Abstract
We examined longitudinal relations between interpartner constructive (negotiation) and destructive (psychological and physical aggression) conflict strategies and couples’ sleep over 1 year. Toward explicating processes of effects, we assessed the intervening role of internalizing symptoms in associations between conflict tactics and couples’ sleep. Participants were 135 cohabiting couples (M age = 37 years for women and 39 years for men). The sample included a large representation of couples exposed to economic adversity. Further, 68% were European American and the remainder were primarily African American. At Time 1 (T1), couples reported on their conflict and their mental health (depression, anxiety). At T1 and Time 2, sleep was examined objectively with actigraphs for 7 nights. Three sleep parameters were derived: efficiency, minutes, and latency. Actor–partner interdependence models indicated that husbands’ use of constructive conflict forecasted increases in their own sleep efficiency as well as their own and their wives’ sleep duration over time. Actor and partner effects emerged, and husbands’ and wives’ use of destructive conflict strategies generally predicted worsening of some sleep parameters over time. Several mediation and intervening effects were observed for destructive conflict strategies. Some of these relations reveal that destructive conflict is associated with internalizing symptoms, which in turn are associated with some sleep parameters longitudinally. These findings build on a small, albeit growing, literature linking sleep with marital functioning, and illustrate that consideration of relationship processes including constructive conflict holds promise for gaining a better understanding of factors that influence the sleep of men and women.
Keywords: sleep, couples, conflict, aggression, actigraphy
Interpartner conflict can have negative consequences for families, heightening spouses’ and children’s vulnerability to mental and physical health problems (Cummings & Davies, 2010; Kiecolt-Glaser & Newton, 2001). Recent evidence indicates that the effects of destructive forms of interpartner conflict, particularly physical (assault on a partner’s body) and psychological (verbal threats, insults, name calling) aggression affect the individual’s sleep and that of other family members. Adults and children exposed to destructive interpartner conflict experience poorer sleep quality and reduced sleep duration both in the short term and over the span of several years (Kelly & El-Sheikh, 2013; Rauer, Kelly, Buckhalt, & El-Sheikh, 2010; Rhoades et al., 2012); pertinent studies from our lab are based on independent samples from the one utilized in the present investigation unless otherwise stated. Further, the sleep of individuals can impact their partners’ sleep (Rauer & El-Sheikh, 2012). Such relations between conflict and sleep are not surprising because sufficient high-quality sleep is achieved more easily for those with a sense of security and safety (Dahl & El-Sheikh, 2007; Troxel, Robles, Hall, & Buysse, 2007), which may be compromised in relationships characterized by destructive conflict.
Destructive conflict captures one facet of couples’ conflict experiences, with aggressive marital conflict—both physical and psychological—representing the overtly hostile behaviors within that domain (Erath, Bierman, & the Conduct Problems Prevention Research Group, 2006; Goeke-Morey, Cummings, Harold, & Shelton, 2003; Straus, Hamby, Boney-McCoy, & Sugarman, 1996). Despite the widespread prevalence of these forms of destructive conflict in community samples (Lawrence, Yoon, Langer, & Ro, 2009; Murphy & Cascardi, 1999; Straus et al., 1996; Vickerman & Margolin, 2008), these behaviors only represent a subset of the everyday conflict tactics couples are likely to employ (Goeke-Morey et al., 2003). Many couples are able to utilize more constructive approaches focused on resolving issues to couples’ mutual satisfaction, such as negotiation tactics (e.g., compromising, reaching a solution together, showing respect during conflict), which can promote well-being for all members of the family (Cummings, Goeke-Morey, & Papp, 2003; Gottman, 1993). However, the effects of constructive conflict strategies on sleep remain unknown because the literature to date on conflict and sleep has focused either exclusively on destructive conflict (physical or psychological; Humphreys & Lee, 2005; Rauer & El-Sheikh, 2012) or on single-item, general reports of conflict (e.g., interpartner interactions involved quarreling; Hicks & Diamond, 2011). Expanding on this scant but growing literature, we utilized a multidimensional approach to examine links between both destructive and constructive forms of conflict and couples’ objectively assessed sleep over time. We also evaluated whether spouses’ mental health acted as an intervening variable linking conflict with sleep. Identifying how constructive and destructive conflict serve to enhance or detract from the duration and quality of sleep is imperative in light of the widespread consequences of poor sleep for health and mortality (Colten, Altevogt, & Institute of Medicine Committee on Sleep Medicine and Research, 2006; Gallicchio & Kalesan, 2009).
Interpartner Conflict and Sleep
One of the most robust findings in the marriage and health literature is that the effects of marriage on well-being are moderated by the quality of the relationship between spouses (Gove, Hughes & Style, 1983; Ren, 1997), with some finding that individuals in distressed marriages are more at risk for poor health than those who are single (Holt-Lunstad, Birmingham, & Jones, 2008). This pattern of effects is consistent with the emerging literature on links between interpartner relations and sleep. In pioneering work, Dahl (1996) proposed that the sense of emotional security necessary to achieve high-quality sleep largely originates within the social environment. Troxel and colleagues (2007) suggested that the romantic relationship affects the individual’s sleep, as couples not only share their beds at night but also share their lives during the day. How they spend this time together is of great consequence for their sleep, as spouses in marriages characterized by low levels of conflict coupled with high satisfaction are thought to have the sense of security and belonging that is conducive to sleep. An underlying assumption in much of the literature is that interpartner conflict is inherently damaging, which is why less conflict is conceptualized as a predictor of better sleep. Frequency and intensity of conflict, however, may not capture the quality of the marriage, as conflict can be beneficial if it enables couples to address and solve their problems through more calm, solution-focused discussions (Cummings et al., 2003). Further, couples who avoid conflict may be at a greater risk for both relationship and health problems than couples who engage in the conflict (Robles & Kiecolt-Glaser, 2003), even if said engagement is not uniformly positive (e.g., criticism; Gottman & Krokoff, 1989).
Instead, it is the hostile and aggressive nature of the conflict that appears to be the key predictor of poor sleep quality and shorter sleep duration. Partners’ exposure to psychological and physical marital aggression is associated with sleep problems (Humphreys & Lee, 2005; Rauer & El-Sheikh, 2012; Woods, Kozachik, & Hall, 2010). Pigeon et al. (2011) found that nearly half of their sample of women exposed to intimate partner violence reported clinically significant insomnia. Looking at the effects of destructive conflict over time, Rauer and colleagues (2010) found spouses who experienced more psychological aggression reported increases in their sleep problems over 2 years. The effects of this type of destructive conflict on sleep are of significance, given the high prevalence of psychological aggression in community samples and in couples seeking relationship therapy (Straus et al., 1996; Vickerman & Margolin, 2008). Even when considered in the presence of physical violence, the effects of psychological aggression are linked to psychological distress in community samples (Lawrence et al., 2009).
Marriages characterized by positivity and happiness can be equally impactful, albeit to the individuals’ and spouses’ benefit. At the global level, happily married women reported fewer sleep problems than did unhappily married women (Troxel, Buysse, Hall, & Matthews, 2009), a finding that was stable over a 4-year period for older adults (Yang et al., 2013). Similarly, women’s reports of having a positive interaction with their partner during the day were linked to their own and their partners’ sleep efficiency that night, underscoring the interdependence of partners’ sleep quality (Hasler & Troxel, 2010). The challenge to reconciling these findings on the effects of marriage on sleep is that they imply a false dichotomy, whereby couples who have positive interactions are happier and have better sleep as a result, whereas couples who engage in destructive conflict are unhappy and unlikely to sleep well. Spouses, however, often engage in positive and negative conflict behaviors simultaneously when trying to solve a problem (Gottman, 1993; Rauer & Volling, 2013). For example, Cummings et al. (2003) found that wives reported that 70% of the marital conflicts that occurred over the past 2 weeks included at least one negative expression (i.e., destructive tactic) and one positive expression (i.e., constructive tactic). Thus, examining conflict processes from a multifaceted angle—one that acknowledges that couples often utilize multiple types of behaviors and that each approach to conflict has the potential to uniquely impact how spouses function at night—represents a key next step in this burgeoning literature.
