Abstract
Objective
Hyperlipidemia-induced endothelial cell (EC) activation is considered as an initial event responsible for monocyte recruitment in atherogenesis. However, it remains poorly defined what is the mechanism underlying hyperlipidemia-induced EC activation. Here we tested a novel hypothesis that mitochondrial reactive oxygen species (mtROS) serve as signaling mediators for EC activation in early atherosclerosis.
Approach and Results
Metabolomics and transcriptomics analyses revealed that several lysophosphatidylcholine (LPC) species, such as 16:0, 18:0 and 18:1, and their processing enzymes, including Pla2g7 and Pla2g4c, were significantly induced in the aortas of apolipoprotein E knockout (ApoE−/−) mice during early atherosclerosis. Using electron spin resonance and flow cytometry, we found that LPC 16:0, 18:0 and 18:1 induced mtROS in primary human aortic ECs (HAECs), independently of the activities of nicotinamide adenine dinucleotide phosphate (NADPH) oxidase. Mechanistically, using confocal microscopy and Seahorse XF mitochondrial analyzer, we showed that LPC induced mtROS via unique calcium entry-mediated increase of proton leak and mitochondrial O2 reduction. In addition, we found that mtROS contributed to LPC-induced EC activation by regulating nuclear binding of AP-1 and inducing intercellular adhesion molecule 1 (ICAM-1) gene expression in vitro. Furthermore, we showed that mtROS inhibitor MitoTEMPO suppressed EC activation and aortic monocyte recruitment in ApoE−/− mice using intravital microscopy and flow cytometry methods.
Conclusions
ATP synthesis-uncoupled, but proton leak-coupled mtROS increase mediates LPC-induced EC activation during early atherosclerosis. These results indicate that mitochondrial antioxidants are promising therapies for vascular inflammation and cardiovascular diseases.
Keywords: mitochondria, reactive oxygen species, endothelial cell, vascular inflammation, atherosclerosis
Introduction
Atherosclerosis is a chronic inflammatory pathogenic process of arteries, which leads to cardiovascular diseases (CVDs), including myocardial infarction and stroke1. Despite current therapies, CVDs remain the number one cause of death in the United States2. We and others have previously shown that hyperlipidemia, along with other CVD stressors, such as hyperglycemia and hyperhomocysteinemia, promote atherosclerosis via several mechanisms. These mechanisms include endothelial cell (EC) activation and injury3, 4; monocyte recruitment and differentiation5, 6; decreased regulatory T cells7, 8; and impaired vascular repair ability of bone marrow-derived progenitor cells9, 10. Hyperlipidemia-induced EC activation is considered as an initial event responsible for monocyte recruitment in atherogenesis1. However, the molecular mechanism underlying hyperlipidemia-induced EC activation remains poorly defined.
Lysophosphatidylcholines (LPCs) are a group of proinflammatory lipids, which are critically involved in the pathogenesis of atherosclerosis11. Multiple lines of evidence indicate that aortic LPCs are induced in advanced atherosclerosis. As early as 1969, it was reported that the concentration of aortic LPCs from monkeys fed on an atherogenic diet for three to six months was nearly eight times higher than that of the control group12. In addition, diabetic and hypercholesterolemic pigs with advanced coronary atherosclerosis showed a 305% increase in arterial LPC content13. Furthermore, different LPC species, including palmitoyl-LPC (16:0), stearoyl-LPC (18:0), and oleoyl-LPC (18:1), were approximately two times higher in atherosclerotic plaques associated with symptoms than those in asymptomatic plaques in humans14. However, whether LPC is induced during early atherogenesis remains unknown.
It was shown thirty years ago that when low-density lipoprotein (LDL) was incubated with ECs, LDL was oxidized and as much as forty percent of the LDL phospholipid was hydrolyzed to LPC by the enzymatic action of phospholipase15. It was later found that LPC could potently activate ECs and induce monocyte adhesion by transcriptionally upregulating intercellular adhesion molecule 1 (ICAM-1) gene expression in human umbilical vein ECs (HUVECs)16. Furthermore, both reactive oxygen species (ROS) inhibitor and intracellular calcium inhibitor could block LPC-induced ICAM-1 gene expression in HUVECs17. Moreover, LPC also activated proinflammatory transcription factors, such as nuclear factor-κB (NF-κB) and activator protein-1 (AP-1), in HUVECs18. Nevertheless, the source of ROS that contributes to LPC-induced EC activation, and the mechanistic links between these cellular signaling events remain unclear.
There are multiple cellular sources of ROS, including mitochondrial electron transport chain, nicotinamide adenine dinucleotide phosphate oxidase (NADPH oxidase), xanthine oxidase, uncoupled nitric oxide synthase, and cytochrome P450. As a major contributor to cellular ROS, mitochondrial ROS (mtROS) are generated from the partial oxygen reduction to form superoxide at complex I and complex III in the mitochondrial electron transport chain19. Although mtROS are historically considered to be toxic by-products of mitochondrial metabolism, it is recently discovered that mtROS are, in fact, signaling molecules that directly contribute to proinflammatory cytokine production19, independently of key cytosolic ROS generator, NADPH oxidase20. In addition, mtROS production is regulated by a number of factors, such as mitochondrial membrane potential, mitochondrial Ca2+, and mitochondrial proton leak19. However, since mtROS and ATP production are both coupled to electron transport chain activity, it still remains unknown how mtROS could be induced independently of ATP synthesis.
Thus, in spite of recent progress, two important knowledge gaps exist: first, it remains unknown whether the expression of LPC is increased during early atherosclerosis; second, the intracellular source of ROS, which contributes to LPC-induced aortic EC activation is unclear. In this study, we test a novel hypothesis that mtROS serve as signaling mediators for LPC-induced EC activation. Using metabolomics analysis and microarray profiling, as well as biochemistry and molecular biology approaches, we found that LPCs were induced in the aorta during early atherosclerosis and that mtROS mediated LPC-induced EC activation. In addition, we uncovered a novel ATP synthesis-uncoupled, but proton leak-coupled mechanism in driving mtROS production in the cell. Thus, mtROS may serve as a novel target for therapeutic intervention in vascular inflammation and CVDs.
