Abstract
Aims
To quantify the extent of squamous metaplasia in bronchial biopsies and relate it to the presence of chronic obstructive pulmonary disease (COPD), a smoking-related pathology.
Methods
Bronchial biopsies (n = 15 in each group) from smokers with COPD GOLD stage1 and GOLD stage2, smokers without COPD and healthy non-smokers were stained immunohistochemically with a panel of antibodies that facilitated the identification of pseudostratified epithelium and distinction of squamous metaplasia and squamous epithelium from tangentially cut epithelium. The percentage length of each of these epithelial phenotypes was measured as a percent of total epithelial length using computerised image analysis. Sections were also stained for carcinoembryonic antigen and p53, early markers of carcinogenesis, and Ki67, and the percentage epithelial expression measured.
Results
The extent of squamous metaplasia was significantly increased in both COPD1 and COPD2 compared to healthy smokers and healthy non-smokers. The amount of fully differentiated squamous epithelium was also increased in COPD1 and COPD2 compared to healthy non-smokers, as was the expression of carcinoembryonic antigen. These features correlated with one other.
Conclusion
In subjects with COPD there is a loss of pseudostratified epithelium accompanied by an increase in squamous metaplasia with transition into a fully squamous epithelium and expression of early markers of carcinogenesis.
Introduction
Squamous metaplasia (SQM) is a pre-neoplastic change of the bronchial epithelium observed in the lungs in response to toxic injury induced by cigarette smoke [1–4]. It is part of a multi-stage process [5–7] which may eventually lead to full neoplastic transformation, i.e. bronchial carcinoma. Not all SQM lesions progress to a neoplasia, particularly if low grade and some may regress to a normal epithelium [8–10], especially after smoking cessation [11].
Initially, during SQM quiescent basal cells within the pseudostratified epithelium re-enter the cell cycle and become hyperproliferative. During the next stage of the process, the epithelium begins to express markers of a squamous phenotype rather than those of the normal pseudostratified epithelium. These include squamous epithelial cytokeratins (CK) [5,6,12–14] and the cell adhesion molecule SQM1 [15]. Finally, when fully differentiated, having a squamous cell morphology, cells will express involucrin, a marker of terminal differentiation [16].
A history of cigarette smoking is associated with 90% of lung cancers with 15% of lifetime smokers developing lung cancer [17–20]. Chronic obstructive pulmonary disease (COPD) is also associated with smoking and is an independent risk factor for developing lung cancer, the risk being increased by up to 4.5 fold [21–26]. Between 50 and 70% of subjects with lung cancer also have COPD [18,27]. The cause of this increased susceptibility in subjects with COPD is unknown. Several possibilities have been suggested, including common molecular pathways [28,29], impaired ability to clear carcinogens due to obstructive airways [30] and ongoing chronic inflammation within the airways [27,31].
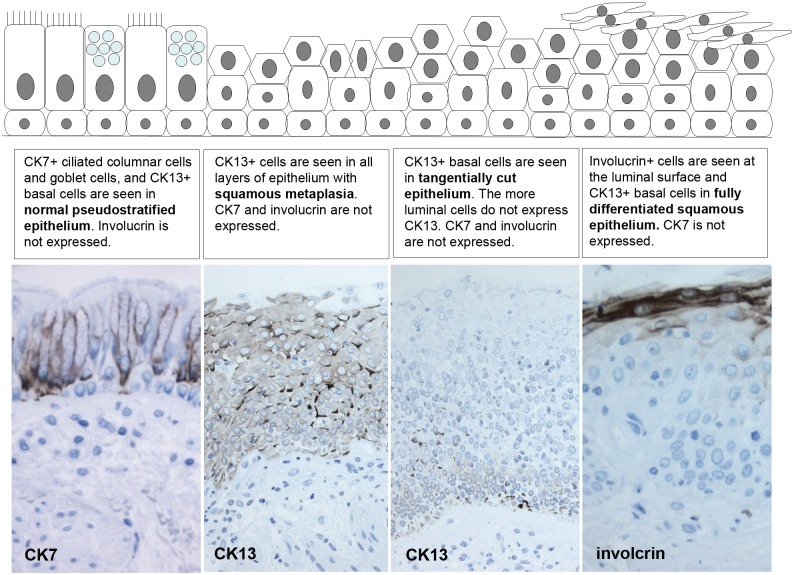
SQM is observed in the bronchial epithelium of smokers [11], but to date there have been, to our knowledge, no studies to quantify it and relate it to the coexistence and severity of COPD. We have previously identified a panel of antibodies, CK7, CK13 and involucrin, that are suitable for identification and distinction of SQM and squamous epithelium in endobronchial biopsies, from tangentially cut epithelium [32], which is difficult based on morphology alone in small biopsies. CK7 is seen in luminal cells of the pseudostratified epithelium and its expression is lost during SQM and absent in squamous epithelium. CK13 expression is restricted to the basal cells of pseudostratified epithelium but is observed throughout the epithelium with SQM or a squamous phenotype. Involucrin is restricted to cells with a fully differentiated squamous morphology. This staining pattern is summarised in Fig 1 in the results.
