Abstract
The aim of this article is to present strategies for preventing and managing the failure of the surgical restoration of intestinal continuity. Despite improvements in surgical technique and perioperative care, anastomotic leaks still occur, and with them occur increased morbidity, mortality, length of stay, and costs. Due to the devastating consequences for patients with failed anastomoses, there have been a myriad of materials and techniques used by surgeons to create better intestinal anastomoses. We will also discuss the management strategies for anastomotic leak when they do inevitably occur.
Keywords: leak, anastomosis, testing, risk factors
Intestinal anastomosis as a viable surgical technique came into use after Antoine Lembert's (1802–1851) recognition of the importance of serosal apposition in an intestinal anastomosis, followed by William Stewart Halsted's (1852–1922) canine experiments identifying the mechanical strength and necessity of including the submucosal layer in an anastomosis.1 Failure of colorectal anastomoses can have dire consequences, both acute and longterm, including longer lengths of stay, more interventions, and increased morbidity and mortality.1 Colorectal anastomotic leak rates vary from 6 to 30% depending on risk factors and varying definitions of anastomotic leak.2 It is paramount to identify leaks early to minimize the potential morbidities of this complication. Despite advances in combating surgical infections, new devices for bowel reapproximation, better understanding of risk factors for anastomotic complications, and improved perioperative care, we continue to struggle with the occurrence and management of this complication.
Risk Factors
The location of an anastomosis is the most consistent determinant of the anastomotic leak. The more distal the anastomosis, the higher the likelihood of failure, with resection of a distal rectal cancer having almost a five-fold increased risk of anastomotic leak compared with resection for colon cancer.3 Multiple studies have found that men undergoing rectal resection have a higher anastomotic leak rate, presumably due to the narrow confines of a male pelvis and the resultant increased technical difficulty of the operation.4 5 Pre-existing conditions in the patients' tissues may also increase the risk of leak. Stumpf and colleagues found a significant difference in the ratio of collagen type I/III deposition as well as an increase in matrix metalloproteinase expression in patients with an anastomotic leak.6 Other risk factors include malnutrition, immunosuppression, diabetes, nonsteroidal anti-inflammatory drug (NSAID) use, and radiation therapy.
Malnutrition
Malnutrition is a risk factor for poor postoperative outcomes.6 A diagnosis of malnutrition can be made in a patient who has experienced a 10% or greater unintentional weight loss, serum albumin < 3.5 g/dL, or total protein concentration < 5.5 g/dL. Identifying these patients allows the surgeon to weigh the risks of proceeding with surgery or delaying operative intervention so that an attempt to correct the malnutrition can be made. In light of the disagreement in the literature over whether preoperative interventions to correct malnutrition are helpful, it may be advisable to continue to treat these patients as highrisk once they have been identified, even if the malnutrition has been addressed.
Immunosuppression
Colorectal anastomoses are frequently made in patients being treated with immunosuppressive therapy for inflammatory bowel disease (IBD) or, less commonly, for solid organ transplants. Unfortunately, much of our data from large patient populations come from retrospective studies as it relate to the effect this therapy has on the healing anastomosis. The conclusions that can be drawn from these studies involving heterogeneous populations tend to be very broad and do not help with specific patient recommendations. Additionally, patients who are immunosuppressed, especially patients with IBD, tend to be sicker with more comorbidities, thusmaking it difficult to attribute specific postoperative complications such as anastomotic leak to a single cause such as immunosuppression. The most widely studied group of these drugs is corticosteroids. The observational evidence for complications in patients treated with corticosteroids is relatively strong. The indications for steroid therapy in patients despite the risks make randomized clinical trials unfeasible. A recent large systematic review that investigated corticosteroids as a risk factor for anastomotic leakage included 12 studies with over 9500 patients.7 They found that 50% of the studies identified a higher leak rate in patients on steroids, and their pooled analysis showed that the anastomotic leakage rate was 6.77% (95% confidence interval [CI] 5.48–9.06) in the corticosteroid group and 3.26% (95% CI 2.94–3.58) in the noncorticosteroid group. While the authors are to be applauded for their efforts at investigating the role of these relatively common drugs and their effects on colorectal anastomosis, their conclusion “to use caution in these patients” illustrates the difficulties of making specific treatment guidelines. Unfortunately, while there is no level 1 data that determine what constitutes an increased risk due to perioperative corticosteroid administration, we can reduce this risk by minimizing exposure as much as possible. The limited efficacy of steroids in the maintenance of remission in patients with IBD results in the treatment of patients with immunomodulators such as azathioprine and 6-mercaptopurine. There is little evidence in the published literature that, alone, these agents increase the risk of an anastomotic leak.8
TNF-α is wellestablished in having a role in wound healing, and agents that block off this signaling pathway are associated with opportunistic infections, justifying concerns about postoperative complications in patients treated with these agents. Changes in IBD treatment paradigms such as the “top-down” approach and more widespread use of these biologic anti-TNF agents means that surgeons are encountering patients with IBD on these agents with increasing frequency. The data are not clear regarding the use of these agents as they relate specifically to the risk of anastomotic leaks after colorectal surgery. The conflicting data in the literature likely reflect the difficulty of performing a randomized controlled trial and differences in study design (retrospective and single institution), therapy duration, and disease severity.9 10 11 12 Although potentially devastating for a patient's postoperative recovery, it is fortunate that anastomotic leaks occur uncommonly. The frequency of this complication does make it difficult to study patient populations large enough to provide strong evidence for the role of immunosuppression as a direct cause for an anastomotic leak. In the absence of direct evidence, it can still be cautioned that patients treated with immunosuppressive therapy can be identified as being sicker or possibly having more extensive intestinal disease and should be treated as having an increased risk of postoperative complications, including anastomotic leak.