Materials and Methods
Materials and Methods are available in the online-only Supplement.
Results
1. LPCs are induced in the aorta during early atherosclerosis in mice
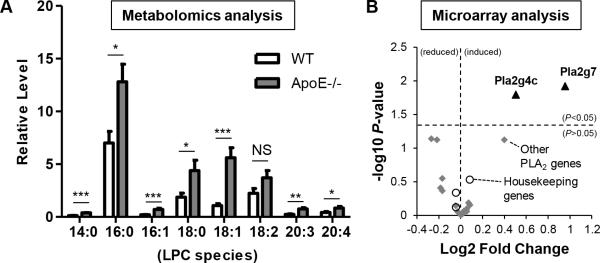
To determine whether LPC is involved in early atherosclerosis development, we examined LPC levels in the aortas of ApoE−/− mice (an atherosclerotic mouse model) in comparison to those of wild-type (WT) control mice. We performed non-targeted metabolomic analysis on the aortas from these mice fed with high-fat (HF) diet for three weeks (Supplemental Figure I). Of note, western-type, HF diet was used to accelerate atherosclerosis and we and others have shown previously that in ApoE−/− mice fed with high-fat diet for 3 weeks, plasma cholesterol level tripled but very minimal plaque developed in the aorta3, 21. Thus, it serves well as an early atherosclerosis mouse model. We were able to detect eight different LPC species in the aortas of WT and ApoE−/− mice. The three most abundant species in the aorta included palmitoyl-LPC (16:0), stearoyl-LPC (18:0), and oleoyl-LPC (18:1). Strikingly, all of the detected LPC species were significantly induced in the aortas of ApoE−/− mice, with the exception of linoleoyl-LPC (18:2) (Figure 1A). LPC is produced by the enzymatic action of phospholipase A2 (PLA2) on phosphatidylcholine; and the PLA2 superfamily enzyme members are critically involved in atherosclerosis11, 22. For these reasons, we also examined the gene expression changes of all the PLA2 superfamily enzymes between ApoE−/− mice and WT mice using microarray analysis. The results showed that Pla2g7 (also known as lipoprotein-associated PLA2) and Pla2g4c were significantly induced in the aortas of ApoE−/− mice in early atherosclerosis (Figure 1B, Supplemental Table I). Notably, the expression levels of three house-keeping genes were within the range of 0.97 to 1.06, suggesting the high quality of our microarray analysis and the specificity of PLA2 upregulation. It is possible that aortic LPC could be increased due to increased substrate availability in ApoE−/− mice. However, it is unlikely to be the case since several long chain fatty acids, including palmitate (16:0), stearate (18:0), and oleate (18:1n9), were not significantly increased in the aortas of ApoE−/− mice (Supplemental Figure I). Taken together, these results indicate that LPC is induced during early atherosclerosis, presumably due to the induction of Pla2g7 and Pla2g4c enzyme expression (Supplemental Figure I).
Figure 1. Aortic lysophoshatidylcholine (LPC) species are induced during early atherogenesis in mice.
Eight-week old wild-type (WT) mice and apolipoprotein E knockout (ApoE−/−) mice were fed with high-fat diet for 3 weeks before they were sacrificed. Aortas were collected from these mice for metabolomics analysis (A) and microarray analysis (B). A. Aortic LPC species were induced during early atherosclerosis. Relative changes of aortic LPC between WT and ApoE−/− were shown (n=8 per group). B. LPC-generating enzymes, including Pla2g4c and Pla2g7, were induced in the aortas during early atherosclerosis. Volcano plot was presented which showed fold change and statistical P value of expression changes of phospholipase A2 superfamily members and 3 housekeeping genes (Actb, Gapdh, and Nono) between ApoE−/− mice and WT mice (n=5 per group; solid triangle, significantly increased PLA2 genes; grey diamond, unchanged PLA2 genes; empty circle, control housekeeping genes). For all panels, values represent mean ± SEM. NS, not significant; *, p<0.05; **, p<0.01; ***, p<0.001. WT, wild-type; ApoE−/−, apolipoprotein E deficient.
2. LPC induces mtROS, independently of NADPH oxidase, in human aortic ECs (HAEC)
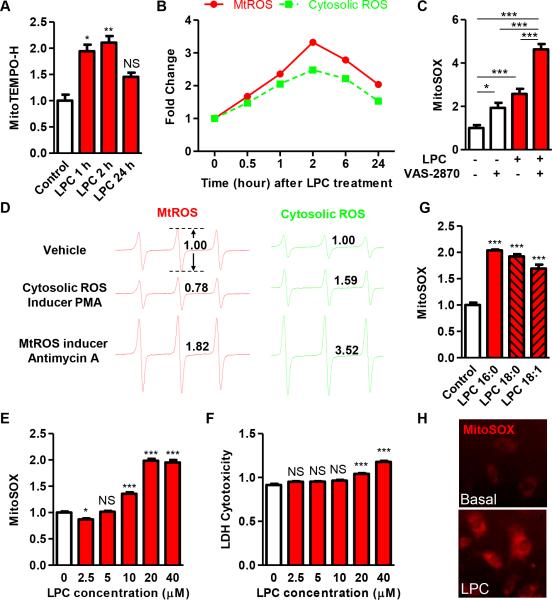
Next, we hypothesized that the induction of aortic LPC could contribute to atherosclerosis development by promoting aortic EC activation. It should be noted that lesional macrophages are also present in early atherosclerosis but our current study focuses on investigating the role of LPC in aortic EC activation. It has been previously demonstrated that LPC induced EC activation in HUVECs16. In addition, LPC-induced EC activation in HUVECs could be blocked by diphenyleneiodonium17, which inhibits ROS generation from mitochondria as well as NADPH oxidase, the latter of which being a major cytosolic ROS generator. Thus, the intracellular source of ROS contributing to LPC-induced HAEC activation remains to be specified. To examine this issue, we first compared the effects of LPC on the production of mtROS and cytosolic ROS in HAECs simultaneously by using electron spin resonance (ESR) method. We found that 10 μM palmitoyl-LPC (16:0) quickly induced mtROS production in 30 minutes, which lasted for at least 6 hours and decreased after 24 hours (Figures 2A and 2B). In addition, LPC induced cytosolic ROS in a similar manner, but to a lesser degree (Figure 2B). Importantly, a specific NADPH oxidase inhibitor, VAS-2870, did not prevent LPC-induced mtROS in HAECs, but rather further increased it (Figure 2C). Of note, VAS-2870 treatment alone also significantly induced mtROS in HAEC, suggesting that mtROS may be induced to compensate for the loss of cytosolic ROS in the cell. It is possible that VAS-2870 itself may have stimulated mtROS production besides inhibiting NADPH oxidase. However, it is unlikely to be the case since another specific NADPH oxidase inhibitor, VAS3947, similarly induced mtROS (data not shown). Furthermore, mtROS-inducer, Antimycin A, induced both mtROS and cytosolic ROS, while NADPH oxidase activator, phorbol myristate acetate (PMA), only induced cytosolic ROS (Figure 2D). Taken together, these results have demonstrated that LPC-induced mtROS are located upstream of the pipeline in generating cytosolic ROS.