How Is Interpartner Conflict Linked to Sleep? Mental Health as a Mechanism
Beyond using longitudinal assessments to examine the long-term effects of engaging in diverse conflict strategies on both spouses’ sleep, it is imperative to explicate mechanisms underlying these pathways. In this study, we examined spouses’ mental health as an intervening variable in the link between interpartner conflict and sleep over 1 year. Destructive interpartner conflict, most notably when in the form of psychological and physical aggression, has been consistently linked to psychological distress (Taft et al., 2006), which is not surprising, as interpartner aggression can foster anxiety and negative self-evaluations in the recipient (Murphy & Cascardi, 1999). Further, those who perpetrate interpartner aggression are not immune from its negative effects on their mental health, especially if the partners are both engaged in these types of destructive conflict behaviors (Johnson, Giordano, Longmore, & Manning, 2014). Distress disrupts how easily individuals can engage in the downregulation required to achieve adequate sleep (Dahl & Lewin, 2002), and individuals who experience more symptoms of depression and anxiety often struggle with sleep problems (Mezick et al., 2009; Taylor, Lichstein, Durrence, Reidel, & Bush, 2005).
Of the few studies that have empirically examined mental health as a pathway linking interpartner conflict with sleep, the focus has been exclusively on destructive conflict. This work reveals that individuals who experience more psychological and physical aggression report more anxiety and depression symptoms, and that these symptoms in turn predict poorer sleep cross-sectionally (El-Sheikh, Kelly, & Rauer, 2013, which was conducted with the first wave of the present study and exclusively examined destructive conflict; Pigeon et al., 2011) and longitudinally (Rauer et al., 2010). However, these findings were not entirely consistent across partners or indices of mental health. Using objective assessments of sleep (e.g., actigraphy) and a cross-sectional design, wives’ anxiety symptoms served as an intervening variable in the link between their husbands’ perpetration of psychological aggression and their own sleep efficiency and duration (El-Sheikh et al., 2013; based on the first study wave). For husbands, it was their symptoms of depression that operated as the process variable connecting their receipt of psychological aggression to lower levels of both sleep duration and quality. Further, engaging in constructive conflict including positive and rational approaches to problem solving may reduce symptoms of depression and anxiety (Kant, D’Zurilla, & Maydeu-Olivares, 1997). Assessment of constructive and destructive forms of conflict are likely to explicate conflict strategies associated with mental health and how that impacts the quality and duration of the individuals’ and spouses’ sleep.
The Current Study
Although destructive forms of conflict contribute to subjective sleep problems years later (Rauer & El-Sheikh, 2012), we know of no study that has examined this association longitudinally with objective sleep parameters. Similarly, we are not aware of studies that have examined the effects of constructive conflict on couples’ sleep. Building on the young literature of marriage and sleep, the primary goal of the current study is to examine how individuals’ conflict engagement is linked to their own and their spouses’ objective sleep duration and quality over 1 year. We use the term sleep problems to refer to shorter sleep duration and poorer sleep quality (efficiency, latency) on a continuum. Because of the interdependent nature of spouses’ functioning, we examined spouses simultaneously using the actor–partner interdependence model (APIM; Kashy & Kenny, 2000). We estimated the autoregressive effects of sleep and allowed the interpartner conflict predictors to covary to decipher the unique contributions of each conflict strategy (psychological aggression, physical aggression, negotiation) to changes in sleep over time. We expected that more engagement in destructive conflict by both the individual and his or her partner would predict declines in both sleep efficiency and duration 1 year later. Conversely, more engagement in constructive conflict by the individual and the partner was expected to predict better sleep over time.
We also examined spouses’ symptoms of anxiety and depression as mediators connecting interpartner conflict and change in sleep. Because symptoms of depression and anxiety often co-occur, we examined both simultaneously to decipher unique effects. We predicted that the effects of conflict on later sleep quality and duration will be explained in part by both partners’ mental health (actor and partner effects). We expected that destructive conflict would be associated with higher levels of anxiety and depression and that constructive conflict would be related to better mental health. Examining the long-term, interdependent effects of spouses’ use of both destructive and constructive conflict strategies on their objectively assessed sleep represents not only a novel contribution to the burgeoning literature on couples’ sleep but also one that better captures the complex nature of conflict as it is likely to be experienced by couples (Cummings et al., 2003).
Method
Participants
Participants were families with at least one school-age child enlisted in a larger longitudinal study examining biopsychosocial influences on health (Auburn University Sleep Study). The current investigation is based on two study waves spanning 2 years that occurred between 2010 and 2012 (second and third waves of the larger longitudinal investigation). To recruit families, letters inviting participation were distributed to children at public schools in the Southeastern United States. Families who were interested in study participation were asked to call our on-campus research laboratory. Given the study’s focus, only cohabiting couples and those in which both the husband and wife participated were included in analyses. In addition, to reduce confounds, night-shift workers were excluded. This resulted in a sample of 135 cohabiting couples (90% married); the average length of cohabitation was 11.54 years (SD = 6.06 months). For simplicity, we refer to couples as wives and husbands. Mean age of husbands was 39 years (SD = 7.33), and mean age of wives was 37 years (SD = 5.93). In relation to ethnicity, 76% of wives and 78% of husbands were European American, and 21% of wives and 18% of husbands were African American; the rest reported other ethnicities. Family income-to-needs ratio (annual family income divided by the poverty threshold considering the family size; U.S. Department of Commerce, n.d.) indicated that approximately 18% of families lived below the poverty line (ratio <1), 21% lived near the poverty line (ratio between 1 and 2), 28% were classified as lower middle class (ratio between 2 and 3), and 33% were middle class (ratio ≥3).
Of the 135 cohabiting couples who participated at Time 1 (T1; corresponds to Time 2 [T2] of the larger study), 127 participated at T2 (Time 3 [T3] of the larger study). The average time lag between T1 and T2 was 338 days (SD = 34 days). The present T1 sample is the same as that reported in El-Sheikh et al. (2013). There were no differences in study variables between couples lost to attrition and retained couples.
Procedures
The study was approved by the university’s institutional review board. At both waves, actigraphs were delivered to families’ homes, and participants were asked to wear them on their non-dominant wrist for 7 consecutive nights. To corroborate actigraphy data, couples completed sleep diary logs nightly (Acebo & Carskadon, 2001). After the actigraphy assessment (typically the following day), couples visited the research laboratory to complete questionnaires. Individuals received monetary compensation for their time.
Measures
Interpartner conflict tactics
At T1, wives and husbands reported on the frequency of psychological aggression, physical aggression, and negotiation tactics used by their partner toward them using the Revised Conflict Tactics Scale (CTS2; Straus, 1995). The CTS2 is frequently used for the assessment of inter-partner conflict tactics and has good psychometric properties (Straus et al., 1996). Destructive conflict was assessed using the Psychological Aggression (eight items; e.g., “My partner insulted or swore at me”) and Physical Aggression (12 items; e.g., “My partner slapped me”) subscales. Constructive conflict was measured using the Negotiation subscale (six items; e.g., “My partner suggested a compromise to a disagreement,” “My partner showed respect for my feelings about an issue,” “My partner said he or she was sure that we could work out a problem”). For each item, individuals reported how often their partner used the specified type of conflict tactic within the past year on a scale with anchors ranging from 0 (this has never happened) to 6 (more than 20 times). For each subscale, items were summed and higher scores reflect greater occurrence of the specified type of conflict tactic; alpha ranged between .77 and .94. Analyses revealed that on average, 79% of wives and husbands reported experiencing psychological aggression tactics directed toward them in the past year. In addition, 8% of wives and 12% of husbands reported that they experienced physical aggression tactics against them. Lastly, 98% of wives and husbands reported that their partner had used negotiation tactics during conflict.