Fig 1. Cytokeratin and involucrin expression in the bronchial epithelium during transition from a normal pseudostratified epithelium to a squamous phenotype.
Diagram, with matching photographs from bronchial biopsies included in this study, illustrating how the expression of CKs and involucrin (brown) changes as the normal pseudostratified bronchial epithelium undergoes transition towards a squamous phenotype.
The aim of the current study was to quantitate, using the above panel of antibodies, the amount of SQM and squamous epithelium (SE) within the bronchial epithelium of smokers with and without COPD, compared to healthy controls. Additionally, we have looked at the expression of the proliferation marker, Ki67, and the early markers of carcinogenesis, carcinoembryonic antigen (CEA) and p53. The relationship to severity of COPD and smoking history was also investigated.
Materials and Methods
Subjects and study design
This study used previously collected glycol methacrylate embedded bronchial biopsies from four subject groups (n = 15 in each group); healthy non-smokers, healthy smokers, and COPD subjects classified according to the GOLD guidelines [33] as having COPD stage 1 airflow obstruction (COPD1) and COPD stage 2 airflow obstruction(COPD2). The clinical characteristics of each subject were fully characterised (Table 1); data from some of these subjects has been reported previously [34].
Table 1. Subject characteristics.
| Group | Gender | Age (years) | FVC / FEV1 | FEV1 (% predicted) | Smoking history (pack years) |
|---|---|---|---|---|---|
| Healthy non-smokers | 6M:9F | 53.6 (8.2) | 77.60 (4.88) | 108.67 (12.20) | zero |
| Healthy smokers | 5M:10F | 48.2 (9.5) | 78.80 (5.24) | 100.53 (9.37) | 36.73 (13.09) |
| COPD 1 | 12M:3F | 56.7 (7.5) | 65.13 (4.41) | 91.53 (5.93) | 44.00 (15.97) |
| COPD 2 | 10M:5F | 56.7 (8.2) | 60.87 (7.09) | 66.60 (7.53) | 50.33 (12.38) |
Data are means and (standard deviations)
This study was approved by National Research Ethics Service Committee South Central—Southampton B (11/SC/0103) and the original biopsy collection for which subjects gave written informed consent by Southampton and South West Hampshire Research Ethics Committee (276/99 and 09/H0502/91).
Immunohistochemistry
Two-micron sections were cut and stained immunohistochemically using an avidin-biotin technique and a panel of antibodies we have previously validated that facilitate the distinction and identification of epithelium with squamous metaplasia and fully squamous phenotype from tangentially cut epithelium in biopsy samples [32](Fig 1). This included mouse monoclonal antibodies to cytokeratin (CK) 7, CK13 and involucrin. We also used mouse monoclonal antibodies to pan-CKs (as a positive control), the proliferation marker Ki67 and to the early carcinogenesis markers p53 and carcinoembryonic antigen (CEA). Negative control sections were incubated with Tris-buffered saline (TBS) in replacement for the primary antibody. Further antibody details are shown in Table 2.
Table 2. Panel of antibodies used.
| Antibody | clone | Catalogue number | Supplier | Working concentration |
|---|---|---|---|---|
| CEA | II-7 | M7072 | Dako, Ely, UK | 0.2 ug/ml |
| CK7 | OV-TL 12/30 | M7018 | Dako, Ely, UK | 0.256 ug/ml |
| CK13 | KS-1A3 | C0791 | Sigma, Poole, UK | 4.94 ug/ml |
| Pan CK | C-11, PCK-26, CY-90, KS-1-A3, M20, A53-B/A2 | C2562 | Sigma, Poole, UK | dilution1:4000* |
| Involucrin | SY5 | MS-126-P1 | ThermoFisher Scientific, Runcorn, UK | 0.5 ug/ul |
| Ki67 | MIB-1 | M7240 | Dako, Ely, UK | 0.102 ug/ml |
| P53 | DO-7 | NCL-L-p53-DO7 | Novocastra, Leica Biosystems, Newcastle, UK | 0.875 ug/ml |
* concentration unavailable
The percentage lengths of epithelium that were either pseudostratified, were undergoing squamous metaplasia or were fully differentiated squamous epithelium, based on the patterns of cytokeratin and involucrin expression, were measured as a percent of total epithelial length (excluding tangentially cut) with the assistance of computerised image analysis (Zeiss KS400, Image Associates, Bicester, UK). The percentages of the epithelium staining for CEA as area ratio and the percentage nuclear epithelial area expression of p53 and Ki67, based on the red/green/blue colour composition of the DAB staining [35] within the intact epithelium, were assessed by computerised image analysis.