Nonsteroidal Anti-inflammatory Drug
Routine use of these medications as part of a scheduled multimodality postoperative pain regimen is a common component of pathways meant to decrease narcotic use and their attendant side effects in surgical patients. Increasing use of perioperative nonnarcotic analgesics as part of multimodal postoperative pain control has led to investigations of the effect of these drugs in colorectal surgery. Care must be taken when interpreting the results of these studies as the class of NSAIDs itself is broad, including both selective and nonselective cyclooxygenase-2 (COX-2) inhibitors. There is no accepted mechanism by which this class of drugs may lead to impaired healing or anastomotic failure that may guide inquiry into the unwanted effects of these agents. Hakkarainen and colleagues used a statewide database to retrospectively identify colorectal and bariatric patients treated with NSAIDs in the perioperative period. They identified patients in which postoperative reintervention was required in the first 90 days, presumably as a result of a failed anastomosis.13 Patients in the NSAID group had a modest increased risk of anastomotic leak after risk adjustment (odds ratio, 1.24 [95%CI 1.01–1.56]; p = 0.04), but further patient subset analysis revealed that the nonelective colorectal surgery patients had the highest risk of anastomotic leak, with 12.3% in the NSAID group and 8.3% in the non-NSAID group (odds ratio, 1.70 [95%CI 1.11–2.68]; p = 0.01). The available data do not allow for the identification of the specific agents used, but the authors do make note of the differential expression of the COX isozymes in periods of stress such as would be commonly encountered in patients undergoing nonelective surgery. Although these data are not definitive, they do suggest that the negative effects of increased narcotic exposure must be weighed against the possible benefits of multimodal therapy in a patient in whom the baseline COX expression is altered, such as in sepsis, infection, or hemodynamic instability. Whether these precautions could be extended to patients with chronic or acute inflammation remains to be seen.
Diabetes
The incidence of diabetes mellitus has doubled in the past 30 years and has been studied by many researchers with varied conclusions as to its role in contributing an increased risk of anastomotic leak after colorectal surgery. The difficulty of linking diabetes to a specific complication is likely a consequence of the disease being linked to other factors, such as obesity, that have already been shown to be associated with anastomotic failure. Studies demonstrating a relationship between diabetes and an anastomotic leak must be sufficiently powered to separate these conditions, which are very often found in the same patient populations. A meta-analysis analyzing data from seven reports that specifically looked at the relationship between diabetes and anastomotic leak rates found an increased risk with diabetes that persisted in subgroup analysis when controlling for BMI.14 An additive effect on risk was seen in patients with both a high BMI and diabetes. These results do not explain whether the mechanism of anastomotic failure is related to the chronic changes associated with the disease or to the effects of perioperative hyperglycemia. Hyperglycemia itself has been associated with increased postoperative complications, but no studies have directly shown an effect on colorectal anastomoses. Several guidelines have suggested that preoperative work-ups should include Hgb A1C levels to identify at-risk patients with a suggested cutoff of 7 g/dL.
Pelvic Radiation
Patients treated with neoadjuvant radiation for rectal cancer have higher risk for anastomotic leak. Surgeons performing rectal resections for cancer may have a lower threshold for proximal diversion due to the higher risk for complications.
Intraoperative Factors
The bowel anastomosis heals in a complex and coordinated fashion that has been arbitrarily divided into phases. The purpose of a surgical anastomosis is to approximate the two ends of bowel until tissue healing has matured to sufficient strength to support the biologic function of digestion. Initially, no strength comes from tissue healing, and the connection must be maintained completely by the chosen surgical technique. The method of anastomosis is often based on surgeon preference. Options include a handsewn or stapled anastomosis in various configurations,for example, side-to-side, end-to-end, side-to-end, or end-to-side. Additional options include suture material, staple heights, number of layers, and other strategies to protect a nascent anastomosis. Whether a handsewn anastomosis has one or two suture layers has not been shown to affect the incidence of anastomotic leak, as long as the serosa is apposed and submucosa is incorporated.15 The preferences of the surgeon will dictate many of these decisions, but the principles of a proper anastomosis remain unchanged: a tension-free approximation of healthy, well-perfused unobstructed bowel.
