Abstract
Normal and limited vision gait was investigated in individuals with Parkinson disease (PD), healthy older and healthy young individuals. Participants walked a GAITRite mat with normal vision or vision of lower limbs occluded. Results indicate individuals with PD walked more slowly, with shorter and wider steps and spent more time in double support with limited vision as compared to full vision. Healthy young and old individuals took shorter steps but were otherwise unchanged between conditions.
Keywords: Parkinson Disease, Proprioception, Gait
1 INTRODUCTION
Parkinson disease (PD) affects as many as one million Americans, making it the second most common neurodegenerative disorder (de Lau & Breteler, 2006). In addition to the four cardinal symptoms (postural instability, resting tremor, bradykinesia, and rigidity) PD is associated with a host of secondary symptoms including depression (Zesiewicz, Gold, Chari, & Hauser, 1999), cognitive impairment (Hely, Reid, Adena, Halliday, & Morris, 2008), sleep disorders (Kumar, Bhatia, & Behari, 2002), olfactory dysfunction (Doty, Bromley, & Stern, 1995) and decreased proprioceptive and kinesthetic sensitivity (for review see Konczak et al., 2009). These secondary symptoms are often debilitating and frequently reduce quality of life.
Proprioception, the awareness of one’s limbs in space (Konczak et al., 2009), and kinesthesia, the conscious perception of limb orientation and motion (Maschke, Tuite, Pickett, Wachter, & Konczak, 2005), allow for skillful motor performance even in the absence of vision (Konczak et al., 2009). Proprioceptive and kinesthetic deficits affect coordination and motor control of the proximal joints due to a lack of awareness of limb location. Individuals with PD may have decreased proprioception and kinesthesia (Maschke, Gomez, Tuite, & Konczak, 2003). These systems are so sensitive in healthy adults that position changes of as little as 0.2 degrees in proximal joints can be correctly perceived (Maschke et al., 2003). In contrast, Konczak et al. (2007) noted that when individuals with PD experienced passive rotation of the elbow, they had more difficulty than controls in detecting position change. This impaired perception was reflected by the need for a greater angular displacement or duration of movement prior to correct detection of movement direction. In addition, individuals with PD experience a reduced ability to detect changes in limb weight or load, thus requiring more pressure to sense heaviness (Maschke, Tuite, Krawczewski, Pickett, & Konczak, 2006). These deficits can also affect active movement. Adamovich et al. (2001) noted that individuals with PD were much less accurate when attempting to point to a visible target when their vision of their arm was occluded. During tasks involving whole body reaching, individuals with PD made smaller center of mass adjustments when pointing to a target with eyes closed (Tagliabue, Ferrigno, & Horak, 2009). Similar results were noted during stepping to a target without vision of the legs; PD patients took shorter steps and had reduced accuracy, resulting in undershooting the target (Jacobs & Horak, 2006). Impaired proprioception may negatively impact the ability of individuals with PD to coordinate movements in the absence of vision.
Although there are known differences in proprioception between healthy individuals and those with PD, the impact of these differences on gait is still being explored. Almeida and colleagues (2005) noted that individuals with PD and age-matched controls both exhibited decreased velocity and stride length with increased stride width when walking in a dark room. This suggests a similar strategy was used by each group to adapt to the low vision condition. However this work focused on gait in a situation where vision is completely removed not just occluded in a manner that prevents compensation for proprioception deficits. That is, vision was limited in its entirety rather than limited in a plane that prevents viewing of the feet and floor.
Individuals with PD are known to have an increased reliance on visual information to guide their movements. Dependence on visual feedback is evident in the effectiveness of ground lines in improving gait in individuals with PD. Azulay and colleagues (1999) used evenly spaced lines on the floor to examine stride length and velocity in individuals with PD. They noted that the presence of visual targets increased stride length and gait velocity during preferred speed overground walking. The cause of this effect is not clear. One of the proposed mechanisms relating to the neuropathology of PD includes a shift of the control of walking to an attentional mechanism thus allowing damaged neural pathways to be bypassed (Vitorio et al., 2012). Other theories include improvement due to strengthened optic flow (Vitorio et al., 2012), or lines facilitating visual compensation for weakened proprioception (Lebold & Almeida, 2011).
