Background
There is increasing demand for home healthcare services and for home healthcare professionals (HHP) to provide needed services. As a workplace, the home environment can be more challenging and variable than other environments, including HHP exposure to varying types of personal health and safety hazards. Although HHP are at high risk of injury and illness, health and safety training is limited, inconsistent, and often incomplete (Centers for Disease Control and Prevention, 2010; Gershon, Dailey, Magda, Riley, Conolly, & Silver, 2012). Existing training approaches are often constrained to written or video-based information, or one-time only passive lectures in classroom settings. There is a need for more active learning methods that can overcome the limitations of these existing approaches.
Zyda (2005) defines Serious Games as “…a mental contest, played with a computer in accordance with specific rules that uses entertainment to further government or corporate training, education, health, public policy, and strategic communication objectives” (p. 25). As an example, Thompson (2007) noted, “Video games, enhanced by behavior-change technology and motivating story lines, offer promise for promoting diet and physical activity change for diabetes and obesity prevention in youth” (p. 916). In contrast, interactive training and assessment methods currently used for training HHP do not engage learners in immersive, interactive training experiences. Clinical simulations offer an alternative to more passive methods of instruction such as classroom lecture, reading, and video viewing. Simulations, which often include physical mockups, mannequins, theatre props, and/or actors, are more interactive and can incorporate the more typical complexities of a home healthcare environment (see Figure 1) (Polivka, Chaudry, & Crawford, 2012; Unsworth, Tuffnell, & Platt, 2011). When providing education on home safety issues, in-person, on-site clinical simulations provide naturalistic ways to expose trainees to hazards in the environment as they navigate through the space. However, on-site simulations often provide limited variability in training experiences, can be costly to construct, maintain, and upgrade, and require the use of physical space, which is often hard to come by, to support often sporadic usage. Additionally, trainees must be at a specific location at a specific time, which may not be convenient or feasible for HHP who often commute between their home and their client’s home and who may rarely visit their agency’s office.
Figure 1.

Scenes from physical theatrical mock-up that was previously used to educate nursing students regarding health and safety hazards within the home.
The use of virtual environments (VE) can successfully overcome these barriers and may have equivalent or superior learning outcomes relative to traditional training approaches. Virtual environments have successfully been used for training and education in a variety of healthcare situations (Feng, Chang, Erdley et al., 2013; Ferrer-García, & Gutiérrez-Maldonado, 2012; Foran, 2011; Stredney, Carlson, Swan,, & and Blostein, 1995). Currently, the Department of Labor’s Occupational Safety & Health Administration (OSHA) is using the Unity™ game engine to provide an interactive, game-based tool to introduce small business owners to work site hazards (OSHA-2015). Advantages of VE include: (1) the ability to precisely track each participant’s activity (e.g., location, direction of gaze, selection, and time on task) during simulated learning events, (2) the ability to quantify and classify risk perception and decision-making, and (3) the ability to tailor the training to the specific needs of the trainee group of interest by engaging them in targeted activities.
A virtual, game-based environment, crafted to represent a realistic and accurate home healthcare environment and containing hazards relevant to the multiple professional disciplines working in home healthcare, has the potential to provide accessible, effective, and engaging training that is both appropriate and relevant to multiple types of home healthcare professionals. The purpose of this paper is to describe the process used for developing and evaluating an interactive virtual simulation training system (VSTS) to educate HHP. The content emphasizes key details of the participatory process used for creating the initial version of the VSTS that could be used and/or adapted for multiple types of virtual training simulations targeted to training of diverse groups of healthcare professionals.
Sample
Occupational therapists, physical therapists, nurses, administrators/educators, and home health aides were eligible to participate in the study if they: 1) identified home healthcare as their primary work setting; and, 2) were able to converse, read, and write in English. Participants were recruited using informational flyers and emails distributed to home healthcare agencies. The study protocols and consent procedures were approved by The Ohio State University and University of Louisville Institutional Review Boards. Participants received a $50 department store gift card as a study incentive.
Method
Participatory Design Process
Study Design
In order to design the VSTS, the interdisciplinary research team used a mixed methods approach, which included a participatory, user-centered, and iterative process to identify the layout and features of a typical client home, the health and safety hazards typically encountered in the home, and worker responses to health and safety hazards. The participatory design process involved completion of a preliminary survey and structured focus group and individual interviews with embedded activities. Once a working version of the VSTS was created, we initiated an ongoing assessment of the usefulness, usability, and desirability (UUD) of the system to facilitate continued development and modification. The development of the initial version of the VSTS is emphasized here.