Figure 2. LPC induces mitochondrial ROS (mtROS) in human aortic endothelial cells (HAECs).
A. LPC time-dependently induced mtROS. HAECs were treated with LPC (16:0, 10 μM) for different time points and cell aliquots were incubated with MitoTEMPO-H (1mM) at 37°C for 20 minutes before electron spin resonance (ESR) analysis (n=4, p values vs control). B. Higher mtROS than cytosolic ROS were induced by LPC. HAECs were treated with LPC (16:0, 10 μM) for different time points and cell aliquots were incubated with either mtROS spin probe MitoTEMPO-H (1mM, red line) or cytosolic ROS spin probe CP-H (1mM, green line) at 37°C for 20min before measurement by ESR. C. The effect of NADPH oxidase inhibition on LPC-induced mtROS. After loading with MitoSOX (5 μM) for 10 min, HAECs were treated with LPC (16:0, 10 μM) with or without NADPH oxidase inhibitor VAS-2870 (5 μM) for 1 hour before flow cytometry analysis (n=6). Fold change of MitoSOX+ cell population was shown. D. The effect of NADPH oxidase activation on mtROS. HAECs were treated with Antimycin A (5 μM) or phorbol myristate acetate (PMA, 5 μM) for 1 hour and cells were incubated with mtROS probe MitoTEMPO-H (1mM) and cytosolic ROS probe CPH (1mM) before measurement by ESR. ESR signals were shown and fold changes were quantified by measuring the difference between maximal and minimal spin probe signal. E. LPC dose-dependently induced mtROS. After loading with MitoSOX (5 μM) for 10 min, HAECs were treated with different doses of LPC (16:0) ranging from 2.5μM to 40 μM for 1 hour before flow cytometry analysis (n=8, p values vs control). F. Higher concentration of LPC induced cytotoxicity. HAECs were treated with different doses of LPC (16:0) for 1 hour and cell mediums were collected for the measurement of LDH release as an indicator of cytotoxicity (n=15, p values vs control). G. Three major LPC species all induced mtROS. Three major LPC species (10 μM) including LPC (16:0), LPC (18:0), and LPC (18:1) all significantly induced mtROS in HAEC after 1-hour treatment as measured by MitoSOX using flow cytometry method (n=6, p values vs control). H. Visualization of mtROS induction by LPC. After treatment of HAEC with vehicle control or LPC (16:0, 10 μM) for 1 hour, MitoSOX staining was visualized by fluorescent microscopy. The data are representative of three randomly chosen field. For all panels, values represent mean ± SEM and data are representative of at least two independent experiments. NS, not significant, *, p<0.05, **, p<0.01, ***, p<0.001. PMA, phorbol myristate acetate.
To confirm the results from ESR, we used another specific mtROS fluorescence probe, MitoSOX, combined with the use of flow cytometry and found that LPC dose-dependently increased mtROS production in HAECs (Figure 2E). Higher dosage of LPC (40 μM), however, did not further induce mtROS but was cytotoxic (Figure 2E and 2F). In addition, we found that the induction of mtROS is a common feature shared by the LPC family members since all the three major LPC species, including LPC (16:0), LPC (18:0), and LPC (18:1), similarly induced mtROS production in HAECs (Figure 2G). Since LPC (16:0) was the most abundantly expressed aortic LPC species (Figure 1A), 10 μM LPC (16:0) was used hereafter in this study. Lastly, we used a third method, fluorescence microscopy, and confirmed that LPC induced mtROS in HAECs (Figure 2H). Collectively, these results indicate for the first time that three major LPC species, upregulated in early atherosclerotic aortas (Figure 1A), could all induce mtROS in HAECs. While high levels of mtROS induced by a high concentration of LPC are associated with EC death, moderate levels of mtROS stimulated by 10 μM LPC could serve as signaling molecules for EC activation.