Anxiety symptoms
At T1, wives and husbands reported on their own anxiety symptoms using the 21-item Beck Anxiety Inventory (BAI; Beck & Steer, 1993), which has good psychometric properties. Participants reported on the extent to which they experienced common symptoms of anxiety over the past month using a 4-point Likert scale (not at all to severely). Researchers have demonstrated that the BAI reliably discriminates symptoms of anxiety from depression in adults (Hewitt & Norton, 1993). For this study, alpha was .85 for both partners.
Analyses indicated that 15% of women and 7% of men reported symptoms in the mild-to-moderate clinical range (scores ranging from 10 to 18), and 4% of women and no men reported symptoms in the moderate-to-severe range (scores ranging from 19 to 29).
Depression symptoms
At T1, wives and husbands reported on their depression symptoms using the 20-item Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977). Symptoms of depression were measured over the past week on anchors ranging from 0 (rarely) to 3 (most or all of the time). The CES-D is widely used and has excellent psychometric properties, including established reliability and convergent validity with clinical and self-report measures of depression across diverse ethnic and socioeconomic backgrounds (Radloff, 1977). In this sample, alpha was .89 for wives and .84 for husbands. Analyses indicated that 18% of wives and 4% of husbands surpassed the clinical cutoff (score >16).
Sleep
At T1 and T2, actigraphy was used to derive sleep parameters. Actigraphy is considered a reliable tool for objectively measuring sleep in the home environment (Rupp & Balkin, 2011). The actigraphs measured motion in 1-min epochs using zero crossing mode. The Octagonal Motionlogger Interface with Actme software and Action W2 analysis software package (Ambulatory Monitoring, Ardsley, NY) were used. Wives and husbands were considered awake or asleep using the established Cole-Kripke scoring algorithm (Cole, Kripke, Gruen, Mullaney, & Gillin, 1992).
Sleep quality, duration, and latency were assessed. To examine sleep quality, we derived sleep efficiency, the percentage of epochs scored as sleep between actigraphy-based sleep onset and wake time. To assess sleep duration, we derived sleep minutes, the number of minutes scored as sleep between sleep onset and wake time. Sleep latency was the duration between bedtime and sleep onset time.
At T1, across the week of actigraphy, husbands and wives had an average of 5.84 nights (SD = 1.63) and 5.44 nights (SD = 1.91) of valid actigraphy data, respectively. At T2, husbands and wives had an average of 5.74 nights (SD = 1.63 nights) and 5.36 nights (SD = 1.98), respectively. Reasons for missing data included forgetting to wear the actigraph and mechanical problems. At least 5 nights of actigraphy are recommended to achieve sufficient reliability and validity (Sadeh, 2011), and thus data points for those with fewer than 5 nights were excluded from analyses. For wives and husbands, intraclass correlations indicated good night-to-night stability over the week of assessment at both T1 and T2 for sleep efficiency (αs = .94 to .98), sleep minutes (αs = .73 to .86), and sleep latency (αs = .54 to .69). Lower coefficients for sleep latency are consistent with those reported in past studies (e.g., Knutson, Rathouz, Yan, Liu, & Lauderdale, 2007). Each of the sleep variables was derived by creating an average from all available nights.
Results
Descriptive Statistics
Means, standard deviations, and correlations among study variables are displayed in Table 1. Independent t tests were conducted to examine differences between men and women on primary study variables. Compared with men, women had greater anxiety, t(104) = 5.46, p <.001, and depression symptoms, t(104) = 2.43, p = .017. No other differences among primary study variables were detected. At T1, wives averaged 6.60 hr of sleep per night and husbands averaged 6.43 hr per night. Similar sleep durations were found at T2 (see Table 1). Illustrating similarities in wives’ and husbands’ sleep, with the exception of sleep latency at T1, women’s and men’s concurrent sleep duration and quality were associated at both T1 and T2.
Table 1.
Means, Standard Deviations, and Correlations Among Primary Study Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Psychological aggression against women T1 | 1.00 | |||||||||||||||||||||
| 2. Psychological aggression against men T1 | .67*** | 1.00 | ||||||||||||||||||||
| 3. Physical aggression against women T1 | .36*** | .27** | 1.00 | |||||||||||||||||||
| 4. Physical aggression against men T1 | .27** | .26** | .46*** | 1.00 | ||||||||||||||||||
| 5. Negotiation tactics toward women T1 | .09 | −.01 | .05 | −.08 | 1.00 | |||||||||||||||||
| 6. Negotiation tactics toward men T1 | .06 | .19* | −.07 | −.21* | .39*** | 1.00 | ||||||||||||||||
| 7. Women’s anxiety symptoms T1 | .32*** | .27** | .06 | .08 | .04 | .01 | 1.00 | |||||||||||||||
| 8. Men’s anxiety symptoms T1 | .32*** | .37*** | .19 | .06 | −.01 | .02 | .45*** | 1.00 | ||||||||||||||
| 9. Women’s depression symptoms T1 | .27** | .29** | .08 | .34*** | −.07 | .01 | .48*** | .20* | 1.00 | |||||||||||||
| 10. Men’s depression symptoms T1 | .25* | .30** | .20* | .14 | −.16 | −.07 | .15 | .36*** | −.18 | 1.00 | ||||||||||||
| 11. Women’s sleep efficiency T1 | .08 | .12 | .13 | .03 | .12 | .23* | −.28** | −.08 | −.14 | −.05 | 1.00 | |||||||||||
| 12. Men’s sleep efficiency T1 | −.06 | −.08 | .02 | −.06 | .23* | .12 | −.11 | −.05 | −.10 | −.18 | .44*** | 1.00 | ||||||||||
| 13. Women’s sleep minutes T1 | −.04 | .08 | .02 | .02 | −.01 | .14 | −.07 | .02 | −.08 | .06 | .54*** | .20 | 1.00 | |||||||||
| 14. Men’s sleep minutes T1 | .01 | −.03 | −.01 | .02 | .24* | .15 | −.08 | .09 | −.05 | −.19 | .27** | .67*** | .26** | 1.00 | ||||||||
| 15. Women’s sleep latency T1 | .05 | −.02 | .00 | .04 | .02 | .07 | .19* | .22* | .07 | .11 | −.36*** | −.25* | −.17 | −.18 | 1.00 | |||||||
| 16. Men’s sleep latency T1 | .14 | .15 | .02 | .02 | −.11 | −.17 | .15 | .07 | .02 | .35*** | −.18 | −.38*** | −.10 | −.32** | .08 | 1.00 | ||||||
| 17. Women’s sleep efficiency T2 | .14 | .14 | .03 | .09 | .19 | .25* | −.18 | −.13 | −.07 | −.01 | .81*** | .46*** | .47*** | .32** | −.19 | −.21 | 1.00 | |||||
| 18. Men’s sleep efficiency T2 | .14 | .02 | −.06 | .02 | .31** | .15 | .04 | −.01 | .13 | −.16 | .28* | .46*** | .03 | .30* | −.08 | −.30* | .27* | 1.00 | ||||
| 19. Women’s sleep minutes T2 | .10 | .05 | .12 | .14 | .23* | .18 | −.15 | −.17 | −.08 | −.01 | .60*** | .24* | .70*** | .27* | −.15 | −.16 | .66*** | .20 | 1.00 | |||
| 20. Men’s sleep minutes T2 | .20 | .08 | .13 | .07 | .35** | .23 | .25* | .19 | .19 | −.06 | .31* | .20 | .35** | .48*** | −.13 | −.16 | .18 | .55*** | .37** | 1.00 | ||
| 21. Women’s sleep latency T2 | .18 | .18 | .14 | .00 | −.12 | −.14 | .20 | .22* | .15 | .17 | −.38*** | −.47*** | −.21 | −.43*** | .26* | .26* | −.62*** | −.24 | −.39*** | −.20 | 1.00 | |
| 22. Men’s sleep latency T2 | .03 | .14 | .26* | .18 | −.17 | −.20 | .06 | .16 | −.06 | .37** | −.33** | −.35** | −.19 | −.30* | .12 | .34** | −.40*** | .57*** | −.27* | −.37*** | .60*** | 1.00 |
| M | 6.50 | 6.63 | .32 | .62 | 19.92 | 19.77 | 6.00 | 3.09 | 9.58 | 7.37 | 93.49 | 91.54 | 396 min | 384 min | 11.68 | 11.13 | 93.54 | 92.46 | 396 min | 388 min | 12.13 | 9.87 |
| SD | 7.18 | 6.79 | 1.58 | 2.51 | 8.55 | 8.49 | 5.96 | 3.86 | 8.05 | 5.53 | 6.34 | 9.09 | 61.60 | 64.81 | 8.70 | 9.59 | 7.08 | 7.74 | 69.61 | 59.78 | 10.58 | 8.73 |
Note. T1 = Time 1; T2 = Time 2.
p < .05.
p < .01.
p < .001.