Splenic Flexure Takedown
The basic tenet of colorectal anastomosis creation is achieving a tension-free approximation of the bowel ends. The traditional recommendation that splenic flexure mobilization decreases the risk of colorectal anastomotic leak is based on the understanding that total mesorectal excision necessitates division of the inferior mesenteric artery and a low pelvic anastomosis. However, in the event of a more proximal anastomosis with the preservation of the left colic artery, then it may be argued that the mobilization of the splenic flexure in an obviously tension-free anastomosis is unnecessary.16
Intraoperative Inspection and Salvage
If the surgeon identifies a questionable aspect of an anastomosis, the anastomosis should be recreated if possible. Repair of the anastomosis can also be attempted. A less ideal choice is proximal diversion and should only be performed if it is impossible to take down the anastomosis and redo it. Methods of anastomotic inspection include gross inspection of the outside of the anastomosis for defects in tissue approximation or poorly inverted serosa or aberrant staples, endoluminal inspection of the lumen, palpation of the anastomosis, and inspection of the anastomotic rings after using the end-to-end stapler. The double-stapled technique has been widely adopted in the creation of low anastomosis, and the crossing of staple lines is a potential site for anastomotic failure vulnerable to ischemia or to the passage of hard stool. Single-stapled colorectal anastomotic techniques or the placement of inverting sutures are more suitable for more proximal anastomoses given the difficulty of placing sutures deep in the pelvis.17 18 Transanal reinforcing sutures may be placed at the crossed staple lines to reinforce low colorectal anastomoses.19
Intraoperative Air-Leak Testing
Intraoperative assessment of left-sided anastomoses is mandatory as they allow for the immediate identification of leaks with the potential for repair, reanastomosis, or diversion. Air-leak testing adds minimal time, risk, or cost, and is typically performed by filling the pelvis with saline, occluding the proximal bowel and instilling air transanally via a bulb syringe, rigid, or flexible endoscope. Air-leak testing may identify leaks in up to 25% of anastomoses.20 While not all positive air-leak tests go on to develop clinically or radiographically evident anastomotic leaks, clinically diagnosed anastomotic leak rates in air-leak–tested patients were lower than leak rates in controls (4 vs. 14%). A recent retrospective review of almost 1,000 patients showed a proportion of 7.9% of positive air-leak tests in left-sided colon resections.21 Patients with positive air-leak tests who were managed with intraoperative suture repair were significantly more likely to develop clinical leaks than those treated with reanastomosis or diversion.
Perfusion
A variety of techniques are available to assess perfusion, including Doppler ultrasonography, fluorescein dye angiography, and gross evaluation of pulsatile flow on transection of the marginal artery. Indocyanine green with intraoperative fluorescence angiography allows for the assessment of bowel wall perfusion by open, laparoscopic, or proctoscopic means.22 23 24
Defunctioning Stoma
Increased understanding of the adequacy of distal margins for rectal cancer has led to more sphincter-preserving operations and the accompanying low pelvic anastomoses.5 The indications for fecal diversion are controversial. A diverting stoma mitigates the clinical consequences of an anastomotic leak but does not prevent one.25 26 However, the need for an additional procedure for stoma closure and hospitalization, inconvenience of the stoma, and its attendant risks of complications is not insignificant.5
Diagnosis of Anastomotic Leak
The most severe consequence of an anastomotic leak is sepsis and mortality. Delay in the recognition and intervention of a significant anastomotic failure has been demonstrated to contribute directly to increased patient mortality.16 If we accept that some rate of anastomotic leak is inevitable, then it is imperative that we care for our postoperative patients with an appropriate level of suspicion for investigating and identifying anastomotic leaks before our patients' condition begin to deteriorate. Unfortunately, many of the findings associated with anastomotic leak are neither sensitive nor specific. Additionally, low rectal anastomoses are often accompanied by diverting ileostomies, which may mask the true extent of a leak, making the clinical presentation even more vague and delaying diagnosis until preoperative studies are performed in anticipation of ostomy reversal. Postoperative tachycardia, hyperthermia, tachypnea, oliguria, or mental status changes should raise one's clinical suspicions of an anastomotic leak. Routine laboratory investigations may reveal leukocytosis or increasing C-reactive protein.
There are a myriad of proposed definitions for anastomotic leaks, although it is generally accepted that radiographic demonstration of a large collection of free fluid, extravasation of contrast material, or a perianastomotic fluid collection is indicative of an anastomotic defect. The sensitivity and specificity of contrast enema for clinically significant abnormalities are 79.9 and 95.4%,respectively.27 Computed tomography (CT) offers the advantage of defining the anatomy to allow for management planning. Intravenous contrast can be very helpful in identifying abscesses, while the utility of oral contrast is debatable, especially with the associated risk of diarrhea from large volume hyperosmotic contrast solutions (Fig. 1). Rectal contrast can be very useful in evaluating the colorectal anastomosis and should be administered by a member of the surgical team or an experienced radiologist in the case of a fresh anastomosis, using a soft pliable catheter rather than a semirigid enema tip and exercising caution while inflating the balloon and instilling contrast to avoid occluding the anatomy and masking a leak or disrupting the anastomosis. Additional diagnostic investigations such as rigid proctoscopy/anoscopy or endoscopy may be required to determine the exact location and extent of the anastomotic dehiscence (Fig. 2).
Fig. 1.