3. Mitochondrial Ca2+ entry mediates LPC-induced mtROS production by increasing mitochondrial proton leak and oxygen reduction in HAECs
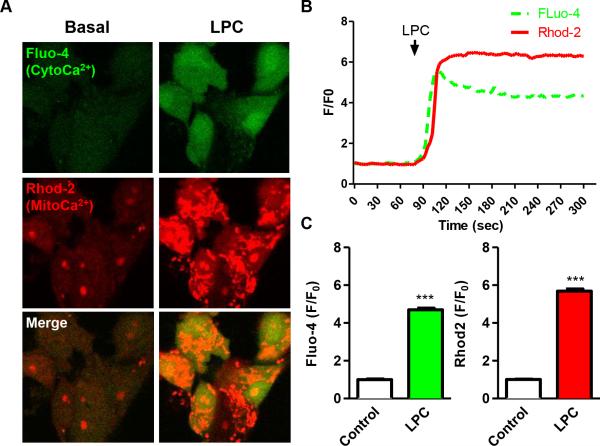
MtROS production is regulated by a number of factors, such as the metabolic state of mitochondria, mitochondrial membrane potential, and mitochondrial Ca2+ influx19, 23. Since previous studies reported that LPC could induce cytosolic Ca2+ levels24; and that Ca2+ influx into mitochondria is a positive regulator of mitochondrial O2 reduction rates25, we hypothesized that LPC-induced Ca2+ entry into the mitochondria could lead to increased mtROS production. Firstly, we examined the effects of LPC on cytosolic and mitochondrial Ca2+ levels simultaneously using confocal microscopy. The results showed that LPC dramatically induced cytosolic Ca2+, which were quickly followed by mitochondrial Ca2+ induction (Figures 3A and 3B). The peak response of mitochondrial Ca2+ entry was similar to that of cytosolic Ca2+, and both signals lasted for at least 5 minutes (Figures 3B and 3C). These results indicate that LPC induces mitochondrial Ca2+ entry from cytosol.
Figure 3. LPC induces mitochondrial Ca2+ entry in HAECs.
A. LPC induced both cytosolic Ca2+ and mitochondrial Ca2+ in HAEC. HAECs loaded with cytosolic Ca2+ (cytoCa2+) indicator Fluo-4/AM (green) and mitochondrial Ca2+ (mitoCa2+) indicator Rhod-2 (red) were stimulated by 10 μM LPC and analyzed by confocal microscopy. Images were taken before and after the stimulation of LPC. B. LPC-induced mitochondrial Ca2+ followed quickly after cytosolic Ca2+ increase. Real-time tracing of cytosolic and mitochondrial Ca2+ mobilization in response to LPC from the confocal microscopy analysis was shown. Each line represents the mean value from three cells. C. LPC induced similar levels of mitochondrial Ca2+ and cytosolic Ca2+. Quantitation of peak response of cytosolic Ca2+ and mitochondrial Ca2+ from the confocal microscopy analysis was shown (n=9). For all panels, values represent mean ± SEM and data are representative of at least three independent experiments. ***, p<0.001. CytoCa2+, cytosolic Ca2+; mitoCa2+, mitochondrial Ca2+. F/F0, fluorescence intensity ratios.
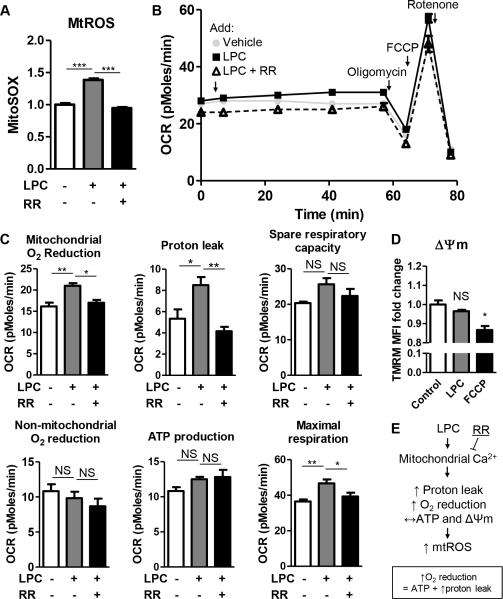
Next, we hypothesized that LPC-induced mitochondrial Ca2+ entry could lead to mtROS production in HAECs. To examine this, we used ruthenium red (RR), which is a mitochondrial calcium uniporter (MCU) inhibitor that can block Ca2+ entry into the mitochondria. We found that RR completely abolished LPC-induced mtROS production (Figure 4A), indicating that mitochondrial Ca2+ entry mediates LPC-induced mtROS in HAECs. To determine how LPC-induced mitochondrial Ca2+ entry accelerated mtROS production, we utilized the Seahorse XF96 Analyzer to assess mitochondria functions. The Seahorse XF analyzer could measure six different mitochondrial parameters, including mitochondrial O2 reduction rate, non-mitochondrial O2 reduction rate, proton leak, ATP production, maximal respiration, and spare respiratory capacity (Supplemental Figure II). We found that LPC significantly induced mitochondrial O2 reduction rate but did not affect non-mitochondrial O2 reduction rate (Figures 4B and 4C), which correlated with our previous findings that LPC-stimulated ROS originated from mitochondria, but not cytosol (Figure 2). In addition, the MCU inhibitor, RR, significantly inhibited LPC-induced mitochondrial O2 reduction rates (Figure 4C), correlating with the previous findings that mitochondrial Ca2+ entry mediates LPC-induced mtROS in HAECs (Figure 4A). LPC also significantly increased maximal respiration rates, but it did not change spare respiratory capacity of mitochondria (Figure 4C), which suggested that LPC-induced maximal O2 reduction increase was mainly due to increased basal O2 reduction. The rate of mitochondrial O2 reduction is coupled to the rates of ATP production and proton leak (Supplemental Figure II). Mitochondrial proton leak is the re-entry of protons from the intermembrane space into the mitochondrial matrix independent of ATP synthesis, which usually leads to a decrease in mitochondrial membrane potential (ΔΨm)25. Interestingly, we found that LPC significantly induced proton leak, but not ATP production and that LPC-induced proton leak could be blocked by the MCU inhibitor, RR (Figure 4C). Moreover, LPC did not change ΔΨm in HAECs (Figure 4D), while chemical mitochondrial membrane uncoupler, FCCP, significantly decreased ΔΨm. These results suggest the following: first, LPC-induced mitochondrial Ca2+ entry preferentially stimulates proton leak but not ATP synthesis, suggesting that LPC at low dose is not an energy-generating stimulus in ECs; second, LPC-induced proton leak is used by EC for the induction of O2 reduction in the electron transport chain; third, mtROS are increased in response to LPC stimulation and reversed by MCU inhibitor RR, and fourth, LPC-induced proton leak is equivalent to the proton efflux into intermembrane space, so that mitochondrial membrane potential is not affected. Taken together, these results indicate that LPC induces mitochondrial Ca2+ entry, which increases ATP synthesis-uncoupled, but proton leak-coupled mtROS (Figure 4E).
