Abstract
Nursing home (NH) patients have a high prevalence of delirium risk factors, experience 2-4 acute medical conditions (e.g., infections) each year, and have an incidence of delirium during these conditions that is similar to that of hospitalized older adults. Many NH patients with delirium do not return to their prior level of cognitive function. As compared to those without delirium, they are more likely to die, be hospitalized, and less likely to be discharged home. Research on the prevention or treatment of delirium in the NH remains limited. This article describes the development and pilot-testing of a multicomponent delirium prevention intervention in the NH setting adapted from the Hospital Elder Life Program (“HELP-LTC”). We developed delirium-risk reducing activities appropriate for functionally-impaired NH patients that were delivered during treatment for and recovery from acute illness, a novel patient targeting approach. Activities were provided by an expertly trained certified nursing assistant (CNA) who visited patients throughout the facility. We report on incident delirium, delirium remission, cognitive and physical function change, hospitalization, and death associated with acute medical conditions as ascertained by a program coordinator. We also report on the integration and acceptance of the CNAs’ activities by patients and staff. Hospitalization and death were ascertained in a non-intervention comparison group. Findings support a test of the intervention in a controlled trial. The potential impact is great: there are approximately 1.4 million NH patients in the U.S. and an estimated 1 million with dementia or cognitive impairment, a key delirium risk factor. An intervention would be broadly adoptable if the cost of the program’s CNAs were offset by a reduction in health care costs through prevention of hospitalization.
Keywords: nursing homes, delirium, nosocomial infection, intervention
INTRODUCTION
Infections and other acute conditions are common in nursing home residents, occurring 2-4 times per resident per year.1 At least three-quarters of these are managed in the nursing home by the unit nursing staff and primary provider.2 Nursing home residents with acute conditions are at risk for delirium because of the near universal presence of multiple risk factors (e.g., cognitive impairment, immobility, sensory impairment, and neuropsychiatric medication use).3 In one study, delirium was present in 16% of patients at the time of nursing home admission.4 In another, delirium occurred during 18% of acute conditions in nursing home residents and appeared a median of 3 days after condition onset.5 Despite this, few interventions exist for delirium prevention or treatment in the nursing home in part because of long lengths of stay and under-recognition by nursing home staff.6
The objective of this study was to determine the feasibility of an innovative approach to reduce delirium and improve outcomes of acute illness in long-term nursing home residents. We chose the Hospital Elder Life Program (HELP)7 as a model for a novel program (“HELP-LTC”) that delivers delirium-risk-reducing components in the nursing home via a mobile Certified Nursing Assistant (CNA) collaborating with the resident’s primary medical and nursing team and a geriatrician program director. Innovative aspects of this intervention highlighted in this report are: 1) training and employment of a dedicated, mobile CNA to deliver the intervention to residents throughout the facility, 2) initiating the intervention at the time of onset of acute illness by case-finding and referral, 3) delivery of delirium-prevention components to individuals with moderate-to-severe physical and cognitive impairment, and 4) discontinuing the intervention after illness recovery. We report on an 18 month study (February 2013 – July 2014) implementing this intervention at an urban nursing home, describe participating residents and their outcomes, and describe the intervention’s acceptance by residents and staff.
METHODS
Model
We chose HELP as a model for our intervention because studies show that adaptations to HELP can be made across multiple domains, including enrollment criteria, screening and assessment tools, and intervention protocols, while remaining effective.8 We selected intervention components that had evidence to support their use in ameliorating delirium risk factors that were highly prevalent in nursing home residents, including cognitive impairment,3 immobility,7,9 dehydration,7,9,10 malnutrition,11 and sleep problems.7 We chose to employ a CNA to deliver HELP-LTC because CNAs have the skills and knowledge to deliver HELP components and they can be drawn from a large available nursing home workforce pool. We trained the CNAs for 16 hours over 2 weeks (i.e., 4 sessions of 4 hours each, each session consisting of 1 hour of didactic followed by 3 hours of demonstration, practice, and observation), after which they were able to work in their new role independently.
