Abstract
Introduction
Little is known about trends in national rates of injection-related skin and soft tissue infections (SSTI) and their relationship to the structural risk environment for heroin users. Use of Mexican-sourced “Black Tar” heroin, predominant in western US states, may have greater risk for SSTI compared with eastern US powder heroin (Colombian-sourced) due to its association with non-intravenous injection or from possible contamination.
Methods
Using nationally representative hospital admissions data from the Nationwide Inpatient Sample and heroin price and purity data from the Drug Enforcement Administration, we looked at rates of hospital admissions for opiate-related SSTI (O-SSTI) between 1993 and 2010. Regression analyses examined associations between O-SSTI and heroin source, form and price.
Results
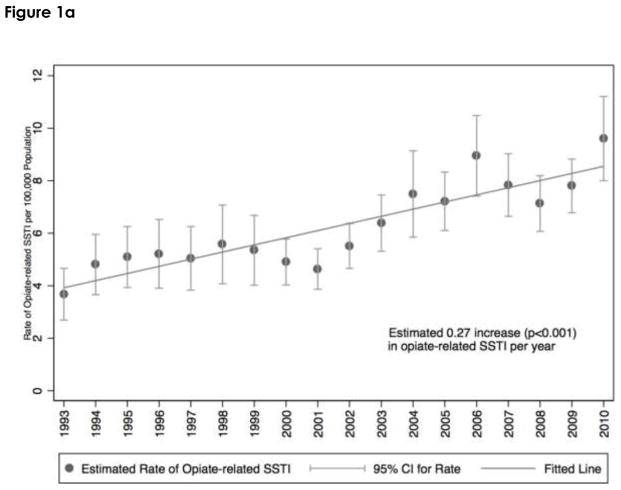
Hospitalization rates of O-SSTI doubled from 4 to 9 per 100,000 nationally between 1993 and 2010; the increase concentrated among individuals aged 20 to 40. Heroin market features were strongly associated with changes in the rate of SSTI. Each $100 increase in yearly heroin price-per–gram-pure was associated with a 3% decrease in the rate of heroin-related SSTI admissions. Mexican-sourced-heroin-dominant cities had twice the rate of O-SSTI compared to Colombian-sourced-heroin-dominant cities.
Discussion
Heroin-related SSTI are increasing and structural factors, including heroin price and source-form, are associated with higher rates of SSTI hospital admissions. Clinical and harm reduction efforts should educate heroin users on local risk factors, e.g., heroin type, promote vein health strategies and provide culturally sensitive treatment services for persons suffering with SSTI.
Keywords: Soft tissue infection, injection drug use, heroin, black tar heroin, drug markets, structural risk environment
1. INTRODUCTION
Bacterial skin and soft tissue infections (SSTI), specifically cellulitis and skin or soft tissue abscesses, are the most common reason for hospitalization of persons who inject drugs (PWID; Ciccarone et al., 2001; Ebright and Pieper, 2002) and carry high social burden and health care costs (Binswanger et al., 2000; Binswanger et al., 2008; Takahashi et al., 2007, 2010). Prevalence estimates of SSTI among PWID range widely: from 10% of PWID at a supervised injection program in Vancouver (Lloyd-Smith et al., 2008), 20% of PWID in Tijuana (Pollini et al., 2010), 24% of heroin PWID inpatients in Detroit (Crane et al., 1986), 32% of street sampled heroin PWID in San Francisco (Binswanger et al., 2000) to 34% of heroin injectors in Glasgow (Ramsay et al., 2010). Takahashi et al. (2010) estimate that 0.07% of all US non-Federal hospitalizations in the United States were due to SSTI among heroin users generating costs over $193 million in 2001 alone. In San Francisco, 7% of all hospital admissions at the large county hospital were for SSTI costing on average $9.9 million per fiscal year; of these cases 70% were in heroin injectors (Ciccarone et al., 2001). The individual burden of heroin-related SSTI in San Francisco has been described as a “hidden epidemic of suffering” (Ciccarone et al., 2000). SSTI have a negative impact on quality of life with persistent pain, mobility restrictions and stigmatization due to disfigurement and wound odor (Palfreyman et al., 2007; Pieper et al., 2007). Stigmatization in turn leads to non-adherence to medical care and self-care practices such as self-lancing abscesses (Bourgois and Schonberg, 2009; Ciccarone et al., 2000; Fink et al., 2013; Messac et al., 2013).
What little is known about the risk factors for SSTI among heroin PWID is focused on individual behaviors. Behavioral risks include type of drug injected (heroin and cocaine, i.e., speedball; Murphy et al., 2001a; Spijkerman et al., 1996), route of injection (subcutaneous or intramuscular vs intravenous; Binswanger et al., 2000; Murphy et al., 2001b) frequency of subcutaneous injection; Binswanger et al., 2000; Hope et al., 2016; Spijkerman et al., 1996) and reuse of syringes (Murphy et al., 2001b). HIV infection was an independent risk in one study (Spijkerman et al., 1996) but not another (Murphy et al., 2001b). Similarly skin cleaning prior to injection was seen as protective in a case-control study (Murphy et al., 2001b) but not so in a cross-sectional one (Binswanger et al., 2000). Type of drug injected is crucial with injection of heroin and speedball (heroin and cocaine) increasing (Lloyd-Smith et al., 2008; Murphy et al., 2001b) and injection of methamphetamine decreasing risk for SSTI (Phillips and Stein, 2010).
Moving beyond individual behavioral risks we consider the structural risk environment–a framework that conceptualizes individual behavior within wider social, environmental and political contexts in which harms result from interactions between macro- and micro-level forces (Rhodes, 2009). For heroin injectors the structural risk environment includes drug supply, i.e., heroin source, form and distribution, which moderates the relationship between individual risk behaviors and health. Risks emanate from global supply, e.g., poppy cultivation, trafficking and interdiction, down to local settings e.g., drug market conditions, (Curtis et al., 1995) syringe availability (Bluthenthal et al., 2000) and size (Bobashev and Zule, 2010) and social norms (Sherman, 2002), all shaping micro-level drug use behavior, e.g., injection route, frequency and hygiene (Ciccarone, 2009; Ciccarone and Bourgois, 2003).
Heroin source and form may entail some structural risk for SSTI. The robust geographic division of US heroin markets by source-form has existed, for political and economic reasons, for the past two to three decades (Ciccarone, 2009; Ciccarone et al., 2009). Since 1985, “black tar” heroin (BTH) has been the predominant form of heroin available in the Western U.S. (US Drug Enforcement Administration, 2000). Mexican in origin, BTH derives its name from its dark brown to black color, as well as its semi-solid, tarry consistency. PWID in Tijuana, Mexico, the majority of whom used BTH, reported a lifetime prevalence of SSTI of 46% (Pollini et al., 2010). Reports suggest BTH use is associated with several clinical SSTI including abscess and cellulitis (Ciccarone et al., 2001), necrotizing fasciitis (Dunbar and Harruff, 2007) and specifically various Clostridia infections including tetanus (Bardenheier et al., 1998), wound botulism (Center for Disease Control and Prevention, 1995; Passaro et al., 1998) and myonecrosis (Bangsberg et al., 2002).