Direct Effects Between Interpartner Conflict Tactics and Change in Sleep
An APIM model (Kenny, Kashy, & Cook, 2006) was fit to examine the impact of self and partner conflict tactics at T1 (psychological aggression, physical aggression, negotiation) on their own and their partner’s sleep 1 year later at T2 (efficiency, minutes, latency). In the present analyses, the actor effects capture the associations between being the recipient of interpartner conflict and sleep, and the partner effects capture the links between being the perpetrator of interpartner conflict and sleep.
Manifest variables of husbands’ and wives’ psychological and physical aggression and negotiation at T1 were included simultaneously in the same models as predictors of husbands’ and wives’ sleep at T2. Similarly, all three sleep variables were examined simultaneously in the same model. Overall, one model was fit to examine direct relations between interpartner conflict and sleep, and a second model was fit to examine mediation and intervening effects. Sleep at T1 was controlled in order to assess change over time across the 1-year lag (within and across partners). In addition, variables associated with interpartner conflict and sleep in the literature were considered as control variables, including T1 socioeconomic status (SES), ethnicity, marital status, duration of cohabitation, age, sleep medication use (35% of wives and 21% of husbands reported taking medication for sleep during the last month), and other medication use. Only significant covariates were retained, which included SES, ethnicity, husbands’ age, and sleep medication use for husbands and wives. All exogenous variables (i.e., covariates, T1 conflict tactics, T1 sleep) were allowed to correlate. Further, residual variances among the sleep variables at T2 were allowed to correlate within and across partners. To reduce outlier effects, values ≥4 standard deviations among the T1 conflict tactics variables and T1 and T2 sleep were set to missing (Cousineau & Chartier, 2010; total n = 9 values). In addition, on the basis of skewness (+2) and kurtosis (+2) statistics and visual inspection, the physical aggression and the sleep latency variables were skewed and log transformed. Analyses were conducted using Amos 22, which utilizes maximum likelihood estimation for handling missing data (Acock, 2005).
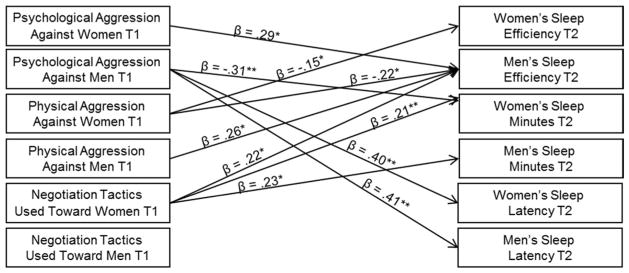
An APIM model was fit to examine relations between interpartner conflict tactics at T1 and couples sleep at T2 (see Figure 1). The model fit was acceptable: χ2(24) = 46.94, p = .02, χ2/df = 1.96, comparative fix index (CFI) = .97, root mean square error of approximation (RMSEA) = .08; wives’ sleep efficiency R2 = .68, husbands’ sleep efficiency R2 = .45, wives’ sleep minutes R2 = .62, husbands’ sleep minutes R2 = .57, wives’ sleep latency R2 = .42, and husbands’ sleep latency R2 = .38. For wives and husbands, respectively, autoregressive effects for sleep were significant from T1 to T2 for sleep efficiency (βs = .64 and .45, ps < .001), sleep minutes (βs = .67 and .38, ps < .001), and sleep latency (βs = .28 and .27, ps < .002; not shown in Figure for clarity). Supportive of partner effects, wives’ sleep minutes at T1 were related to husbands’ sleep minutes at T2 (β = .23, p < .001), and wives’ sleep latency at T1 was related to husband’s sleep latency at T2 (β = .26, p .005).
Figure 1.
Pathways between couples’ Time 1 (T1) interpartner conflict tactics and Time 2 (T2) sleep. Only significant standardized estimates are provided to enhance the clarity of the figure. Correlations among exogenous variables are not depicted. Residual variances among sleep variables at T2 were allowed to correlate within and across partners (not depicted in figure). For autoregressive effects, sleep efficiency, minutes, and latency were controlled at T1 (not depicted in figure). Covariates were T1 socioeconomic status, ethnicity, husbands’ age, and wives’ and husbands’ sleep medication use (not depicted in figure). Model fit: χ2(24) = 46.94, p = .02, χ2/df = 1.96, CFI = .97, RMSEA = .08. * p < .05. ** p < .01. *** p < .001.
Husbands who perpetrated greater psychological aggression at T1 (indicated by psychological aggression against women in Figure 1) had increased sleep efficiency at T2 (β = .29, p =.027; Figure 1). In addition, wives who perpetrated more psychological aggression at T1 (indicated by psychological aggression against men in Figure 1) had fewer sleep minutes (β = −.31, p = .002) and a longer sleep latency at T2 (β = .40, p < .001). Men exposed to higher levels of psychological aggression at T1 had a longer sleep latency at T2 (β = .41, p = .003).
Women who were exposed to higher levels of physical aggression tactics at T1 had reduced sleep efficiency at T2 (β = −.15, p = .047). Further, husbands who perpetrated more physical aggression at T1 (indicated by physical aggression against women in Figure 1) had decreased sleep efficiency at T2 (β = −.22, p = .036). In addition, men who experienced higher levels of physical aggression at T1 had increased sleep efficiency at T2 (β = .26, p = .019).
Greater negotiation tactics used toward women at T1 forecasted an increase in their sleep minutes at T2 (β = .21, p = .008). Lastly, husbands who used greater negotiation tactics toward their wives at T1 (indicated by negotiation tactics used toward women in Figure 1) had increased sleep efficiency (β = .22, p = .03) and sleep minutes at T2 (β = .23, p = .012).
Anxiety and Depression Symptoms as Mechanisms of Effects
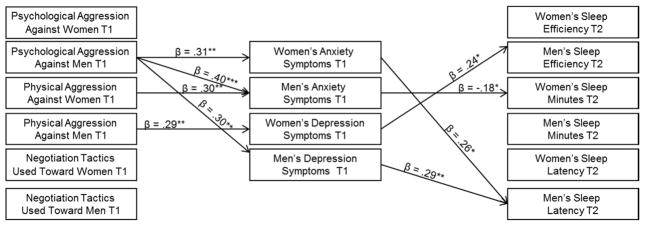
Next, wives’ and husbands’ anxiety and depression symptoms at T1 were added to the model to examine their roles as process variables (see Figure 2). To identify “unique” effects, symptoms of depression and anxiety were examined simultaneously. In preliminary analyses, models were fit while examining symptoms of depression and anxiety separately; results are similar to those reported hereafter. Consistent with Figure 1, autoregressive effects for sleep were controlled from T1 to T2.
Figure 2.
Examination of anxiety and depression symptoms at Time 1 (T1) as mechanisms of relations between couples’ T1 interpartner conflict tactics and Time 2 (T2) sleep. Only significant standardized estimates pertaining to the indirect effects are provided to enhance the clarity of the figure. Correlations among exogenous variables are not depicted. Residual variances among anxiety and depression symptoms were allowed to correlate within persons. Residual variances among the sleep variables at T2 were allowed to correlate within and across partners. Significant direct effects between interpartner conflict at T1 and sleep at T2 are not depicted for clarity. For autoregressive effects, sleep efficiency, minutes, and latency were controlled at T1. Covariates were T1 socioeconomic status, ethnicity, husbands’ age, and wives’ and husbands’ sleep medication use. Model fit: χ2(52) = 107.02, p < .001, χ2/df = 2.06, CFI = .94, RMSEA = .09. * p < .05. ** p < .01. *** p < .001.