Figure 4. Mitochondrial Ca2+ entry mediates LPC-induced mtROS by increasing mitochondrial O2 reduction and proton leak in HAECs.
A. LPC induced mtROS via mitochondrial Ca2+ entry. After loading with MitoSOX (5 μM) for 10 min, HAECs were treated with vehicle control, LPC (10 μM), or LPC (10 μM) plus Ruthenium Red (RR) (10 μM) for 1 hour and mtROS were measured by flow cytometer (n=8). B & C. LPC induced mitochondrial O2 reduction and proton leak via mitochondrial Ca2+ entry. After the addition of vehicle control, LPC (10 μM), and LPC (10 μM) plus RR (10 μM), oxygen consumption rate (OCR) was measured every 20 minutes for 1 hour. Afterwards, XF Mito Stress Test was performed by sequential adding of Oligomycin (1 μM), FCCP (1 μM), and Rotenone (1 μM). Experiment curve (B) and quantification of six mitochondrial parameters (C) were shown (n=6). D. LPC did not affect mitochondrial membrane potential (ΔΨm). After HAECs were treated with vehicle control, LPC (10 μM), or FCCP (1 μM) for 1 hour, they were loaded with ΔΨm probe TMRM (30 nM) for 20 min, and ΔΨm was measured by flow cytometer (n=4, p values vs control). E. Schematic representation of how LPC induced mtROS. For all panels, values represent mean ± SEM and data are representative of at least two independent experiments. NS, not significant, *, p<0.05, **, p<0.01, ***, p<0.001. RR, Ruthenium Red; ΔΨm, mitochondrial membrane potential. OCR, oxygen consumption rate; MFI, mean fluorescence intensity.
Since ROS production in mitochondria is determined by the rates of both mtROS production and disposal19, we also investigated the effects of LPC on regulating the expression of mitochondrial antioxidant superoxide dismutase 2 (SOD2) and uncoupling molecules including uncoupling protein 3 (UCP3) and adenine nucleotide translocator (ANT). We found that LPC did not regulate the expression of SOD2 and UCP3, although there was a trend of ANT induction after LPC stimulation (Supplemental Figure III). ANT, also known as the ADP/ATP translocator, exports ATP from the mitochondrial matrix, imports ADP into the matrix, and also mediates both basal and inducible proton conductance. The induction of ANT by LPC correlated with the findings that LPC induced mitochondrial proton leak in HAECs (Figure 4C).
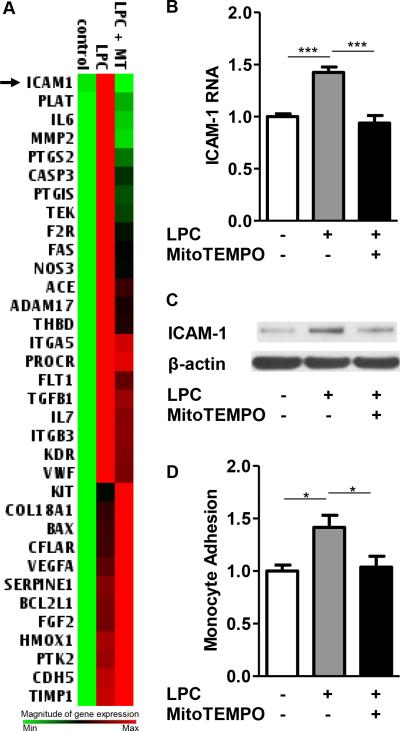
4. MtROS contribute to LPC-induced upregulation of ICAM-1 and other EC activation-related genes by regulating nuclear binding of AP-1
To determine the downstream effects of LPC-induced mtROS in ECs, we determined the effects of LPC in regulating EC-related gene expressions by performing Human Endothelial Cell Biology PCR array profiling. HAECs were stimulated by LPC with or without a specific mtROS scavenger, MitoTEMPO. PCR array was performed afterwards to screen for the changes of 84 genes related to EC functions, including vessel tone, angiogenesis, EC activation, and EC injury. We were able to detect the expressions of 57 genes in both control and LPC-treated HAECs. Among these 57 expressed genes, we found that 34 genes were induced more than 1.2-fold by LPC, and 3 genes were decreased more than 1.2-fold (Supplemental Table II). More importantly, we found that 14 out of these 34 LPC-induced genes (41.2%), such as ICAM-1, plasminogen activator, tissue (PLAT), interleukin 6 (IL-6), and matrix metalloproteinase-2 (MMP2), could be blocked by co-treatment of mtROS inhibitor, MitoTEMPO. Importantly, the expression of EC adhesion molecule, ICAM-1, was the most sensitive gene in response to mtROS scavenging (Figure 5A). By using RT-PCR and Western blots, we confirmed that LPC increased ICAM-1 RNA and protein expression, which could be inhibited by MitoTEMPO co-treatment (Figures 5B and 5C). Furthermore, we performed monocyte adhesion assay and showed that LPC-treated HAECs had increased their adhesion to untreated monocytes, which was inhibited by MitoTEMPO (Figure 5D). Taken together, these results demonstrate for the first time that LPC-induced mtROS are required for LPC-induced EC activation by regulating the mRNA and protein expressions of certain EC biology-related genes, including ICAM-1.
Figure 5. LPC-induced mtROS are required for ICAM-1 upregulation in HAECs.