Heroin market conditions, e.g., retail price and purity, are also components of the structural risk environment. Our analyses of structural changes in the US heroin supply, 1990–2008, revealed that the entry of a novel source-form of powder heroin (PH) from Colombia led to a nationwide decline in the price and increase in the purity of heroin (Rosenblum et al., 2014). Cities in the mid-US with more heroin source-forms had more competition and the greatest decline in purity-adjusted price over the time period (Rosenblum et al., 2014). Another study used representative national hospital data combined with heroin market data to investigate a link between structural heroin market characteristics and heroin-related overdose over 17 years. We found that each $100 decrease in the price per gram pure of heroin resulted in a 3% increase in the number of HOD hospitalizations (Unick et al., 2014). An unexpected finding was that Colombian-sourced heroin had a positive effect, independent of purity, on the rates of HOD in our national model (Unick et al., 2014).
This study focuses on identifying national trends in heroin-related SSTI and quantifying the role that the heroin market, specifically price, purity, and heroin source-form (i.e., BTH vs PH), has on community SSTI risk. This is the first study, to our knowledge, that uses representative national hospital data combined with US Drug Enforcement Administration (DEA) heroin market data to investigate a link between structural heroin market factors and SSTI. We hypothesize that decreases in heroin price are associated with higher hospitalization rates nationally for SSTI and that communities with predominantly BTH have higher rates of SSTI hospitalizations.
2. METHODS
2.1 Sample Metropolitan Statistical Areas
We used Metropolitan Statistical Areas (MSAs), to define geographic entities as defined by the Office of Management and Budget. These units function as integrated economic and social entities that span multiple counties but have a common urban core population over 50,000 (Office of Management and Budget, 2010). We used 27 MSAs to construct the price and purity series for retail level heroin purchases and samples (under 1 gram) between 1993 and 2010 in the DEA System to Retrieve Information from Drug Evidence (STRIDE) dataset. These 27 MSAs were selected because they had data reported in STRIDE for each of the years analyzed. They also represent all of the top 15 and 22 of the top 30 MSAs by population size in the country. Table 1 lists all 27 MSAs with heroin price and purity data. Albuquerque, Atlanta, Dallas, Detroit, El Paso, Houston New Orleans and San Antonio were excluded from the regression analysis due to restrictions on identifying hospital locations, which prevent specification of the hospitals’ MSA (Agency for Healthcare Research and Quality Healthcare Cost and Utilization Project (HCUP), 2008). The 19 MSAs with heroin overdose frequency counts identify the MSAs included in the regression analysis.
Table 1.
MSA, hospital and heroin market characteristics
| MSA | Mean Count of MSA SSTI Hospitalization | Hospital SD | Mean Count of Signature Samples per Year | Signature SD | Mean Percent Mexican Samples | Mexican SD |
|---|---|---|---|---|---|---|
| Albuquerque | - | - | 5.88 | 5 | 93.39 | 14.86 |
| Atlanta | - | - | 28.88 | 8.92 | 4.66 | 9.49 |
| Baltimore | 10.47 | 6.33 | 39.5 | 15.15 | 0.66 | 1.44 |
| Boston | 13.71 | 3.72 | 41.56 | 9.83 | 0.7 | 1.45 |
| Bridgeport | 3.24 | 0.97 | 5.25 | 5.47 | 0 | 0 |
| Chicago | 27.53 | 8.62 | 51.75 | 12.36 | 8.65 | 6.19 |
| Dallas | - | - | 27.38 | 13.98 | 84.9 | 14.97 |
| Denver | 4.94 | 0.97 | 34 | 6.76 | 99.18 | 2.52 |
| Detroit | - | - | 38.71 | 16.29 | 2.65 | 3.05 |
| El Paso | - | - | 12.56 | 7.41 | 71.88 | 18.74 |
| Houston | - | - | 38.62 | 7.23 | 80.81 | 8.96 |
| Los Angeles | 39.53 | 3.61 | 53.12 | 12.67 | 85.05 | 16.2 |
| Miami | 8.24 | 3.85 | 196 | 108.05 | 0.74 | 1.12 |
| Milwaukee | 9.59 | 5.33 | 2.25 | 3.07 | 0 | 0 |
| New Orleans | - | - | 25.69 | 14.12 | 2.33 | 4.75 |
| New York | 16.71 | 2.26 | 272.5 | 68.23 | 0.33 | 0.66 |
| Newark | 3.82 | 1.24 | 70.94 | 16.61 | 0.33 | 0.76 |
| Orlando | 3.53 | 1.97 | 30.93 | 18.01 | 0.59 | 1.29 |
| Philadelphia | 12.71 | 6.11 | 50.44 | 11.45 | 1.89 | 3.12 |
| Phoenix | 6.18 | 1.94 | 38.56 | 8.07 | 99.69 | 0.87 |
| Portland | 3.94 | 1.30 | 7.38 | 6.76 | 96.99 | 7.09 |
| San Antonio | - | - | 10.62 | 9.16 | 86.62 | 27.28 |
| San Diego | 4.71 | 2.02 | 67.69 | 14.07 | 96.19 | 3.31 |
| San Francisco | 15.06 | 2.11 | 41 | 14.76 | 91.67 | 12.65 |
| Seattle | 5.76 | 1.20 | 37.44 | 10.59 | 97.34 | 5.02 |
| St. Louis | 8.94 | 4.25 | 29.44 | 8.04 | 76.44 | 29.42 |
| Washington, DC | 5.94 | 1.82 | 44.31 | 17.99 | 1.71 | 2.29 |
2.2 Counts of Opiate-Related Skin and Soft Tissue Injury Hospital Admissions
The dependent variable for these analyses is a count of opiate-related skin and soft tissue injury (O-SSTI) hospital admissions in a given hospital in a given year in one of 19 MSAs. O-SSTI hospitalization data come from the Nationwide Inpatient Sample (NIS), an approximately 20-percent stratified national random sample of United States Community Hospitals (HCUP, 2008). For each year’s sample of hospitals, the NIS randomly draws 20% of hospitals from its stratified sampling frame to construct the dataset so each individual hospital only appears a limited number of times (a mean of 3.7 times per hospital). Overall there were 3,409 hospitals sampled from the 19 MSAs. Data from 1993 through 2010 NIS were used to estimate the number of O-SSTI in hospitals in each of 19 MSAs.
Cases of O-SSTI were identified using ICD-9 codes included in the NIS discharge records. Individuals were considered to have a SSTI if they had ICD-9 codes 681.1–682.9, were between the ages of 15 and 65 and did not have a diagnosis of diabetes type 1 or type 2. We also tested a model that included the above SSTI ICD-9 codes and codes for gas gangrene, wound botulism and necrotizing fasciitis. These second diagnoses were very rare, were highly correlated (r = 0.99), did not improve the fit of models presented here and did not change any of the inferences. We elected to go with the more parsimonious model. We also considered a number of drug comorbidities, from less sensitive all drug models that included all the dependence, abuse, intoxication and poisoning ICD-9 codes for amphetamines, cocaine, heroin, opiates and general drug categories. All the drug comorbidity models were highly correlated (r = 0.98) and did not change any inferences. The best fitting, and most specific, models included one of several heroin and opiate comorbidity variables including ICD-9 codes for opioid dependence (304.00–304.3), opioid and other drug dependence (304.70–304.73), opioid abuse (305.50–305.53), poisoning by opium, heroin, methadone or other opiates (956.00–956.02, 956.09, 970.1) and accidental poisoning by heroin, methadone or other opiates (E850.0–E850.2).