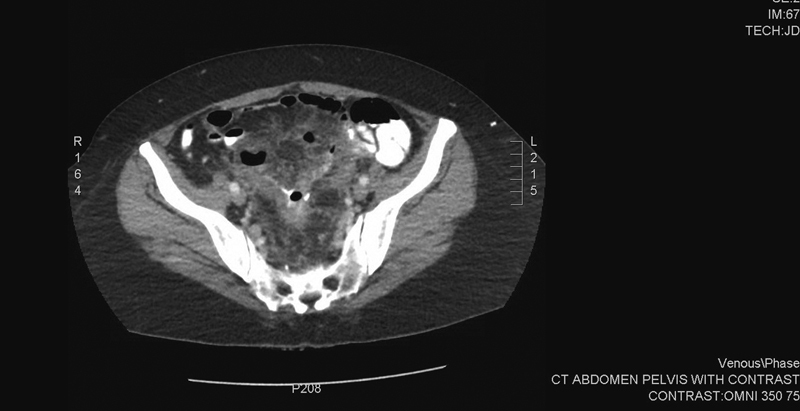
CT scan showing an anastomotic leak after sigmoid colectomy.
Fig. 2.
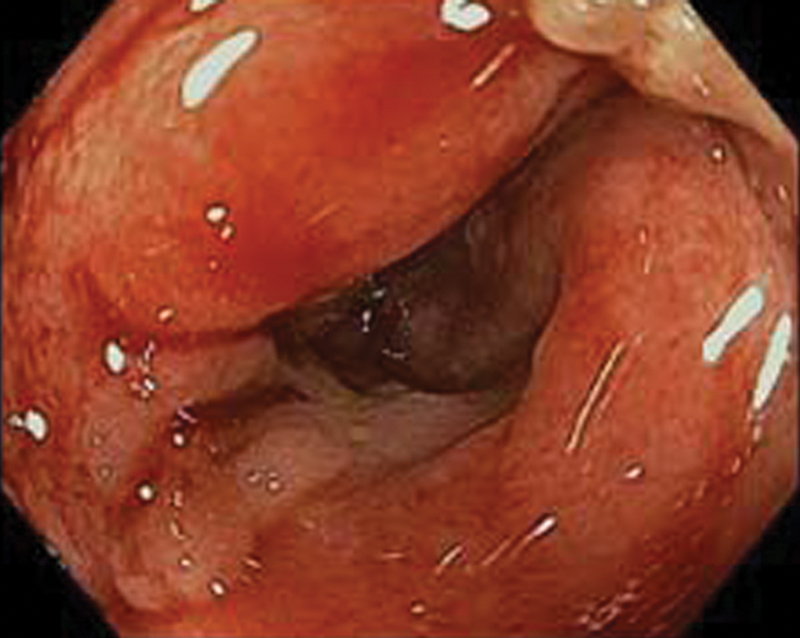
Endoscopic view of an anastomotic leak.
Management of Anastomotic Leak
Management of leaks must be guided by the patient's clinical course as some leaks are asymptomatic while others present as life-threatening surgical emergencies. Long-term considerations are also important, such as plans for adjuvant chemotherapy, expected bowel function, and quality of life. The International Study Group of Rectal Cancer proposed a grading system for the management of colorectal anastomotic leaks.28 Grade A anastomotic leaks are identified by radiographic findings of a perianastomotic fluid collection, leakage of contrast through the anastomosis, or observation of new drainage of enteric contents through either a drain or through a fistula but without accompanying clinical complaints. These may be managed expectantly. These may become apparent during the preoperative work-up prior to closure of a diverting ostomy and will at least delay reversal. Grade B leakage requires therapeutic intervention but does not necessarily require reoperation. Antibiotics and percutaneous drainage of fluid collections are the most common nonoperative interventions. Grade C anastomotic leakage requires relaparotomy. Surgical treatment is performed with the goal of controlling life-threatening sepsis. The traditional operation with takedown of the anastomosis and end colostomy may be appropriate, but washout with drain placement and diverting loop ileostomy may also be appropriate.
Antibiotics
Antibiotics are often our firstline of treatment in a symptomatic but stable patient and may be used alone or in combination with percutaneous drainage or reoperation depending on the severity of the leak. Treatment with broad-spectrum antibiotic with gram negative and anaerobic coverage is a reasonable option for small fluid collections that are not amenable to percutaneous drainage.
Drainage
Much of what we know about the effectiveness of image-guided percutaneous drainage comes from the clinical experience with processes such as diverticulitis, perforated appendicitis, and fistulizingCrohn's disease rather than with anastomotic leak. The decision to proceed with percutaneous drainage is based on the presence of a safe radiographic “window,” the availability of an experienced radiologist, the homogeneity of the fluid collection, and a large enough abscess (at least 3cm).29 30 Continuing leakage of enteric contents or lack of clinical improvement should be treated with more aggressive interventions.
