Abstract
Background
Therapeutic hypothermia (TH) attenuates reperfusion injury in comatose survivors of cardiac arrest. The utility of TH in patients with non-shockable initial rhythms has not been widely accepted. We sought to determine whether TH improved neurologic outcome and survival in post-arrest patients with non-shockable rhythms.
Methods and Results
We identified 519 patients after in- and out-of-hospital cardiac arrest with non-shockable initial rhythms from the Penn Alliance for Therapeutic Hypothermia (PATH) registry between 2000–2013. Propensity score matching was used. Patient and arrest characteristics used to estimate the propensity to receive TH were age, sex, location of arrest, witnessed arrest, and duration of arrest. To determine the association between TH and outcomes, we created two multivariable logistic models controlling for confounders. Of 201 propensity score matched pairs, mean age was 63±17 years; 51% were male; and 60% had an initial rhythm of pulseless electrical activity. Survival to hospital discharge was greater in patients who received TH (17.6% vs. 28.9%; p<0.01), as was discharge CPC of 1–2 (13.7% vs 21.4%; p= 0.04). In adjusted analyses, patients who received TH were more likely to survive (OR 2.8, 95% CI: 1.6–4.7) and have better neurologic outcome (OR 3.5, 95% CI: 1.8–6.6) than those that did not receive TH.
Conclusions
Using propensity score matching, we found patients with non-shockable initial rhythms treated with TH had better survival and neurologic outcome at hospital discharge than those who did not receive TH. Our findings further support the use of TH in patients with initial non-shockable arrest rhythms.
Keywords: Heart arrest, Cardiopulmonary resuscitation, Resuscitation, Therapeutic Hypothermia
INTRODUCTION
Therapeutic hypothermia (TH) or targeted temperature management (TTM) has been widely accepted as the only known therapy to impart neuroprotection to the post-cardiac arrest patient with anoxic injury resulting in coma after return of spontaneous circulation (ROSC). The landmark studies that documented this phenomenon were performed on comatose patients after an out-of-hospital cardiac arrest (OHCA) with an initial shockable rhythm of ventricular fibrillation (VF) or pulseless ventricular tachycardia (pVT).1,2 The incidence of initial shockable arrest rhythms, specifically VF and pVT, has been declining over recent years while the incidence of cardiac arrest continues to be estimated at approximately 530,00 individuals per year in the United States alone.3,4 This phenomenon results in a larger proportion of individuals who have suffered a cardiac arrest due to a non-shockable initial rhythm and who might benefit from aggressive post-resuscitation care. Despite this increasing burden of disease related to non-shockable arrests, randomized controlled trials to examine the utility of TH in patients with non-shockable rhythms (pulseless electrical activity (PEA) and asystole) have not been completed, and available observational studies have yielded conflicting results. Nielsen et al. presented the only randomized controlled trial in post-cardiac arrest care that included non-shockable initial rhythms with the objective to compare targeted temperature management (TTM) at 33°C vs. 36°C; however, the question of benefit for patients with initial non-shockable rhythms was not specifically addressed and the study did not include a control group that did not receive active temperature management.5
Multiple retrospective cohort studies have examined the association between TH and neurologic outcomes in patients who arrest with non-shockable rhythms; however, the results have been varied, thus reinforcing the controversy surrounding the use of TH in this cohort of patients. Specifically, the association between TH use in the cohort of patients with non-shockable rhythms and good neurologic outcome has yielded both a positive association6 as well as no effect,7 leaving experts in the field of resuscitation requesting more evidence and resulting in a decision by the American Heart Association to render TH a level IIB recommendation in patients who have ROSC after a cardiac arrest with an initial rhythm of PEA or asystole (in stark contrast to the recommendation made for shockable rhythms (Level Ia)).8
We sought to further explore the association between TH and neurologic outcomes in patients with an initial non-shockable rhythm by simulating a randomized-controlled trial utilizing a propensity score to create our treatment and control groups.9 We hypothesized that patients with a non-shockable rhythm treated with TH would have better neurologic outcomes (defined as a Cerebral Performance Category (CPC) of 1 or 2) at hospital discharge versus their propensity score matched counterparts who did not receive TH.