A. LPC induced ICAM-1 and other EC function-related genes via mtROS. HAECs were treated with vehicle control, LPC (10μM), and LPC (10μM) plus MT (1μM) for 6 hours and RNA was collected for Human EC Biology PCR array (QIAGEN) analysis. Non-supervised hierarchical clustering of genes was used to generate heat map to show the genes that were regulated by LPC-induced mtROS. Three samples were pooled in each group. B. Confirmation by real-time PCR. HAECs were treated with LPC (10 μM) with/without MitoTEMPO (1 μM) for 18 hours before RNA was collected for real-time PCR analysis. Quantitation of ICAM-1 RNA expression normalized by β-actin was shown (n=6). C. Confirmation by Western blot. HAECs were treated with LPC (10 μM) with/without MitoTEMPO (1 μM) for 18 hours before proteins were collected for ICAM-1 expression. Representative Western blots from three independent experiments were shown. D. Effects of mtROS inhibition on LPC-induced monocyte adhesion to HAECs. HAECs were treated with LPC (10 μM) with/without MitoTEMPO (1 μM) for 4 hours, after which the adhesion of non-stimulated, fluorescence-labeled human peripheral blood mononuclear cells to stimulated HAECs was quantified (n=5). For all panels, values represent mean ± SEM and data are representative of at least two independent experiments. *, p<0.05, **, p<0.01, ***, p<0.001. MT, MitoTEMPO.
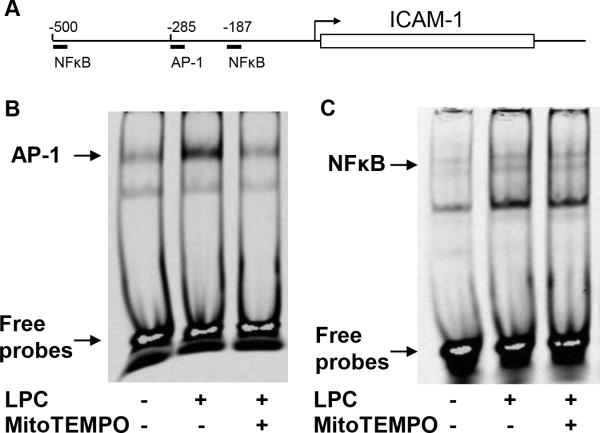
Transcription factor binding sites of NFκB and AP-1 have been previously identified in the promoter region of ICAM-126 (Figure 6A). In addition, LPC has been shown to increase the nuclear translocation of NFκB and AP-1 in HUVECs18. Thus we hypothesized that LPC-induced mtROS contribute to the nuclear bindings of pro-inflammatory transcription factors to the promoter of ICAM-1 in HAECs, which leads to ICAM-1 upregulation. Using electrophoretic mobility shift assay (EMSA), we showed that LPC potently induced nuclear translocation of AP-1 but weakly induced NFκB in HAECs (Figures 6B and 6C). In addition, co-treatment of MitoTEMPO almost completely abolished LPC-induced AP-1 but not NFκB nuclear binding. These results correlated well with our previous finding that AP-1 mediated LPC-induced EC activation3. Moreover, by performing a literature search, we found that out of the 14 upregulated genes that were the targets of LPC-induced mtROS (Figure 5A), 12 genes, including ICAM-1, were also previously proposed to be the downstream targets of AP-1 or ROS pathway (Supplemental Table III). Taken together, these results suggest that mtROS contribute to upregulated expressions of ICAM-1 and other genes involved in EC activation by upregulating AP-1-targeted gene transcription.
Figure 6. MtROS contribute to LPC-induced endothelial activation by upregulating nuclear binding of AP-1 on the promoter of ICAM-1.
A. Putative AP-1 and NFκB binding site in the promoter of ICAM-1. B & C. MtROS inhibitor MitoTEMPO blocked LPC-induced nuclear AP-1 binding. HAECs were treated with vehicle or LPC (10 μM) for 1 hour with or without MitoTEMPO (1 μM) 1-hour pre-incubation, and nuclear proteins were collected afterwards for electrophoretic mobility shift assay (EMSA). 2 μg nuclear proteins were used for AP-1 EMSA (B) and 5 μg nuclear proteins were used for NFκB EMSA (C). Representative images from three independent experiments were shown.
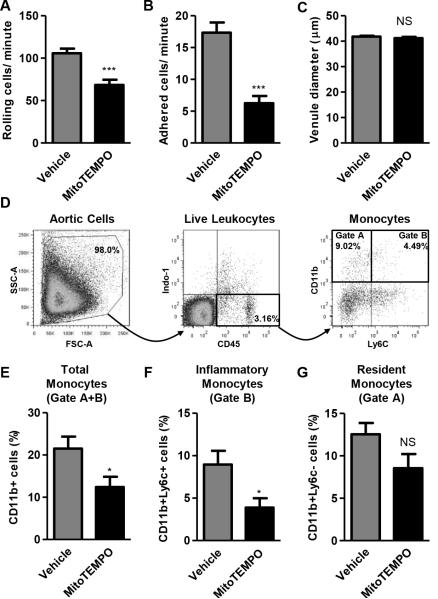
5. MtROS inhibition suppresses EC activation and monocyte recruitment into the aorta during early atherosclerosis in vivo
To examine whether mtROS contribute to EC activation during early atherosclerosis in vivo, we implanted the ALZET osmotic mini-pumps containing either saline control or MitoTEMPO (1500 μg/kg/day) subcutaneously into 8-week old ApoE−/− mice before they were put on a high fat diet for another 3 weeks. We determined their EC activation status afterwards by examining leukocyte rolling and adhesion to the endothelium in cremaster muscle vessels using intravital microscopy. We found that MitoTEMPO significantly inhibited leukocyte rolling and adhesion to the endothelium on the post-capillary venule wall (Figures 7A and 7B). Of note, there was no difference in the venule diameters between the two groups (Figure 7C), suggesting that MitoTEMPO did not significantly change the venule diameters. In addition, we did not detect any leukocyte rolling or adhesion in the arterioles of the cremaster muscle (data not shown) due to the rapid movement of blood cells within these vessels, as shown previously27. Similarly, the high blood flow speeds and high pulse vibrations in middle and aortic arteries make the current technology of intravital microscope unsuitable in determining in vivo leukocyte rolling and adhesion to the endothelium in aortic arteries28. To determine whether MitoTEMPO could decrease the recruitment of monocytes into the aortas of ApoE−/− mice, we prepared aortic single cell suspensions from these mice and performed flow cytometric analysis with fluorescence-conjugated antibodies staining for Indo-1 (dead cell), CD45 (leukocyte), CD11b (monocyte), and Ly6c (inflammatory or resident monocyte), as we reported previously6 (Figure 7D). The results showed that MitoTEMPO significantly decreased the recruitment of CD45+CD11b+ total monocytes as well as CD45+CD11b+Ly6c+ inflammatory monocytes into the aortas of ApoE−/− mice (Figures 7E and 7F), while MitoTEMPO did not significantly affect the recruitment of CD45+CD11b+Ly6c− resident monocytes (Figure 7G). We further determined whether aortic monocyte composition changes resulted from the global changes in the peripheral blood monocyte composition. The results showed that MitoTEMPO did not significantly affect the populations of CD45+CD11b+ monocytes and CD45+CD11b+Ly6C+ monocytes in the blood (Supplemental Figure IV). Taken together, these results demonstrate that MitoTEMPO treatment suppresses aortic EC activation in ApoE−/− mice but do not rule out the potential beneficial effects of MitoTEMPO on lesional macrophages.