Instruments and Data Collection
Quantitative data collection included completion of two assessments: the Modified Home Healthcare Worker Questionnaire (MHHWQ), which includes questions about demographics, professional affiliation, work history, and commonly encountered hazards, and the Usefulness, Usability and Desirability (UUD) survey assessment, which includes ratings of the ease of use of the simulation, value and applicability to professional health and safety, and overall appeal or interest in the VSTS as a health and safety training tool. The MHHWQ was completed prior to the start of each focus group/individual interview during the initial development of the VSTS. Once developed, participants were invited to return and interact with the preliminary version of the VSTS, complete the UUD assessment, and provide the research team with feedback and input.
Qualitative data collection included structured focus group/individual interviews with embedded activities. Focus group and interview participants took part in an in-depth discussion of the hazards they encountered and completed an activity in which they created drawings of rooms and hazards, prioritized hazards, and provided insights about VSTS design (such as the time to complete a training module) and what hazards should be included. Once the preliminary working version of the VSTS was created (basic four-room home environment consisting of living room, kitchen, bathroom, bedroom), participants were, and continue to be, invited back to review the VSTS, in small groups or individually, as part of the ongoing UUD evaluation of the preliminary version of the VSTS. They provide feedback about the overall design, including the appearance, specific hazards, and methods for conveying information, and answer questions on topics such as access, ease of use, realistic depiction of environments, length of time, and structure of content.
Virtual Simulation Modeling
Insert publisher after modeling software as follows: The VSTS was modeled using a combination of software including Autodesk Maya™ 2015 (Autodesk, CA), Autodesk Mudbox™ 2015 (Autodesk, CA), and Adobe Photoshop™ C56 (Adobe Systems, CA) to structurally model, color, and pattern various household items. 3D modeling was completed using Maya™. The 3D gaming engine, Unity 3D™ (Unity Technologies, CA), was used to interactively visualize and navigate the virtual environment. Unity3D™ is free to use with basic functionality. Expanded features can be obtained for a nominal research/educational license fee. The simulation can be run as a stand-alone program, or in a web browser. Unity 3D™ plugins are available for both Windows™ and Mac OS X ™. The goal is to provide an immersive, highly realistic, interactive 3D world for the VE that is accessible to individuals with lower end technology and slower internet speeds.
Data Analysis
Quantitative data (MHHWQ and UUD assessment tools) were analyzed descriptively (SPSS v.21). Focus group/individual interviews and participant drawings were analyzed qualitatively. Interviews and discussions were recorded, transcribed, verified, and analyzed. Transcripts were independently coded by a minimum of two researchers. Researchers routinely met to discuss discrepancies in coding and reconcile discrepancies to 100% agreement. A detailed room by room analysis also was completed to examine hazard concentration and distribution across the home (Polivka et al., 2015). Drawings were analyzed by participants and investigators. Participant consensus about priority hazards was achieved through a systematic method of hazard prioritization in which the participants placed color-coded sticky dots on hazards to indicate relative priority, and then discussed them as a group to come to agreement. Data sources and analysis were triangulated to establish credibility, and final themes were confirmed in multiple consensus meetings. Prioritized hazards were verified through a process of member checking and review of available literature, injury/illness data from the Bureau of Labor Statistics, and expert review. Usability, usefulness, and desirability of the VSTS were assessed qualitatively, through participant feedback, and quantitatively through the completion of the UUD assessment instrument. The UUD is an iterative process that continues to inform changes to the VSTS.
Results
Participants
Sixty-eight HHP participated in the study. The majority were female (95%) and white (71%). Approximately 67% worked in Ohio and Kentucky, with the remaining spread throughout the United States. They represented multiple professions, including registered nurses (31%), aides/homemakers (21%), administrators/educators (19%), and physical/occupational therapists (19%). The average age of participants was 49 years (SD=11.8). Of those, seven participated in member checking to ensure we accurately captured the hazards and realistically depicted the environment and four, to date, returned to complete the UUD assessment of the initial version. For a detailed description of study participants, see Polivka et al., 2015.
