Abstract
Introduction
It has been argued in current studies that anabolic androgenic steroids (AAS) are misused by a great number of bodybuilders and athletes. However, there is diverse and often conflicting scientific data on the cardiac and metabolic complications caused by the misuse of AAS. There may be various reasons for myocardial infarction (MI) with normal coronary arteries. However, for the majority of patients, the exact cause is still unknown.
Case report
A 32 year-old male who was complaining about severe chest pain was admitted to our emergency department. He had been taking methenolone acetate 200 mg weekly for a period of three years for body building. His cardiac markers were significantly elevated and electrocardiogram (ECG) showed peaked T waves in all derivations, which did not show ST elevation or depression. Both right and left coronary artery systems were found to be completely normal as a result of the angiogram.
Conclusion
The purpose of this study is to show that AAS induced MI can be encountered with normal coronary arteries during acute coronary syndrome.
Keywords: Bodybuilder, Anabolic steroids, Methenolone acetate, Acute coronary syndrome
1. Introduction
Anabolic steroids, which are synthetic by-products of testosterone, were initially formed as supplemental therapy for various medical conditions. In several countries, they are used to increase muscle mass and improve athletic performance.1 Whether illegal or medically recorded, use of anabolic steroid has been correlated with a great number of subsequent defects within the systems of the body.2 AAS use has been linked to a range of different cardiovascular side effects and is associated with cardiotoxicity.3 In case reports, acute MI very commonly presented, but a small number of other adverse cardiovascular effects such as left ventricular hypertrophy, reduced left ventricular function, arterial thrombosis, and several cases of sudden cardiac death have also been reported.4 Even after the discontinuation of its use, these effects continue for a long time and they are found to have an important impact on subsequent morbidity and mortality.2 This case report discusses the mechanism of coronary spasm resulting from the use of anabolic steroids.
2. Case
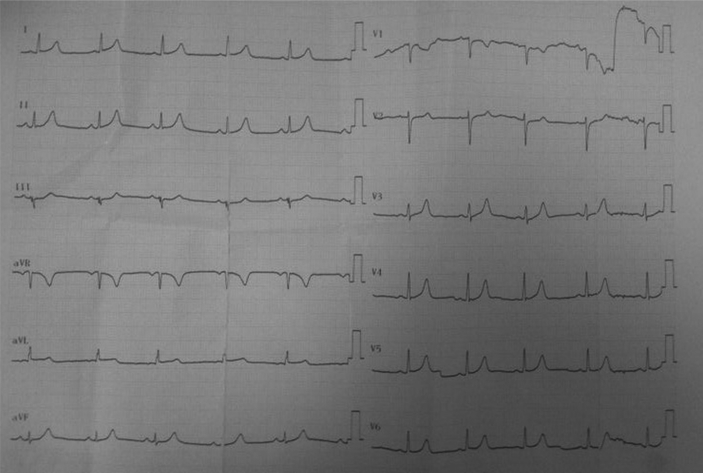
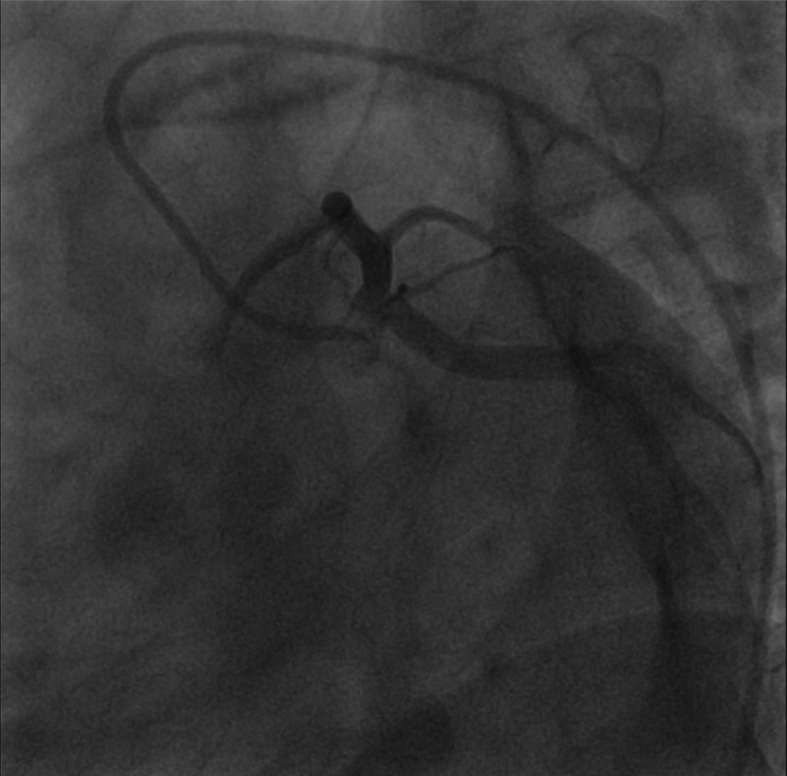
A 32 year-old male who was complaining of severe chest pain was admitted to our emergency department. He was discharged from the hospital where he was admitted two days prior with similar complaints since his ECG and cardiac marker results were normal. His chest pain continued on and off for two days, the longest of which continued for half an hour straight. Three hours prior to coming to the hospital, his chest pain started again and didn't go away. The pain spread to the patient's neck and left arm. Before he came to the hospital, he had been taking methenolone acetate 200 mg weekly for a period of three years for body building. Although the maintenance dose of the medicine was prescribed as 100 mg bi-weekly, the patient had exceeded this dose. The patient's anamnesis did not show any other illness or history of using other medication. His physical examination showed that he was conscious but extremely anxious. He had a blood pressure of 125/75 mmHg, a pulse rate of 74 beats/min and a respiratory rate of 16 breaths/min. Although his cardiac markers