METHODS
Study design and setting
This is a retrospective cohort study utilizing data from the Penn Alliance for Therapeutic Hypothermia (PATH) Registry. The PATH registry was created as a national, on-line repository for patient data from multiple centers utilizing TH in the management of post-cardiac arrest patients. This was a multi-center study evaluating patient data from 16 institutions that currently contribute to the PATH registry. This collaborative study was approved by the University of Pennsylvania Institutional Review Board (IRB), and each center obtained site specific IRB approval prior to their participation in the PATH registry.
Study cohort
Patients enrolled in this study were age 18 or older, had suffered either an in-hospital or out-of-hospital non-traumatic cardiac arrest (OHCA) with an initial non-shockable cardiac arrest rhythm of either PEA or asystole. All patients were comatose after return of spontaneous circulation, and therefore, eligible for TH. Patients in this cohort did not have an active Do Not Resuscitate order.
Treatment
Patients either underwent TH according to the respective institutional protocols (all with standard goal temperatures of 32°–34°C in accordance with AHA guidelines) or received standard post-arrest care without the application of TH.
Data collection
Patient specific data were added to the online registry by trained data abstractors at each contributing site. Demographic data were obtained for each subject, including age at arrest, sex, and race. Arrest characteristics were collected including location of arrest (in- vs. out-of-hospital), initial non-shockable rhythm (asystole vs. PEA), witnessed arrest, administration of bystander cardiopulmonary resuscitation (CPR), and finally the “duration of arrest”. Duration of arrest is defined as the time from pre-hospital notification for OHCA, or activation of a “code call” for in-hospital cardiac arrest till ROSC respectively. The primary outcome was neurologic outcome at hospital discharge as characterized by CPC dichotomized into “good” outcome (CPC 1–2) or “poor” outcome (CPC 3–5),9–11 and a secondary outcome analyzed was survival to hospital discharge.
Statistical analysis
We described the baseline characteristics of the study population utilizing frequencies for categorical variables and means with standard deviations for continuous variables. Comparisons for continuous data were made via Student’s t-tests or Mann-Whitney U tests, and chi2 testing was applied to categorical data.
To control for confounding by indication, we utilized a propensity score (PS) matching method to determine a score for each patient’s propensity to receive TH.12,13 A propensity score, defined as the conditional probability of being treated given the covariates, was created utilizing a nonparsimonious logistic regression model accounting for patient and arrest characteristics identified a priori based on prior literature.14 Using a specialized statistical package (psmatch2), scores were created and cases were matched on the propensity score in a 1:1 block using nearest neighbor matching algorithm with replacement. Replacement allows for a unit (patient) to be selected more than once, thus reducing the distance between the matched units and allowing each pair to be matched to it’s closest neighbor. After deriving the PS and completing the matched pairs, post-estimation diagnostics were applied to ensure balance between the two cohorts, that use of the propensity score matching led to a reduction of bias (as opposed to not using a propensity score match), and to identify outliers for exclusion to avoid undue bias. Utilizing the propensity score matched cohort, we created multivariable conditional logistic regression models to determine the association between 1.) TH and neurologic outcome (cerebral performance category (CPC) dichotomized into “good” (CPC 1 and 2) and “poor” (CPC 3–5)) and 2.) TH and survival to hospital discharge, accounting for relevant confounding variables as identified on univariate analysis. All analysis was completed using basic statistical software (STATA v.12, College Station, TX). For propensity score derivation and matching, we utilized the STATA program psmatch2 (E. Leuven and B. Sianesi. (2003). “PSMATCH2: Stata module to perform full Mahalanobis and propensity score matching, common support graphing, and covariate imbalance testing”. http://ideas.repec.org/c/boc/bodone/s432001.html).
RESULTS
Between 2000 and 2013, 519 patients in the PATH registry suffered a cardiac arrest due to a non-shockable initial rhythm (PEA or asystole), had return of spontaneous circulation and were comatose at hospital admission. Of the entire cohort of patients, 50.5% (262) of comatose survivors underwent TH according to their respective hospital protocols. Table 1 reports the demographic and arrest characteristics for patients who underwent TH and those in the standard care (no TH) group. Of note, patients who underwent TH were younger (62 vs. 69 yrs of age, p<0.001), had longer durations of arrest (23 vs. 13 min, p<0.001), and had a higher incidence of asystole as their primary rhythm (45% vs. 35%, p<0.001). Patients who underwent TH were more frequently patients who had suffered an out of hospital cardiac arrest (82% vs. 39%, p<0.001), which most likely reflects a preference for one aspect of the patient population studied in the landmark trials of 2002.1,2 The median time to hospital discharge varied and was highest (19.0 days, (Q1, Q3) 13.0–25.7 days) in the cohort of patients who survived after TH and lowest in the cohort that died without TH (0.9 days, (Q1, Q3) 0.2–2.3 days).