Symptoms of anxiety and depression at T1 were examined as both mediators and intervening variables. In both a mediation model and intervening variable model, the independent variable (i.e., interpartner conflict at T1) is significantly related to the mediator or intervening variable (i.e., anxiety and depression symptoms at T1), which in turn is significantly related to the outcome variable (i.e., sleep at T2; MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002). In a mediation model, the relation between the independent and dependent variable is significant prior to the inclusion of the mediating variable (Baron & Kenny, 1986), whereas in an intervening model, no such association is required.
Tests of indirect effects were examined using Monte Carlo simulation (Preacher & Selig, 2012). This method produces confidence intervals of the hypothesized indirect effect by generating a large number of estimates (20,000 for these analyses) of an indirect effect by resampling from the distributions of the direct effect. Selig and Preacher’s (2008) interactive tool was used for creating confidence intervals to test indirect effects, with an indirect effect being demonstrated when the confidence interval does not contain zero.
Lastly, the error variances among anxiety and depression symptoms at T1 were allowed to correlate within person. Values ≥4 standard deviations among the T1 depression and anxiety variables were set to missing (n = 4 values).
Dyadic path model
An APIM model was fit to examine anxiety and depression symptoms at T1 as mechanisms of relations between interpartner conflict tactics at T1 and couples sleep at T2 (see Figure 2). The model yielded acceptable fit: χ2(52) = 107.02, p < .001, χ2/df = 2.06, CFI = .94, RMSEA = .09. Wives’ anxiety symptoms R2 = .30; husbands’ anxiety symptoms R2 = .28; wives’ depression symptoms R2 = .19; husbands’ depression symptoms R2 = .28; wives’ sleep efficiency R2 = .69; husbands’ sleep efficiency R2 = .50; wives’ sleep minutes R2 = .66; husbands’ sleep minutes R2 = .59; wives’ sleep latency R2 > .46; and husbands’ sleep latency R2 = .41.
Regarding direct relations between interpartner conflict at T1 and sleep at T2, more psychological aggression against women forecasted an increase in their sleep minutes (β = .20, p = .034; direct effects are not shown in Figure 2 for clarity). Further, women who perpetrated greater psychological aggression at T1 had fewer sleep minutes at T2 (β = −.21, p = .041) and a longer sleep latency (β = .39, p = .002). Men who used more negotiation tactics at T1 had increased sleep efficiency (β = .27, p = .008) and more sleep minutes at T2 (β = .23, p = .009). More negotiation tactics used toward women predicted an increase in their sleep minutes at T2 (β = .19, p = .013).
Wives who perpetrated more psychological aggression (indicated by psychological aggression against men in Figure 2) had more concurrent symptoms of anxiety (β = .31, p = .007). Further, men who were exposed to higher levels of psychological aggression had higher levels of anxiety (β = .40, p < .001) and depression (β = .30, p = .012). In addition, men who perpetrated more physical aggression (indicated by physical aggression against women in Figure 2) had higher levels of anxiety symptoms (β = .30, p = .003). Finally, wives who perpetrated more physical aggression (indicated by physical aggression against men) had higher levels of depression symptoms (β = .29, p = .005).
Higher levels of anxiety symptoms among women at T1 forecasted a longer sleep latency among men at T2 (β = .26, p = .029). Further, greater symptoms of anxiety among men at T1 predicted a decrease in women’s sleep minutes at T2 (β = −.18, p = .026). In addition, more symptoms of depression among women at T1 predicted increased sleep efficiency among men at T2 (β = .24, p = .020). Lastly, more depression symptoms among men at T1 predicted an increase in their sleep latency at T2 (β = .29, p = .009).
Test of indirect effects
A total of five possible indirect effects emerged. Wives’ perpetration of psychological aggression (indicated by psychological aggression against men in Figure 2) was related to their own anxiety symptoms at T1, which in turn was associated with increases in their husbands’ sleep latency at T2. Consequently, the mediating role of anxiety symptoms at T1 was assessed in this relation. While examining one potential mediator, we constrained the pathway between the other potential mediators and the sleep outcome variable of interest. The level of significance of the direct effect of women’s perpetration of psychological aggression at T1 on men’s sleep latency at T2 became nonsignificant (β changed from .41 to .18; p value changed from .003 to .145) with the inclusion of anxiety as a mediator, thus suggesting a mediating effect. The indirect effect was significant (95% CI [.006, .24]).
Psychological aggression against men at T1 was related to their anxiety symptoms at T1, which in turn was associated with reduced sleep minutes for women at T2. Examination of mediation effects indicated that the level of significance between psychological aggression against men and women’s sleep minutes was reduced (β changed from −.31 to −.21; p value changed from .002 to .041) after the inclusion of anxiety in the model, thus suggesting a partial mediation effect. The indirect effect was significant (95% CI [−1.52, −.06]).
Psychological aggression against men at T1 was concurrently related to higher levels of husbands’ depression symptoms at T1, which in turn was associated with increases in their sleep latency at T2. After the inclusion of depression symptoms in the model, the level of significance between psychological aggression against men at T1 and their sleep latency at T2 became nonsignificant (β changed from .41 to .19; p value changed from .003 to .165), and the indirect effect was significant (95% CI [.01, .25]). Thus, depression symptoms functioned as a mediator of effects in these relations.
Husbands’ perpetration of physical aggression at T1 (indicated by physical aggression against women in Figure 2) was related concurrently to higher levels of men’s anxiety symptoms, which in turn was related to decreases in women’s sleep minutes at T2. Because husbands’ perpetration of physical aggression at T1 was not directly related to wives’ sleep minutes at T2, husbands’ anxiety symptoms served as an intervening process in these relations, and the indirect effect was significant (95% CI [−44.37, −1.32]).
Lastly, wives’ perpetration of physical aggression at T1 (indicated by physical aggression against men in Figure 2) was related to their own depression symptoms at T1, which in turn was associated with increases in husbands’ sleep efficiency at T2. After the inclusion of depression symptoms in the model, and supportive of a mediation effect, the level of significance between wives’ perpetration of physical aggression at T1 and husbands’ sleep efficiency at T2 became nonsignificant (β changed from .26 to .05; p value changed from .019 to .614); the indirect effect was significant (95% CI [.32, .5.82]).
Discussion
A growing literature has illustrated that family functioning, including interpartner conflict, influences sleep. Existing studies have focused on destructive conflict tactics including psychological and physical aggression. We considered the influence of constructive (negotiation) and destructive (psychological and physical aggression) conflict on couples’ sleep. Toward explicating processes of effects, we examined depression and anxiety symptoms as mediators of relations between constructive and destructive interpartner conflict and spouses’ sleep. For a more rigorous assessment of research questions, we utilized a two-wave longitudinal design that spanned 1 year, used actigraphy to objectively measure three important sleep parameters (minutes, efficiency, latency), controlled for prior levels of sleep to measure change over time, and used an APIM to capture actor and partner effects.
Couples use multiple conflict tactics concurrently during disagreements (Cummings et al., 2003; Rauer & Volling, 2013). Consequently, and to better ascertain the unique influence that psychological aggression, physical aggression, and negotiation tactics have on sleep, we examined the three conflict tactics simultaneously in analyses. Results are the first to demonstrate that greater use of negotiation tactics during conflict predicted better sleep over time. Specifically, path models indicated that greater negotiation tactics initiated by husbands during conflict forecasted an increase in their own sleep duration and efficiency, as well as an increase in their wives’ sleep duration, over 1 year. In addition, bivariate correlations showed that constructive conflict strategies were associated with better sleep in women and men at T1. Overall, these findings illustrate that consideration of relationship processes including constructive conflict holds promise for gaining a better understanding of factors that influence the sleep of men and women. Negotiation tactics might provide a sense of comfort and certainty about the intactness of the relationship, reduce arousal that frequently accompany destructive conflict, and reflect a resolution to a dispute, thereby facilitating longer and better quality sleep.