were significantly elevated (Table 1), his ECG showed peaked T waves in all derivations, which did not show ST elevation or depression (Fig. 1). There was no ECG alteration until performing diagnostic coronary angiogram. The type of the pain brought to mind the possibility of unstable angina. His bedside transthoracic echocardiogram was normal. Since the patient had constant chest pain, a diagnostic coronary angiogram was performed. Both the right and left coronary artery systems were found to be completely normal as a result of the angiogram (Fig. 2, Fig. 3). The patient had another ECG which revealed no structural heart disease. Detailed hematologic tests were performed to test for coagulation defect, but the results were negative. The patient's thyroid functions were also normal. He was prescribed oral diltiazem (60 mg) three times a day and ramipril (2.5 mg) once a day, then discharged from the hospital. Upon follow up a week later, it was found that the patient had not had any angina attacks for a week and his echocardiography was normal.
Table 1.
The patient's pathological cardiac test results.
| 2 days Before | Admitted | 2th day | 3th day | 5th day | |
|---|---|---|---|---|---|
| CK | 198 | 1909 | 2550 | 1758 | 254 |
| CK-MB | 16 | 80 | 115 | 79 | 38 |
| TROPONIN-I | 0.003 | 36,783 | >50,000 | 8645 | 2770 |
CK: Creatine Kinase; CK-MB: Creatine Kinase-MB.
Fig. 1.
The patient's ECG when he first came to the hospital.
Fig. 2.
The patient's left coronary angiography.
Fig. 3.
The patient's right coronary angiography.
3. Discussion
Coronary embolism, hypercoagulable states, intense sympathetic stimulation, non atherosclerotic coronary diseases, coronary trauma, coronary spasm, coronary thrombosis, imbalance between oxygen demand and supply, and endothelial dysfunction are the possible pathophysiological mechanisms that cause myocardial infarction with normal coronary arteries.5 Most commonly used stimulants (e.g. cocaine, cigarettes, marijuana, alcohol, butane, and amphetamines) have been reported to cause acute MI secondary to intense coronary vasospasm in youths when used alone or in combination.6
Congenital coagulation abnormalities are another possible cause of MI with normal coronary arteries. Due to the small number of the samples in previous studies, no definitive conclusion could be obtained. In a multicenter study of patients with MI and normal coronary arteries, a higher prevalence of factor V Leiden has been shown.7 However, PT, aPTT, INR, and hypercoagulopathy tests of our case were normal. Thus, hypercoagulability was not considered.
Other reported causes of MI include coronary vasculitis, either isolated or secondary to systemic connective tissue disorders like systemic lupus erythematosus and dermatomyositis.8 Since the patient had no history of systemic diseases and since his physical examination revealed normal C-reactive protein and sedimentation, connective tissue disorders were not considered.
When non-ischemic reasons that coincide with cardiac enzyme elevation are considered, congestive cardiac failure, pulmonary embolism, cardiac trauma, and myocardial agents such as adriamycin or 5-fluorouracil come to mind.9 However, the character of the patient's pain, absence of tachypnea and dyspnea, the patient's age and trauma history, absence of other medications, and the significant elevation in cardiac markers exclude these diagnoses.