Statistical analysis
Non-parametric statistical tests were used to analyse the results of the immunohistochemical analysis and data presented as medians and interquartile ranges. The Kruskall-Wallis ANOVA test was used to test for differences between the 4 groups and, where appropriate, the Mann Whitney U test was used for further analyses, with p<0.05 considered statistically significant. The Spearman Rank test was used to test for correlations between immunohistochemical data and clinical parameters.
Results
Staining with CK7, CK13 and involurin enabled us to identify normal pseudostratified epithelium, that was undergoing squamous metaplasia and that had had undergone transition to a fully squamous epithelium (Fig 1). In normal pseudostratified epithelium the columnar and goblet cells were CK7+ and the basal cells CK13+. In squamous metaplasia CK13+ cells were seen throughout epithelium. In fully differentiated squamous epithelium involucrin+ cells were observed at the luminal surface (Fig 1).
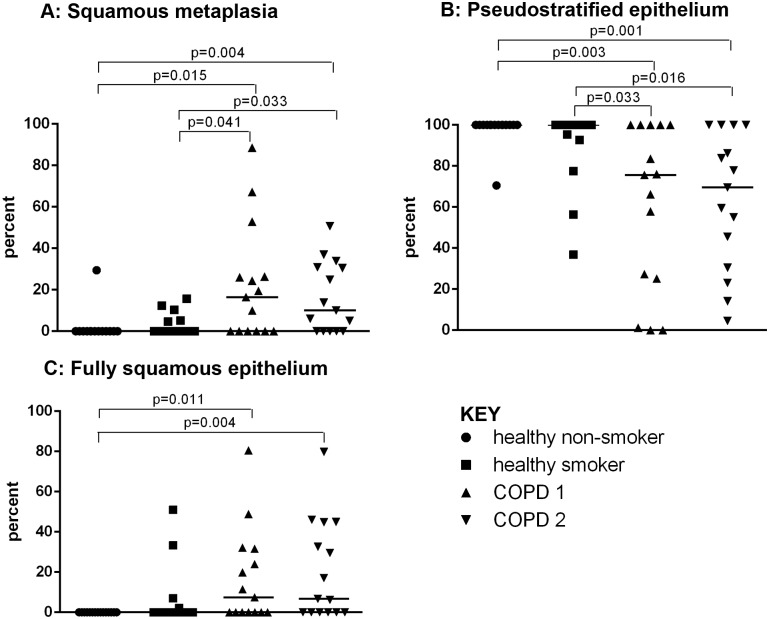
A mean length of 2.04mm of epithelium was assessed for each subject. The extent of squamous metaplasia was increased in both COPD1 and COPD2, 16.5% (0–23.4%) & 10.0% (0–30.9%), respectively, when compared to healthy smokers (0% (0–5.2%)(p = 0.041 & p = 0.033) and healthy non-smokers (0%(0–0%))(p = 0.015 & p = 0.004)(Fig 2A). This was paralleled by a decrease in pseudostratified epithelium (Fig 2B). The amount of fully differentiated squamous epithelium was also increased in COPD1 (7.4% (0–32.7%)) and COPD2 (6.67%(0–44.8%)) compared to healthy non-smokers (0%(0–0%)), p = 0.011 and p = 0.004, respectively but not healthy smokers (Fig 2C).
Fig 2. Graphs showing epithelial phenotype.
The percentage of epithelium with squamous metaplasia (A), that with a pseudostratified (B) and a fully squamous (C) phenotype are shown in healthy non-smokers (●), healthy smokers (■) and subjects with COPD1(▲) and COPD2(▼). Significant differences between the groups are indicated.
There was a positive correlation between the extent of this squamous metaplastic and fully differentiated squamous epithelium and a corresponding negative relationship to the amount of pseudostratified epithelium as it is replaced by these altered phenotypes (Table 3).