Consistent with hypotheses, both actor and partner effects were found for direct relations between destructive marital conflict and sleep disruptions. Perpetration of psychological aggression against husbands was associated with reductions in wives’ sleep duration, and increases in the sleep latency for both husbands and wives over time. Further, perpetration of physical aggression against wives was related to reduced sleep efficiency for both men and women. Collectively, these findings are consistent with prior studies linking marital aggression with sleep problems. Women exposed to intimate partner violence have reported high levels of insomnia (Pigeon et al., 2011), and spouses who were subject to relatively high levels of psychological aggression reported increases in their sleep problems over time (Rauer et al., 2010). Results build on the existing literature by establishing longitudinal relations between interpartner destructive conflict and objectively measured sleep. Objective and subjective measures of sleep are related, yet distinct, constructs, and there is a recognized need to examine sleep objectively in the context of relationship processes (Hasler & Troxel, 2010; Troxel et al., 2007). Curiously, direct relations between destructive conflict and sleep were not found in the cross-sectional study with the first wave of data utilized in the present investigation (El-Sheikh et al., 2013). Rather, destructive conflict was indirectly related to sleep through shared associations with mental health of the individual or the partner. As this area of inquiry develops, answers to these inconsistencies may emerge.
Partial support for mediation effects was evident for destructive but not constructive conflict; only direct effects were observed for the latter. For both men and women, greater anxiety and depression symptoms mediated (and in one instance functioned as an intervening variable) some relations between destructive conflict and their own sleep and/or the sleep of their partners. The vast majority of the mediation and intervening effects were in the expected direction, and no specific variable emerged as a particularly more robust mediator. These results support a chain reaction such that destructive conflict ultimately undermines sleep through mental health. The perpetration and receipt of relationship aggression can compromise mental health, including elevations in anxiety and depression (Johnson et al., 2014; Murphy & Cascardi, 1999), which can disrupt sleep (Taylor et al., 2005). Further, incorporating a biopsychosocial perspective, those who experience internalizing symptoms often have elevated levels of cortisol (Pariante & Lightman, 2008), which can compromise sleep (Vgontzas et al., 2003). Given that anxiety and depression have outward manifestations, this may explain why partner’s mental health may influence one’s sleep.
Findings add to the existing literature and identify “unique” effects of anxiety and depression as mediators and intervening variables of relations between destructive interpartner conflict and objectively assessed sleep over 1 year. With an independent sample from the one used in the present investigation, anxiety and depression functioned as mediators of some of the links between initial levels of psychological aggression, and change in aggression over 3 years (slope effects), and subjective sleep problems; some of the effects varied for husbands and wives (Rauer et al., 2010). Further, in a cross-sectional study based on the first wave of the present investigation, the APIM showed that women’s anxiety symptoms served as intervening variables of relations between their receipt of psychological aggression and their own objectively assessed sleep efficiency and duration (El-Sheikh et al., 2013). For men, their symptoms of depression functioned as intervening variables in similar associations involving their own sleep, and their anxiety symptoms influenced their wives’ sleep. Thus, although findings from the cross-sectional and longitudinal investigations are not identical, they both support the importance of mental health as a potential pathway of effects. Of course, longitudinal effects pertain to change in sleep over time versus sleep per se, possibly accounting for some of the differential effects. Collectively, results highlight the importance of examining not only one’s mental health but also that of the partner for a more nuanced explication of sleep in a family context.
Findings from this study have important implications. The National Sleep Foundation (2011) recommends allotting 7 to 9 hr of sleep per night. On average, sleep duration was on the low end of the recommended amount in our sample (M time spent in bed was 7 hr, 1 min per night at T1, and 6 hr, 56 min per night at T2). In addition, the autoregressive effects were highly stable for sleep duration and moderately stable for sleep quality, indicating that most individuals who had insufficient and poor quality sleep at T1 continued to do so over the course of 1 year. Taken together, there is a continued need to identify the sources of short and poor quality sleep. Further, prevention efforts aimed at promoting the use negotiation strategies during conflict hold promise for optimizing sleep.
Findings need to be interpreted within the study’s methodology and limitations. Although we examined symptoms of depression and anxiety as intervening and mediating variables in the link between conflict and sleep, other models are plausible. For example, although much evidence suggests that depression and anxiety symptoms can jeopardize sleep, the opposite direction of effects is possible because insufficient sleep can compromise mental health (Dinges, Rogers, & Baynard, 2005; Vanderlind et al., 2014). It is also possible that individuals experiencing mental health problems are not likely to engage in effective conflict tactics (Du Rocher Schudlich, Papp, & Cummings, 2004; Najman et al., 2014). Although the two study waves may constitute an advance in this area of inquiry, mediation effects are best examined with at least three waves of data. Further, results are based on a community sample, and thus results may not translate to clinical populations. However, given that significant relations were found between these variables using a community sample, it is likely that findings would be more robust among clinical samples. In addition, although actigraphy can effectively measure several important sleep parameters, it cannot assess sleep architecture. Examining relations between conflict and sleep architecture is an important future step toward better understanding the influence of familial processes on sleep. Further, differential effects observed for the various conflict strategies may be influenced by their endorsed frequency and associated variability (e.g., negotiation was endorsed more frequently than physical aggression). Despite these limitations, the current study builds on the literature in important ways and demonstrates that constructive conflict tactics forecast improved sleep, and that symptoms of depression and anxiety mediate relations between destructive interpartner conflict tactics and sleep over time.
Acknowledgments
The project described was supported by Grant R01HL093246 from the National Heart, Lung, and Blood Institute awarded to Mona El-Sheikh. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We thank our lab staff, most notably Bridget Wingo and Lori Elmore-Staton, for data collection and preparation, and the school personnel and participating families.
Contributor Information
Mona El-Sheikh, Mona El-Sheikh, Department of Human Development and Family Studies, Auburn University.