For low-lying anastomosis that can be reached by endoscopic or transanal drainage, there are other options for potentially salvaging the failed anastomosis given the relative confines of the pelvic cavity. During an examination under anesthesia, proctoscopy can be used to place a drain (small Mallinckrodt) through the defect into the extraluminal fluid collection.31 This is especially effective in cases of small (<1 cm) defects with a draining sinus cavity in the pelvis. Placement of a transanal drain also allows for follow-up radiographic surveillance of the abscess cavity by the instillation of contrast through the drain. The drain may be removed when the cavity has decreased to the size of the drain. Successful resolution of the defect does not remove the risk of long-term complications associated with anastomotic leaks such as stricture formation and poor bowel function.
Stenting
Although not FDA-approved, several groups have investigated the role of endoscopically placed self-expanding metal stents or covered stents in the treatment of an anastomotic leak with promising results32 33 (Figs. 3 4 5). Stent migration remains a significant issue as most patients were found to spontaneously expel the stent, some of whom required stent replacement for unhealed defects. The stents appear to be welltolerated. While the use of self-expanding metal stents remains an investigative therapy for anastomotic leak, we find it an attractive option in patients with favorable anatomy, provided that percutaneous drainage of the extraluminal abscess is performed. The current covered stents do not have a large enough diameter to minimize stent migration. Until appropriate stents are available, the risk of stent migration may be mitigated by the use of endoclips; however, these case series demonstrate that clips remain marginally effective.
Fig. 3.
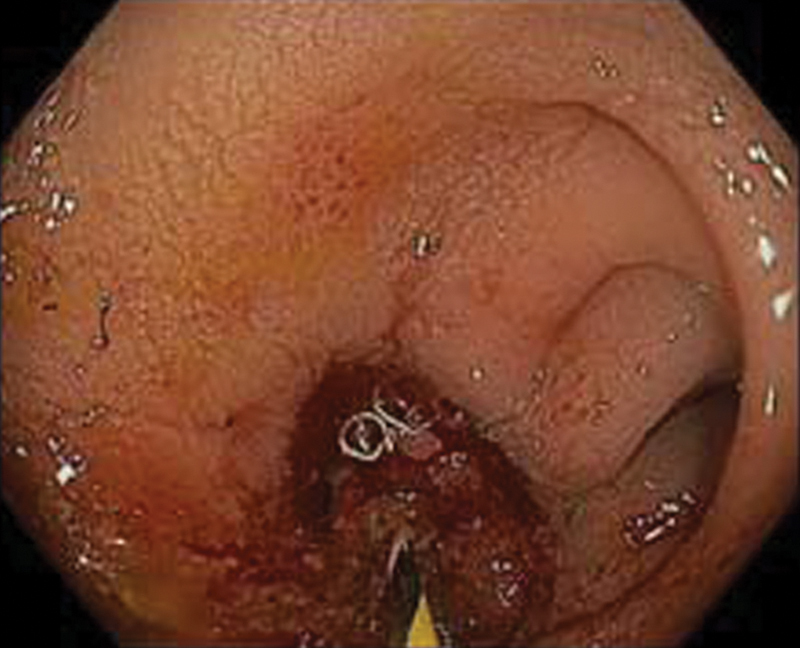
Guide wire placement prior to stent placement.
Fig. 4.
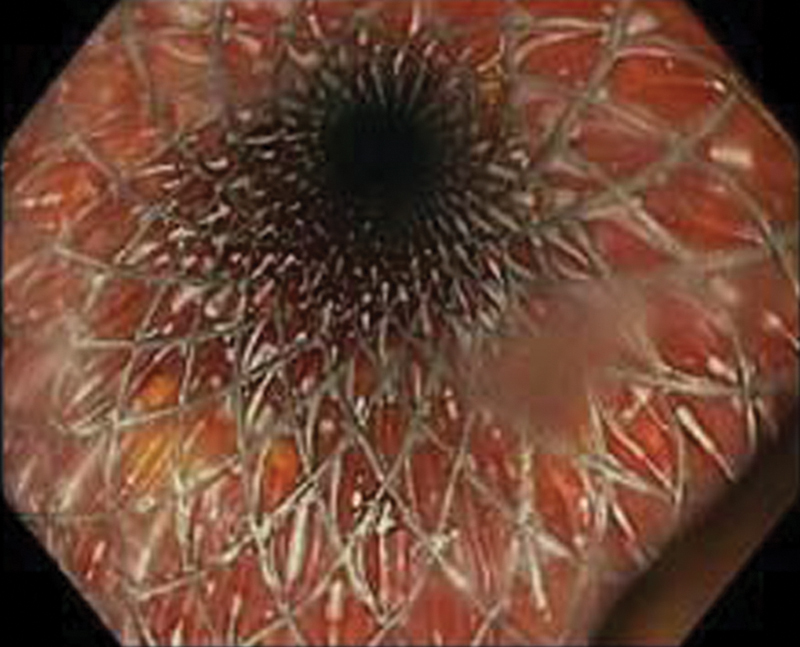
Deployed stent.
Fig. 5.
