Abstract
Wellens' Syndrome is a pattern of electrocardiographic T-wave changes associated with critical, proximal left anterior descending (LAD) artery stenosis. Diagnostic criteria of Wellens' Syndrome are history of chest pain, little or no cardiac enzyme elevation, little or no ST-segment elevation, no loss of precordial R waves, no pathologic precordial Q waves and typical T-wave changes. Urgent cardiac catheterization is vital to prevent myocardial necrosis. Here we are presenting two cases with Wellens' Syndrome who had been sent for catheterization before marked myocardial infarction developed.
The first case was 63 years old woman admitted to emergency room with a typical chest pain lasting for 7 h. Electrocardiography (ECG) revealed characteristic Type A Wellens' Syndrome. The second case was also a 64 years old female patient. She was admitted to emergency room with a chest pain lasting for 2 days. Type B Wellens' Syndrome was considered according to ECG and clinical findings. Emergency angiography revealed critical LAD occlusions which were resolved before marked MI occurred in both of the cases.
It is important for the emergency physicians, to recognize the typical ECG findings of Wellens' Syndrome, because these characteristic ECG findings are considered as a marker for critical LAD occlusions.
Keywords: Wellens' Syndrome, LAD occlusion, Wellens', Acute MI
1. Introduction
Wellens' Syndrome first described by de Zwaan1 in 1982 is the characteristic T wave inversions indicating left anterior descending arterial (LAD) occlusion determined at chest derivations. Identifying the syndrome carries significant diagnostic any prognostic value. Because typical electrocardiographic (ECG) symptoms refer to critical occlusion of LAD and the patients with Wellens' Syndrome generally have acute myocardial infarction (MI) in a week and the risk of sudden cardiac arrest is respectively high.1
2. Case reports
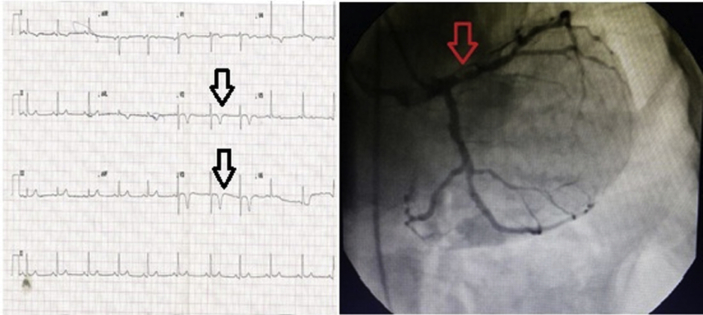
Case 1: A 65 year old female patient admitted to emergency department with the complaint of typical, pressure like chest pain lasting for about 7 h. She had type 2 diabetes mellitus (DM) and hypertension (HT). Physical examination and ECG results were interpreted as normal. She was expressing that the severity of the pain was gradually decreasing. On ECG which was taken two hours later, in the painless period, T wave inversions were seen in the leads V2 and V3. Troponin I was found as 0.06 ng/mL (0–0.04 ng/mL). The echocardiography (ECHO) demonstrated hypokinetic apex. The patient was brought to angiography laboratory immediately and 90–95% LAD occlusion was observed. The patient was discharged from the hospital without any complication after angiographic intervention (Fig. 1).
Fig. 1.
Type A Wellens' Syndrome: symmetrical T waves on ECG and 90–95% occlusion in LAD.
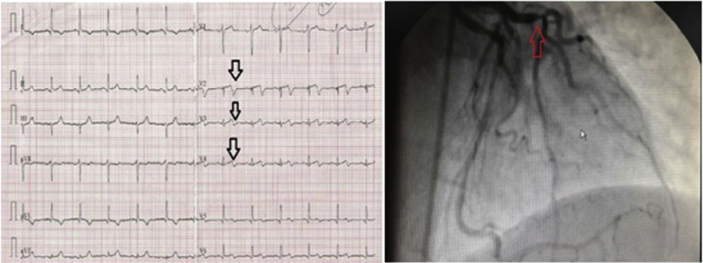
Case 2: A 63 year old female patient admitted to emergency department with the compliant of intermittent chest pain lasting for two days. The pain was located at the mid-thoracic region and was aggravated with movement. The patient was also describing exertional dyspnea. She had type 2 DM and HT. ECG taken at painless period showed biphasic T waves at V2–4. Troponin I was found as 1.28 ng/mL. Immediate angiography was done and occlusions were observed at the right coronary artery, circumflex artery and LAD. Balloon dilatation was applied to the critically occluded LAD and the patient was discharged from the hospital without any complication (Fig. 2).
Fig. 2.
Type B Wellens' Syndrome: biphasic T waves on ECG and critical stenosis in LAD.
3. Discussion
T wave inversion is the most common ECG finding on the patients who are evaluated for the possible acute coronary syndrome in the emergency department (30%) and generally interpreted as nonspecific ST-T deviations.2 Negative T waves caused by ischemia are symmetrical and deep. The other pathologies which are leading to negative T waves are MI (with or without ST elevation), myocarditis, pulmonary embolism, left ventricular hypertrophy, Wolf-Parkinson-White Syndrome, Juvenile T wave pattern and digitalis effect. Biphasic T wave is such a wave that has two components starting with a positive wave which is then passing below the isoelectric line. It is more specific for MI than the rest of the pathologies leading to negative T waves and should be alarming for emergency physicians.3, 4
Wellens' Syndrome refers to the two different types of T wave pattern that are seen at the painless period. In Type A, which is the commonest form (75%), there are deep negative T waves in leads V2 and V3 as in our first case. In type B (25%), there are biphasic T waves typically observed in V2 and V3 as we have seen in our second case. This type of T wave deviations can also be observed in the other precordial leads depending on the proximity of the lesion in the associated artery. In addition to the T wave deviations in V2–3, there might be some extra findings in V4 (three out of four cases) and in V1 (two out of three cases). Studies also showed that these variances also might be seen in leads V5–V6 even the possibility is rare.1 Positive T waves and mild ST elevations are expected with pain. The character of the chest pain might be in the form of typical or atypical angina. The criteria of the syndrome which was defined according to the ECG changes and the clinical findings are summarized at Table 1.5, 6
Table 1.