Impaired gait in PD can lead to falls and limit an individual’s ability to carry out daily tasks, leading to a loss of independence (Morris, Iansek, Matyas, & Summers, 1994) and decreased quality of life (Earhart, 2009; Kleiner-Fisman, Gryfe, & Naglie, 2013). As compared to healthy individuals of the same age, altered gait has been repeatedly reported in individuals with PD who often show reduced stride length, reduced gait velocity, and smaller step amplitude (Earhart & Williams, 2012; Vitorio et al., 2012). Additionally, people with PD move the pelvis and thorax together, while healthy individuals move the pelvis and thorax out of phase during walking. Gait in PD is also marked by increased flexion of hips and knees compared to healthy individuals (Morris, Huxham, McGinley, Dodd, & Iansek, 2001).
To fully understand how gait is altered in PD we must also understand characteristics of healthy gait change throughout the lifespan. For example, walking without vision leads to age-specific gait adaptations such as a larger increase in postural sway in children compared to adults. Increased postural sway and shorter stride length are present in all age groups during walking without vision (Hallemans et al., 2009). In childhood, vision plays an especially important role, and in its absence, vestibular and proprioceptive information cannot fully compensate. This may be due in part to a proprioceptive sense that is not yet fully developed (Pickett & Konczak, 2009). As individuals age, they develop increasingly effective strategies for walking without vision, reducing postural sway in no or limited vision conditions until mature adaptations are achieved at roughly age 11 (Hallemans et al., 2009). Gait speed tends to decline with age (Schrack, Simonsick, & Ferrucci, 2010), and processing of sensory information may change (Chaput & Proteau, 1996). Therefore, in order to fully understand the relationship between proprioception and gait throughout the lifespan, an examination of gait between young and older individuals is necessary.
The goal of this pilot study was to investigate the role of vision on gait in individuals with PD as compared to both healthy older and healthy young participants. We observed gait in two conditions: vision (normal vision) and limited vision (vision of the body was occluded but visual feedback from the surrounding environment was intact). We hypothesized that individuals with PD would be more reliant on vision and as a result would demonstrate changes in gait parameters related to stability such as widening base of support, shorter stride length, and decreased gait velocity from the vision to the limited vision condition. We predicted that the healthy young and healthy older adult groups would perform similarly to a reduction of vision, and be less affected or not affected at all by the change in visual condition.
2 METHODS
2.1 Participants and Recruitment
Twenty-five individuals with idiopathic PD, 17 age-matched healthy older adults, and 18 healthy young adults completed the study. See Table 1 for subject demographics. Participants with PD were tested in the ‘off’ state, at least twelve hours after their last dose of anti-parkinsonian medication. One individual with PD was removed as his Off state Hoehn and Yahr score was a 4. All other individuals were below 3 or in the mild to moderate stage. Individuals with PD had received a diagnosis of idiopathic PD from a board certified neurologist using previously established criteria (Hughes, Daniel, Kilford, & Lees, 1992; Schaafsma et al., 2003).
Table 1.
Subject Demographics
| Characteristic | Healthy Young (N=18) | Healthy Age- Matched (N=17) | PD (N=25) |
|---|---|---|---|
| Sex (M/F) | 9/9 | 6/11 | 14/11 |
| Age(yrs) | 25.3 ± 2.9 | 68.4 ± 7.5 | 68.9 ± 8.5 |
| UPDRS III | 34.6 ± 15.0 | ||
| Hoehn&Yahr OFF | 2.2 ± 0.5 |
Values are means +/− SDs
Inclusion criteria for all individuals were: 1) ability to walk independently without the use of an assistive device; 2) ability to follow multiple step commands; 3) vision corrected to 20/40 or better; 4) no history of vestibular disease; 5) no evidence of any other serious medical problem; 7) no history or evidence of neurological deficit (other than PD), such as previous stroke or muscle disease; and 8) no history or evidence of orthopedic, muscular, or psychological problem that would interfere with the study.