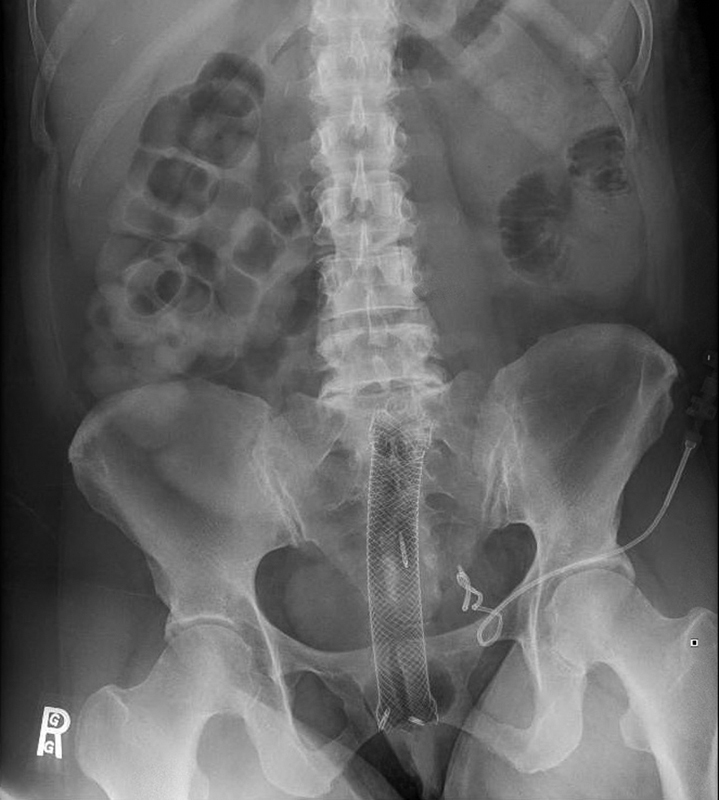
Final stent placement with endoclips to secure percutaneously placed drain.
Vacuum Therapy/Endo-Sponge
Initially described in 2008, endoscopic placed negative pressure therapy or VAC therapy has been shownto be effective in closing extraperitoneal anastomotic leaks.34 Weidenhagen and colleagues reported successful treatment with endosponge in 29 out of 34 patients with anastomotic leaks, with a mean duration of therapy of 34 days requiring an average of 11 sponge exchanges.35 Arezzo and colleagues reported a 79% cure rate in 14 anastomotic leaks with a mean healing time of 40 days, noting greater success in patients undergoing early therapy and who did not have prior pelvic radiation.36 Despite FDA approval in 2012 and a 10-year history of use in Europe, B. Braun Medical® (Melsungen, Germany) no longer manufactures or markets the Endo-Sponge® in the United States.
Surgical Intervention
Despite the increasing array of nonoperative options, surgical intervention still has an important role in the management of anastomotic leak. Patients who do not improve with nonoperative measures or who have sepsis and peritonitis must undergo surgical treatment. Source control with washout and fecal diversion are the main goals of surgical intervention for anastomotic leak. Fecal diversion can be accomplished by taking down the anastomosis and creating an end colostomy, proximal diversion with a loop ileostomy while leaving the leaking anastomosis alone, or repair or revision of the leaking anastomosis with proximal diversion.37 38
Minimally Invasive Techniques
The role of minimally invasive surgery in the treatment of colorectal anastomotic leaks is an active area of study. Retrospective analysis of laparoscopic peritoneal lavage and ileostomy creation has shown low morbidity and mortality rates compared with open surgery.39
References
- 1.Dietz U A, Debus E S. Intestinal anastomoses prior to 1882; a legacy of ingenuity, persistence, and research form a foundation for modern gastrointestinal surgery. World J Surg. 2005;29(3):396–401. doi: 10.1007/s00268-004-7720-x. [DOI] [PubMed] [Google Scholar]
- 2.Peel A L Taylor E W; Surgical Infection Study Group. Proposed definitions for the audit of postoperative infection: a discussion paper Ann R CollSurgEngl 1991736385–388. [PMC free article] [PubMed] [Google Scholar]
- 3.Mirnezami A, Mirnezami R, Chandrakumaran K, Sasapu K, Sagar P, Finan P. Increased local recurrence and reduced survival from colorectal cancer following anastomotic leak: systematic review and meta-analysis. Ann Surg. 2011;253(5):890–899. doi: 10.1097/SLA.0b013e3182128929. [DOI] [PubMed] [Google Scholar]
- 4.Kingham T P, Pachter H L. Colonic anastomotic leak: risk factors, diagnosis, and treatment. J Am CollSurg. 2009;208(2):269–278. doi: 10.1016/j.jamcollsurg.2008.10.015. [DOI] [PubMed] [Google Scholar]
- 5.Boccola M A, Buettner P G, Rozen W M. et al. Risk factors and outcomes for anastomotic leakage in colorectal surgery: a single-institution analysis of 1576 patients. World J Surg. 2011;35(1):186–195. doi: 10.1007/s00268-010-0831-7. [DOI] [PubMed] [Google Scholar]
- 6.Stumpf M, Klinge U, Wilms A. et al. Changes of the extracellular matrix as a risk factor for anastomotic leakage after large bowel surgery. Surgery. 2005;137(2):229–234. doi: 10.1016/j.surg.2004.07.011. [DOI] [PubMed] [Google Scholar]
- 7.Eriksen T F, Lassen C B, Gögenur I. Treatment with corticosteroids and the risk of anastomotic leakage following lower gastrointestinal surgery: a literature survey. Colorectal Dis. 2014;16(5):O154–O160. doi: 10.1111/codi.12490. [DOI] [PubMed] [Google Scholar]
- 8.Rullier E, Laurent C, Garrelon J L, Michel P, Saric J, Parneix M. Risk factors for anastomotic leakage after resection of rectal cancer. Br J Surg. 1998;85(3):355–358. doi: 10.1046/j.1365-2168.1998.00615.x. [DOI] [PubMed] [Google Scholar]