Clinical and electrocardiographic diagnostic criteria of Wellens' Syndrome.
|
| or |
|
| and |
|
|
|
|
|
de Zwann and colleagues1 examined the ECG results of the 145 patients who were excepted as unstable angina patients in 1982. They described the T wave deviations which were observed in the 26 of the patients (18%) as characteristic for the syndrome. Among these patients 16 were decided to be followed up conservatively only with medication. They discovered anterior MI in a few weeks in 12 of these 16 patients. They concluded that the patients who had typical ECG findings described above should necessitate an immediate invasive treatment. In 1983 Haines and colleagues7 found out similar results in another study.
These ECG findings were described as Wellens' Syndrome by a lot of authors. In 1980 Gerson and Mc Henry8 studied the ECG findings of 760 patients who underwent angiography. They defined the similar findings in the leads DI, AVL and V4–6 as negative U waves. There were 27 patients with the defined negative U wave in their study. Eighty nine percent of these 27 patients had critical occlusions in LAD or left main artery similar to the lesions described in the de Zwann's study. They also reported 80% of the patients had also left ventricular dysfunction.
Although there are some management strategies for the Wellens' Syndrome in the literature there is not any clinical suggestion for the syndrome in the recent guidelines. Stress tests were not recommended for the patients with typical Wellens' Syndrome due to the possibility of a critical occlusion in the emergency department.9 Medical treatment was shown to be unsatisfactory for the prevention of the mortality and morbidity. Invasive angiographic intervention is advised for definitive treatment.1 In our patients presented in this report, immediate angiography was applied and critical LAD occlusions observed in both of the cases. They were managed without any complication before an overt MI happens.
Another debate about the subject is that, the necessity of the advanced diagnostic tests for the patients who have characteristic Wellens' Syndrome findings on their routine ECG examinations without angina symptoms. There are not any standardized rules described for the emergency physicians and the cardiologist, in the management of the patients with typical ECG findings who do not have any chest pain admitted to emergency department or the outpatient clinics. However we thought that it might be necessary to progress with advanced diagnostic methods other than the stress tests, especially in patients with type B Wellens' Syndrome. Because in the formation of biphasic T waves seen in type B, another reason in the etiology likely to be very low, except ischemia.
4. Conclusion
Although there are some management strategies for the Wellens' Syndrome in the literature there is not any clinical suggestion for the syndrome in the recent guidelines. However, it is important for the emergency physicians, to recognize the characteristic ECG findings which may be a warning signal for a critical LAD lesion that can result in acute MI and sudden death in a week.
Footnotes
Peer review under responsibility of The Emergency Medicine Association of Turkey.
References
- 1.de Zwaan C., Bär F.W., Wellens H.J. Characteristic electrocardiographic pattern indicating a critical stenosis high in left anterior descending coronary artery in patients admitted because of impending myocardial infarction. Am Heart J. 1982;103:730–736. doi: 10.1016/0002-8703(82)90480-x. [DOI] [PubMed] [Google Scholar]
- 2.Mead N.E., O'Keefe K.P. Wellen's Syndrome: an ominous EKG pattern. J Emerg Trauma Shock. 2009;2:206–208. doi: 10.4103/0974-2700.55347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rhinehardt J., Brady W.J., Perron A.D., Mattu A. Electrocardiographic manifestations of Wellens' Syndrome. Am J Emerg Med. 2002;20:638–643. doi: 10.1053/ajem.2002.34800. [DOI] [PubMed] [Google Scholar]
- 4.Haines D.E., Raabe D.S., Gundel W.D., Wackers F.J. Anatomic and prognostic significance of new T wave inversion in unstable angina. Am J Cardiol. 1983;52:14–18. doi: 10.1016/0002-9149(83)90061-9. [DOI] [PubMed] [Google Scholar]
- 5.Gerson M.C., McHenry P.L. Resting U wave inversion as a marker of stenosis of the left anterior descending coronary artery. Am J Med. 1980;69:545–550. doi: 10.1016/0002-9343(80)90465-9. [DOI] [PubMed] [Google Scholar]
- 6.Lindsell C.J., Anantharaman V., Diercks D. The Internet Tracking Registry of Acute Coronary Syndromes (i*trACS): a multicenter registry of patients with suspicion of acute coronary syndromes reported using the standardized reporting guidelines for emergency department chest pain studies. Ann Emerg Med. 2006;48:666–677. doi: 10.1016/j.annemergmed.2006.08.005. [DOI] [PubMed] [Google Scholar]
- 7.Tandy T.K., Bottomy D.P., Lewis J.G. Wellens' Syndrome. Ann Emerg Med. 1999;33:347–351. doi: 10.1016/s0196-0644(99)70373-2. [DOI] [PubMed] [Google Scholar]
- 8.Brady W.J., Harrigan R.A., Chan T.C. Acute coronary syndrome. In: John A., Marx M.D., editors. Rosen's Emergency Medicine Concepts and Clinical Practice. 7th ed. Mosby; Philadelphia: 2010. pp. 947–983. [Google Scholar]
- 9.Tatli E., Aktoz M. Wellens' Syndrome: the electrocardiographic finding that is seen as unimportant. Cardiol J. 2009;16:73–75. [PubMed] [Google Scholar]