The detailed results of the data analyses used to design the initial version of the VSTS have been published elsewhere (Polivka et al., 2015; Wills et al., 2015). In brief, analysis of the MHHWQ and the focus group/individual interviews revealed that participants routinely encounter hazards in client homes. They identified multiple, discrete hazards that were organized into three large categories: trip/slip/lift (e.g. clutter, throw rugs), environmental (e.g. bodily fluids, tobacco smoke), and electrical/fire (e.g. overloaded outlets, damaged electrical cords). The analysis of the drawings from the focus group/individual interviews revealed the locations where these hazards were typically encountered (e.g. water on the floor as a slip hazard in the bathroom and kitchen). These elements formed the basis of the home and individual room design. The process was iterative; in other words, the process of developing the home, rooms, and hazards was an ongoing process, continually informed by additional focus group/individual interviews and analyses.
In addition, HHP described 353 hazard management dilemmas with these hazard categories. They explained multiple types of “making do” solutions for the hazards, most of which were classified as “less-than-optimal,” in which HHP set their needs aside, delayed action, and/or focused on suboptimal solutions (Wills et al., 2015). Lack of resources, training, and/or administrative policies, beliefs about available options, and the placement of the needs of the client over their own health and safety are the primary reasons for the use of these sub-optimal decisions. These issues reflect a training need, and receive particular emphasis in the VSTS.
Discussion
Modeling of the VSTS
The initial version of the VSTS was modeled based on the results of both quantitative and qualitative data analysis reading types of hazards and common environmental features. Using the information gained from the participants, a prototype VE was developed that combined features of the home healthcare environment identified through input from HHP together with a cost-effective training environment that does not expose the learner to hazardous conditions. In general, the VE included the representation of various rooms, the targeted hazards, and distractors.
The VE began as a basic 4-room environment (Figure 2), into which was added greater detail through the iterative design and analysis process. An archetypical dwelling was created, consisting of a modest living room, kitchen, bedroom, and bathroom, along with associated closets and hallways. Eventually, as data analyses of the interviews and drawings were completed and interpreted, a limited basement (with laundry facility) and a second floor bedroom with a full bathroom were added.
Figure 2.
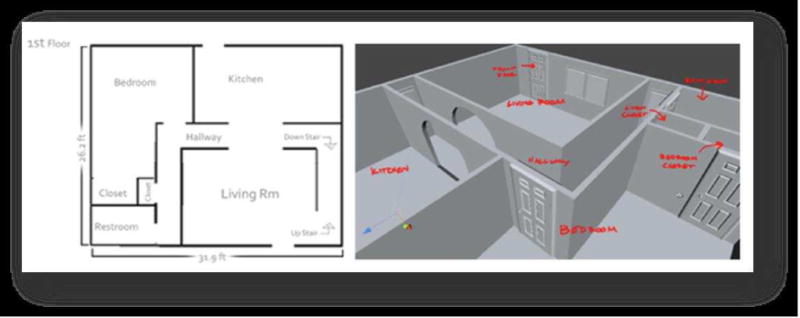
The two and three dimensonal representations of the floor plan for the home that was incorporated into the VSTS.
Upon completion of the architectural plans, the 3D environment was modeled. Predominantly, the models are comprised of a polygonal surface to depict form, with texture mapping to impart colors, patterns, and surface attributes, such as dirt. These structural components included walls, doors, windows, light switches and electrical outlets. By frequently posting updates to the game in a web version, we were able to tighten the design cycle and increase iterations with research team members, facilitating more rapid modifications and the introduction of nuances. Web conferencing allowed the research team to commonly view the game to discuss and clarify updates and modifications, and focus the interdisciplinary team’s development efforts.
Assets
Following completion of the 3D architecture, a list of assets (key objects and effects in the VE) was determined and developed. Assets included typical furniture (e.g., bed, tables, chairs), appliances (e.g., stove, refrigerator, heaters, lights), household items (e.g., books, dishes, bottles, drapes), and special effects (e.g. smoke, fire, pet/companion animal movements). The types and locations of these assets were based on the analysis of focus group/individual interviews and drawings. For example, participants described homes where books were stacked on bookshelves and other homes where books were included in clutter and posed a slip/trip hazard.