- 9.Appau K A, Fazio V W, Shen B. et al. Use of infliximab within 3 months of ileocolonic resection is associated with adverse postoperative outcomes in Crohn's patients. JGastrointestSurg. 2008;12(10):1738–1744. doi: 10.1007/s11605-008-0646-0. [DOI] [PubMed] [Google Scholar]
- 10.Kunitake H Hodin R Shellito P C Sands B E Korzenik J Bordeianou L Perioperative treatment with infliximab in patients with Crohn's disease and ulcerative colitis is not associated with an increased rate of postoperative complications JGastrointestSurg 200812101730–1736., discussion 1736–1737 [DOI] [PubMed] [Google Scholar]
- 11.Selvasekar C R Cima R R Larson D W et al. Effect of infliximab on short-term complications in patients undergoing operation for chronic ulcerative colitis J Am CollSurg 20072045956–962., discussion 962–963 [DOI] [PubMed] [Google Scholar]
- 12.Syed A, Cross R K, Flasar M H. Anti-tumor necrosis factor therapy is associated with infections after abdominal surgery in Crohn's disease patients. Am J Gastroenterol. 2013;108(4):583–593. doi: 10.1038/ajg.2012.464. [DOI] [PubMed] [Google Scholar]
- 13.Hakkarainen T W, Steele S R, Bastaworous A. et al. Nonsteroidal anti-inflammatory drugs and the risk for anastomotic failure: a report from Washington State's Surgical Care and Outcomes Assessment Program (SCOAP) JAMA Surg. 2015;150(3):223–228. doi: 10.1001/jamasurg.2014.2239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lin X, Li J, Chen W. et al. Diabetes and risk of anastomotic leakage after gastrointestinal surgery. JSurg Res. 2015;196(2):294–301. doi: 10.1016/j.jss.2015.03.017. [DOI] [PubMed] [Google Scholar]
- 15.Shikata S, Yamagishi H, Taji Y, Shimada T, Noguchi Y. Single- versus two- layer intestinal anastomosis: a meta-analysis of randomized controlled trials. BMC Surg. 2006;6:2. doi: 10.1186/1471-2482-6-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kennedy R, Jenkins I, Finan P J. Controversial topics in surgery: splenic flexure mobilisation for anterior resection performed for sigmoid and rectal cancer. Ann R CollSurgEngl. 2008;90(8):638–642. doi: 10.1308/003588408X358774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hüttner F J, Tenckhoff S, Jensen K. et al. Meta-analysis of reconstruction techniques after low anterior resection for rectal cancer. Br J Surg. 2015;102(7):735–745. doi: 10.1002/bjs.9782. [DOI] [PubMed] [Google Scholar]
- 18.Ikeda T, Kumashiro R, Oki E. et al. Evaluation of techniques to prevent colorectal anastomotic leakage. JSurg Res. 2015;194(2):450–457. doi: 10.1016/j.jss.2014.11.045. [DOI] [PubMed] [Google Scholar]
- 19.Kim I Y, Kim B R, Kim Y W. Applying reinforcing sutures to stapled colorectal anastomosis after low anterior resection for rectal cancer. Eur J SurgOncol. 2015;41(6):808–809. doi: 10.1016/j.ejso.2015.03.230. [DOI] [PubMed] [Google Scholar]
- 20.Beard J D, Nicholson M L, Sayers R D, Lloyd D, Everson N W. Intraoperative air testing of colorectal anastomoses: a prospective, randomized trial. Br J Surg. 1990;77(10):1095–1097. doi: 10.1002/bjs.1800771006. [DOI] [PubMed] [Google Scholar]
- 21.Ricciardi R Roberts P L Marcello P W Hall J F Read T E Schoetz D J Anastomotic leak testing after colorectal resection: what are the data? Arch Surg 20091445407–411., discussion 411–412 [DOI] [PubMed] [Google Scholar]
- 22.Ris F, Hompes R, Cunningham C. et al. Near-infrared (NIR) perfusion angiography in minimally invasive colorectal surgery. SurgEndosc. 2014;28(7):2221–2226. doi: 10.1007/s00464-014-3432-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jafari M D, Wexner S D, Martz J E. et al. Perfusion assessment in laparoscopic left-sided/anterior resection (PILLAR II): a multi-institutional study. J Am CollSurg. 2015;220(1):82–920. doi: 10.1016/j.jamcollsurg.2014.09.015. [DOI] [PubMed] [Google Scholar]
- 24.Kin C, Vo H, Welton L, Welton M. Equivocal effect of intraoperative fluorescence angiography on colorectal anastomotic leaks. Dis Colon Rectum. 2015;58(6):582–587. doi: 10.1097/DCR.0000000000000320. [DOI] [PubMed] [Google Scholar]