Table 1.
Patient demographics and arrest characteristics for patients who were treated with TH versus those who were treated with standard post-arrest care (that excluded TH).
| Standard Care (No TH) (n=257) | Treated with TH (n=262) | p-value† | |
|---|---|---|---|
| Age, y (Q1, Q3) | 69 (55.5, 80) | 62 (49, 73) | <0.001 |
| Duration of arrest, min (Q1, Q3) | 13 (8, 28) | 23 (14, 36) | <0.001 |
| Male Sex, No. (%) | 127 (49) | 143 (55) | 0.239 |
| OHCA, No. (%) | 100 (39) | 216 (82) | <0.001 |
| Witnessed arrest, No. (%)* | 215 (84) | 182 (70) | <0.001 |
| Initial rhythm, Asystole (%) | 89 (35) | 119 (45) | <0.001 |
12 patients in this cohort had missing data for “witnessed arrest”.
P-values derived by comparing patient groups with Student’s t-tests or Mann-Whitney U for continuous variables and chi-square for categorical variables.
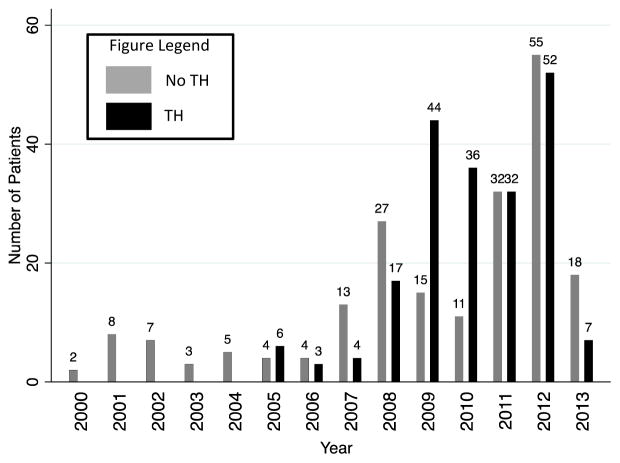
Propensity scores were calculated based on the factors influencing the likelihood of receiving TH: age, sex, initial rhythm, witnessed arrest, duration of arrest, and location of arrest.14 After generating propensity scores, 291 patients were matched to form 201 pairs. One outlier patient was excluded after post-estimation testing showed that their inclusion caused bias. Figure 1 represents the distribution of patients enrolled over time (calendar year) for the propensity score matched cohort. Table 2 describes the propensity score matched cohort, where there is no statistical difference between the demographic and arrest characteristics of the TH and standard care cohorts.
Figure 1.
Distribution of post-arrest patients with initial non-shockable rhythms enrolled over time (year).
Table 2.
Propensity score matched cohort demographics and arrest characteristics.
| Standard Care (NO TH) (n=201) | Treated with TH (n=201) | p-value† | |
|---|---|---|---|
| Age, y (Q1, Q3) | 62 (50, 70) | 60 (48, 72) | 0.49 |
| Duration of arrest, min (Q1, Q3) | 25 (9, 36) | 23 (14, 36) | 0.63 |
| Male Sex, No. (%) | 113 (56) | 108 (54) | 0.62 |
| OHCA, No. (%) | 163 (81) | 159 (79) | 0.62 |
| Witnessed arrest, No. (%)* | 147 (73) | 137 (68) | 0.38 |
| Initial rhythm, Asystole (%) | 77 (38) | 91 (45) | 0.16 |
4 patients in this cohort had missing data for “witnessed arrest”.
P-values derived by comparing patient groups with Mann-Whitney U for continuous variables and chi-square for categorical variables.
In univariate analysis, we found that female gender (OR 0.50; 95% CI: 0.28 – 0.88), PEA as the initial rhythm (OR 2.04; 95% CI: 1.14 – 3.66), witnessed arrest (OR 3.7; 95% CI: 1.78 – 7.90) and duration of arrest in minutes (OR 0.94; 95% CI: 0.92 – 0.96) are independently associated with neurologic outcome. In the propensity matched cohort, 29% of patients who underwent TH survived to hospital discharge versus 15% that did not receive hypothermia (p=0.001). In this same population, 21% of patients who underwent TH survived to hospital discharge with a CPC 1 or 2 in comparison to only 10% in the cohort who did not receive TH (p=0.003). In multivariate analysis (Table 3), we found that TH was associated with improved neurologic outcomes for patients who suffered cardiac arrest due to a non-shockable rhythm 3.5 fold (95% CI: 1.8–6.6). Additionally, we found that TH was associated with improved survival to hospital discharge in this same cohort with an odds ratio of 2.8 (95% CI: 1.6–4.7).