Participants
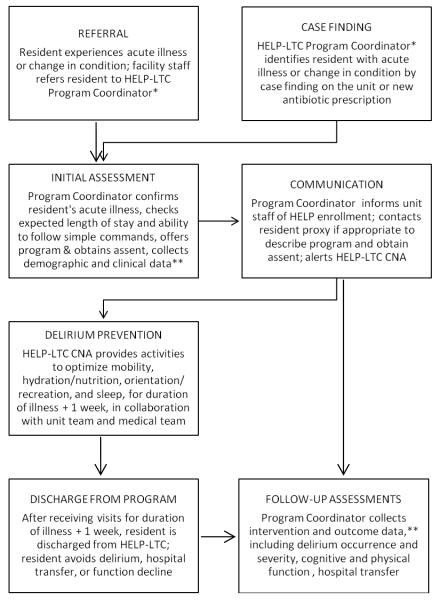
Our targeting approach was to identify nursing home residents at onset of acute illness by referral and case-finding (Figure). Residents on 17 long-term care units at an 816-bed academic urban nursing home who had new acute illnesses were referred to a coordinator by unit-based staff and by a pharmacy query that provided names of residents newly prescribed antibiotics, intravenous fluids, or intravenous medication. A small number of residents were also identified by review of medical and nursing notes for individuals with a significant new diagnosis or who fulfilled change in condition criteria as described in nursing home guidelines.12 Exclusion criteria were: 1) anticipated nursing home stay less than 2 months (i.e., post-acute patients who receive rehabilitation services that overlap with HELP-LTC components), 2) receiving hospice care (since intervention activities could be a burden to residents with comfort care priorities), 3) nonverbal or unable to participate in any intervention activities, or 4) declined participation. In Building 1 (11 units) eligible residents were offered the HELP-LTC intervention. In Building 2 (6 units) residents with acute illness were enrolled using the same methods but did not receive the intervention. We received Jewish Home Lifecare human subjects approval to implement program activities with assent rather than written consent, since the intervention required implementation within 1-2 days of acute illness onset and was minimal risk.
Figure 1. HELP-LTC Referral and Flow.
*In this pilot, the Program Coordinator position was a grant-supported staff person. In actual practice the Program Coordinator’s responsibilities could be performed by the HELP-LTC CNA, a nurse manager (e.g., infection control nurse), or other management staff.
**In this pilot, the Program Coordinator collected data from patient, staff, and medical record during the program and after discharge. However, it would be possible to demonstrate program impact from collecting data just from the medical record after discharge.
Intervention
For residents enrolled in the program, CNA visits occurred 7 days per week for the duration of the illness and 1 week following illness end. The CNA provided intervention components (Table) daily guided by structured protocols and a visit form. A typical visit lasted 30 minutes and began with an orientation activity followed by provision of water, a reminiscence activity or game, a physical exercise, and a snack and second cup of water. Patients who reported sleep difficulty received an evening relaxation visit with a hand or foot massage, quiet music and a warm drink. All HELP-LTC CNA visits were designed to avoid overlap with unit staff’s daily nursing activities, and the CNA communicated with the unit staff regularly to tailor activities and ensure safety (e.g., swallowing and mobility safety). During weekly staff meetings residents were seen with a geriatrician program director and discussed with the primary medical and nursing team as needed. We aimed for a daily CNA caseload of 8 residents.
Table 1.
HELP-LTC intervention components* (N= 231 cases of acute illness and 3671 CNA visits).