Table 3. Epithelial correlations.
| Fully squamous epithelium | Pseudostratified epithelium | CEA expression | Ki67 expression | |
|---|---|---|---|---|
| SQM Epithelium | Rho = 0.686 p<0.001 | Rho = -0.909 p<0.001 | Rho = 0.329 P = 0.010 | Rho = 0.408 P = 0.001 |
| Fully squamous epithelium | na | Rho = -0.885 p<0.001 | Rho = 0.407 p = 0.001 | Rho = 0.414 p = 0.001 |
| Pseudostratified epithelium | na | na | Rho = -0.423 p = 0.001 | Rho = -0.468 p<0.001 |
Spearman’s rho
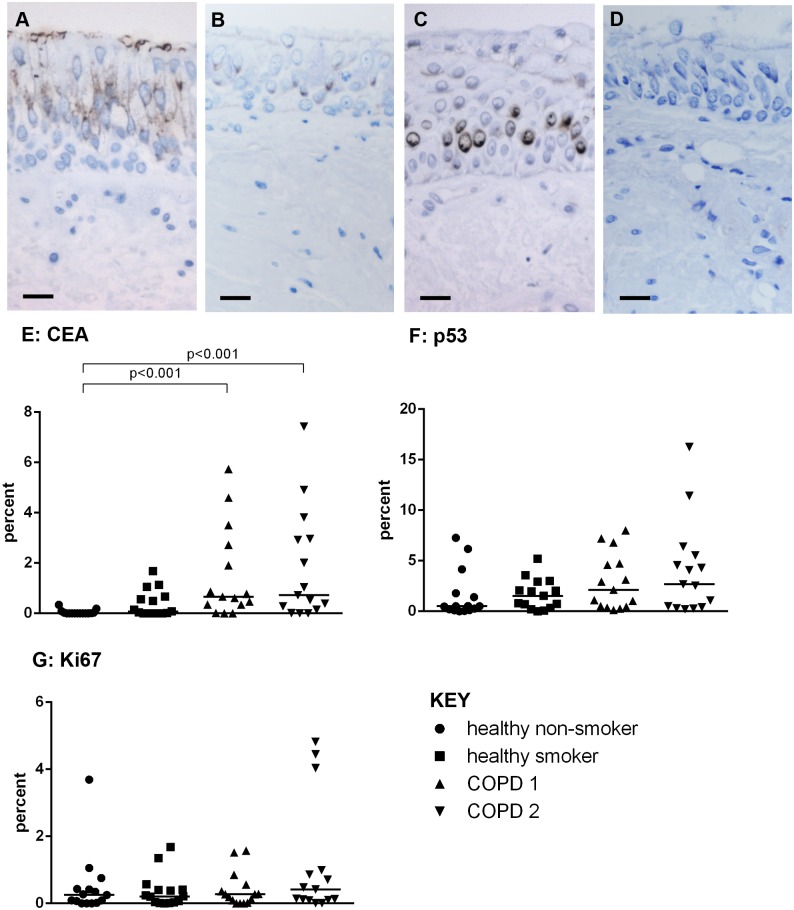
Staining for CEA was observed in the luminal cells of the pseudostratified bronchial epithelium (Fig 3A) and was increased in COPD1 (0.7% (0.3–2.7%)) and COPD2 (0.7%(0.1–3.0%)) compared to healthy non-smokers (0%(0–0%))(p<0.001 for both groups)(Fig 3E). P53 was weakly expressed in the perinuclear region of cells (Fig 3B), Ki67 staining was also nuclear (Fig 3C). There was no difference in the expression of p53 or Ki67 across the groups (KW p = 0.14 and p = 0.52, respectively)(Fig 3F and 3G)).
Fig 3. Epithelial expression of early markers of carcinogenesis and proliferation.
CEA is expressed in the luminal cells of pseudostratified epithelium (A), p53 is weakly expressed in the perinuclear region of suprabasal cells (B), nuclear expression of ki67 can also be seen (C). Positive staining is brown. No staining was observed in the negative controls sections (D). Scale bar = 20 um. The percentage of the epithelium expressing CEA (E), p53 (F) and Ki67 (G) are shown in healthy non-smokers (●), healthy smokers (■) and subjects with COPD1(▲) and COPD2(▼). Significant differences and Kruskall Wallis P values between the groups are indicated.
The expression of both CEA and Ki67 had a positive relationship with the amount of epithelium with squamous metaplasia and that with a fully differentiated squamous phenotype and a negative relationship with pseudostratified epithelium. There were no correlations with p53 (Table 3).
The epithelial phenotype and expression of CEA and Ki67correlated with lung function but not with smoking history (Table 4). There was a negative relationship between squamous metaplasia, the amount of fully squamous epithelium, CEA expression with both Forced Expiratory Volume in 1 second (FEV1) and Forced Vital Capacity (FVC) /FEV1 and a positive relationship between the amount of pseudostratified epithelium and lung function. Ki67 had a negative correlation with FEV1 only.