Hazards
Grounded in analysis of the focus group/individual interview hazard data, we adopted a pedagogical design that is case-based and includes three Training Modules based on three primary categories of hazards that emerged from our analyses: (1) Electrical and Fire, (2) Slip, Trip and Lift, and (3) Environmental, and one Evaluation Module that combines all hazard categories into one assessment environment. Hazards identified by participants were further investigated by the research team to confirm they were hazardous (e.g. are overloaded outlets identified as hazardous by electrical and fire experts?), to determine the extent to which they were associated with illness or injury to HHP (e.g. is lifting a patient associated with illness or injury according to BLS injury data?), and to determine the appropriate responses (e.g. what actions should be taken if an HHP observes a client smoking while using oxygen, according to fire prevention experts and oxygen suppliers). If necessary, hazards were removed or modified (e.g. the explanation of spoiled food as a hazard, identified by many participants, was modified to indicate that it is not a hazard if not touched or consumed, but is if eaten).
The Electrical and Fire module includes hazards such as overloaded outlets, frayed/damaged electrical cords, oxygen use and cigarette smoking, and unattended candles. The Slip, Trip, Lift module includes hazards such as clutter, space-restricted work areas, and throw rugs. The Environmental module includes hazards such as human waste and bodily fluids, pests, and second-hand smoke. Ecological validity of hazard distribution was confirmed through ensuring that the distribution of hazards in the VSTS was consistent with the distribution of hazards revealed in the analyses of the room drawings (Polivka et al., 2015). UUD review of the hazards, to date, reveals that the hazards are accurate, and that they are placed appropriately.
Cases were designed to provide HHP with initial cues regarding potential hazards, and are embedded with client characteristics and hazards that emerged from the data analysis. One example is a smoker in the Electric and Fire training module who uses home oxygen, which is considered a potential fire hazard. A second example, in the Slip, Trip, and Lift training module, is a client with limited mobility who does not have grab bars in the bathroom and thus poses a potential musculoskeletal injury hazard to the HHP. The basic environment remains constant in each module; however, hazards and specific assets vary to allow users to focus on particular environmental features. For example, supplemental oxygen and space heaters are in use in the Electrical and Fire training module, but not in the other two training modules (Figure. 3).
Figure 3.

A kitchen view in the VSTS. Note performance information is provided in the upper-left corner of the screen as to the number of hazards that have been found.
Tracking Progress through the Game
Study participants advised that the VSTS should contain elements similar to a game, such as a score, and feedback about correct and incorrect answers. A running count is provided that tells the game user the number of hazards that have been identified in each room and in the entire VSTS learning module. This “score” is shown in the upper left of the screen (Figure 3). Each module is comprised of seven rooms, one hallway, and two staircases within the house where a given number of hazards can be found. By selecting the object and properly identifying it as a hazard (or not) one gains a point towards their total score. With each identified hazard within the VSTS, users obtain information regarding the significance of the hazard and options on how to manage the hazards, particularly options that are within their control. Results of UUD to date confirm that this is a valued addition to the VSTS.
For a subset of hazards, there are additional “Think About” questions posed to users that prompt further reflection and support development of critical thinking about these selected hazards. For example, an unattended candle yields the following “Think About” question: “What happens when an unattended lit candle is left near a lampshade”? A space heater in a home with oxygen in use queries, “What other kinds of motorized appliances have you seen in homes that could cause a spark and a fire in a home where there is oxygen in use?” “Think About” questions promote a sense of control over hazard responses, facilitating thoughtful reflections about available options to the HHP for solution development.
Movement and Navigation
The user selectively moves through the VE using the basic keys of “W” (forward), “A” (left), “S” (back), and “D” (right). This paradigm is prevalent and familiar to those more accustomed to gaming. However, for those who are less “gaming literate”, it presents a learning curve that can be frustrating to the user. In a recent UUD session, some participants reported difficulty and reluctance to use these keys to move through the environment. We have built a training module to familiarize the user with this method of navigation and are exploring the introduction of new interfaces to provide more intuitive navigation through the VE (see discussion below).