| Component | Delirium Risk Factor |
Staffing | Description and Timing | Imple- mented |
Reasons not Implemented |
|---|---|---|---|---|---|
| Orientation | Cognitive Impairment |
HELP CNA | Day, month, year, season, and place reviewed using props; hearing aids and glasses provided; daily |
97% | 2.3% off floor or unavailable; 0.5% not enough time |
| Therapeutic activity |
Cognitive Impairment |
HELP CNA | Discussion of past using resident’s own or other pictures; reading, music, games w/props; daily |
97% | 2.3% off floor or unavailable; 0.5% not enough time; 0.4% refused |
| Mobilizatio n |
Immobility | HELP CNA in collaboration w/physical therapist & unit CNA |
“Head-to-toe” physical activity at resident’s max ability, including active range of motion,walking, chair stands; daily |
84% | 12.9% refused; 2.4% off floor or unavail; 0.6% not enough time; 0.4% medical reason |
| Hydration | Dehydration | HELP CNA in collaboration w/unit CNA & RN |
Two 6-ounce cups of fluid orally unless not indicated (e.g., congestive heart or renal failure or at risk for fluid overload); daily |
90% | 6.4% refused; 0.8% medical reason; 2.4% off floor or unavailable; 0.6% not enough time |
| Snack | Under- nutrition |
HELP CNA in collaboration w/unit CNA and RN |
Yogurt or nutritional shake unless within 15 min before or after a meal; daily |
76% | 19% refused; 0.9% medical reason; 3.3% off floor or unavailable; 0.8% not enough time |
| Sleep or relaxation |
Sleep problems; Medications |
HELP CNA | Massage, warm drink, quiet music for those who report sleep difficul- ties; daily in PM |
85% | 10.1% off floor or unavailable; 3.7% not enough time; 1.5% refused |
| Medication alerts |
Medications | Automated w/MD oversight |
Computerized alerts to medical staff of prescribed meds associated with delirium |
Not imple- mented |
-- |
Adapted with permission from the Hospital Elder Life Program <www.hospitalelderlifeprogram.org>
Measurements
We collected data on resident demographic and clinical characteristics, characteristics of the acute illness, delirium risk factors, and hospital use. The program coordinator was trained to use the Confusion Assessment Method (CAM),13 to ascertain incident delirium while residents received the HELP-LTC program. Delirium severity was ascertained using the Delirium Index (DI), which is a weighted count of delirium features.14 Physical and cognitive function were determined using the nursing home Minimum Data Set (MDS) Activities of Daily Living (ADL) scale15 and the Brief Interview of Mental Status (BIMS),16 respectively, at onset and end of intervention activities. We conducted semi-structured interviews with residents and staff to ascertain acceptability of and satisfaction with the program.
Analyses
Characteristics of residents and their acute illnesses were summarized using descriptive statistics. Component implementation was defined as frequency that a CNA recorded that an indicated intervention activity had been delivered, with a pre-stated goal of completion of 75% of indicated interventions. Reliability of delivery was estimated using positive percent agreement.17 Delirium incidence was calculated as the percentage of residents who had CAM-positive delirium (not including sub-syndromal delirium) on any day while receiving the HELP-LTC intervention. Average DI and cognitive and physical function scores at the beginning and end of intervention activities were calculated, and paired t-tests were used to determine significant within group changes in scores. Percentages of residents who experienced hospitalization or death were calculated. Because the trial was not designed to test for significant differences between groups, p values are not presented for between group comparisons All analyses were conducted using SAS software version 9.2 (SAS, Inc, Cary, NC).
RESULTS
HELP-LTC was delivered to 143 long-term care nursing home residents during 231 acute illness episodes over an 18 month period. Sixty-five percent of recipients were female, with an average age of 82 years. At enrollment the mean BIMS score (possible range 0-15; higher=better cognitive function) was 8.9 (± 4.8), indicating moderate cognitive impairment. The mean ADL Score (possible range 0-28; higher=worse physical function) was 19 (± 6.4), indicating extensive need for ADL assistance. The most common illnesses precipitating referral were infections of bladder (33%), skin (20%), and lower respiratory tract (15%).
HELP-LTC CNAs delivered 15.9 (± 6.8) once-daily visits per illness episode with average visit duration of 32.3 (± 13.1) minutes. Among 3671 visits, a cognitive activity was completed in 97%, most often reminiscence, music, and reading activities; a physical activity was completed in 84%, most often walking, chair stands, and range of motion exercises; fluid administration was provided in 90% and a snack in 76%. Among 377 visits when residents were offered a sleep or relaxation visit 86% received it. The most common cause of not receiving a component was resident refusal, followed by resident being off the floor or unavailable (Table). On days when 2 CNAs visited the same resident (n=179) there was a positive percent agreement of 88%, 90%, and 96% for the physical activity, fluid administration, and orientation, respectively, indicating good reliability of delivery of intervention components.17 The average daily resident visit caseload was 6.7 residents.