Healthy young participants were recruited from the Program in Physical Therapy at Washington University School of Medicine. Individuals with PD were recruited from a separate study in the Locomotor Control Laboratory. The age-matched control group was composed primarily of partners and caregivers of individuals with PD. All individuals provided informed written consent in accordance with the procedures approved by the Institutional Review Board of Washington University School of Medicine.
2.2 Materials
A 4.8m instrumented GAITRite walkway system (CIR systems, Inc., Havertown, PA) was used to measure temporal and spatial gait parameters. A vision occlusion collar (VOC) made of stiffened fabric was used to occlude vision of the lower body, periphery and the floor directly in front of the participant (Figure 1). This device was chosen because the open superior surface allowed visual tracking at and above eye level, permitting participant visual feedback to guide their trajectory while restricting vision of the arms, legs and feet.
Figure 1.
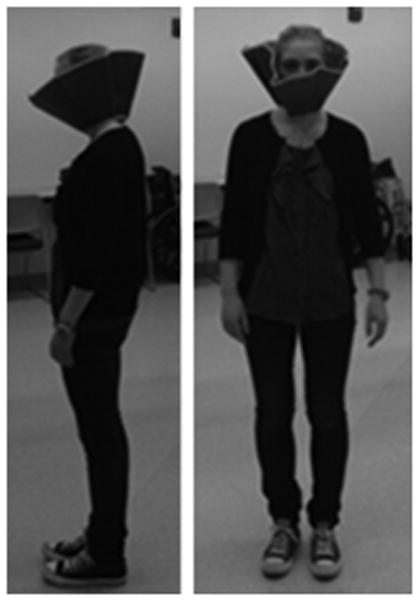
Participant wearing the vision occlusion collar (VOC).
2.3 Procedure
All testing was conducted in the Locomotor Control Laboratory at Washington University School of Medicine. During a single testing session, participants were evaluated under two conditions: vision and limited vision. In both conditions, participants began walking one meter before the GAITRite walkway and continued until completely across and off the mat. Verbal cues signaled participants to begin and end each trial. Participants in both conditions wore their normal athletic shoes. In the vision condition, participants were instructed to walk down the GAITRite walkway at their self-selected pace. In the limited vision condition, participants donned the VOC and traversed the mat at their self-selected pace. Identical instructions “walk down the mat in your normal fashion” were provided for both conditions. The order of the conditions was randomized between subjects, and each condition was repeated ten times per person. Participants were encouraged to rest as often as necessary. Fatigue did not appear to cause difficulty for any participants.
2.4 Data Analysis
The independent variable was vision condition. Dependent variables included: cadence (Cad), steps per minute; normalized gait velocity (NVel), gait velocity normalized to the distance from the head of the femur to the lateral malleolus; average base of support (BoS), the average distance between the left and right heel during gait; normalized step length (NSL), or the length of a step normalized by the length of the lower limb; and average double support time (DSupp), or the period of time when both feet are on the ground. IBM© SPSS© Statistics Version 20 (IBM Corporation, Armonk, New York) was used for statistical analysis. A paired samples t-test was used to compare vision and limited vision conditions within each group, with an a priori alpha value set at 0.05. A paired sample t-test was selected to examine the data for within group differences from the vision to the limited vision condition. This methodology was selected to allow for three vastly different groups to be included in the analysis. A mixed model ANOVA, with post-hoc comparisons would allow for within and between group comparisons but would also be penalized for the large between group variance. As this study is a small sample pilot study, designed to examine these three populations for within group differences, we have elected to use the more liberal approach and report only the within group differences.
3 RESULTS
Demographic data for each group are shown in Table 1. A significant main effect of age was present. A post hoc comparison showed individuals with PD and age-matched controls did not differ in age (p≤0.8298) but, as expected, the health young group was significantly younger than both the age-matched controls (p ≤ 0.01) and the PD group (p ≤ 0.01).