Selection of Objects in the Game and Dialogue Box
Selecting objects involves placing the mouse pointer over an object. This causes the object to become tinted white and provides the user with a visual confirmation of their selection. A mouse click then engages the dialogue box. The dialogue box provides the main interface between the user and the game pedagogy (Figure 4). Upon successful selection of an object, the scene is locked. A dialogue box appears and queries the user whether the selected item on the screen is or is not a hazard. If the participant selects, “Yes” to the question of, “Is this a hazard?” an appropriate hazard symbol is displayed and the “Continue” button appears green. Selecting the green “Continue” button leads the user to information about “Why” the selected object is a hazard, which is then followed via another press of the “Continue” button with information about “What to do” about the selected hazard if it is encountered during their work process. Some items have a “testable” function, i.e., on/off, or open/close, that allow the user to press a test button, which will appear green, so the function can be tested. A final selection of “Continue” returns the user to the game.
Figure 4.

Consequences were of selected hazards were modeled using animation effects. In this image from the living room a lampshade is shown to be on fire which resulted from an untended candle.
Design, Delivery and Dissemination
We have created an interactive VSTS that is intended to be part of an improved methodology for training and assessment of HHP. As the virtual simulation technologies continue to advance, we envision more realistic emulations that provide an even more immersive and engaging environment. It is expected that the immediate scoring of performance and more continuous assessment will result in an increased desire to train and improve, eventually leading to better-informed professionals. It is also anticipated that the use of simulation for training and assessment will contribute to fewer injuries experienced at work for both the HHP and their clients. Future research will test both of these hypotheses.
The design, delivery, and dissemination of trainings such as this can be challenging. The adult learners engaging in such trainings are diverse in educational background, experience, care duties and responsibilities, as well as in their access to training technology. As the need for HHP rapidly increases, a broadly available and innovative system of training will be required (IOM/NRC, 2015). This project aims to develop a computerized VSTS that meets the needs of the adult learner and provides accessible, effective, and engaging instruction to a diverse population of home healthcare professionals. Additionally, HHP face fairly unique challenges in their work environments, which are rife with complexity and variability. Trainings must therefore prepare them for autonomous problem solving and decision making, requiring active, not passive, engagement in the training course.
Several key features of the VSTS facilitate the active learning and critical thinking processes that are crucial for HHP. In general, HHP are highly autonomous professionals who work independently in an unpredictable environment and must problem solve to create solutions to unexpected or complicated events that affect their health and safety, and the health and safety of their clients. Health and safety trainings, therefore, must emphasize realistic scenarios, flexible solutions, and independent problem solving activities.
The VSTS includes immersion in a realistic and compelling environment, engagement through a process of identification, response, and problem solving (‘think about’ feature described above), and feedback. The processes of engaging in the virtual environment, assessing the environment for hazards in multiple rooms, receiving feedback both about successful identification and correct and incorrect answers, problem solving about potential strategies, and assessment of progress in both a training and evaluation environment facilitate deliberate practice, a powerful component of skill acquisition (Ericsson, 2004; McGaghie et al., 2010). Immersion in simulation has the added advantage of encouraging engagement and deliberate practice, including consequences of errors, without risking adverse patient consequences (Keengwe, 2015; Issenberg et al., 2005), and can enhance procedural skills, perceptual interpretation, and knowledge (Issenberg et al., 1999).
Formative feedback, provided each time a participant selects a hazard, informs the user whether their identification of a hazard was correct/incorrect and the rationale for the correct answer. Summative feedback is provided at the conclusion of the game, when users receive an overall score, based on the number of hazards they identified in the simulation. Both forms of feedback contribute to effective learning in clinical simulation (McGaghie et al., 2010). Developing expertise as a healthcare provider involves immersion, opportunities for decision making and problem solving, and discrimination between solutions in one context versus another (Dreyfus, 2004). The VSTS allows the user to engage with a realistic environment, evaluate hazards, and identify solutions. Particularly challenging situations, in which no single solution is readily available or apparent, include opportunities for independent reflection and problem solving. High fidelity with real life, complex scenarios was achieved through the participatory, iterative process of development, and, we believe, will contribute to the translation of skills acquired in the VSTS to clinical practice.
The current VSTS is designed to be accessible to users from multiple disciplines. To this end, it was designed by a multidisciplinary team and multidisciplinary pool of participants. The hazards are comprehensive and reflect the varied perspectives of these professionals. Indeed, opportunities for inter-professional learning exist with the VSTS: when done in a group training setting, users can discuss the hazards and problem solve as a team. Inter-professional simulation training has been shown to improve self-efficacy, communication, and understanding of professional roles (Tofil et al, 2014).