Delirium was assessed by the coordinator on average 6.1 (± 2.7) times during an acute illness episode (range 1-15), or approximately 3 times per week. Delirium occurred during 18.0% of acute illnesses, and its severity declined over the course of the acute illness. The mean DI score was 3.9 on Day 0 of the acute illness, declining to 2.3 by day 12 (p= 0.033). The mean BIMS score increased from 10.0 to 11.1 from beginning to end of acute illness (p<0.001). The mean ADL score did not change (19.6 vs. 19.7; p=0.936).
Among HELP-LTC residents, 29 (13.2%) were transferred to the hospital and 23 (11.3%) died during the acute illness or within 3 months after discharge from the program. For an exploratory comparison, among 48 non-intervention (Building 2) residents, 23.9% were transferred to the hospital, and 15.4% died during the acute illness or within 3 months after discharge from the program.
Among 28 residents who were capable of providing feedback, 27 had high satisfaction with the intervention and endorsed the value of each intervention component. Among 4 physicians and 13 unit nursing staff, all indicated that communication between unit and HELP-LTC staff was effective and 14 endorsed that work stress was lower with the intervention.
DISCUSSION
In this paper we describe development and implementation of a delirium-prevention intervention for long-term care nursing home residents. The intervention was modeled after HELP, which has been shown to prevent delirium in hospitalized older adults.7 Novel features of the intervention were its delivery to nursing home residents during treatment for and recovery from acute illness and the use of a mobile CNA to provide daily visits targeting delirium risk factors, notably cognition, mobility, hydration, and nutrition. Mobile, dedicated CNAs increased care intensity to nursing home residents during acute illness -- at a time of greater need. This flexibility has precedence in the nursing home setting in such roles as CNA rehabilitation or oral care specialists or recreation therapists. During high-activity periods we reduced the amount of time the CNA spent with each resident so that they could still visit each resident at least once daily. We think that the intervention could work with a CNA who shared HELP-LTC duties with other duties as long as residents at high risk for delirium (i.e., experiencing an acute illness) were provided HELP-LTC services at least once daily.
In the current nursing home staffing model it is challenging for unit-based nursing staff -- in a fixed staff-to-resident ratio -- to provide the level of additional care (30-60 minutes of additional time daily) likely needed to prevent delirium. We found that unit-based staff approved of the design of HELP-LTC and endorsed having lower stress levels associated with the intervention. This has implications for improving job satisfaction and overall staff turnover in the nursing home setting. Our HELP-LTC CNAs frequently spoke of the benefit of functioning in a new role that provided more role independence and an opportunity to provide services that went beyond custodial care, which was a big incentive for them to participate in this pilot project. The HELP-LTC CNA role could be a new nursing home workforce position that could provide a career advancement track for CNAs or other nursing home staff.
A strength of this project was the careful design of the intervention with input from content experts and front-line providers in an under-studied area. A Cochrane review18 identified only 2 prior prevention trials in nursing homes: one small study (n=98) of a hydration intervention that showed no reduction in delirium,10 and one of a medication reduction intervention that reduced “potential” delirium by 58%.19 Among the few nursing home delirium treatment trials, a multi-factorial intervention that was designed to be delivered by existing nursing home staff to delirious post-acute nursing home patients was not effective in shortening delirium or reducing its severity.20 Our study findings suggest that our intervention ameliorated delirium severity and resulted in individuals being able to retain their baseline cognitive function after acute illness.