Fig. 7. MitoTEMPO treatment decreases in vivo endothelial activation during early atherosclerosis.
At eight weeks of age, mini-pumps containing saline or MitoTEMPO (1500 μg/kg/day) were implanted in ApoE−/− mice before they were fed with a high fat diet for three weeks. Afterwards, intravital microscopy (A-C, n=4-6 mice per group, 3 vein vessels per mouse were recorded) and flow cytometry analyses (D to G, n=7-9 mice per group) were carried out to determine the endothelial activation status in vivo. A. MitoTEMPO treatment decreased leukocyte rolling to endothelium. Number of leukocytes that rolled past an imaginary line that was perpendicular to the vessels during a 1-minute period observed. B. MitoTEMPO decreased leukocyte adhesion to endothelium. Number of cells adhered to the endothelium for 1 minute, 100um length observed. C. MitoTEMPO did not change mean vessel diameter of venule. D. Gating strategy of aortic monocyte by flow cytometry. Total monocytes were gated as Indo-1−CD45+CD11b+ and inflammatory monocytes were gated as Indo-1-CD45+CD11b+Ly6c+. E. MitoTEMPO decreased aortic monocyte infiltration. Percentages of CD11b+ monocytes (Gate A+B in panel C) in total aortic leukocyte cell population (Indo-1−CD45+) were shown in each group. F. MitoTEMPO decreased aortic inflammatory monocyte infiltration. Percentages of CD11b+Ly6c+inflammatory monocytes (Gate B in panel C) in total aortic leukocyte cell population were shown in each group. G. MitoTEMPO did not significantly affect aortic resident monocyte infiltration. Percentages of CD11b+Ly6c− resident monocytes (Gate A in panel C) in total aortic leukocyte cell population were shown in each group. For all panels, values represent mean ± SEM. NS, not significant, *, p<0.05, ***, p<0.001.
Discussion
Atherosclerosis is a chronic inflammatory disease that is a major pathogenic process underlying the development of coronary heart disease, stroke and peripheral vascular disease. In spite of recent progress, novel anti-inflammatory strategies are still in urgent need for prevention and treatment of atherosclerotic CVD29. LPCs are a group of endogenous proinflammatory lipids considered to be a causative factor for atherosclerosis. For this reason, inhibitors of sPLA2 and Lp-PLA2, the key enzymes responsible for the generation of LPC, have been developed in the hope of developing novel anti-inflammatory therapies against atherosclerosis29. The beneficial effects of sPLA2 inhibitor (Varespladib) and Lp-PLA2 inhibitor (Darapladib) have been demonstrated in atherosclerotic animal models13, 30 and human phase 2 clinical trials31, 32. However, three recent phase 3 clinical trials failed to show their therapeutic efficacy33-35. One possibility that may explain these failures is related to the fact that LPC also plays important physiological roles, such as stimulating insulin release from pancreatic β cells36 and transporting essential fatty acids37. For this reason, targeting the pathogenic downstream effects of LPC, instead of blocking the production of LPC itself, may lead to the development of better therapeutics. Along this line, our approaches using metabolomics and transcriptomics in the current study demonstrated for the first time that 7 out of 8 detected LPC species were induced in the aorta of early atherosclerotic mice, presumably due to increased expression of PLA2 in the aorta. More importantly, we found for the first time that proatherogenic lipid, LPC, via a mtROS-mediated mechanism, induced EC activation, which is an initiation step of atherogenesis. Therefore, blocking excessive mtROS production downstream of LPC might protect arteries against atherogenesis. This idea is supported by previous findings reporting that various other vascular stressors, including oxidized LDL, glucose, angiotensin II, hypoxia, and proinflammatory cytokines also induced mtROS production in ECs19. In addition, pharmacological drugs, such as statins, metformin, resveratrol, and cannabidiol could inhibit glucose-induced mtROS production in ECs19. Moreover, it has been shown previously that ApoE−/− mice deficient in superoxide dismutase 2 gene, which scavenges mtROS, displayed accelerated atherogenesis38. EC-specific overexpression of thioredoxin 2, another mitochondrial antioxidant enzyme, improved endothelial function and reduced atherosclerosis development in ApoE−/− mice39. Collectively, we and others have demonstrated a critical proatherogenic role for mtROS in EC activation during early atherosclerosis. Notably, LPC could also activate macrophages besides promoting EC activation11 and diminishing mtROS in macrophages reduced lesion development in atherosclerotic mice40. Further study is needed to determine the role of LPC-induced mtROS in lesional macrophages during the development of atherosclerosis.
Previous studies have reported that LPC could induce NADH oxidase (mitochondrial)/ NADPH oxidase (cytosolic)-related ROS in ECs41. In addition, it was found that LPC-induced ROS was more prominent in mitochondria and much less abundant in cytosol24. It has also been shown that mitochondria, rather than NADPH oxidase, was the major source of inflammatory ROS in monocytes20. Along the same line, we identified that LPC-induced mtROS production was independent of NADPH oxidase in ECs.