Kalsea J. Koss, Institute of Child Development, University of Minnesota
Ryan J. Kelly, Ryan J. Kelly, Department of Individual, Family, and Community Education, University of New Mexico
Amy J. Rauer, Department of Human Development and Family Studies, Auburn University
References
- Acebo C, Carskadon M. Scoring actigraphs data using ACTION-W2. Providence, RI: Bradley Sleep Center, Brown University; 2001. [Google Scholar]
- Acock AC. Working with missing values. Journal of Marriage and Family. 2005;67:1012–1028. http://dx.doi.org/10.1111/j.1741-3737.2005.00191.x. [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. http://dx.doi.org/10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA. Beck Anxiety Inventory Manual. San Antonio, TX: Psychological Corporation; 1993. [Google Scholar]
- Cole RJ, Kripke DF, Gruen W, Mullaney DJ, Gillin JC. Automatic sleep/wake identification from wrist activity. Sleep. 1992;15:461–469. doi: 10.1093/sleep/15.5.461. [DOI] [PubMed] [Google Scholar]
- Colten HR, Altevogt BM Institute of Medicine Committee on Sleep Medicine and Research. Sleep disorders and sleep deprivation: An unmet public health problem. Washington, DC: National Academies Press; 2006. [PubMed] [Google Scholar]
- Cousineau D, Chartier S. Outliers detection and treatment: A review. International Journal of Psychological Research. 2010;3:58–67. [Google Scholar]
- Cummings EM, Davies PT. Marital conflict and children: An emotional security perspective. New York, NY: Guilford Press; 2010. [Google Scholar]
- Cummings EM, Goeke-Morey MC, Papp LM. Children’s responses to everyday marital conflict tactics in the home. Child Development. 2003;74:1918–1929. doi: 10.1046/j.1467-8624.2003.00646.x. http://dx.doi.org/10.1046/j.1467-8624.2003.00646.x. [DOI] [PubMed] [Google Scholar]
- Dahl RE. The regulation of sleep and arousal: Development and psychopathology. Development and Psychopathology. 1996;8:3–27. http://dx.doi.org/10.1017/S0954579400006945. [Google Scholar]
- Dahl RE, El-Sheikh M. Considering sleep in a family context: Introduction to the special issue. Journal of Family Psychology. 2007;21:1–3. doi: 10.1037/0893-3200.21.1.1. http://dx.doi.org/10.1037/0893-3200.21.1.1. [DOI] [PubMed] [Google Scholar]
- Dahl RE, Lewin DS. Pathways to adolescent health sleep regulation and behavior. Journal of Adolescent Health. 2002;31(Suppl):175–184. doi: 10.1016/s1054-139x(02)00506-2. http://dx.doi.org/10.1016/S1054-139X(02)00506-2. [DOI] [PubMed] [Google Scholar]
- Dinges DF, Rogers NL, Baynard MD. Chronic sleep deprivation. In: Kryger MH, Roth T, Dement WC, editors. Principles and practices of sleep medicine. 4. Philadelphia, PA: W. B. Saunders; 2005. pp. 67–76. http://dx.doi.org/10.1016/B0-72-160797-7/50013-6. [Google Scholar]
- Du Rocher Schudlich TD, Papp LM, Cummings EM. Relations of husbands and wives dysphoria to marital conflict resolution strategies. Journal of Family Psychology. 2004;18:171–183. doi: 10.1037/0893-3200.18.1.171. http://dx.doi.org/10.1037/0893-3200.18.1.171. [DOI] [PubMed] [Google Scholar]
- El-Sheikh M, Kelly R, Rauer A. Quick to berate, slow to sleep: Interpartner psychological conflict, mental health, and sleep. Health Psychology. 2013;32:1057–1066. doi: 10.1037/a0031786. http://dx.doi.org/10.1037/a0031786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erath SA, Bierman KL the Conduct Problems Prevention Research Group. Aggressive marital conflict, maternal harsh punishment, and child aggressive-disruptive behavior: Evidence for direct and mediated relations. Journal of Family Psychology. 2006;20:217–226. doi: 10.1037/0893-3200.20.2.217. http://dx.doi.org/10.1037/0893-3200.20.2.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallicchio L, Kalesan B. Sleep duration and mortality: A systematic review and meta-analysis. Journal of Sleep Research. 2009;18:148–158. doi: 10.1111/j.1365-2869.2008.00732.x. http://dx.doi.org/10.1111/j.1365-2869.2008.00732.x. [DOI] [PubMed] [Google Scholar]
- Goeke-Morey MC, Cummings EM, Harold GT, Shelton KH. Categories and continua of destructive and constructive marital conflict tactics from the perspective of U.S. and Welsh children. Journal of Family Psychology. 2003;17:327–338. doi: 10.1037/0893-3200.17.3.327. http://dx.doi.org/10.1037/0893-3200.17.3.327. [DOI] [PubMed] [Google Scholar]
- Gottman JM. The roles of conflict engagement, escalation, and avoidance in marital interaction: A longitudinal view of five types of couples. Journal of Consulting and Clinical Psychology. 1993;61:6–15. doi: 10.1037//0022-006x.61.1.6. http://dx.doi.org/10.1037/0022-006X.61.1.6. [DOI] [PubMed] [Google Scholar]
- Gottman JM, Krokoff LJ. Marital interaction and satisfaction: A longitudinal view. Journal of Consulting and Clinical Psychology. 1989;57:47–52. doi: 10.1037//0022-006x.57.1.47. http://dx.doi.org/10.1037/0022-006X.57.1.47. [DOI] [PubMed] [Google Scholar]
- Gove WR, Hughes M, Style CB. Does marriage have positive effects on the psychological well-being of the individual? Journal of Health and Social Behavior. 1983;24:122–131. http://dx.doi.org/10.2307/2136639. [PubMed] [Google Scholar]
- Hasler BP, Troxel WM. Couples’ nighttime sleep efficiency and concordance: Evidence for bidirectional associations with daytime relationship functioning. Psychosomatic Medicine. 2010;72:794–801. doi: 10.1097/PSY.0b013e3181ecd08a. http://dx.doi.org/10.1097/PSY.0b013e3181ecd08a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hewitt PL, Norton GR. The Beck Anxiety Inventory: A psychometric analysis. Psychological Assessment. 1993;5:408–412. http://dx.doi.org/10.1037/1040-3590.5.4.408. [Google Scholar]
- Hicks AM, Diamond LM. Don’t go to bed angry: Attachment, conflict, and affective and physiological reactivity. Personal Relationships. 2011;18:266–284. http://dx.doi.org/10.1111/j.1475-6811.2011.01355.x. [Google Scholar]
- Holt-Lunstad J, Birmingham W, Jones BQ. Is there something unique about marriage? The relative impact of marital status, relationship quality, and network social support on ambulatory blood pressure and mental health. Annals of Behavioral Medicine. 2008;35:239–244. doi: 10.1007/s12160-008-9018-y. http://dx.doi.org/10.1007/s12160-008-9018-y. [DOI] [PubMed] [Google Scholar]
- Humphreys J, Lee K. Sleep disturbance in battered women living in transitional housing. Issues in Mental Health Nursing. 2005;26:771–780. doi: 10.1080/01612840591008401. http://dx.doi.org/10.1080/01612840591008401. [DOI] [PubMed] [Google Scholar]
- Johnson WL, Giordano PC, Longmore MA, Manning WD. Intimate partner violence and depressive symptoms during adolescence and young adulthood. Journal of Health and Social Behavior. 2014;55:39–55. doi: 10.1177/0022146513520430. http://dx.doi.org/10.1177/0022146513520430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kant GL, D’Zurilla TJ, Maydeu-Olivares A. Social problem solving as a mediator of stress-related depression and anxiety in middle-aged and elderly community residents. Cognitive Therapy and Research. 1997;21:73–96. http://dx.doi.org/10.1023/A:1021820326754. [Google Scholar]
- Kashy DA, Kenny DA. The analysis of data from dyads and groups. In: Reis HT, Judd CM, editors. Handbook of research methods in social and personality psychology. New York, NY: Cambridge University Press; 2000. pp. 451–477. [Google Scholar]
- Kelly RJ, El-Sheikh M. Longitudinal relations between marital aggression and children’s sleep: The role of emotional insecurity. Journal of Family Psychology. 2013;27:282–292. doi: 10.1037/a0031896. http://dx.doi.org/10.1037/a0031896. [DOI] [PubMed] [Google Scholar]
- Kenny DA, Kashy DA, Cook WL. Dyadic data analysis. New York, NY: Guilford Press; 2006. [Google Scholar]
- Kiecolt-Glaser JK, Newton TL. Marriage and health: His and hers. Psychological Bulletin. 2001;127:472–503. doi: 10.1037/0033-2909.127.4.472. http://dx.doi.org/10.1037/0033-2909.127.4.472. [DOI] [PubMed] [Google Scholar]
- Knutson KL, Rathouz PJ, Yan LL, Liu K, Lauderdale DS. Intra-individual daily and yearly variability in actigraphically recorded sleep measures: The CARDIA study. Sleep: Journal of Sleep and Sleep Disorders Research. 2007;30:793–796. doi: 10.1093/sleep/30.6.793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence E, Yoon J, Langer A, Ro E. Is psychological aggression as detrimental as physical aggression? The independent effects of psychological aggression on depression and anxiety symptoms. Violence and Victims. 2009;24:20–35. doi: 10.1891/0886-6708.24.1.20. http://dx.doi.org/10.1891/0886-6708.24.1.20. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. http://dx.doi.org/10.1037/1082-989X.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mezick EJ, Matthews KA, Hall M, Kamarck TW, Buysse DJ, Owens JF, Reis SE. Intra-individual variability in sleep duration and fragmentation: Associations with stress. Psychoneuroen-docrinology. 2009;34:1346–1354. doi: 10.1016/j.psyneuen.2009.04.005. http://dx.doi.org/10.1016/j.psyneuen.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy CM, Cascardi M. Psychological abuse in marriage and dating relationships. In: Hampton RL, editor. Family violence prevention and treatment. 2. Beverly Hills, CA: Sage; 1999. pp. 198–226. http://dx.doi.org/10.4135/9781452231983.n8. [Google Scholar]
- Najman JM, Khatun M, Mamun A, Clavarino A, Williams GM, Scott J, … Alati R. Does depression experienced by mothers leads to a decline in marital quality: A 21-year longitudinal study. Social Psychiatry and Psychiatric Epidemiology. 2014;49:121–132. doi: 10.1007/s00127-013-0749-0. http://dx.doi.org/10.1007/s00127-013-0749-0. [DOI] [PubMed] [Google Scholar]
- National Sleep Foundation. How much sleep do we really need? 2011 Retrieved from http://www.sleepfoundation.org/article/how-sleepworks/how-much-sleep-do-we-really-need.