Significant differences between the vision and limited vision conditions were seen in the PD group for nVel (p = 0.035), BoS (p = 0.014), NSL (p ≤ 0.001) and DSupp (p = 0.016). Specifically, individuals with PD walked slower with a wider BoS, shorter steps and spent more time in double support during the limited vision condition. Cadence was not significantly affected by vision for the PD group (p = 0.419).
Only NSL was significantly altered and was shorter for both the healthy young (p = 0.03) and healthy age-matched (p = 0.01) groups in the limited vision condition. Cadence, nVel, BoS and DSupp were not significantly affected by vision for either group (Table 2).
Table 2.
Gait Parameters (Mean +/− SD)
| Cadence (steps/min) | p-value | Normalized Velocity (meters/sec) | p-value | Avg HH Base Support | p-value | Normalized Step Length | p-value | Avg Double Support Time | p-value | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| Healthy Young | V | 109.23 ± 10.99 | 0.108 | 1.51 ± 0.34 | 0.421 | 8.31 ± 2.50 | 0.269 | 0.82 ± 0.11 | 0.025 * | 0.25 ± 0.07 | 0.561 |
|
|
|
|
|
|
|||||||
| NV | 110.89 ± 12.45 | 1.49 ± 0.37 | 8.05 ± 2.10 | 0.80 ± 0.11 | 0.26 ± 0.07 | ||||||
|
| |||||||||||
| Healthy Age-matched | V | 114.31 ± 9.94 | 0.182 | 1.45 ± 0.19 | 0.220 | 9.11 ± 2.59 | 0.118 | 0.76 ± 0.08 | 0.010 * | 0.27 ± 0.05 | 0.631 |
|
|
|
|
|
|
|||||||
| NV | 116.02 ± 9.30 | 1.40 ± 0.22 | 9.43 ± 2.50 | 0.72 ± 0.10 | 0.27 ± 0.05 | ||||||
|
| |||||||||||
| PD | V | 109.99 ± 9.75 | 0.419 | 1.21 ± 0.26 | 0.035 * | 9.50 ± 2.92 | 0.014 * | 0.66 ± 0.12 | 0.001 * | 0.29 ± 0.06 | 0.016 * |
|
|
|
|
|
|
|||||||
| NV | 110.76 ± 11.69 | 1.16 ± 0.31 | 10.12 ± 3.07 | 0.63 ± 0.14 | 0.31 ± 0.08 | ||||||
4 DISCUSSION
The results from our study suggest that when walking with vision of the body occluded but some vision of the surround intact, individuals with PD walk more slowly, spend more time in double support and take shorter and wider steps than when full vision is allowed. Conversely, healthy age matched and healthy young individuals only show reductions in stride length. No changes in cadence were observed for any of the groups. These results support our original hypothesis but are not as robust as we had expected.
Extensive research suggests that proprioception is significantly more impaired in Parkinson disease than in healthy aging (Jacobs & Horak, 2006; Mongeon, Blanchet, & Messier, 2009; Vaugoyeau, Hakam, & Azulay, 2011). Konczak et al (2007) used passive motion of the forearm on a padded splint to examine the ability of individuals with PD to detect passive limb displacement and velocity changes. They reported that individuals with PD had an average of 92–166% longer detection times than controls. Wright et al (Wright et al., 2010) examined passive twisting of the trunk and noted that the threshold for detection was much higher in individuals with PD than in healthy individuals. Furthermore, changes in motor control without vision of the body have also been explored in the context of more active motor tasks. Adamovich et al. (Adamovich et al., 2001) used a pointing task in three different conditions to explore the influences of visual information, proprioceptive feedback, and spatial working memory on the accuracy of individuals with Parkinson disease. They noted that the pointing of individuals with PD was selectively impaired in conditions requiring integration of visual and proprioceptive information. This would suggest that deficits may also be present during gait tasks in PD. The current findings support these conclusions. Our results showed that individuals with PD were significantly affected in four of the five measured gait variables while healthy individuals, both young and older, were significantly impacted only with regard to stride length.