A key limitation of this study is that it was not designed to test effectiveness because there was not a formal comparison group. The delirium incidence of 18.0% is similar to our previous study5 which found a delirium incidence of 17.7% in acutely ill long-term care residents. Second, the intervention is designed with dedicated CNA staffing, which could be a resource barrier in many nursing facilities. However, if the intervention prevented hospital transfer, it could lower healthcare costs and be cost-effective despite the extra staffing required. Third, this program was implemented at single, large facility affiliated with an academic institution which may limit the general applicability of the findings. Finally, future iterations should consider including medication review for drugs associated with delirium, with provider alerting to increase the potential impact of the intervention.
Delirium is reported to be an uncomfortable and traumatic experience by those who have experienced it and for family witnesses. The new HELP-LTC program is feasible and consistent with CMS initiatives to develop and implement improvements in nursing homes, which opens up potential for broad adoption and potential impact on nursing home resident health and experience.
ACKNOWLEDGMENTS
Financial Support: Financial support for the study was provided by Fan Fox and Leslie R. Samuels Foundation, National Institute on Aging (P30 AG028741; K07AG041835), Jewish Home Lifecare Parkinson’s Research Fund and the Hospital Elder Life Program (HELP). Dr. Boockvar is supported by the Greenwall Foundation. Dr. Inouye holds the Milton and Shirley F. Levy Family Chair. This work was supported with resources and the use of facilities at the James J. Peters VA Medical Center, Bronx, NY. The contents do not represent the views of the U.S. Department of Veterans Affairs or the United States Government.
We gratefully acknowledge the contributions of the following individuals: Carole Michelsen, MD, (conception and design), Nancy Brooks, RN, NP, (conception and design), Carole Smyth, NP, (conception and design, acquisition of data), Liang Wen, NP, (conception and design, acquisition of data), Sarah Dowal, RN (conception and design), James Judge, MD, (conception and design), Vivian Guerrero, (acquisition of data), Jeanette Torres, (acquisition of data), Kuana Beckford, (acquisition of data), Onie Manzano, (analysis of data), Joseph Eimicke, (analysis of data), Stephanie Silver , (acquisition of data), Daniel Signor, (analysis of data), Daniel Sun, (acquisition of data), Eve Gottesman (analysis of data).
Sponsors’ Role: The sponsors had no role in the design, methods, subject recruitment, data collections, analysis or preparation of this paper.
Footnotes
Presented in part at the 2013, 2014, and 2015 American Geriatrics Society Annual Scientific Meeting and at the 2013 and 2014 International HELP Conference.
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper.
Author Contributions: Kenneth S. Boockvar (conception and design, acquisition of data, analysis and interpretation of data; drafting the article and revising it critically for important intellectual content); Jeanne A. Teresi (conception and design, analysis and interpretation of data; revising article critically for important intellectual content); Sharon K. Inouye (conception and design, analysis and interpretation of data; revising article critically for important intellectual content)
REFERENCES
- 1.Alessi CA, Harker JO. A prospective study of acute illness in the nursing home. Aging (Milano) 1998;10:479–489. doi: 10.1007/BF03340162. [DOI] [PubMed] [Google Scholar]
- 2.Boockvar KS, Gruber-Baldini AL, Burton L, et al. Outcomes of infection in nursing home residents with and without early hospital transfer. J Am Geriatr Soc. 2005;53:590–596. doi: 10.1111/j.1532-5415.2005.53205.x. [DOI] [PubMed] [Google Scholar]
- 3.Inouye SK, Charpentier PA. Precipitating factors for delirium in hospitalized elderly persons. Predictive model and interrelationship with baseline vulnerability. JAMA. 1996;275:852–857. [PubMed] [Google Scholar]