- 25.Hüser N, Michalski C W, Erkan M. et al. Systematic review and meta-analysis of the role of defunctioning stoma in low rectal cancer surgery. Ann Surg. 2008;248(1):52–60. doi: 10.1097/SLA.0b013e318176bf65. [DOI] [PubMed] [Google Scholar]
- 26.Tan W S, Tang C L, Shi L, Eu K W. Meta-analysis of defunctioning stomas in low anterior resection for rectal cancer. Br J Surg. 2009;96(5):462–472. doi: 10.1002/bjs.6594. [DOI] [PubMed] [Google Scholar]
- 27.Habib K, Gupta A, White D, Mazari F A, Wilson T R. Utility of contrast enema to assess anastomotic integrity and the natural history of radiological leaks after low rectal surgery: systematic review and meta-analysis. Int J Colorectal Dis. 2015;30(8):1007–1014. doi: 10.1007/s00384-015-2225-7. [DOI] [PubMed] [Google Scholar]
- 28.den Dulk M, Noter S L, Hendriks E R. et al. Improved diagnosis and treatment of anastomotic leakage after colorectal surgery. Eur J SurgOncol. 2009;35(4):420–426. doi: 10.1016/j.ejso.2008.04.009. [DOI] [PubMed] [Google Scholar]
- 29.Kumar R R, Kim J T, Haukoos J S. et al. Factors affecting the successful management of intra-abdominal abscesses with antibiotics and the need for percutaneous drainage. Dis Colon Rectum. 2006;49(2):183–189. doi: 10.1007/s10350-005-0274-7. [DOI] [PubMed] [Google Scholar]
- 30.Phitayakorn R, Delaney C P, Reynolds H L. et al. Standardized algorithms for management of anastomotic leaks and related abdominal and pelvic abscesses after colorectal surgery. World J Surg. 2008;32(6):1147–1156. doi: 10.1007/s00268-008-9468-1. [DOI] [PubMed] [Google Scholar]
- 31.Sirois-Giguère E, Boulanger-Gobeil C, Bouchard A. et al. Transanal drainage to treat anastomotic leaks after low anterior resection for rectal cancer: a valuable option. Dis Colon Rectum. 2013;56(5):586–592. doi: 10.1097/DCR.0b013e31827687a4. [DOI] [PubMed] [Google Scholar]
- 32.Abbas M A. Endoscopic management of acute colorectal anastomotic complications with temporary stent. JSLS. 2009;13(3):420–424. [PMC free article] [PubMed] [Google Scholar]
- 33.Lamazza A, Sterpetti A V, De Cesare A, Schillaci A, Antoniozzi A, Fiori E. Endoscopic placement of self-expanding stents in patients with symptomatic anastomotic leakage after colorectal resection for cancer: long-term results. Endoscopy. 2015;47(3):270–272. doi: 10.1055/s-0034-1391403. [DOI] [PubMed] [Google Scholar]
- 34.Glitsch A, von Bernstorff W, Seltrecht U, Partecke I, Paul H, Heidecke C D. Endoscopic transanal vacuum-assisted rectal drainage (ETVARD): an optimized therapy for major leaks from extraperitoneal rectal anastomoses. Endoscopy. 2008;40(3):192–199. doi: 10.1055/s-2007-995384. [DOI] [PubMed] [Google Scholar]
- 35.Weidenhagen R, Gruetzner K U, Wiecken T, Spelsberg F, Jauch K W. Endoluminal vacuum therapy for the treatment of anastomotic leakage after anterior rectal resection. RozhlChir. 2008;87(8):397–402. [PubMed] [Google Scholar]
- 36.Arezzo A, Verra M, Passera R, Bullano A, Rapetti L, Morino M. Long-term efficacy of endoscopic vacuum therapy for the treatment of colorectal anastomotic leaks. Dig Liver Dis. 2015;47(4):342–345. doi: 10.1016/j.dld.2014.12.003. [DOI] [PubMed] [Google Scholar]
- 37.Fraccalvieri D, Biondo S, Saez J. et al. Management of colorectal anastomotic leakage: differences between salvage and anastomotic takedown. Am J Surg. 2012;204(5):671–676. doi: 10.1016/j.amjsurg.2010.04.022. [DOI] [PubMed] [Google Scholar]
- 38.Rickert A Willeke F Kienle P Post S Management and outcome of anastomotic leakage after colonic surgery Colorectal Dis 201012(10 Online):e216–e223. [DOI] [PubMed] [Google Scholar]
- 39.Lee C M, Huh J W, Yun S H. et al. Laparoscopic versus open reintervention for anastomotic leakage following minimally invasive colorectal surgery. SurgEndosc. 2015;29(4):931–936. doi: 10.1007/s00464-014-3755-8. [DOI] [PubMed] [Google Scholar]