The effect of vision of the body during more complex tasks such as gait has also been investigated, with several other studies suggesting that individuals with PD adapt similarly to healthy individuals when walking without vision of their bodies. Almeida et al. (2005) measured gait and accuracy when walking to a target in light or dark conditions as well as with a light on the chest, on the target and on the chest, or pushed in a wheelchair to the remembered target. Their goal was to examine the relative influence of visual and proprioceptive inputs on locomotion and target accuracy in individuals with PD. They reported that both healthy and PD groups improved accuracy with availability of vision or proprioception, and that individuals with PD were significantly less accurate in conditions requiring them to integrate vision and proprioception than healthy controls. Individuals with PD improved significantly with greater sensory feedback, including with availability of proprioception. This suggests that while proprioception is impaired, it is still providing enough information to facilitate significant gait improvement. While individuals with PD were significantly less accurate at walking to a target with limited sensory information, their gait adaptations in the dark were the same as those noted in healthy controls, with both groups decreasing velocity and step length while increasing double support time. These results suggest that while positioning of body in space to match an external target is impaired, overall gait is fairly intact even in the absence of vision of the body. While our results did not investigate body positioning in space, the results of Almeida et al. may help to explain why the observed changes were smaller than expected. We noted similar adaptations by both healthy groups and individuals with PD in measures of NSL and no significant changes for any group in cadence.
In addition to effects of vision of the body during gait, the effects of vision of the surrounding environment on gait have been investigated. Efficacy of visual cues in improving gait performance in PD suggests an increased reliance on vision, but studies show mixed results. Azulay and colleagues (Azulay et al., 1999) used evenly spaced lines on the floor to examine the effect of visual cues on gait in PD, noting that the presence of visual targets increased stride length and gait velocity during preferred speed overground walking (Azulay et al., 1999). This improvement implies increased dependence on visual information, especially dynamic information. The VOC utilized in the present study allowed for optic flow from the walls or ceiling, and given the increased reliance on vision of individuals with PD, this may have been sufficient to play a part in normalizing gait despite possibly impaired proprioception.
Proprioceptive changes are known to occur with age. Pai (1997) and colleagues assessed the threshold for detection of knee joint displacement in healthy older adults, individuals with osteoarthritis, and healthy young adults. They noted a moderate correlation between joint displacement threshold and age, and a large difference between healthy older adults and older adults with osteoarthritis, correlating with their disease-specific functional status (Pai et al., 1997). Different from what would be predicted by these results, we noted similar performance on gait tasks with and without vision in healthy young and healthy older adults. Both healthy older adults and healthy young adults walked with significantly shorter normalized step length in the limited vision than the vision condition. Aside from NSL, no significant differences were observed for either group between the vision and limited vision conditions. This could be in part because the changes reported by Pai et al. (1997) in proprioception between older and younger adults were very subtle, and these relatively small changes in proprioception may not be of sufficient magnitude to impact the gait parameters we examined. Pai et al. also noted the largest differences in older adults with worse disease-specific functional status due to osteoarthritis, while age-matched controls in our study were all healthy.
While complex gait tasks such as backwards walking or dual task walking are commonly assessed, gait is less commonly assessed with an experimentally induced reduction of sensory input. The VOC could be a simple and inexpensive tool to screen for visual dependence, with a basic test requiring only two pieces of tape, a vision occlusion collar, and a stopwatch. Use of the vision occlusion collar minimizes fall risk by providing some vision of the environment while still enabling measurement of the effects of limited vision on tasks important for everyday function. Given that inadequate light levels are a known contributor to fall risk in independently living older adults (Paul & Yanlong 2012; Reed, Lowrey, & Vallis, 2006), information obtained through use of limited vision screening tools like the VOC could be useful for identifying individuals most at risk for falls in low vision conditions. Walking with vision occluded or removed may be a useful screening tool to evaluate dependence on vision for locomotor control. Those who perform poorly with limited vision could then be directed to therapies designed to assist them in learning to upweight other senses, thereby enhancing safe performance in low light conditions. Finally, as a greater reliance on vision appears to be present in this population, clinicians working with individuals with PD on a regular basis may want to stress the importance of visual testing and use of corrective procedures to ensure the highest possible levels of visual acuity.