2.3 Heroin Price, Purity and Source Series
The heroin price and purity series and heroin source data come from the DEA administered STRIDE dataset. The STRIDE data is collected through several procedures. Included in the purity series are all samples collected that include purity analysis. Included in the price series are purchases made as part of an investigation or through the Domestic Monitoring Program. Because the collection of STRIDE data is a convenience sample and not based on random selection we used estimated purity and price data in the models. To construct the estimated price and purity series we followed previous suggestions for data cleaning and modeling with some adjustments (Caulkins, 2005). Because we are interested in the effect of heroin price and purity on users we used only the retail market (less than or equal to a gram) samples for our price and purity series. These analytic methods are further described in previous papers (Rosenblum et al., 2014; Unick et al., 2014).
To construct the purity series we used random coefficient models from Arkes et al (2008) that predict purity as a function of the amount collected and the year the sample was collected. The resulting price and purity series are based on the expected purity hypothesis that better models the user’s expected experience in the drug market (Caulkins, 2005). Specifically, the estimated price and purity data use the model generated expected purity per gram rather than the actual purity, compensating for the presence of outliers due to “bunk” samples with zero percent heroin purity.
Part of the STRIDE data is collected for use in the Heroin Signature Program that collects heroin samples for the purpose of identifying source region (Toske et al., 2006). We used this series to construct a variable identifying the percentage of heroin samples in each MSA for each year that originates from Colombia or Mexico. Heroin originating from these two source countries accounts, by some estimates, for 99% of US retail heroin (Office of Drug Control Policy, 2012). The entry of Colombian-sourced heroin in the early 1990’s effectively displaced two other heroin source-forms, those from Southeast and Southwest Asia, in the retail markets of the eastern US (Ciccarone et al., 2009). Heroin originating from Mexico, going to western US markets, has traditionally been BTH (US Drug Enforcement Administration, 2000). Heroin originating from Colombia is PH (Ciccarone et al., 2009).
2.4 Demographic MSA Controls
Data for local MSA conditions come from several sources. Yearly MSA unemployment and poverty rates were collected from the March Current Population Survey (CPS) supplement. Data on yearly MSA percent male by race and five-year age categories and MSA population size were constructed from the Surveillance, Epidemiology, and End Results (SEER) dataset. Yearly crime estimates for MSAs were taken from the Uniform Crime Reports. We also estimated models with data documenting arrests for heroin and cocaine possession and sales but due to missing data in this variable we used total crime in all presented models. The choice of the crime variable did not affect the models in any substantive way.
2.5 Statistical Model for Counts of O-SSTI Hospital Admissions
We constructed population rates of hospitalizations for O-SSTI, and race, age and region adjusted population rates. Calculations of the sample design adjusted counts of O-SSTI was done using the hospital survey weights and survey design variables provided by HCUP in SAS Proc Surveyfreq and using the populations statistics provided by HCUP (Barrett et al., 2014). We also constructed rates of the number of O-SSTIs as a percentage of all opiate admissions using total hospital counts of admissions as the denominator.
In our model we combined three datasets; the yearly O-SSTI hospital admission count data, the DEA heroin price and purity data and the demographic control data. The resulting dataset had an observation for each hospital-year with hospital-year nested in MSAs. For the regression analysis we used a Random Intercept Negative Binomial model with robust standard errors to predict the counts of yearly O-SSTIs in the sampled hospitals and adjust for the overdispersion of the variance of the count data relative to the mean. We estimate a random intercept for each hospital, resulting in a two level model. The random hospital intercept models the within hospital covariance over time and provides an additional method for modeling the overdispersion of the O-SSTI data. We also used robust standard errors to further correct for the effect of overdispersion and heteroskedasticity on the standard errors (Rabe-Hesketh and Skrondal, 2013)
O-SSTI in hospital i in year j are modeled as a function of the coefficients α1-5 respectively representing raw price, purity or price per pure gram (P), percent Mexican-sourced heroin, total count of crime, unemployment and percent in poverty in year j and MSA k. Coefficient α6 is a vector of demographic controls with percent male and black, Hispanic and white for year j in MSA k. Coefficient α7 is a vector of cubic time variables. Hospitals each have a random intercept (ζi) that are assumed to be normally distributed. All regression models were estimated in Stata 13 using MENBREG with adaptive quadrature (StataCorp, 2013).
Because we are interested in the rate of O-SSTI irrespective of the count of PWID in a population, we need to use a rate of O-SSTI over some denominator representing the population at-risk. Because we do not know the number of PWID in an MSA and because the unit of analysis is hospitals for which we do not know the population at-risk within hospital catchment areas, we use the logged count of all opiate-related hospital admissions as the offset. We tested several other potential counts including all drug-related admissions and opiates admissions excluding overdose, but the count of opiate-related admissions models had the lowest AIC/BIC statistics and was conceptually the most clear and consistent with the dependent variable; the choice of offset did not meaningfully alter the statistical inferences from the model.
3. RESULTS
Table 1 displays the 27 MSAs that had DEA data and the 19 of those that also had hospital data that could be matched with an MSA. For each of the MSAs we provide the available statistics for mean yearly hospital O-SSTI admissions, the yearly mean number of DEA signature samples and the mean yearly percent of those signature samples that are identified as being produced in Mexico. The mean yearly number of hospitals per MSA range from 3.24 in Bridgeport CT to 39.53 in Los Angeles CA. The mean yearly number of signature samples ranges from 3.07 in Milwaukee to 272.5 in New York City. MSAs are divided between Mexican-sourced-heroin-dominant (MHD) and non-Mexican-heroin-dominant cities (non-MHD) with little overlap. Most MHD cities are on the West region. The Northeast and Midwest are non-MHD (i.e., Colombian-sourced-heroin-dominant (CHD)). The South is more split but the most MHD southern locations are all in Texas, which does not provide hospital identifiers in their data, and so are not included in the regression analysis.