Future Directions
Currently, we are integrating more precise methods of position tracking, allowing for more intuitive interfaces. By moving toward more intuitive interfaces in our VE, we hope to accommodate those not as familiar with gaming movement protocols. For example, future versions of this virtual simulation training system could include sonic and optic tracking, instrumented gloves, gesture recognition, and the use of a head mounted display such as the Oculus Rift. Thus in lieu of a keyboard, mouse, or even a game controller, a participant could gesture using instrumented gloves. Instead of limited space directly in front of the display, a more ambulatory, free-ranging navigation can be achieved. Instead of a two-dimensional computer screen, a cost-effective head mounted display will provide the world in stereo.
Evaluating the effectiveness of the VSTS as a training tool is an immediate and necessary next step. At present, the process described herein has resulted in an ecologically valid and engaging training program, but the effects on learning, decision making, and risk perception must be evaluated through future efficacy studies. Additionally, we must assess the ability of the VSTS to enhance both the translation of knowledge and skills to clinical practice and the confidence of HHP in their ability to protect themselves at work through future effectiveness studies. Finally, the ability to use the VSTS both individually and in the context of inter-professional simulation trainings must be assessed, particularly given the body of evidence that inter-professional training contributes to improved quality of care, communication, and self-efficacy.
Conclusion
The long-term goal of this project is to improve the health and safety of HHP who work in client homes. The purpose of this paper was to describe the development of a VSTS that motivates and educates HHP to identify potential hazards that often exist in the home environment in which they work and prepare them to appropriately respond. This system is designed to be easily and widely disseminated and used by multiple professional disciplines involved in home healthcare and has the potential to substantially impact the design and delivery of health and safety training for these at-risk workers.
Key Points.
Home healthcare professionals (HHPs) often are faced with limited opportunities for health and safety training to address the hazards they encounter in client homes.
The virtual simulation training system (VSTS) provides an engaging environment for training HHP in the recognition, identification, and response to health and safety hazards in client homes.
The VSTS stimulates critical thinking and decision making regarding the risk assessments HHP must make when facing often unpredictable and varied health and safety hazards in client homes.
Highlights.
Participatory design processes were applied to the design of a virtual simulation training system to create a naturalistic, engaging, and informative training environment for home healthcare professionals (HHP).
The virtual simulations developed through this process offer opportunities to provide health and safety training that uses an active learning process that incorporates immediate feedback on task performance and decision making.
The Virtual Simulation Training System supports critical thinking, decision making, and risk analysis for HHP.
Acknowledgments
Role of the funding source: This research was supported in part by the National Institute for Occupational Safety and Health (NIOSH) of the Centers for Disease Control and Prevention under award number R01OH010425. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the NIOSH. The funder had no role in the research activities.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Amy R. Darragh, Email: darragh.6@osu.edu.
Steve Lavender, Email: lavender.1@osu.edu.
Barbara Polivka, Email: barbara.polivka@louisville.edu.
Carolyn M. Sommerich, Email: Sommerich.1@osu.edu.
Celia E. Wills, Email: wills.12@osu.edu.
Donald L. Stredney, Email: don@osc.edu.
References
- Centers for Disease Control and Prevention. NIOSH Hazard Review: Occupational Hazards in Home Healthcare. Cincinnati, Ohio: CDC; 2010. [Google Scholar]
- Dreyfus SE. The five-stage model of adult skill acquisition. Bulletin of Science Technology & Society. 2004;24(3):177–181. doi: 10.1177/0270467604264992. [DOI] [Google Scholar]
- Ericsson KA. Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Academic Medicine. 2004;79(S10):70–81. doi: 10.1097/00001888-200410001-00022. [DOI] [PubMed] [Google Scholar]