- Pariante CM, Lightman SL. The HPA axis in major depression: Classical theories and new developments. Trends in Neuro-sciences. 2008;31:464–468. doi: 10.1016/j.tins.2008.06.006. http://dx.doi.org/10.1016/j.tins.2008.06.006. [DOI] [PubMed] [Google Scholar]
- Pigeon WR, Cerulli C, Richards H, He H, Perlis M, Caine E. Sleep disturbances and their association with mental health among women exposed to intimate partner violence. Journal of Women’s Health. 2011;20:1923–1929. doi: 10.1089/jwh.2011.2781. http://dx.doi.org/10.1089/jwh.2011.2781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Selig JP. Advantages of Monte Carlo confidence intervals for indirect effects. Communication Methods and Measures. 2012;6:77–98. http://dx.doi.org/10.1080/19312458.2012.679848. [Google Scholar]
- Radloff LS. The CES-D scale is a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. http://dx.doi.org/10.1177/014662167700100306. [Google Scholar]
- Rauer AJ, El-Sheikh M. Reciprocal pathways between intimate partner violence and sleep in men and women. Journal of Family Psychology. 2012;26:470–477. doi: 10.1037/a0027828. http://dx.doi.org/10.1037/a0027828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rauer AJ, Kelly RJ, Buckhalt JA, El-Sheikh M. Sleeping with one eye open: Marital abuse as an antecedent of poor sleep. Journal of Family Psychology. 2010;24:667–677. doi: 10.1037/a0021354. http://dx.doi.org/10.1037/a0021354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rauer A, Volling B. More than one way to be happy: A typology of marital happiness. Family Process. 2013;52:519–534. doi: 10.1111/famp.12028. http://dx.doi.org/10.1111/famp.12028. [DOI] [PubMed] [Google Scholar]
- Ren XS. Marital status and quality of relationships: The impact on health perception. Social Science & Medicine. 1997;44:241–249. doi: 10.1016/s0277-9536(96)00158-x. http://dx.doi.org/10.1016/S0277-9536(96)00158-X. [DOI] [PubMed] [Google Scholar]
- Rhoades KA, Leve LD, Harold GT, Mannering AM, Neiderhiser JM, Shaw DS, … Reiss D. Marital hostility and child sleep problems: Direct and indirect associations via hostile parenting. Journal of Family Psychology. 2012;26:488– 498. doi: 10.1037/a0029164. http://dx.doi.org/10.1037/a0029164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robles TF, Kiecolt-Glaser JK. The physiology of marriage: Pathways to health. Physiology & Behavior. 2003;79:409–416. doi: 10.1016/s0031-9384(03)00160-4. http://dx.doi.org/10.1016/S0031-9384(03)00160-4. [DOI] [PubMed] [Google Scholar]
- Rupp TL, Balkin TJ. Comparison of Motionlogger Watch and Actiwatch actigraphs to polysomnography for sleep/wake estimation in healthy young adults. Behavior Research Methods. 2011;43:1152–1160. doi: 10.3758/s13428-011-0098-4. http://dx.doi.org/10.3758/s13428-011-0098-4. [DOI] [PubMed] [Google Scholar]
- Sadeh A. The role and validity of actigraphy in sleep medicine: An update. Sleep Medicine Reviews. 2011;15:259–267. doi: 10.1016/j.smrv.2010.10.001. http://dx.doi.org/10.1016/j.smrv.2010.10.001. [DOI] [PubMed] [Google Scholar]
- Selig JP, Preacher KJ. Monte Carlo method for assessing mediation: An interactive tool for creating confidence intervals for indirect effects [Computer software] 2008 Retrieved from http://quantpsy.org/
- Straus MA. Manual for the Conflict Tactics Scales (CTS) and test forms for the Revised Conflict Tactics Scales. Durham, NH: Family Research Laboratory, University of New Hampshire; 1995. [Google Scholar]
- Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The revised Conflict Tactics Scales (CTS-2): Development and preliminary psychometric data. Journal of Family Issues. 1996;17:283–316. http://dx.doi.org/10.1177/019251396017003001. [Google Scholar]
- Taft CT, O’Farrell TJ, Torres SE, Panuzio J, Monson CM, Murphy M, Murphy CM. Examining the correlates of psychological aggression among a community sample of couples. Journal of Family Psychology. 2006;20:581–588. doi: 10.1037/0893-3200.20.4.581. http://dx.doi.org/10.1037/0893-3200.20.4.581. [DOI] [PubMed] [Google Scholar]
- Taylor DJ, Lichstein KL, Durrence HH, Reidel BW, Bush AJ. Epidemiology of insomnia, depression, and anxiety. Sleep. 2005;28:1457–1464. doi: 10.1093/sleep/28.11.1457. [DOI] [PubMed] [Google Scholar]
- Troxel WM, Buysse DJ, Hall M, Matthews KA. Marital happiness and sleep disturbances in a multi-ethnic sample of middle-aged women. Behavioral Sleep Medicine. 2009;7:2–19. doi: 10.1080/15402000802577736. http://dx.doi.org/10.1080/15402000802577736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troxel WM, Robles TF, Hall M, Buysse DJ. Marital quality and the marital bed: Examining the covariation between relationship quality and sleep. Sleep Medicine Reviews. 2007;11:389–404. doi: 10.1016/j.smrv.2007.05.002. http://dx.doi.org/10.1016/j.smrv.2007.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Commerce. How the Census Bureau measures poverty. n.d Retrived from http://www.census.gov/hhes/www/poverty/about/overview/measure.html.
- Vanderlind WM, Beevers CG, Sherman SM, Trujillo LT, McGeary JE, Matthews MD, … Schnyer DM. Sleep and sadness: Exploring the relation among sleep, cognitive control, and depressive symptoms in young adults. Sleep Medicine. 2014;15:144–149. doi: 10.1016/j.sleep.2013.10.006. http://dx.doi.org/10.1016/j.sleep.2013.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vgontzas AN, Zoumakis M, Bixler EO, Lin HM, Prolo P, Vela-Bueno A, … Chrousos GP. Impaired nighttime sleep in healthy old versus young adults is associated with elevated plasma interleukin-6 and cortisol levels: Physiologic and therapeutic implications. The Journal of Clinical Endocrinology and Metabolism. 2003;88:2087–2095. doi: 10.1210/jc.2002-021176. http://dx.doi.org/10.1210/jc.2002-021176. [DOI] [PubMed] [Google Scholar]
- Vickerman KA, Margolin G. Trajectories of physical and emotional marital aggression in midlife couples. Violence and Victims. 2008;23:18–34. doi: 10.1891/0886-6708.23.1.18. http://dx.doi.org/10.1891/0886-6708.23.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods SJ, Kozachik SL, Hall RJ. Subjective sleep quality in women experiencing intimate partner violence: Contributions of situational, psychological, and physiological factors. Journal of Traumatic Stress. 2010;23:141–150. doi: 10.1002/jts.20495. [DOI] [PubMed] [Google Scholar]
- Yang HC, Suh S, Kim H, Cho ER, Lee SK, Shin C. Testing bidirectional relationships between marital quality and sleep disturbances: A 4-year follow-up study in a Korean cohort. Journal of Psychosomatic Research. 2013;74:401–406. doi: 10.1016/j.jpsychores.2013.01.005. http://dx.doi.org/10.1016/j.jpsychores.2013.01.005. [DOI] [PubMed] [Google Scholar]