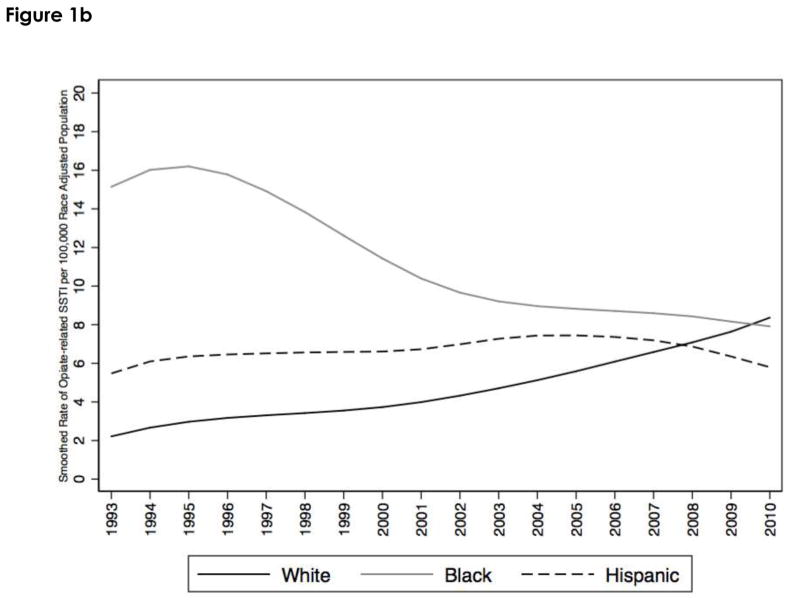
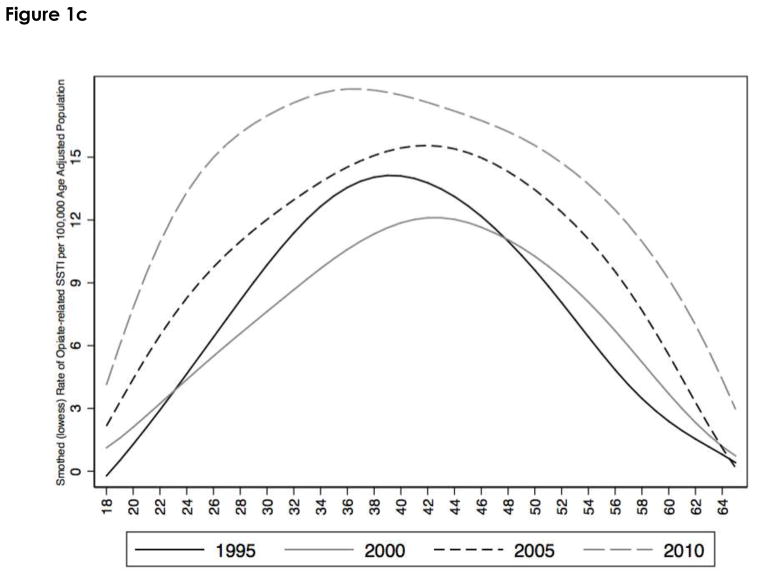
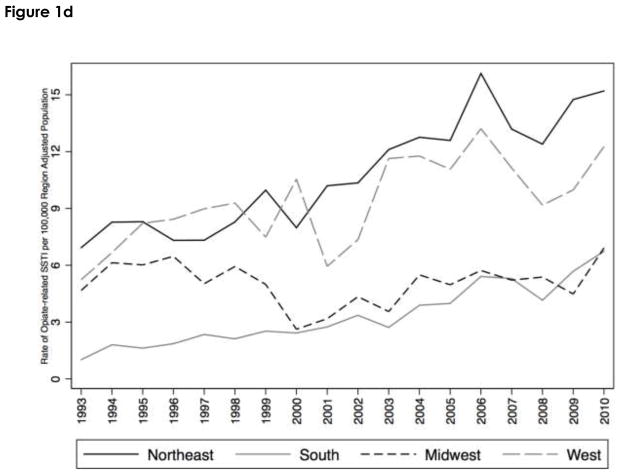
Figures 1a–d show the national rates of O-SSTI. Figure1a is the rate of O-SSTI in the US population. Hospitalizations increased from under 4 per 100,000 pop. in 1993 to over 9 per 100,000 in 2010 with rates increasing fairly steadily from 2001 to 2010; and an overall rate of increase between 1993 and 2010 of 0.27 per 100,000 per year. Figure 1b shows that the rates of O-SSTI have not increased equally between Black, White and Hispanic populations. Black rates peaked in 1996 at a rate of 18.42 per 100,000 declining to 6.59 in 2008 and increasing to 9.33 in 2010. Hispanic rates have remained relatively flat with a minimum rate of 4.82 per 100,000 in 1994 and a maximum rate of 9.91 in 2006. White rates have steadily increased from 1.94 per 100,000 in 1993 to 8.80 per 100,000 in 2010. Figure 1c shows the age distribution for O-SSTI in five-year intervals between 1995 and 2010. In the lowess smoothed data displayed in the graph, the peak rate for all ages was 2010. In the raw rate data there is slightly more variability, with 23 of the 48 included ages having their max rate in 2010 and 42 of 48 having their max rate in 2006 or later. The graph also shows that the mean of the age distribution has skewed younger between 2000 and 2010. Figure 1d shows the rates across region. The Northeast generally has the higher rate of O-SSTI admissions followed by the West.
Figure 1.
Figure 1a. Rate of Opiate-related SSTI Hospitalizations between 1993 and 2010
Figure 1b. Rate of Opiate-related SSTI Hospitalizations between 1993 and 2010 by Race
Figure 1c. Rate of Opiate-related SSTI Hospitalizations between 1993 and 2010 by Age
Figure 1d. Rate of Opiate-related SSTI Hospitalizations between 1993 and 2010 by Region
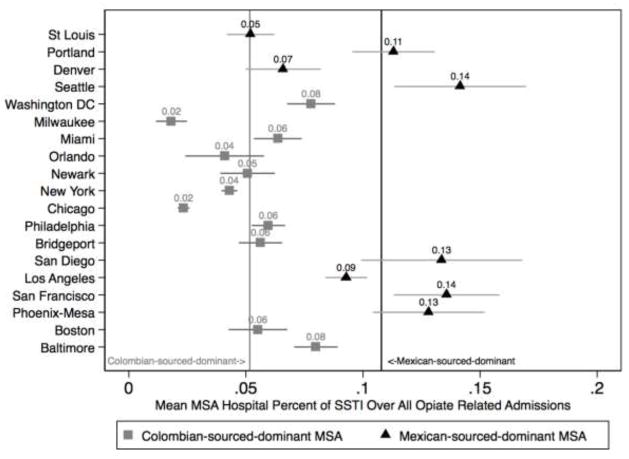
Figure 2 adjusts the data to show the MSA mean hospital rate of O-SSTI over all admissions for opiate-related diagnoses. Because we do not have counts of individuals who inject opiates by hospital catchment area, we used the total yearly count of opiate-related hospital admissions as the denominator in our rate calculations. Using all individuals who were admitted with opiate-related diagnoses we can get an approximation of the population of opiate users at-risk for O-SSTI in the hospital catchment area. The vertical lines represent the means of the MHD cities in black and CHD cities in gray and show higher rates of O-SSTI over all opiate admissions in MHD compared with CHD cities with only St. Louis and Denver being closer to the Colombian mean. In the MHD cities 10.7% of opiate-related admissions are for a primary diagnosis of O-SSTI versus 5.2% in CHD cities, a statistically significantly difference (p<0.001).
Figure 2.