4.1 Limitations
Other studies examining vision and gait have occluded vision completely, while the open design of the VOC used in our study did not eliminate optic flow from the walls and ceiling. We designed the VOC in this way so participants could guide movements to remain on the GAITRite walkway, however allowing some visual input rather than completely removing vision may explain the difference between our hypothesis and the observed changes. Additionally, allowing for intact vision of the periphery but not of the floor directly in front of the individuals most certainly altered visuospatial attention. This alteration may allow for altered attentional focus during the gait tasks. For the individuals with PD, this altered attention in conjunction with the proprioceptive deficits may be contributing to the observed effects on gait. In addition, participants in this study had mild to moderate PD and as such may not be impacted by occlusion of vision as much as individuals in a more advanced disease state. Finally, we focused on gross motor changes in gait with normal and limited vision. In the future, it would be interesting to measure the relationship of proprioception to gait more directly. This could be done by conducting both finely graded single joint movement tasks of upper and lower extremity joints and gait tasks with and without vision, allowing direct comparison of an individual’s performance across tasks.
5 CONCLUSIONS
We noted that individuals with PD walked more slowly, spend more time in double support and took shorter and wider steps when vision was occluded than when full vision was allowed. Healthy age-matched and healthy young individuals took shorter steps during the occluded vision condition, but otherwise were not significantly affected. These results suggest that individuals with PD may a reliance on vision during gait while healthy young and older individuals do not.
Acknowledgments
The authors thank April Brown and Daniel Peterson for their help with data collection for this study.
Support for this work was provided by the Parkinson’s Disease Foundation, NIH grants R01NS077595, 2T32HD007434, and TL1RR024995, the American Parkinson Disease Association (APDA) Advanced Center for PD Research at Washington University School of Medicine and the Greater St. Louis Chapter of the APDA.
Footnotes
CONFLICT OF INTERESTS
The authors declare that there is no conflict of interests regarding the publication of this article.
Contributor Information
Laura M. Pilgram, Email: lpqxc@health.missouri.edu.
Gammon M. Earhart, Email: kpickett2@wisc.edu.
Kristen A. Pickett, Email: earhartg@wusm.wustl.edu.
References
- Adamovich SV, Berkinblit MB, Hening W, Sage J, Poizner H. The interaction of visual and proprioceptive inputs in pointing to actual and remembered targets in Parkinson’s disease. Neuroscience. 2001;104(4):1027–1041. doi: 10.1016/s0306-4522(01)00099-9. [DOI] [PubMed] [Google Scholar]
- Almeida QJ, Frank JS, Roy EA, Jenkins ME, Spaulding S, Patla AE, Jog MS. An evaluation of sensorimotor integration during locomotion toward a target in Parkinson’s disease. Neuroscience. 2005;134(1):283–293. doi: 10.1016/j.neuroscience.2005.02.050. [DOI] [PubMed] [Google Scholar]
- Azulay JP, Mesure S, Amblard B, Blin O, Sangla I, Pouget J. Visual control of locomotion in Parkinson’s disease. Brain. 1999;122(Pt 1):111–120. doi: 10.1093/brain/122.1.111. [DOI] [PubMed] [Google Scholar]