Table 3.
Outcomes for the multivariate analysis of the propensity-matched cohort of patients treated with and without therapeutic hypothermia.
| Status at Hospital Discharge | Adjusted Odds Ratio† |
|---|---|
| Survival | |
| Total cohort | 2.8 (95% CI: 1.6–4.7) |
| IHCA | 2.2 (95% CI: 0.8–6.2) |
| OHCA | 3.1 (95% CI: 1.6–5.8) |
| Neurologic Recovery* | |
| Total cohort | 3.5 (95% CI: 1.8–6.6) |
| IHCA | 4.2 (95% CI 1.2–14.9) |
| OHCA | 2.1 (95% CI 1.0–4.4) |
CPC 1 or 2;
variables included in multivariable model include age, sex, witnessed arrest, initial rhythm (PEA/Asystole), and duration of arrest.
We completed a subgroup analysis of in- versus out-of-hospital cardiac arrest, given that the survival rate for the two cohorts is markedly different.15,16 The propensity score matched cohort was separated by location of arrest and novel propensity scores were generated for each cohort using the same variables as previously defined. After matching, 159 pairs of OHCA patients and 42 pairs of IHCA patients were analyzed. Using multivariable logistic regression to analyze these two subgroups separately (table 3), we found that regardless of location of arrest, patients who underwent TH were more likely to survive to hospital discharge neurologically intact (OHCA: OR 2.1, 95% CI 1.01–4.36, IHCA: OR 4.23, 95% CI 1.20–14.94). Despite location of arrest, patients with initial non-shockable arrest rhythms benefited from treatment with TH.
DISCUSSION
The findings suggest that TH is a beneficial treatment for comatose post-arrest patients when the initial rhythm was either PEA or asystole. Through using propensity score matching in in a retrospective registry of post-cardiac arrest patients with non-shockable initial rhythms (both PEA and asystole), patients who underwent TH had increased rates of survival with good neurologic outcome (OR 3.5, 95% CI:1.8–6.6) versus those who did not receive TH. Additionally, when completing a subgroup analysis of in- versus out-of hospital arrest, patients treated with TH uniformly had better neurologic outcomes than those who were not. This study is the first study to address the specific question of utility of TH in this patient population using advanced statistical methodology to control for confounding by indication and to define a study population that is statistically uniform between the treatment cohort and standard care arm. These results lend support to a broadening of indications for TH in comatose post-arrest patients with initial non-shockable rhythms.
The randomized trials of 2002 established precedence for the use of TH in post-cardiac arrest care. These two studies focused primarily on patients who suffered an out-of-hospital cardiac arrest due to VF or pVT.1,2 This fact has lead to much controversy in recent years. Many clinicians have expanded the use of TH to comatose patients regardless of initial rhythm (VF, pVT, PEA, asystole) or location of arrest (out-of-hospital vs. in-hospital), searching for a clinical strategy to improve outcomes in this critically ill patient population. Simultaneously, many clinicians have questioned the utility of TH in patients who suffer an arrest due to a rhythm that is not VF or pVT, citing the fact that the evidence to support TH use did not arise from a study of this population specifically. Since that time, investigators have sought to evaluate the use of TH in all rhythms via retrospective single institution studies and large registry studies, with the majority of those not endorsing TH in patients with non-shockable rhythms continuing to call for a randomized controlled trial to prove efficacy. Clinical investigators are reticent to design such a trial, as standard of care in many cardiac arrest centers nationwide employs TH in patients with all presenting rhythms who achieve return of spontaneous circulation. This unfortunately creates a conundrum where clinicians are divided amongst those who continue to call for more evidence and those who find it ethically questionable to randomize patients into a study where patients may have care withheld that they would have received were they to not enroll in the study. This led our study group to look to advanced statistical methodology in order to further investigate this topic.