Rates of Opiate-related SSTI over all Opiate Hospitalizations by MSA
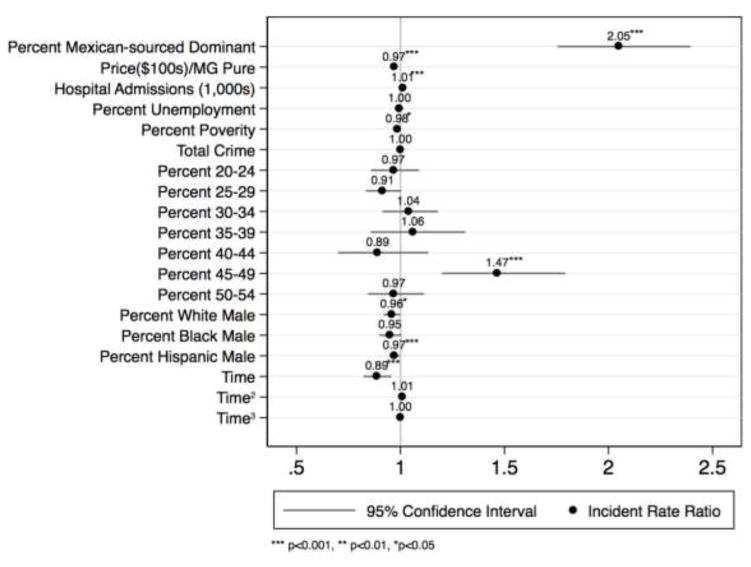
Figure 3 is the graphical representation of the coefficients of the multilevel negative binominal model. Using the same rate adjustment as Figure 2, we estimated the Incident Rate Ratio for O-SSTI as a function of the proportion of Mexican heroin in an MSA. We found that the rate of O-SSTI doubles (P<0.001) as you move from a 0% MHD city to a 100% MHD city. As Table 1 shows most cities are either MHD or CHD. Price of a pure gram of heroin also predicts O-SSTI, with a $100 increase in price resulting in a 3% decrease in the rate of O-SSTI.
Figure 3.
Negative Binomial Regression of Hospital Opiate-related SSTI Yearly Counts
4. DISCUSSION
Hospitalizations for heroin-related SSTI are rising in the US with rates doubling between 2000 and 2010; the increase concentrated among individuals aged 20 to 40. Consistent with our hypotheses we found that heroin market features are strongly associated with changes in the rate of SSTI: each $100 increase in the average yearly MSA heroin price-per-pure gram was associated with a 3% decrease in the rate of heroin-related SSTI hospital admission. Heroin source-form also matters: after adjusting for covariates, BTH-dominant cities had twice the rate of SSTIs compared to PH-dominant cities.
Source and form of heroin are structural factors in the risk environment: each heroin source-form has specific characteristics–color, physical state, cold/hot water solubility, pH, heat stability, weight to volume ratio and purity–that affect how it is used and which risks are inherent in that use pattern (Ciccarone, 2009; Ciccarone and Bourgois, 2003; Ciccarone and Harris, 2015). Colombian-sourced PH is off-white to light brown, powdered, with cold water solubility. BTH is dark brown to black, solid, vaporizable, of lower purity and requires heat to go into aqueous solution. Differential medical consequences stem from each source-form, e.g., cities with greater proportions of Colombian-sourced PH have greater risk for heroin-related overdose controlling for heroin purity (Unick et al., 2014). Heroin source-forms correlate to differential medical consequences e.g., HIV prevalence among PWID is much higher in cities with PH than in cities where BTH is endemic (Ciccarone and Bourgois, 2003). The ritual syringe residue rinsing observed among BTH injectors likely leads to reduced HIV transmission risk as the potential viral load of a reused syringe has been reduced by the rinsing (Ciccarone and Bourgois, 2003). In addition, BTH appears to induce venous sclerosis and users migrate to subcutaneous or intramuscular injection (Binswanger et al., 2000; Ciccarone et al., 2001; Murphy et al., 2001b; Williamson et al., 2001); it is likely this mechanism that leads to the association between BTH and SSTI, both common, i.e., abscess and cellulitis, and rare, e.g., wound botulism. Heroin solution acidity has been proposed as the proximal causal link to venous sclerosis and SSTI (Ciccarone and Harris, 2015) but the acidity of BTH solutions relative to other heroin forms is unknown. Some have suggested that the heating process to put BTH into solution is not sufficient to kill spore-forming bacteria such as Clostridia species (Gordon and Lowy, 2005; Passaro et al., 1998). Beyond this, the exact nature of the association between BTH use and infection remains ill-defined.
Rising SSTI rates are likely due to rising heroin use in the US. A nationwide multifaceted transition is occurring from opioid pill misuse to heroin injecting (Cicero and Ellis, 2015; Cicero et al., 2012; Daniulaityte et al., 2006; Dart et al., 2015; Lankenau et al., 2012; Peavy et al., 2012). National survey data found past-year heroin users rose from 373,000 in 2007 to 669,000 in 2012; heroin initiation has risen since the mid-2000s, signaling a growing epidemic (Substance Abuse and Mental Health Services Administration, 2013). Our research shows that heroin use is increasing among young people with an “intertwined epidemic” of heroin-related and prescription opioid-related overdose (Unick et al., 2013). Younger users we interviewed had typically transitioned from pills to insufflating and then injecting heroin after finding their pill supply unreliable or unaffordable (Mars et al., 2014). The unequal rates of O-SSTI between Black, White and Hispanic populations reflect the demographics of the unfolding heroin epidemic (Unick et al., 2013). The public health implications of this nationwide heroin epidemic, including regional and generational differences in risk taking and rising medical consequences, remain to be expounded.
Interventions at the behavioral and social-structural levels can address the rising SSTI problem. Clinical and harm reduction efforts should educate heroin users on local risk factors, e.g., heroin type, promote vein health strategies and provide culturally sensitive treatment services for persons suffering with SSTI (Ciccarone and Harris, 2015; Harris and Rhodes, 2012; Messac et al., 2013). Tailored SSTI interventions for BTH injectors include safer muscling and possibly buffered heroin (Ciccarone and Harris, 2015); for PH injectors emphasis should be placed on reducing the risks from concurrent cocaine, i.e., speedball, use. In San Francisco, a specialized SSTI clinic was developed following a report on the extent and costliness of this problem at the county hospital (Ciccarone et al., 2001). This community-stimulated intervention proved popular, cost-saving and durable (Harris and Young, 2002; Messac et al., 2013). SSTI clinics can also be a component of syringe exchange, including mobile, services (Grau et al., 2002; Robinowitz et al., 2014; Smith et al., 2014). Medical care offered within supervised injection facilities helps reduce the social and structural barriers to SSTI care (Small et al. 2008).
4.1 Limitations
There are a number of limitations to this study. First we have only observed correlations not causal relationships between type of heroin, cost of heroin and SSTI rates. While consistent with our hypothesis of a causal relationship these findings are not proof of a causal relationship. One potential source of bias is that different injection cultures or different environmental bacterial risks exist in the West compared to the East and that these are associated with different levels of SSTI risk. Other ecological fallacy risks exist where differences in the population risk are not related to individual actors.
