlib I. H. (1999). Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review, 106, 458–490. doi:10.1037/0033-295X.106.3.458 [DOI] [PubMed] [Google Scholar]
- Greenfield E. A., Marks N. F. (2006). Linked lives: Adult children’s problems and their parents’ psychological and relational well- being. Journal of Marriage and Family, 68, 442–454. doi:10.1111/j.1741-3737.2006.00263.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossman M. (1972). On the concept of health capital and the demand for health. Journal of Political Economy, 80, 223–255. doi:10.1086/259880 [Google Scholar]
- Hobfoll S. E. (1989). Conservation of resources: A new attempt at conceptualizing stress. American Psychologist, 44, 513–524. doi:10.1037/0003-066X.44.3.513 [DOI] [PubMed] [Google Scholar]
- Hoyert D. L., Xu J. Q. (2012). Deaths: Preliminary data for 2011: National vital statistics reports (Vol. 61, No. 6). Hyattsville, MD: National Center for Health Statistics. [PubMed] [Google Scholar]
- Keyes C. L. M., Westerhof G. J. (2012). Chronological and subjective age differences in flourishing mental health and major depressive episode. Aging & Mental Health, 16, 67–74. doi:10.1080/13607863.2011.596811 [DOI] [PubMed] [Google Scholar]
- Kim Y., Wellisch D. K., Spillers R. L.(2008). Effects of psychological distress on quality of life of adult daughters and their mothers with cancer. Psycho-Oncology, 17, 1129–1136. doi:10.1002/pon.1328 [DOI] [PubMed] [Google Scholar]
- Kohl P. L., Kagotho J. N., Dixon D. (2011). Parenting practices among depressed mothers in the child welfare system. Social Work Research, 35, 215–225. doi:10.1093/swr/35.4.215 [Google Scholar]
- Letourneau N., Young C., Secco L., Stewart M., Hughes J., Critchley K. (2011). Supporting mothering: Service providers’ perspectives of mothers and young children affected by intimate partner violence. Research in Nursing & Health, 34, 192–203. doi:10.1002/nur.20428 [DOI] [PubMed] [Google Scholar]
- Lin W. F., Chen L. H., Li T. (2013). Adult children’s caregiver burden and depression: The moderating roles of parent–child relationship satisfaction and feedback from others. Journal of Happiness Studies, 14, 673–687. doi:10.1007/s10902-012-9348-0 [Google Scholar]
- Low N., Dugas E., Constatin E., Karp I., Rodriguez D., O’Loughlin J. (2012). The association between parental history of diagnosed mood/anxiety disorders and psychiatric symptoms and disorders in young adult offspring. BMC Psychiatry, 12, 188–195. doi:10.1186/1471-244X-12-188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markowitz J. C. (2008). Depressed mothers, depressed children. The American Journal of Psychiatry, 165, 1086–1088. doi:10.1176/appi.ajp.2008.08060861 [DOI] [PubMed] [Google Scholar]
- Marks N. F., Bumpass L. L., Jun H. (2004). Family roles and well-being during the middle life course. In Brim O. G., Ryff C. D., Kessler R. C. (Eds.), How healthy are we?: A national study of well-being at midlife (pp. 514–549). Chicago, IL: University of Chicago Press. [Google Scholar]
- Marks N. F., Lambert J. D., Jun H., Song J. (2008). Psychosocial moderators of the effects of transitioning into filial caregiving on mental and physical health. Research on Aging, 30, 358–389. doi:10.1177/0164027507312998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLoyd V. C. (1998). Socioeconomic disadvantage and child development. The American Psychologist, 53, 185–204. doi:10.1037/0003-066X.53.2.185 [DOI] [PubMed] [Google Scholar]
- Meadows-Oliver M. (2009). Adolescent mothers’ experiences of caring for their children while homeless. Journal of Pediatric Nursing, 24, 458–467. doi:10.1016/j.pedn.2008.06.007 [DOI] [PubMed] [Google Scholar]
- Merz E., Consedine N. S., Schulze H., Schuengel C. (2009). Wellbeing of adult children and ageing parents: Associations with intergenerational support and relationship quality. Ageing & Society, 29, 783–802. doi:10.1017/S0144686X09008514 [Google Scholar]
- Murray L., Sinclair D., Cooper P., Ducournau P., Turner P., Stein A. (1999). The socioemotional development of 5-year-old children of postnatally depressed mothers. Journal of Child Psychology and Psychiatry, 40, 1259–1271. doi:10.1017/S002196309900476X [PubMed] [Google Scholar]
- Myers B. J., Smarsh T. M., Amlund-Hagen K., Kennon S. (1999). Children of incarcerated mothers. Journal of Child and Family Studies, 8, 11–25. doi:10.1023/A:1022990410036 [Google Scholar]
- Raveis V. H., Pretter S. (2005). Existential plight of adult daughters following their mother’s breast cancer diagnosis. Psycho-Oncology, 14, 49–60. doi:10.1002/pon.819 [DOI] [PubMed] [Google Scholar]
- Riffin C., Suitor J. J., Reid M. C., Pillemer K. (2012). Chronic pain and parent-child relations in later life: An important, but understudied issue. Family Science, 3, 75–85. doi:10.1080/19424620.2012.707619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossi A. S., Rossi P. H. (1990). Of human bonding: Parent-child relations across the life course. New York, NY: Aldine de Gruyter. [Google Scholar]
- Rossi A. S., Rossi P. H. (1991). Normative obligations and parent-child help exchange across the life course. In Pillemer K., McCartney K. (Eds.), Parent-child relations throughout life (pp. 201–224). Hillsdale, NJ: Erlbaum. [Google Scholar]
- Seiger C. P., Wiese B. S. (2009). Social support from work and family domains as an antecedent or moderator of work–family conflicts? Journal of Vocational Behavior, 75, 26–37. doi:10.1016/j.jvb.2009.03.001 [Google Scholar]
- Steinhausen H., Mas S. D., Ledermann C., Metzke C. W. (2006). Risk factors for the development of emotional and behavioural problems in children born to drug-dependent mothers. European Child & Adolescent Psychiatry, 15, 460–466. doi:10.1007/s00787-006-0568-x [DOI] [PubMed] [Google Scholar]
- Street H., O’Connor M., Robinson H. (2007). Depression in older adults: Exploring the relationship between goal setting and physical health. International Journal of Geriatric Psychiatry, 22, 1115–1119. doi:10.1002/gps.1797 [DOI] [PubMed] [Google Scholar]
- Timko C., Cronkite R. C., Swindle R., Robinson R. L., Sutkowi A., Moos R. H. (2009). Parental depression as a moderator of secondary deficits of depression in adult offspring. Child Psychiatry and Human Development, 40, 575–588. doi:10.1007/s10578-009-0145-x [DOI] [PubMed] [Google Scholar]
- Tolkacheva N., van Groenou M. B., van Tilburg T. (2010). Sibling influence on care given by children to older parents. Research on Aging, 32, 739–759. doi:10.1177/0164027510383532 [Google Scholar]
- Tse S., Hong S., Wang C., Cunningham-Williams R. M. (2012). Gambling behavior and problems among older adults: A systematic review of empirical studies. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 67, 639–652. doi:10.1093/geronb/gbs068 [DOI] [PubMed] [Google Scholar]
- Waite L. J., Laumann E. O., Das A., Schumm L. P. (2009). Sexuality: Measures of partnerships, practices, attitudes, and problems in the national social life, health, and aging study. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 64(Suppl. 1), i56–i66. doi:10.1093/geronb/gbp038 [DOI] [PMC free article] [PubMed] [Google Scholar]