Previous studies have found variability in the association between TH and neurologic survival in patients who suffer cardiac arrest due to non-shockable rhythms. In one large retrospective registry study, investigators found that TH was not associated with good neurologic outcome in patients with an initial non-shockable rhythm (OR 0.71; 95% CI 0.37–1.36).7 This study utilized multivariable logistic regression to determine the association between initial rhythm and the use of TH for all post-cardiac arrest patients admitted to a single tertiary care institution in Paris, France from 2000 to 2009. In contrast, a separate retrospective study conducted by Lundbye et al. determined that patients with initial non-shockable rhythms treated with TH had improved outcomes when compared to a historical cohort of cardiac arrest patients treated prior to the implementation of a TH protocol. That study, like our result, supports the use of TH in patients with initial non-shockable rhythms. The authors utilized data from a single institution with a total of 100 patients (52 in the TH cohort, 48 in the historical cohort) enrolled. Despite the small sample size, on adjusted analysis, patients treated with TH had significantly improved chance of neurologic recovery versus the historical cohort that did not receive TH (OR 5.65, 95% CI: 1.66–19.23). Both aforementioned studies were observational in nature, therefore, it is plausible that provider bias and confounding by indication may have affected which patients received TH. In our study, by matching based on propensity score, the control arm (no TH) and the interventional arm (treated with TH) were statistically uniform. This methodology was employed to reduce the role that selection bias may have on the final outcome, survival to hospital discharge neurologically intact.
Patients with initial non-shockable rhythms were not included in the study design of the landmark trials of 2002.1,2 However, in 2013 Nielsen et al. published a large multicenter RCT of out-of-hospital cardiac arrest patients with all initial rhythms treated with TTM at different maintenance temperatures (33°C vs. 36° C).5 Although not a primary study question, the authors did report a subgroup analysis where they found an unadjusted overall survival of 16.1% for patients with initial non-shockable rhythms. In comparison, this survival rate is considerably higher than some previously reported for patients with initial non-shockable rhythms ranging from 4.6–10%6,17 but less than that reported in a large database of TH patients, The Hypothermia Network, where 6 month survival for PEA patients was 23% and asystole patients was 27%.18
Despite established guidelines for the use of TH in patients who suffer cardiac arrest,8 adoption of this practice has been low, especially for in-hospital cardiac arrest patients19 and patients who arrest with initial non-shockable rhythms.7 This finding is surely influenced by current guidelines that continue to assign TH a class IIB recommendation in these populations. Undoubtedly, both subpopulations of patients require further investigation in order to increase our scientific knowledge of efficacy and continue to improve clinical outcome. Our findings provide further support for the use of TH in patients with initial non-shockable rhythms, given the lack of randomized controlled trial data, and should encourage its use in this patient population while awaiting data from randomized trials. In addition, if more widespread utilization of aggressive post-arrest care (including TH) in patients with initial non-shockable rhythms is implemented systematically and studied prospectively, further data will be obtained to optimize outcomes in this subpopulation of cardiac arrest patients, which is increasing in number each year.
LIMITATIONS
This study utilized advanced statistical methodology in order to limit confounding by indication as well as to create two study arms that had similar demographic and arrest characteristics. Despite every effort to minimize bias, we recognize that this methodology does not replace a randomized controlled trial; however, at this juncture this type of study may be the best means of ethically answering the proposed question.
We utilized data from the PATH registry, and therefore these outcomes are limited by the retrospective nature of the data as well as all other bias frequently encountered from large registry studies. The PATH registry is audited quarterly for trends, with established internal review to ensure validity of the data maintained in the registry.
When conducting our analysis to explore associations between TH and neurologic recovery, we accounted for arrest characteristics as well as patient demographics. One limitation was that we did not account for in-patient therapy, aside from TH. Specifically, our analysis did not account for the use of early percutaneous coronary intervention, which in the setting of ventricular dysrhythmia has been associated with improved outcomes from cardiac arrest20. Unfortunately, the literature to support PCI in non-shockable arrest rhythms is scarce. We do report lack of PCI data as a limitation in our analysis however, given limited data to support this practice we propose that the utilization of early PCI will undoubtedly be low in our cohort of patients who all arrested with initial nonshockable rhythms.
As is true in most retrospective studies of this nature, patients made “Do not resuscitate” (DNR) or who had “Withdrawal of life-sustaining therapy” (WLST) may alter the outcomes of both cohorts due to misclassification of the primary outcome, as strict neurologic prognostic algorithms have yet to be established and the reasons for such end of life decisions are not specifically known.