A separate set of limitations is related to the use of DEA data on heroin price, purity and source region along with limitations related to hospital coding practices. Both the main independent and dependent data could be subject to various sources of bias. For example there is some evidence that the use of DEA data for estimating price, purity and source region is flawed (Horowitz, 2001). Furthermore, the geographic spread of the MSAs was not selected to be representative. While the MSAs were included because of the quantity of samples collected by the DEA, differences across local DEA offices, e.g., different approaches sampling from the local heroin market, could bias the price and purity data series. While we have employed several methods, from sensitivity checks for diagnosis of SSTIs to statistical price and purity models for the DEA data, there is uncertainty about the reliability and validity of the data.
4.2 Conclusion
Consistent with the increase in reported heroin use is an increase in heroin-related SSTI. Structural factors, including heroin market dynamics, specifically BTH and lower price-per-pure gram of heroin, predict higher counts/rates of SSTI hospital admissions. Understanding PWID’ risk behavior in the context of the structural risk environment enables tailoring structural, behavioral and clinical interventions e.g., syringe exchange programs (Hurley et al., 1997) and harm-reduction oriented SSTI clinics (Grau et al., 2002; Harris and Young, 2002; Messac et al., 2013; Robinowitz et al., 2014). Future investigations into the causes of SSTI among heroin injectors should consider both physiological and chemical mechanisms, including the measurement of histamine as an injection induced inflammatory marker (Maurer et al., 2014), and drug solution acidity (Ciccarone and Harris, 2015).
Highlights.
Hospitalization rates for opiate related soft tissue infections (SSTI) have doubled nationally
Heroin price increases were associated with decreases in the rate of heroin-related SSTI
Mexican-sourced-heroin-dominant cities had twice the rate of SSTI
Acknowledgments
Role of Funding Source
This work was funded by grants DA037820 and DA27599 from the National Institutes of Health, National Institute Drug Abuse.
The authors acknowledge the National Institutes of Health, National Institute Drug Abuse for the following grants which funded this research: DA037820 and DA27599. In addition, we acknowledge the sources of the data used in these analyses: healthcare data from the Healthcare Cost and Utilization Project (HCUP) sponsored by the Agency for Healthcare Research and Quality (AHRQ) and the drug market data from the U.S. Drug Enforcement Administration.
Footnotes
Contributors
Daniel Ciccarone was PI of the grant, developed the research hypothesis, assisted with the data collection and data analysis and led the writing of the paper. George Unick led the analysis and contributed to the writing of the paper. Jenny Cohen led the data collection, assisted with the analysis and contributed to the writing of the paper. Sarah Mars contributed to the writing of the paper. Dan Rosenblum assisted with the analysis and contributed to the writing of the paper.
Conflicts of Interest
No conflict declared by any of the authors
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Dan Ciccarone, Email: Daniel.Ciccarone@UCSF.edu, University of California San Francisco, Dept. of Family and Community Medicine, 500 Parnassus Ave., MU-3E, Box 900, San Francisco, CA 94143-0900; 415-514-0275.
George Jay Unick, School of Social Work, University of Maryland.
Jenny Cohen, University of California San Francisco.
Sarah G. Mars, University of California San Francisco, Dept. of Family and Community Medicine
Dan Rosenblum, Dalhousie University, Dept. of Economics.
References
- Agency for Healthcare Research and Quality Healthcare Cost and Utilization Project (HCUP) Introduction to the HCUP Nationwide Inpatient Sample (NIS) Rockville, MD: 2008. from http://www.hcup-us.ahrq.gov/db/nation/nis/NIS_2008_INTRODUCTION.pdf. [Google Scholar]
- Arkes J, Pacula R, Paddock S, Caulkins JP, Reuter P. Why the DEA Stride data are still useful for understanding drug markets. Nber Working Paper Series. 2008 Retrieved from http://www.nber.org/papers/w14224.pdf.
- Bangsberg DR, Rosen JI, Aragon T, Campbell A, Weir L, Perdreau-Remington F. Clostridial myonecrosis cluster among injection drug users: a molecular epidemiology investigation. Arch Intern Med. 2002;162:517–522. doi: 10.1001/archinte.162.5.517. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=11871919. [DOI] [PubMed] [Google Scholar]
- Bardenheier B, Prevots DR, Khetsuriani N, Wharton M. Tetanus surveillance--United States, 1995–1997. MMWR Surveill Summ. 1998;47:1–13. http://www.ncbi.nlm.nih.gov/pubmed/9665156. [PubMed] [Google Scholar]
- Barrett ML-GL, Coffey R, Levit K. Population Denominator Data for Use with the HCUP Databases (Updated with 2013 Population Data) 201. Retrieved from http://www.hcup-us.ahrq.gov/reports/methods/methods.jsp.
- Binswanger IA, Kral AH, Bluthenthal RN, Rybold DJ, Edlin BR. High prevalence of abscesses and cellulitis among community-recruited injection drug users in San Francisco. Clin Infect Dis. 2000;30:579–581. doi: 10.1086/313703. [DOI] [PubMed] [Google Scholar]
- Binswanger IA, Takahashi TA, Bradley K, Dellit TH, Benton KL, Merrill JO. Drug users seeking emergency care for soft tissue infection at high risk for subsequent hospitalization and death. J Stud Alcohol Drugs. 2008;69:924–932. doi: 10.15288/jsad.2008.69.924. http://www.ncbi.nlm.nih.gov/pubmed/18925351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bluthenthal RN, Kral AH, Gee L, Erringer EA, Edlin BR. The effect of syringe exchange use on high-risk injection drug users: a cohort study. AIDS. 2000;14:605–611. doi: 10.1097/00002030-200003310-00015. http://www.ncbi.nlm.nih.gov/pubmed/10780722. [DOI] [PubMed] [Google Scholar]
- Bobashev GV, Zule WA. Modeling the effect of high dead-space syringes on the human immunodeficiency virus (HIV) epidemic among injecting drug users. Addiction. 2010;105:1439–1447. doi: 10.1111/j.1360-0443.2010.02976.x. [DOI] [PubMed] [Google Scholar]
- Bourgois P, Schonberg J. Righteous Dopefiend. University of California Press; Berkeley: 2009. [Google Scholar]
- Caulkins JP. Price and purity analysis for illicit drug: data and conceptual issues. Health Serv Res. 2005;25 doi: 10.1016/j.drugalcdep.2006.08.014. [DOI] [PubMed] [Google Scholar]
- Center for Disease Control and Prevention. Wound botulism - California, 1995. MMWR. 1995;44:889–892. [Google Scholar]