Table 4. Correlations between epithelial phenotype and measures of lung function.
| SQM epithelium | Fully squamous epithelium | Pseudostratified epithelium | CEA expression | Ki67 expression | |
|---|---|---|---|---|---|
| FVC/FEV1 | rho = -0.49 p<0.001 | rho = -0.44 p = 0.001 | rho = 0.51 p<0.001 | rho = -0.40 p = 0.001 | ns |
| FEV1 | rho = -0.42 p = 0.001 | rho = -0.40 p = 0.002 | rho = 0.44 p<0.001 | rho = -0.45 p<0.001 | Rho = -0.298 p = 0.021 |
Spearman’s rho
Discussion
This study demonstrates increased expression of epithelial markers that are consistent with a squamous metaplastic phenotype, together with a loss of normal pseudostratified epithelium, in smokers with COPD when compared to both healthy smokers and healthy non-smokers. Furthermore an increase in the amount of epithelium with a fully differentiated squamous phenotype is observed in smoking COPD patients when compared to healthy non-smokers (Figs 1 & 2). These changes are accompanied by increased expression of the early carcinogenesis marker, CEA.
To our knowledge this is the first study assessing the extent of SQM within the bronchial epithelium of smokers with and without COPD and healthy control participants. Cosio et al [1] have reported increased SQM in the small airways of subjects with FVC/FEV1 ratios in the COPD range compared to those with lung function in the normal range. Together these data suggest that SQM can occur throughout the airways in response to cigarette exposure.
SQM has been observed to be increased in the bronchial epithelium of COPD patients who are current smokers when compared to those who are ex-smokers [11] and to be related to the intensity of smoking (number of cigarettes smoked in a day), but not pack year history [3]. In our study, all of the COPD subjects were current smokers and we also did not observe any relationship with pack-year history. We found no difference in SQM between healthy non-smokers and healthy current smokers, suggesting that COPD is a contributing factor to these SQM changes rather than smoking alone. The correlation of SQM with both FVC/FEV1 and FEV1 may suggest that similar mechanisms are driving the loss of lung function and the development of SQM. This is supported by the study of Araya et al [36] who linked SQM with evidence of fibroblast activation and correlated this with small airway wall thickening in COPD and disease severity.
In our study transition to a fully differentiated squamous epithelium, indicated by positive staining for involucrin in epithelium with a squamous phenotype, was higher in subjects with COPD1 and 2 compared to healthy non-smokers but not compared to healthy smokers. This suggests this is a consequence of both smoking and COPD. This concurs with the study by Araya [36] in which increased intensity of involucrin staining was reported in samples obtained during surgery for lung cancer in patients who also had stage 2 and 3 COPD, when compared to healthy organ donor lungs.
A possible mechanism for this shift towards a squamous epithelial phenotype is via activation of the epidermal growth factor (EGF) / EGF receptor (EGFR) pathway due to the oxidative stress induce by cigarette smoke [37]. Shakhiev et al have demonstrated that EGF in air liquid interface cultures skews the epithelium to differentiate towards a squamous phenotype with the expression of cytokeratin 14 and involucrin [37]. We have previously demonstrated upregulation of EGFR in conjunction with goblet cell hyperplasia in these subjects, but did not investigate the relevance to the presence of SQM [38].
We also studied the expression of CEA and p53 markers of early carcinogenesis and the expression of the cell proliferation marker Ki67.
The expression of CEA in the bronchial epithelium was increased in subjects with COPD 1 and 2 when compared to healthy non-smokers and correlated with the extent of SQM and a fully differentiated squamous epithelium. Previous studies have found increased CEA levels in serum and secretions of healthy smokers and subjects with COPD compared to healthy non-smokers [39], but no difference with COPD severity [40], suggesting raised CEA is a marker of smoking rather than the presence of COPD. However, our data and that of Athanassiadou [13], have demonstrated that CEA expression is related to the pre-neoplastic change of SQM, suggesting that it could be a useful marker of this pre-neoplastic change.
We did not observe any differences in the expression of either p53 or Ki67 across our subject groups. P53, a tumour suppressor gene, expression is not observed in normal cells [41] but is reported to be expressed in areas of epithelium with SQM [42–44] increasing as the epithelium becomes more dysplastic [42,43,45,46]. Ki67 is also reported to be increased in areas of SQM, and to be of predictive value in the progression to lung cancer [44]. To our knowledge none of our subjects had lung cancer or a history of lung cancer so the pre-neoplastic changes we have observed may be early events in this transition process, and these markers may have yet to be upregulated. Also, we only assessed expression in areas of epithelium with a normal pseudostratified appearance we did not assess expression in areas of SQM which may have been more appropriate. However, we did observe a significant correlation between Ki67 expression and the extent of epithelium that had a SQM and a fully squamous phenotype. Therefore future work assessing the expression in SQM and epithelium with a fully squamous phenotype is warranted.