CONCLUSION
Via propensity score matching to create treatment and control cohorts, we found that patients who arrest with initial non-shockable rhythms (PEA and Asystole) have improved neurologic outcome when treated with TH versus those who do not receive therapeutic hypothermia after cardiac arrest. Our findings further support the use of TH in patients with initial non-shockable post-cardiac arrest rhythms and we encourage further investigation into the utility of neuro-protective strategies in this cohort of cardiac arrest patients.
Supplementary Material
Acknowledgments
Funding Sources: Dr. Perman was supported by an NIH T-32 training grant (5T32 NSO61779-05) for the duration of this research project.
Footnotes
Disclosures: None.
References
- 1.Mild Therapeutic Hypothermia to Improve the Neurologic Outcome after Cardiac Arrest. N Engl J Med. 2002;346:549–556. doi: 10.1056/NEJMoa012689. [DOI] [PubMed] [Google Scholar]
- 2.Bernard SA, Gray TW, Buist MD, Jones BM, Silvester W, Gutteridge G, Smith K. Treatment of Comatose Survivors of Out-of-Hospital Cardiac Arrest with Induced Hypothermia. N Engl J Med. 2002;346:557–563. doi: 10.1056/NEJMoa003289. [DOI] [PubMed] [Google Scholar]
- 3.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, de Ferranti S, Després JP, Fullerton HJ, Howard VJ, Huffman MD, Judd SE, Kissela BM, Lackland DT, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Matchar DB, McGuire DK, Mohler ER, 3rd, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Willey JZ, Woo D, Yeh RW, Turner MB American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation. 2015;131:e29–e322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 4.Merchant RM, Yang L, Becker LB, Berg RA, Nadkarni V, Nichol G, Carr BG, Mitra N, Bradley SM, Abella BS, Groeneveld PW American Heart Association Get With the Guideline-Resuscitation Investigators. . Incidence of treated cardiac arrest in hospitalized patients in the United States*. Crit Care Med. 2011;39:2401–2406. doi: 10.1097/CCM.0b013e3182257459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nielsen N, Wetterslev J, Cronberg T, Erlinge D, Gasche Y, Hassager C, Horn J, Hovdenes J, Kjaergaard J, Kuiper M, Pellis T, Stammet P, Wanscher M, Wise MP, Åneman A, Al-Subaie N, Boesgaard S, Bro-Jeppesen J, Brunetti I, Bugge JF, Hingston CD, Juffermans NP, Koopmans M, Køber L, Langørgen J, Lilja G, Møller JE, Rundgren M, Rylander C, Smid O, Werer C, Winkel P, Friberg H TTM Trial Investigators. Targeted Temperature Management at 33°C versus 36°C after Cardiac Arrest. N Engl J Med. 2013;369:2197–206. doi: 10.1056/NEJMoa1310519. Epub 2013 Nov 17. [DOI] [PubMed] [Google Scholar]
- 6.Lundbye JB, Rai M, Ramu B, Hosseini-Khalili A, Li D, Slim HB, Bhavnani SP, Nair SU, Kluger J. Therapeutic hypothermia is associated with improved neurologic outcome and survival in cardiac arrest survivors of non-shockable rhythms. Resuscitation. 2012;83:202–207. doi: 10.1016/j.resuscitation.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 7.Dumas F, Grimaldi D, Zuber B, Fichet J, Charpentier J, Pène F, Vivien B, Varenne O, Carli P, Jouven X, Empana JP, Cariou A. Is hypothermia after cardiac arrest effective in both shockable and nonshockable patients?: insights from a large registry. Circulation. 2011;123:877–886. doi: 10.1161/CIRCULATIONAHA.110.987347. [DOI] [PubMed] [Google Scholar]
- 8.Peberdy MA, Callaway CW, Neumar RW, Geocadin RG, Zimmerman JL, Donnino M, Gabrielli A, Silvers SM, Zaritsky AL, Merchant R, Vanden Hoek TL, Kronick SL American Heart Association. Part 9: Post–Cardiac Arrest Care 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122(18 suppl 3):S768–S786. doi: 10.1161/CIRCULATIONAHA.110.971002. [DOI] [PubMed] [Google Scholar]
- 9.Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet. 1975;1:480–484. doi: 10.1016/s0140-6736(75)92830-5. [DOI] [PubMed] [Google Scholar]