- Ciccarone D. Heroin in brown, black and white: structural factors and medical consequences in the US heroin market. Int J Drug Policy. 2009;20:277–282. doi: 10.1016/j.drugpo.2008.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciccarone D, Bamberger J, Kral A, Hobart CJ, Moon A, Edlin BR, et al. Soft tissue infections among injection drug users - San Francisco, California, 1996–2000. JAMA. 2001;285:2707–2709. [PubMed] [Google Scholar]
- Ciccarone D, Bourgois P. Explaining the geographical variation of HIV among injection drug users in the United States. Subst Use Misuse. 2003;38:2049–2063. doi: 10.1081/JA-120025125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciccarone D, Bourgois P, Murphy E, Kral A, Seal K, Moore J, Edlin BR. Soft Tissue Infections Among Users Of Black Tar Heroin: A Cross-Methodological Examination. Paper presented at the Community Epidemiology Working Group Meeting; San Francisco, CA. December 12–15.2000. [Google Scholar]
- Ciccarone D, Harris M. Fire in the vein: heroin acidity and its proximal effect on users’ health. Int J Drug Policy. 2015 doi: 10.1016/j.drugpo.2015.04.009. epub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciccarone D, Unick GJ, Kraus A. Impact of South American heroin on the US heroin market 1993–2004. Int J Drug Policy. 2009;20:392–401. doi: 10.1016/j.drugpo.2008.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicero TJ, Ellis MS. Abuse-deterrent formulations and the prescription opioid abuse epidemic in the United States: lessons learned from oxycontin. JAMA Psychiatry. 2015;72:424–430. doi: 10.1001/jamapsychiatry.2014.3043. [DOI] [PubMed] [Google Scholar]
- Cicero TJ, Ellis MS, Surratt HL. Effect of abuse-deterrent formulation of oxycontin. N Engl J Med. 2012;367:187–189. doi: 10.1056/NEJMc1204141. [DOI] [PubMed] [Google Scholar]
- Crane LR, Levine DP, Zervos MJ, Cummings G. Bacteremia in narcotic addicts at the Detroit Medical Center. I Microbiology, epidemiology, risk factors, and empiric therapy. Rev Infect Dis. 1986;8:364–373. doi: 10.1093/clinids/8.3.364. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=3636987. [DOI] [PubMed] [Google Scholar]
- Curtis R, Friedman SR, Neaigus A, Jose B, Goldstein M, Ildefonso G. Street-level drug markets: Network structure and HIV risk. Soc Networks. 1995;17:229–249. [Google Scholar]
- Daniulaityte R, Carlson RG, Kenne DR. Initiation into pharmaceutical opioids and patterns of misuse: preliminary qualitative findings obtained by the Ohio Substance Abuse Monitoring Network. J Drug Issues. 2006;36:787–809. [Google Scholar]
- Dart RC, Surratt HL, Cicero TJ, Parrino MW, Severtson SG, Bucher-Bartelson B, Green JL. Trends in opioid analgesic abuse and mortality in the United States. N Engl J Med. 2015;372:241–248. doi: 10.1056/NEJMsa1406143. [DOI] [PubMed] [Google Scholar]
- Dunbar NM, Harruff RC. Necrotizing fasciitis: manifestations, microbiology and connection with black tar heroin. J Forensic Sci. 2007;52:920–923. doi: 10.1111/j.1556-4029.2007.00452.x. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=17524065. [DOI] [PubMed] [Google Scholar]
- Ebright J, Pieper B. Skin and soft tissue infections in injection drug users. Infect Dis Clin North Am. 2002;16:697–712. doi: 10.1016/s0891-5520(02)00017-x. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=12371123. [DOI] [PubMed] [Google Scholar]
- Fink DS, Lindsay SP, Slymen DJ, Kral AH, Bluthenthal RN. Abscess and self-treatment among injection drug users at four California syringe exchanges and their surrounding communities. Subst Use Misuse. 2013;48:523–531. doi: 10.3109/10826084.2013.787094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon RJ, Lowy FD. Bacterial infections in drug users. N Engl J Med. 2005;353:1945–1954. doi: 10.1056/NEJMra042823. [DOI] [PubMed] [Google Scholar]
- Grau LE, Arevalo S, Catchpool C, Heimer R. Expanding harm reduction services through a wound and abscess clinic. Am J Public Health. 2002;92:1915–1917. doi: 10.2105/ajph.92.12.1915. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=12453808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris HW, Young DM. Care of injection drug users with soft tissue infections in San Francisco, California. Arch Surg. 2002;137:1217–1222. doi: 10.1001/archsurg.137.11.1217. http://www.ncbi.nlm.nih.gov/pubmed/12413304. [DOI] [PubMed] [Google Scholar]
- Harris M, Rhodes T. Venous access and care: harnessing pragmatics in harm reduction for people who inject drugs. Addiction. 2012;107:1090–1096. doi: 10.1111/j.1360-0443.2011.03749.x. [DOI] [PubMed] [Google Scholar]
- Hope VD, Parry JV, Ncube F, Hickman M. Not in the vein: ‘missed hits’, subcutaneous and intramuscular injections and associated harms among people who inject psychoactive drugs in Bristol, United Kingdom. Int J Drug Policy. 2016;28:83–90. doi: 10.1016/j.drugpo.2015.11.003. [DOI] [PubMed] [Google Scholar]
- Horowitz JL. Should the DEA’s STRIDE data be used for economic analyses of markets for illegal drugs? J Am Stat Assoc. 2001;96:1254–1262. Retrieved from http://www.scopus.com/inward/record.url?eid=2-s2.0-1542469782&partnerID=40&md5=c1e6b3c4f63fc1ee93dc35f6ea7afd31. [Google Scholar]
- Hurley SF, Jolley DJ, Kaldor JM. Effectiveness of needle-exchange programmes for prevention of HIV infection. Lancet. 1997;349:1797–1800. doi: 10.1016/S0140-6736(96)11380-5. [DOI] [PubMed] [Google Scholar]
- Lankenau SE, Teti M, Silva K, Jackson Bloom J, Harocopos A, Treese M. Initiation into prescription opioid misuse amongst young injection drug users. Int J Drug Policy. 2012;23:37–44. doi: 10.1016/j.drugpo.2011.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lloyd-Smith E, Wood E, Zhang R, Tyndall MW, Montaner JS, Kerr T. Risk factors for developing a cutaneous injection-related infection among injection drug users: a cohort study. BMC Public Health. 2008;8:405. doi: 10.1186/1471-2458-8-405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mars SG, Bourgois P, Karandinos G, Montero F, Ciccarone D. “Every ‘never’ I ever said came true”: transitions from opioid pills to heroin injecting. Int J Drug Policy. 2014;25:257–266. doi: 10.1016/j.drugpo.2013.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maurer U, Kager C, Fellinger C, Loader D, Pollesbock A, Spitzer B, Jarisch R. Risk of anaphylaxis in opioid dependent persons: effects of heroin versus substitution substance. Subst Abuse Treat Prev Policy. 2014;9:12. doi: 10.1186/1747-597X-9-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messac L, Ciccarone D, Draine J, Bourgois P. The good-enough science-and-politics of anthropological collaboration with evidence-based clinical research: four ethnographic case studies. Soc Sci Med. 2013 doi: 10.1016/j.socscimed.2013.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy EL, DeVita D, Liu H, Vittinghoff E, Leung P, Ciccarone D, Edlin B. Risk factors for skin and soft-tissue abscesses among injection drug users: a case-control study. Clin Infect Dis. 2001a;33:35–40. doi: 10.1086/320879. Epub 2001 http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=11389492. [DOI] [PubMed] [Google Scholar]