In this case, when the type of the pain was considered during the prediagnosis, the patient was thought to have unstable angina pectoris. However, peaked T waves and hyperacute ST elevation suggested MI, while elevated cardiac markers brought non ST elevation to mind. The fact that the coronary arteries were normal in the angiogram showed that the patient had vasospastic Prinzmetal's angina. Steroids activate vasospasm by a number of other mechanisms. It has been shown by Ferrer et al that following chronic nandrolone therapy, decreased relaxation of the thoracic aorta is correlated with decreased concentrations of arterial endothelial cyclic guanosine monophosphate (cGMP), which suggests that guanylyl cyclase may also be directly inhibited by androgens.10 We are of the opinion that our patient developed cGMP inhibition caused by anabolic androgenic steroid use, which led to coronary vasospasm.
4. Conclusion
Individuals, particularly athletes and those on a specific diet, should be under the supervision of a physician so that the short- and long-term effects of the chemical and biological substances they are using can be monitored. Asking about herbal or hormonal therapies that the patient uses for weight loss, body building, or diluting the blood in addition to the medication that they use regularly while gathering the patient's history will be helpful in making a diagnosis.
Conflict of interest
The authors declare that there are no conflicts of interest.
Footnotes
Peer review under responsibility of The Emergency Medicine Association of Turkey.
References
- 1.Martinez-Quintana E., Saiz-Udaeta B., Marrero-Negrin N., Lopez-Mérida X., Rodriguez-Gonzalez F., Nieto-Lago V. Androgenic anabolic steroid, cocaine and amphetamine abuse and adverse cardiovascular effects. Int J Endocrinol Metab. 2013;11:8755. doi: 10.5812/ijem.8755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weinberger I., Rotenberg Z., Fuchs J., Sagy A., Friedmann J., Agmon J. Myocardial infarction in young adults under 30 years: risk factors and clinical course. Clin Cardiol. 1987;10:9–15. doi: 10.1002/clc.4960100104. [DOI] [PubMed] [Google Scholar]
- 3.Luijkx T., Velthuis B.K., Backx F.J., Buckens C.F., Prakken N.H., Rienks R. Anabolic androgenic steroid use is associated with ventricular dysfunction on cardiac MRI in strength trained athletes. Int J Cardiol. 2013;167:664–668. doi: 10.1016/j.ijcard.2012.03.072. [DOI] [PubMed] [Google Scholar]
- 4.Vanberg P., Atar D. Androgenic anabolic steroid abuse and the cardiovascular system. Handb Exp Pharmacol. 2010;195:411–457. doi: 10.1007/978-3-540-79088-4_18. [DOI] [PubMed] [Google Scholar]
- 5.Sullivan M.L., Martinez C.M., Gennis P., Gallagher E.J. The cardiac toxicity of anabolic steroids. Prog Cardiovasc Dis. 1998;41:1–15. doi: 10.1016/s0033-0620(98)80019-4. [DOI] [PubMed] [Google Scholar]
- 6.Ozgur S., Kaya H., Gokdemir M.T., Sezen Y. Acute myocardial infarction and coronary vasospasm associated with the ingestion of cayenne pepper pills in a 25-year-old male. Int J Emerg Med. 2012;5:5 doi: 10.1186/1865-1380-5-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abid L., Bahloul A., Frikha Z., Mallek S., Abid D., Akrout M. Myocardial infarction and normal coronary arteries: the experience of the cardiology department of Sfax, Tunisia. Intern Med. 2012;51:1959–1967. doi: 10.2169/internalmedicine.51.6545. [DOI] [PubMed] [Google Scholar]
- 8.Rangel A., Lavalle C., Chávez E., Jiménez M., Acosta J.L., Baduí E. Myocardial infarction in patients with systemic lupus erythematosus with normal findings from coronary arteriography and without coronary vasculitis: case reports. Angiology. 1999;50:245–253. doi: 10.1177/000331979905000310. [DOI] [PubMed] [Google Scholar]
- 9.Habif S. Cardiac troponins. T Klin J Med Sci. 2003;23:74–80. [Google Scholar]
- 10.Ferrer M., Encabo A., Marin J., Balfagon G. Chronic treatment with anabolic steroid, nandrolone, inhibits vasodilatory responses in rabbit aorta. Eur J Pharmacol. 1994;252:233–241. doi: 10.1016/0014-2999(94)90602-5. [DOI] [PubMed] [Google Scholar]