- 10.Brain Resuscitation Clinical Trial I Study group (BRCT-1) Randomized clinical study of thiopental loading in comatose survivors of cardiac arrest. N Engl J Med. 1986;314:397–403. doi: 10.1056/NEJM198602133140701. [DOI] [PubMed] [Google Scholar]
- 11.Becker LB, Aufderheide TP, Geocadin RG, Callaway CW, Lazar RM, Donnino MW, Nadkarni VM, Abella BS, Adrie C, Berg RA, Merchant RM, O’Connor RE, Meltzer DO, Holm MB, Longstreth WT, Halperin HR American Heart Association Emergency Cardiovascular Care Committee; Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Primary Outcomes for Resuscitation Science Studies A Consensus Statement From the American Heart Association. Circulation. 2011;124:2158–2177. doi: 10.1161/CIR.0b013e3182340239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.D’Agostino RB., Jr Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med. 1998;17:2265–2281. doi: 10.1002/(sici)1097-0258(19981015)17:19<2265::aid-sim918>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 13.Leon AC, Hedeker D, Teres JJ. Bias reduction in effectiveness analyses of longitudinal ordinal doses with a mixed-effects propensity adjustment. Stat Med. 2007;26:110–123. doi: 10.1002/sim.2458. [DOI] [PubMed] [Google Scholar]
- 14.Lindner T, Langørgen J, Sunde K, Larsen AI, Kvaløy JT, Heltne JK, Draegni T, Søreide E. Factors predicting the use of therapeutic hypothermia and survival in unconscious out-of-hospital cardiac arrest patients admitted to the ICU. Crit Care Lond Engl. 2013;17:R147. doi: 10.1186/cc12826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Daya MR, Schmicker RH, Zive DM, Rea TD, Nichol G, Buick JE, Brooks S, Christenson J, MacPhee R, Craig A, Rittenberger JC, Davis DP, May S, Wigginton J, Wang H Resuscitation Outcomes Consortium Investigators. Out-of-hospital cardiac arrest survival improving over time: Results from the Resuscitation Outcomes Consortium (ROC) Resuscitation. 2015;91:108–115. doi: 10.1016/j.resuscitation.2015.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Girotra S, Cram P, Spertus JA, Nallamothu BK, Li Y, Jones PG, Chan PS American Heart Association’s Get With the Guidelines®-Resuscitation Investigators. . Trends in survival after inhospital cardiac arrest. N Engl J Med. 2012;367:1912–1920. doi: 10.1056/NEJMoa1109148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kudenchuk PJ, Redshaw JD, Stubbs BA, Fahrenbruch CE, Dumas F, Phelps R, Blackwood J, Rea TD, Eisenberg MS. Impact of changes in resuscitation practice on survival and neurological outcome after out-of-hospital cardiac arrest resulting from nonshockable arrhythmias. Circulation. 2012;125:1787–1794. doi: 10.1161/CIRCULATIONAHA.111.064873. [DOI] [PubMed] [Google Scholar]
- 18.Nielsen N, Hovdenes J, Nilsson F, Nielsen N, Hovdenes J, Nilsson F, Rubertsson S, Stammet P, Sunde K, Valsson F, Wanscher M, Friberg H Hypothermia Network. Outcome, timing and adverse events in therapeutic hypothermia after out-of-hospital cardiac arrest. Acta Anaesthesiol Scand. 2009;53:926–934. doi: 10.1111/j.1399-6576.2009.02021.x. [DOI] [PubMed] [Google Scholar]
- 19.Mikkelsen ME, Christie JD, Abella BS, Kerlin MP, Fuchs BD, Schweickert WD, Berg RA, Mosesso VN, Shofer FS, Gaieski DF American Heart Association’s Get With the Guidelines-Resuscitation Investigators. . Use of therapeutic hypothermia after in-hospital cardiac arrest. Crit Care Med. 2013;41:1385–1395. doi: 10.1097/CCM.0b013e318287f2c4. [DOI] [PubMed] [Google Scholar]
- 20.Cronier P, Vignon P, Bouferrache K, Aegerter P, Charron C, Templier F, Castro S, El Mahmoud R, Lory C, Pichon N, Dubourg O, Vieillard-Baron A. Impact of routine percutaneous coronary intervention after out-of-hospital cardiac arrest due to ventricular fibrillation. Crit Care Lond Engl. 2011;15:R122. doi: 10.1186/cc10227. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.