SQM is a reversible pre-neoplastic change in the epithelium [8–10]. On long-term cessation of smoking, Lapperre et al [11] report a reduction in SQM in patients with COPD when compared to current smokers with COPD. Cessation also reduces the risk of progression to lung cancer [47, 48], as does corticosteroid therapy [49]. Hence early detection of these pre-neoplastic changes is important to facilitate early intervention. This is a challenge as at this early stage patients are asymptomatic, only presenting when progression to lung cancer has occurred. Autofluorescence bronchoscopy facilitates earlier detection of pre-invasive lesions [10,50–52] especially if used with appropriate biomarkers and histological assessment. This may be a strategy for monitoring high risk patients.
In conclusion we demonstrated that there is a loss of the normal pseudostratified epithelium in smokers with COPD together with pre-neoplastic changes evidenced by increased presence of SQM and fully differentiated squamous epithelium, together with expression of CEA. This may warrant aggressive smoking cessation strategies, with long-term follow up to assess regression to a normal phenotype or progression to lung cancer.
Acknowledgments
The authors wish to acknowledge the NIHR Southampton Respiratory Biomedical Research Unit for help with the bronchoscopies and the Histochemistry Research Unit for support with the immunohistochemical staining.
Data Availability
All relevant data are within the paper.
Funding Statement
The authors have no support or funding to report.
References
- 1.Cosio M, Ghezzo H, Hogg JC, Corbin R, Loveland M, Dosman J, et al. The relationship between structural changes in small airways and pulmonary function tests. N Engl J Med 1977; 298: 1277–1281. [DOI] [PubMed] [Google Scholar]
- 2.Mathe G, Gouveia J, Hercend T, Gros F, Dorval T, Hazon J, et al. Correlation between precancerous bronchial metaplasia and cigarette consumption, and preliminary results of retinoid treatment. Cancer Detect Prev 1982; 5: 461–466. [PubMed] [Google Scholar]
- 3.Peters EJ, Morice R, Benner SE, Lippman S, Lukeman J, Lee JS, et al. Squamous metaplasia of the bronchial mucosa and its relationship to smoking. Chest 1993; 103: 1429–1432. [DOI] [PubMed] [Google Scholar]
- 4.Barsky SH, Roth MD, Kleerup EC, Simmons M, Tashkin DP. Histopathological and molecular alterations in bronchial epithelium in habitual smokers of marijuana, cocaine and/or tobacco. J Natl Cancer Inst 1998; 90: 1198–1205. [DOI] [PubMed] [Google Scholar]
- 5.Jetten AM. Multistep process of squamous differentiation of tracheobronchial epithelial cells in vitro. Analogy with epidermal differentiation. Environ Health Perspect 1989; 80: 149–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leube RE, Rustad TJ. Squamous cell metaplasia in the human lung: molecular characteristics of epithelial stratification. Virchows Arch B Cell Pathol Incl Mol Pathol 1991; 61: 227–253. [DOI] [PubMed] [Google Scholar]
- 7.Wistuba II, Behrens C, Milchgrub S, Bryant D, Humg J, Minna JD, et al. Sequential molecular abnormalities are involved in the multistage development of squamous cell lung carcinoma. Oncogene 1999; 18: 643–650. [DOI] [PubMed] [Google Scholar]
- 8.Bertram JF, Rogers AW. Recovery of bronchial epithelium on stopping smoking. Br Med J 1981; 283: 1567–1569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Breuer RH, Pasic A, Smit EF, van Vilet E, Noordegraaf AV, Risse EJ, et al. The natural course of pre-neoplastic lesions in bronchial epithelium. Clin Can Res 2005; 11: 537–543. [PubMed] [Google Scholar]
- 10.George PJ, Banerjee AK, Read CA, O’Sullivan C, Falzon M, Pezzella F, et al. Surveillance for the detection of early lung cancer in patients with bronchial dysplasia. Thorax 2007; 62: 43–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lapperre TS, Sont JK, van Schadewijk A, Gosman MME, Postma DS, Bajema IM, et al. GLUCOLD study group. Smoking cessation and bronchial epithelial remodelling in COPD: a cross-sectional study. Respir Res 2007; 8: 85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moll R, Franke WW, Schiller DL, Geiger B, Krepler R. The catalog of human cytokeratins: patterns of expression in normal epithelia, tumours and cultured cells. Cell 1982; 31: 11–24. [DOI] [PubMed] [Google Scholar]