- Murphy EL, DeVita D, Liu H, Vittinghoff E, Leung P, Ciccarone DH, Edlin BR. Risk factors for skin and soft-tissue abscesses among injection drug users: a case-control study. Clin Infect Dis. 2001b;33:35–40. doi: 10.1086/320879. [DOI] [PubMed] [Google Scholar]
- Office of Drug Control Policy. Drug Availability Estimates in the United States, 2001–2006. 2012. [Google Scholar]
- Office of Management and Budget. 2010 Standards for Delineating Metropolitan and Micropolitan Statistical Areas. Federal Register. 2010;75:37246–39052. [Google Scholar]
- Palfreyman SJ, Tod AM, King B, Tomlinson D, Brazier JE, Michaels JA. Impact of intravenous drug use on quality of life for patients with venous ulcers. J Adv Nurs. 2007;58:458–467. doi: 10.1111/j.1365-2648.2007.04251.x. [DOI] [PubMed] [Google Scholar]
- Passaro DJ, Werner SB, McGee J, Mac Kenzie WR, Vugia DJ. Wound botulism associated with black tar heroin among injecting drug users. JAMA. 1998;279:859–863. doi: 10.1001/jama.279.11.859. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/9516001. [DOI] [PubMed] [Google Scholar]
- Peavy KM, Banta-Green CJ, Kingston S, Hanrahan M, Merrill JO, Coffin PO. “Hooked on” prescription-type opiates prior to using heroin: results from a survey of syringe exchange clients. J Psychoactive Drugs. 2012;44:259–265. doi: 10.1080/02791072.2012.704591. [DOI] [PubMed] [Google Scholar]
- Phillips KT, Stein MD. Risk practices associated with bacterial infections among injection drug users in Denver, Colorado. Am J Drug Alcohol Abuse. 2010;36:92–97. doi: 10.3109/00952991003592311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pieper B, Kirsner RS, Templin TN, Birk TJ. Injection drug use - an understudied cause of venous disease. Arch Dermatol. 2007;143:1305–1309. doi: 10.1001/archderm.143.10.1305. [DOI] [PubMed] [Google Scholar]
- Pollini RA, Gallardo M, Hasan S, Minuto J, Lozada R, Vera A, Zuniga ML, Strathdee SA. High prevalence of abscesses and self-treatment among injection drug users in Tijuana, Mexico. Int J Infect Dis. 2010;14(Suppl 3):e117–122. doi: 10.1016/j.ijid.2010.02.2238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabe-Hesketh S, Skrondal A. Multilevel And Longitudinal Modeling Using Stata. Stata Corp; College Station, TX: 2013. [Google Scholar]
- Ramsay CN, Stirling A, Smith J, Hawkins G, Brooks T, Hood J, Penrice G, Browning LM, Ahmed S. An outbreak of infection with Bacillus anthracis in injecting drug users in Scotland. EuroSurveill. 2010;15 doi: 10.2807/ese.15.02.19465-en. [DOI] [PubMed] [Google Scholar]
- Rhodes T. Risk environments and drug harms: a social science for harm reduction approach. Int J Drug Policy. 2009;20:193–201. doi: 10.1016/j.drugpo.2008.10.003. [DOI] [PubMed] [Google Scholar]
- Robinowitz N, Smith ME, Serio-Chapman C, Chaulk P, Johnson KE. Wounds on wheels: implementing a specialized wound clinic within an established syringe exchange program in Baltimore, Maryland. Am J Public Health. 2014;104:2057–2059. doi: 10.2105/Ajph.2014.302111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenblum D, Unick GJ, Ciccarone D. The entry of Colombian-sourced heroin into the US market: the relationship between competition, price, and purity. Int J Drug Policy. 2014;25:88–95. doi: 10.1016/j.drugpo.2013.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherman SG, Smith L, Laney G, Strathdee S. Social influences on the transition to injection drug use among young heroin sniffers. Int J Drug Policy I. 2002;(13):113–120. [Google Scholar]
- Small W, Wood E, Lloyd-Smith E, Tyndall M, Kerr T. Accessing care for injection-related infections through a medically supervised injecting facility: qualitative study. Drug Alcohol Depend. 2008;98:159–162. doi: 10.1016/j.drugalcdep.2008.05.014. [DOI] [PubMed] [Google Scholar]
- Smith ME, Robinowitz N, Chaulk P, Johnson KE. Self-care and risk reduction habits in older injection drug users with chronic wounds: a cross-sectional study. Harm Reduct J. 2014;11:28. doi: 10.1186/1477-7517-11-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spijkerman IJvAE, Mientjes GH, Coutinho RA, van den Hoek A. Human immunodeficiency virus infection and other risk factors for skin abscesses and endocarditis among injection drug users. J Clin Epidemiol. 1996;49:1149–1154. doi: 10.1016/0895-4356(96)00180-1. [DOI] [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software: Release 13. College Station, TX: 2013. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: 2013. NSDUH Series H-46, HHS Publication No. (SMA) 13–4795. [Google Scholar]
- Takahashi TA, Baerstein A, Binswanger I, Bradley K, Merrill JO. Predictors of hospitalization for injection drug users seeking care for soft tissue infections. J Gen Intern Med. 2007;22:382–388. doi: 10.1007/s11606-006-0079-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takahashi TA, Maciejewski ML, Bradley K. US hospitalizations and costs for illicit drug users with soft tissue infections. J Behav Health Serv Res. 2010;37:508–518. doi: 10.1007/s11414-009-9177-z. [DOI] [PubMed] [Google Scholar]
- Toske SG, Cooper SD, Morello DR, Hays PA, Casale JF, Casale E. Neutral heroin impurities from tetrahydrobenzylisoquinoline alkaloids. J Forensic Sci. 2006;51:308–320. doi: 10.1111/j.1556-4029.2006.00057.x. Retrieved from http://onlinelibrary.wiley.com/store/10.1111/j.1556-4029.2006.00057.x/asset/j.1556-4029.2006.00057.x.pdf?v=1&t=hri4mq70&s=77a88e6d51e848c6305d4e415ff0e33a99ed5878. [DOI] [PubMed] [Google Scholar]
- Unick G, Rosenblum D, Mars S, Ciccarone D. The relationship between US heroin market dynamics and heroin-related overdose, 1992–2008. Addiction. 2014;109:1889–1898. doi: 10.1111/add.12664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unick GJ, Rosenblum D, Mars S, Ciccarone D. Intertwined epidemics: national demographic trends in hospitalizations for heroin- and opioid-related overdoses, 1993–2009. PLoS One. 2013;8:e54496. doi: 10.1371/journal.pone.0054496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Drug Enforcement Administration. The Mexican Heroin Trade. 2000. DEA-20014. [Google Scholar]
- Williamson N, Archibald C, Van Vliet JS. Unexplained deaths among injection drug users: a case of probable Clostridium myonecrosis. CMAJ. 2001;165:609–611. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11563214. [PMC free article] [PubMed] [Google Scholar]