- 4.Kiely DK, Bergmann MA, Murphy KM, et al. Delirium among newly admitted postacute facility patients: Prevalence, symptoms, and severity. J Gerontol A Biol Sci Med Sci. 2003;58:M441–445. doi: 10.1093/gerona/58.5.m441. [DOI] [PubMed] [Google Scholar]
- 5.Boockvar K, Signor D, Ramaswamy R, et al. Delirium during acute illness in nursing home residents. J Am Med Dir Assoc. 2013;14:656–660. doi: 10.1016/j.jamda.2013.06.004. [DOI] [PubMed] [Google Scholar]
- 6.Fick DM, Kolanowski AM, Hill NL, et al. Using standardized case vignettes to evaluate nursing home staff recognition of delirium and delirium superimposed on dementia. Ann LongTerm Care. 2013;21 [PMC free article] [PubMed] [Google Scholar]
- 7.Inouye SK, Bogardus ST, Jr., Charpentier PA, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999;340:669–676. doi: 10.1056/NEJM199903043400901. [DOI] [PubMed] [Google Scholar]
- 8.Chen CC, Chen CN, Lai IR, et al. Effects of a Modified Hospital Elder Life Program on Frailty in individuals undergoing major elective abdominal surgery. J Am Geriatr Soc. 2014;62:261–268. doi: 10.1111/jgs.12651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Voyer P, Richard S, Doucet L, et al. Predisposing factors associated with delirium among demented long-term care residents. Clin Nurs Res. 2009;18:153–71. doi: 10.1177/1054773809333434. [DOI] [PubMed] [Google Scholar]
- 10.Culp K, Mentes J, Wakefield B. Hydration and acute confusion in long-term care residents. West J Nurs Res. 2003;25:251–73. doi: 10.1177/0193945902250409. [DOI] [PubMed] [Google Scholar]
- 11.Culp KR, Cacchione PZ. Nutritional status and delirium in long-term care elderly individuals. Appl Nurs Res. 2008;21:66–74. doi: 10.1016/j.apnr.2006.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Levenson S, Vance J, editors. Protocols for Physician Notification: Assessing Patients and Collecting Data on Nursing Facility Patients. American Medical Directors Association; Columbia, Maryland: 2004. [Google Scholar]
- 13.Inouye SK, van Dyck CH, Alessi CA, et al. Clarifying confusion: The confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113:941–948. doi: 10.7326/0003-4819-113-12-941. [DOI] [PubMed] [Google Scholar]
- 14.McCusker J, Cole MG, Voyer P, et al. Environmental factors predict the severity of delirium symptoms in long-term care residents with and without delirium. J Am Geriatr Soc. 2013;61:502–511. doi: 10.1111/jgs.12164. [DOI] [PubMed] [Google Scholar]
- 15.Morris JN, Fries BE, Morris SA. Scaling ADLs within the MDS. J Gerontol A Biol Sci Med Sci. 1999;54:M546–553. doi: 10.1093/gerona/54.11.m546. [DOI] [PubMed] [Google Scholar]
- 16.Chodosh J, Edelen MO, Buchanan JL, et al. Nursing home assessment of cognitive impairment: Development and testing of a brief instrument of mental status. J Am Geriatr Soc. 2008;56:2069–2075. doi: 10.1111/j.1532-5415.2008.01944.x. [DOI] [PubMed] [Google Scholar]
- 17.Cicchetti DV, Feinstein AR. High agreement but low kappa: II. Resolving the paradoxes. J Clin Epidemiol. 1990;43:551–558. doi: 10.1016/0895-4356(90)90159-m. [DOI] [PubMed] [Google Scholar]
- 18.Clegg A, Siddiqi N, Heaven A, et al. Interventions for preventing delirium in older people in institutional long-term care. Cochrane Database Syst Rev. 2014;1:CD009537. doi: 10.1002/14651858.CD009537.pub2. [DOI] [PubMed] [Google Scholar]
- 19.Lapane KL, Hughes CM, Daiello LA, et al. Effect of a pharmacist-led multicomponent intervention focusing on the medication monitoring phase to prevent potential adverse drug events in nursing homes. J Am Geriatr Soc. 2011;59:1238–1245. doi: 10.1111/j.1532-5415.2011.03418.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marcantonio ER, Bergmann MA, Kiely DK, et al. Randomized trial of a delirium abatement program for postacute skilled nursing facilities. J Am Geriatr Soc. 2010;58:1019–1026. doi: 10.1111/j.1532-5415.2010.02871.x. [DOI] [PMC free article] [PubMed] [Google Scholar]