- 13.Athanassiadou P, Psyhoyou H, Kyrkou K, Athanassiades P, Moulopoulos S. Expression of keratins and carcinoembryonic antigen in bronchial squamous metaplasia and lung carcinomas. Acta Cytol 1995; 39: 1161–1166. [PubMed] [Google Scholar]
- 14.Fisseler-Eckhoff A, Erfkamp S, Muller K-M. Cytokeratin expression in pre-neoplastic lesions and early squamous cell carcinoma of the bronchi. Pathol Res Pract 1996; 192: 552–556. [DOI] [PubMed] [Google Scholar]
- 15.Wong Y-C, Kakefuda M, Bernal SD. A new membrane marker for commitment of the human bronchial epithelial cells to terminal squamous differentiation. In Vivo 1997; 11: 495–498. [PubMed] [Google Scholar]
- 16.Said JW, Nash G, Sassoon AF, Shintaku IP, Banks-Schlegel S. Involucrin in lung tumours. A specific marker for squamous differentiation. Lab Invest 1983; 49: 563–568. [PubMed] [Google Scholar]
- 17.Godtfredson NS, Prescott E, Osler M. Effect of smoking reduction on lung cancer risk. JAMA 2005; 294: 1505–1510. [DOI] [PubMed] [Google Scholar]
- 18.Rooney C, Sethi T. The epithelial cell and lung cancer: the link between chronic obstructive pulmonary disease and lung cancer. Respiration 2011; 81: 89–104. 10.1159/000323946 [DOI] [PubMed] [Google Scholar]
- 19.Dubey S, Powell CA. Update in lung cancer 2007. Am J Respir Crit Care Med 2008; 177: 941–946. 10.1164/rccm.200801-107UP [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Caramori G, Casolari P, Cavallesco GN, Giuffre S, Adcock I, Papi A. Mechanisms involved in lung cancer development in COPD. Int J Biochem Cell Biol 2011; 43: 1030–1044. 10.1016/j.biocel.2010.08.022 [DOI] [PubMed] [Google Scholar]
- 21.Koshiol J, Rotunno M, Consonni D, Pesatori AC, De Matteis S, Goldstein AM, et al. Chronic obstructive pulmonary disease and aletred risk of lung cancer in a population-based case-controlled study. PLoS One 2009; 4: e7380 10.1371/journal.pone.0007380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brennar DR, McLaughin JR, Hung RJ. Previous lung disease and lung cancer risk; a systematic review and meta-analysis. PLoS One 2011; 6: e17479 10.1371/journal.pone.0017479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Skillrud DM, Offord KP, Miller RD. Higher risk of lung cancer in chronic obstructive pulmonary disease. A prospective, matched, controlled study. Ann Intern Med 1986; 105: 503–507. [DOI] [PubMed] [Google Scholar]
- 24.Tockman MS, Anthonisen NR, Wright EC, Donithan MG. Airways obstruction and the risk of lung cancer. Ann Intern Med 1987; 106: 512–518. [DOI] [PubMed] [Google Scholar]
- 25.Papi A, Caramori G, Guzzinati I, Boschetto P, Ravenna F, Calia N, et al. COPD increases the risk of squamous histological subtype in smokers who develop non-small cell lung carcinoma. Thorax 2004; 59: 679–681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.De Torres JP, Marin JM, Casanova C, Cote C, Carrizo S, Cordoba-Lanus E, et al. Lung cancer in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2011; 184: 913–919. 10.1164/rccm.201103-0430OC [DOI] [PubMed] [Google Scholar]
- 27.Yao H, Rahman I. Current concepts on the role of inflammation in COPD and lung cancer. Curr Opin Pharmacol 2009; 9: 375–383. 10.1016/j.coph.2009.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Barnes PJ, Adcock IM. Chronic obstructive pulmonary diseases and lung cancer: a lethal association. Am J Resp Crit Care Med 2011; 184: 866–867. 10.1164/rccm.201108-1436ED [DOI] [PubMed] [Google Scholar]
- 29.Houghton AM, Mouded M, Shapiro SD. Common origins if lung cancer and COPD. Nat Med 2008; 14: 1023–1024. 10.1038/nm1008-1023 [DOI] [PubMed] [Google Scholar]
- 30.Wasswa-Kintu S, Gan WQ, Man SFP, Pare PD, Sin DD. Relationship between reduced forced expiratory volume in one second and the risk of lung cancer: a systematic review and meta-analysis. Thorax 2005; 60: 570–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Balkwill F, Mantovani A. Inflammation and cancer; back to Virchow? Lancet 2001; 357: 539–545. [DOI] [PubMed] [Google Scholar]
- 32.Merrifield J, O’Donnell R, Davies DE, Djukanovic R, Wilson SJ. A panel of antibodies for identifying squamous metaplasia in endobronchial biopsies from smokers. Biotech Histochem 2011; 86: 340–4. 10.3109/10520295.2010.502844 [DOI] [PubMed] [Google Scholar]
- 33.Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease. NHLBI / WHO workshop report. Bethesda, National Heart, Lung and Blood Institute, April 2001 updated 2013.www.goldcopd.org