- Chaput S, Proteau L. Modifications with aging in the role played by vision and proprioception for movement control. Exp Aging Res. 1996;22(1):1–21. doi: 10.1080/03610739608253994. [DOI] [PubMed] [Google Scholar]
- de Lau LM, Breteler MM. Epidemiology of Parkinson’s disease. Lancet Neurol. 2006;5(6):525–535. doi: 10.1016/S1474-4422(06)70471-9. [DOI] [PubMed] [Google Scholar]
- Doty RL, Bromley SM, Stern MB. Olfactory testing as an aid in the diagnosis of Parkinson’s disease: development of optimal discrimination criteria. Neurodegeneration. 1995;4(1):93–97. doi: 10.1006/neur.1995.0011. [DOI] [PubMed] [Google Scholar]
- Earhart GM. Dance as therapy for individuals with Parkinson disease. Eur J Phys Rehabil Med. 2009;45(2):231–238. [PMC free article] [PubMed] [Google Scholar]
- Earhart GM, Williams AJ. Treadmill training for individuals with Parkinson disease. Phys Ther. 2012;92(7):893–897. doi: 10.2522/ptj.20110471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallemans A, Beccu S, Van Loock K, Ortibus E, Truijen S, Aerts P. Visual deprivation leads to gait adaptations that are age- and context-specific: I. Step-time parameters. Gait Posture. 2009;30(1):55–59. doi: 10.1016/j.gaitpost.2009.02.018. [DOI] [PubMed] [Google Scholar]
- Hely MA, Reid WG, Adena MA, Halliday GM, Morris JG. The Sydney multicenter study of Parkinson’s disease: the inevitability of dementia at 20 years. Mov Disord. 2008;23(6):837–844. doi: 10.1002/mds.21956. [DOI] [PubMed] [Google Scholar]
- Hughes AJ, Daniel SE, Kilford L, Lees AJ. Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: a clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry. 1992;55(3):181–184. doi: 10.1136/jnnp.55.3.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobs JV, Horak FB. Abnormal proprioceptive-motor integration contributes to hypometric postural responses of subjects with Parkinson’s disease. Neuroscience. 2006;141(2):999–1009. doi: 10.1016/j.neuroscience.2006.04.014. [DOI] [PubMed] [Google Scholar]
- Kleiner-Fisman G, Gryfe P, Naglie G. A Patient-Based Needs Assessment for Living Well with Parkinson Disease: Implementation via Nominal Group Technique. Parkinsons Dis. 2013;2013:974964. doi: 10.1155/2013/974964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konczak J, Corcos DM, Horak F, Poizner H, Shapiro M, Tuite P, … Maschke M. Proprioception and motor control in Parkinson’s disease. J Mot Behav. 2009;41(6):543–552. doi: 10.3200/35-09-002. [DOI] [PubMed] [Google Scholar]
- Konczak J, Krawczewski K, Tuite P, Maschke M. The perception of passive motion in Parkinson’s disease. J Neurol. 2007;254(5):655–663. doi: 10.1007/s00415-006-0426-2. [DOI] [PubMed] [Google Scholar]
- Kumar S, Bhatia M, Behari M. Sleep disorders in Parkinson’s disease. Mov Disord. 2002;17(4):775–781. doi: 10.1002/mds.10167. [DOI] [PubMed] [Google Scholar]
- Lebold CA, Almeida QJ. An evaluation of mechanisms underlying the influence of step cues on gait in Parkinson’s disease. J Clin Neurosci. 2011;18(6):798–802. doi: 10.1016/j.jocn.2010.07.151. [DOI] [PubMed] [Google Scholar]
- Maschke M, Gomez CM, Tuite PJ, Konczak J. Dysfunction of the basal ganglia, but not the cerebellum, impairs kinaesthesia. Brain. 2003;126(Pt 10):2312–2322. doi: 10.1093/brain/awg230. [DOI] [PubMed] [Google Scholar]
- Maschke M, Tuite PJ, Krawczewski K, Pickett K, Konczak J. Perception of heaviness in Parkinson’s disease. Mov Disord. 2006;21(7):1013–1018. doi: 10.1002/mds.20876. [DOI] [PubMed] [Google Scholar]