- Feng JY, Chang YT, Chang HY, Erdley WS, Lin CH, Chang YJ. Systematic review of effectiveness of situated e-learning on medical and nursing education. Worldviews on Evidence-Based Nursing. 2013;10(3):174–183. doi: 10.1111/wvn.12005. [DOI] [PubMed] [Google Scholar]
- Ferrer-García M, Gutiérrez-Maldonado J. The use of virtual reality in the study, Assessment, and treatment of body image in eating disorders and nonclinical samples: A review of the literature. Body Image. 2012;9(1):1–11. doi: 10.1016/j.bodyim.2011.10.00. [DOI] [PubMed] [Google Scholar]
- Foran AC. Learning from experience: shared constructs in virtual reality and occupational therapy. International Journal of Therapy & Rehabilitation. 2011;18(7):362–369. [Google Scholar]
- Gershon RR, Dailey M, Magda LA, Riley HE, Conolly J, Silver A. Safety in the home healthcare sector: Development of a new household safety checklist. Journal of Patient Safety. 2012;8(2):51–59. doi: 10.1097/PTS.0b013e31824a4ad6. [DOI] [PubMed] [Google Scholar]
- IOM (Institute of Medicine) and NRC (National Research Council) The future of home healthcare: Workshop summary. The National Academies Press; Washington, DC: 2015. [Google Scholar]
- Issenberg SB, McGaghie WC, Hart IR, Mayer JW, Felner JM, Petrusa ER, Waugh RA, Brown DD, Safford RR, Gessner IH, Gordon DL, Ewy GA. Simulation technology for healthcare professional skills training and assessment. Journal of the American Medical Association. 1999;282(9):861–6. doi: 10.1001/jama.282.9.861. [DOI] [PubMed] [Google Scholar]
- Issenberg SB, McGaghie WC, Petrusa ER, Lee GD, Scalese RJ. Features and uses of high-fidelity medical simulations that lead to effective learning: A BEME systematic review. Medical Teaching. 2005;27(1):10–28. doi: 10.1080/01421590500046924. [DOI] [PubMed] [Google Scholar]
- Keengwe J. Handbook of Research on Educational Technology Integration and Active Learning. Hershey, PA: IGI Global; 2015. pp. 1–435. [DOI] [Google Scholar]
- McGaghie WC, Issenberg SB, Petrusa ER, Scalese RJ. A critical review of simulation-based medical education research: 2003–2009. Medical Education. 2010;44(1):50–63. doi: 10.1111/j.1365-2923.2009.03547.x. [DOI] [PubMed] [Google Scholar]
- National Occupational Research Agenda (NORA) National healthcare and social assistance agenda for occupational safety and health research and practice in the U.S healthcare and social assistance sector. National Institute for Occupational Safety and Health(NIOSH); 2009. [Google Scholar]
- OSHA. https://www.osha.gov/hazfinder/index.html.
- Polivka BJ, Chaudry RV, Crawford J. Home environmental hazard education for undergraduate and pre-licensure nursing students. Journal of Nursing Education. 2012;51(10):577–581. doi: 10.3928/01484834-20120820-07. [DOI] [PubMed] [Google Scholar]
- Polivka BJ, Wills CE, Darragh A, Lavender S, Sommerich C, Stredney D. Environmental health and safety hazards experienced by home healthcare providers: A room by room analysis. Workplace Health & Safety. 2015;63(11):512–522. doi: 10.1177/2165079915595925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stredney D, Carlson W, Swan JE, Blostein B. The Determination of Environmental Accessibility and ADA Compliance through virtual wheelchair simulation. Presence: Teleoperators and Virtual Environments. 1995;4(3):297–305. [Google Scholar]
- Thompson D, Baranowski T, Buday R, Baranowski J, Juliano M, Frazior M, Jago R. In pursuit of change: Youth response to intensive goal setting embedded in a serious video game. Journal of Diabetes Science and Technology (Online) 2007;1(6):907–917. doi: 10.1177/193229680700100617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tofil NM, Morris JL, Peterson DT, Watts P, Epps C, Harrington KF, Leon K, Pierce C, White ML. Interprofessional simulation training improves knowledge and teamwork in nursing and medical students during internal medicine clerkship. Journal Hospital Medicine. 2014;9(3):189–92. doi: 10.1002/jhm.212610.1002/jhm.2126. [DOI] [PubMed] [Google Scholar]
- Unsworth J, Tuffnell C, Platt A. Safer care at home: Use of simulation training to improve standards. British Journal of Community Nursing. 2011;16(7):334–339. doi: 10.12968/bjcn.2011.16.7.334. [DOI] [PubMed] [Google Scholar]
- Wills CE, Polivka BJ, Darragh AR, Lavender S, Sommerich CM, Stredney D. “Making Do” decisions: How home healthcare personnel manage their exposure to home hazards. Western Journal of Nursing Research. 2015:1–16. doi: 10.1177/0193945915618950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zyda M. From visual simulation to virtual reality to games. Computer. 2005;38(9):25–32. [Google Scholar]