- 34.O’Donnell RA, Peebles C, Ward JA, Daraker A, Angco G, Broberg P, et al. relationship between peripheral airway dysfunction, airway obstruction and neutrophilic inflammation in COPD. Thorax 2004; 59: 837–842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Puddicombe SM, Polosa R, Richter A, Krishna MT, Howarth PH, Holgate ST, et al. Involvement of the epidermal growth factor receptor in epithelial repair in asthma. FASEB J 2000; 14: 1362–1374. [DOI] [PubMed] [Google Scholar]
- 36.Araya J, Cambier S, Markovics JA, Wolters P, Jablons D, Hill A, et al. Squamous metaplasia amplifies pathologic epithelial-mesenchymal interactions in COPD patients. J Clin Invest 2007; 117: 3551–3562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shaykhiev R, Zuo W-L, Chao I, Fukui T, Witover B, Brekman A, et al. EGF shifts human airway basal cell fate toward a smoking-associated airway epithelial phenotype. PNAS 2013; 110: 12102–12107. 10.1073/pnas.1303058110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.O’Donnell R, Richter A. Ward J, Angco G, Mehta A, Rousseau K, et al. Expression of ErbB receptors and mucins in the airways of ling term current snokers. Thorax 2004; 59: 1032–1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Stockley RA, Sha J, Whitfiled AGW, Whitehead TP, Clarke CA, Burnett D. Effect of cigarette smoking, pulmonary inflammation and lung disease on concentrations of carinoembryonic antigen in serum and secretions. Thorax 1986; 41: 17–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bulut I, Arbak P, Coskan A, Balbay O, Annakkaya AN, Yavuz O, et al. Comparison of serum CA 19.9, CA 125 and CEA levels with severity of chronic obstructive pulmonary disease. Med Princ Pract 2009; 18: 289–293. 10.1159/000215726 [DOI] [PubMed] [Google Scholar]
- 41.Chang F, Syrjänen A, Tervahauta A, Syrjänen K. Tumourgenesis associated with the p53 tumour suppressor gene. Br J Cancer 1993; 68: 653–661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bennet WP, Colby TV, Travis WD, Borkowski A, Jones RT, Lane DP, et al. p53 protein accumulates frequently in early bronchial neoplasia. Cancer Res 1993; 53: 4817–4822. [PubMed] [Google Scholar]
- 43.Klein N, Vignaud JM, Sadmi M, Plenat F, Borelly J, Duprez A, et al. Squamour metaplasia expression of proto-oncogenes and p53 in lung cancer patients. Lab Invest 1993; 68: 26–32. [PubMed] [Google Scholar]
- 44.Boers JE, Ten Velde GPM, Thunnissen FBJM. P53 in squamous metaplasia: a marker for risk of respiratory tract carcinoma. Am J Respir Crit Care Med 1996; 153: 411–416. [DOI] [PubMed] [Google Scholar]
- 45.Rusch V, Klimstra D, Linkov I, Dmitrovsky E. Aberrant expression of p53 or the epidermal growth factor receptor is frequent in early bronchial neoplasia, and coexpression precedes squamous cell carcinoma development. Cancer Res 1995; 55; 1365–1372. [PubMed] [Google Scholar]
- 46.Ponticiello A, Barra E, Giani U, Bocchino M, Sanduzzi A. p53 immunohistochemistry can identify bronchial dysplastic lesions proceeding to lung cancer: a prospective study. Eur Respir J 2000; 15: 547–552. [DOI] [PubMed] [Google Scholar]
- 47.Anthonisen NR, Skeans MA, Wise RA, Manreda J, Kanner RE, Connett JE. The effects of a smoking cessation intervention on 14.5 year mortality. Anns Int Med 2005; 142: 233–239. [DOI] [PubMed] [Google Scholar]
- 48.Dragnev KH, Stover D, Dmitrovsky E. Lung cancer prevention; the guidelines. Chest 2003; 123: 60s–71s. [DOI] [PubMed] [Google Scholar]
- 49.Parimon T, Chien JW, Bryson CL, McDonell MB, Udris EM, Au DH. Inhaled corticosteroids and risk of lung cancer among patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2007; 175: 712–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Paris C, Benichou J, Bota S, Sagnier S, Metayer J, Eloy S, et al. Occupational and nonoccupational factors associated with high grade bronchial pre-invasive lesions. Eur Respir J 2003; 21: 32–341. [DOI] [PubMed] [Google Scholar]
- 51.Haussinger K, Becker H, Stanzel F, Kreuzer A, Schmidt B, Strausz J, et al. Autofluorescence bronchoscopy with white light bronchoscopy compared with white light bronchoscopy alone for the detection of precancerous lesions: a European randomized controlled multicenter trial. Thorax 2005;60:496–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Loewen G, Natarajan N, Tan D, Nava E, Klippenstein D, Mahoney M, et al. Autofluorescence bronchoscopy for lung cancer surveillance based on risk assessment. Thorax 2007;62:335–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.