- Maschke M, Tuite PJ, Pickett K, Wachter T, Konczak J. The effect of subthalamic nucleus stimulation on kinaesthesia in Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2005;76(4):569–571. doi: 10.1136/jnnp.2004.047324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mongeon D, Blanchet P, Messier J. Impact of Parkinson’s disease and dopaminergic medication on proprioceptive processing. Neuroscience. 2009;158(2):426–440. doi: 10.1016/j.neuroscience.2008.10.013. [DOI] [PubMed] [Google Scholar]
- Morris ME, Huxham F, McGinley J, Dodd K, Iansek R. The biomechanics and motor control of gait in Parkinson disease. Clin Biomech (Bristol, Avon) 2001;16(6):459–470. doi: 10.1016/s0268-0033(01)00035-3. [DOI] [PubMed] [Google Scholar]
- Morris ME, Iansek R, Matyas TA, Summers JJ. The pathogenesis of gait hypokinesia in Parkinson’s disease. Brain. 1994;117(Pt 5):1169–1181. doi: 10.1093/brain/117.5.1169. [DOI] [PubMed] [Google Scholar]
- Pai YC, Rymer WZ, Chang RW, Sharma L. Effect of age and osteoarthritis on knee proprioception. Arthritis Rheum. 1997;40(12):2260–2265. doi: 10.1002/art.1780401223. [DOI] [PubMed] [Google Scholar]
- Paul SaL, Yanlong Inadequate light levels and their effect on falls and daily activities of community dwelling older adults: A review of literature. New Zealand Journal of Occupational Therapy. 2012;59(2):39–42. [Google Scholar]
- Pickett K, Konczak J. Measuring kinaesthetic sensitivity in typically developing children. Dev Med Child Neurol. 2009;51(9):711–716. doi: 10.1111/j.1469-8749.2008.03229.x. [DOI] [PubMed] [Google Scholar]
- Reed RJ, Lowrey CR, Vallis LA. Middle-old and old-old retirement dwelling adults respond differently to locomotor challenges in cluttered environments. Gait Posture. 2006;23(4):486–491. doi: 10.1016/j.gaitpost.2005.06.010. [DOI] [PubMed] [Google Scholar]
- Schaafsma JD, Giladi N, Balash Y, Bartels AL, Gurevich T, Hausdorff JM. Gait dynamics in Parkinson’s disease: relationship to Parkinsonian features, falls and response to levodopa. J Neurol Sci. 2003;212(1–2):47–53. doi: 10.1016/s0022-510x(03)00104-7. [DOI] [PubMed] [Google Scholar]
- Schrack JA, Simonsick EM, Ferrucci L. The energetic pathway to mobility loss: an emerging new framework for longitudinal studies on aging. J Am Geriatr Soc. 2010;58(Suppl 2):S329–336. doi: 10.1111/j.1532-5415.2010.02913.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tagliabue M, Ferrigno G, Horak F. Effects of Parkinson’s disease on proprioceptive control of posture and reaching while standing. Neuroscience. 2009;158(4):1206–1214. doi: 10.1016/j.neuroscience.2008.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaugoyeau M, Hakam H, Azulay JP. Proprioceptive impairment and postural orientation control in Parkinson’s disease. Hum Mov Sci. 2011;30(2):405–414. doi: 10.1016/j.humov.2010.10.006. [DOI] [PubMed] [Google Scholar]
- Vitorio R, Lirani-Silva E, Barbieri FA, Raile V, Batistela RA, Stella F, Gobbi LT. The role of vision in Parkinson’s disease locomotion control: free walking task. Gait Posture. 2012;35(2):175–179. doi: 10.1016/j.gaitpost.2011.09.002. [DOI] [PubMed] [Google Scholar]
- Wright WG, Gurfinkel VS, King LA, Nutt JG, Cordo PJ, Horak FB. Axial kinesthesia is impaired in Parkinson’s disease: effects of levodopa. Exp Neurol. 2010;225(1):202–209. doi: 10.1016/j.expneurol.2010.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zesiewicz TA, Gold M, Chari G, Hauser RA. Current issues in depression in Parkinson’s disease. Am J Geriatr Psychiatry. 1999;7(2):110–118. [PubMed] [Google Scholar]