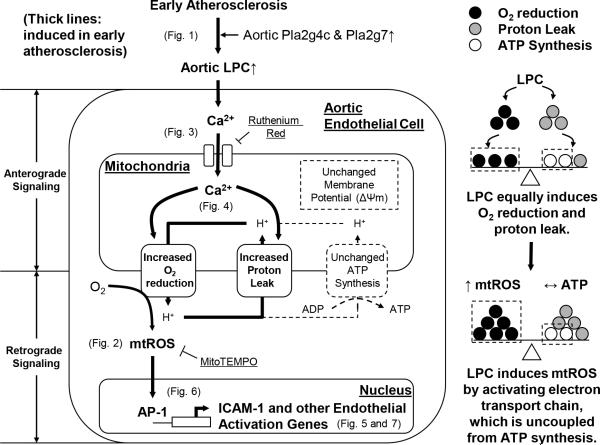
Even when there is ample oxygen, ECs rely heavily on glycolysis for their ATP demand, yet ECs contain functional mitochondria and very little is known about the role of mitochondria in endothelium42. By using the novel, state-of-art mitochondrial Seahorse XF96 analyzer for assaying mitochondrial functions, we demonstrate for the first time that when ECs are activated, LPC induces mtROS by accelerating electron transport chain and proton efflux, which is uncoupled from ATP synthesis by simultaneously accelerating proton leak. Thus, we propose that one of the major functions of mitochondrial proton leak in ECs may be fine-tuning mtROS generation for cell signaling purpose, such as endothelial activation. By doing this, in response to proatherogenic/proinflammatory stimuli including LPC, ECs could upregulate mtROS production without affecting ATP level and EC survival (Figure 8). This hypothesis is supported by the findings that mtROS were involved in regulating important physiological endothelial functions, such as hypoxia adaptation and angiogenesis effects, and in activating proinflammatory signaling pathways in response to various vascular stressors19.
Figure 8. A new working model.
Left, during early atherosclerosis, LPCs are induced in the aorta, presumably due to increased expression of Pla2g4c and Pla2g7. LPC then induces cytosolic Ca2+, which then enters into the mitochondria of aortic endothelial cells. LPC-induced mitochondrial Ca2+ then stimulates mitochondrial electron transport chain and proton leak without affecting ATP synthesis and mitochondrial membrane potential. As a result, mitochondrial reactive oxygen species (mtROS) are specifically induced without causing mitochondria injury. LPC-induced mtROS could then be released to the cytosol, where they regulate nuclear binding of AP-1 to the promoter of intercellular adhesion molecule-1 (ICAM-1) and other genes, contributing to endothelial activation. Anterograde signaling describes signal transduction from cytosol to mitochondria and retrograde signaling describes signal transduction from mitochondria to cytosol and nucleus. Right, LPC induces ATP-uncoupled, but proton leak-coupled mtROS. ICAM-1, intercellular adhesion molecule-1; mtROS, mitochondrial reactive oxygen species. ΔΨm, mitochondrial membrane potential.
Although controversies exist regarding what the real LPC receptor(s) is in the cell, LPC has been shown to stimulate cytosolic Ca2+ in different cell types11. In addition, it has been shown that LPC induced cellular Ca2+ uptake from an extracellular source via transient receptor potential vanilloid 2 (TRPV2) channel43. Interestingly, ruthenium red, which was used in this study for inhibiting MCU for mitochondrial Ca2+ entry, could also potently inhibit TRPV2 for cytosolic Ca2+ entry. Future studies are needed to determine the roles of MCU and TRPV2 in LPC-induced mtROS production.
To summarize (Figure 8), our study suggests that during early atherosclerosis, aortic LPCs are induced, presumably due to increased enzyme expression of Pla2g4c and Pla2g7. LPC then induces Ca2+ entry from cytosol to mitochondria, where it drives ATP synthesis-uncoupled, but proton leak-coupled mtROS. LPC-induced mtROS then regulate nuclear binding of AP-1 to the promoters of ICAM-1 and other EC activation-related genes, contributing to endothelial activation, monocyte adhesion to ECs, and monocyte recruitment into aorta. These findings are important, as they have improved our understanding of the molecular mechanisms of hyperlipidemia stimuli-induced EC activation in early atherogenesis. Such findings may, in turn, lead to the development of novel therapies, such as mitochondria-targeting antioxidant, which might greatly improve the outcome of CVDs.
Supplementary Material
Highlights.
Aortic LPCs and their processing enzymes are induced during early atherogenesis.
LPC-induced mitochondrial Ca2+ triggers mtROS independently from ATP synthesis.
MtROS mediate LPC-induced endothelial cell activation and monocyte adhesion.
MtROS inhibition is a promising target of early therapy for vascular inflammation.
Acknowledgements
We are very grateful to Drs. Ji-Youn Youn and Kin Lung Siu at the University of California, Los Angeles for their generous consultation of ESR.
Funding Sources
This work was partially supported by the National Institutes of Health Grants to XFY and HW.
Non-standard Abbreviations and Acronyms
- ECs
Endothelial cells
- HAECs
Human aortic endothelial cells
- LPC
Lysophosphatidylcholine
- MtROS
mitochondrial reactive oxygen species
- WT
Wild-type
- RR
Ruthenium Red
Footnotes
Disclosures: None
References
- 1.Libby P, Ridker PM, Hansson GK. Progress and challenges in translating the biology of atherosclerosis. Nature. 2011;473:317–25. doi: 10.1038/nature10146. [DOI] [PubMed] [Google Scholar]
- 2.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics-2015 update: a report from the american heart association. Circulation. 2015;131:e29–e322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 3.Yin Y, Li X, Sha X, et al. Early hyperlipidemia promotes endothelial activation via a caspase-1-sirtuin 1 pathway. Arteriosclerosis, thrombosis, and vascular biology. 2015;35:804–16. doi: 10.1161/ATVBAHA.115.305282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shao Y, Cheng Z, Li X, Chernaya V, Wang H, Yang XF. Immunosuppressive/anti-inflammatory cytokines directly and indirectly inhibit endothelial dysfunction- a novel mechanism for maintaining vascular function. Journal of hematology & oncology. 2014;7:80. doi: 10.1186/s13045-014-0080-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Combadiere C, Potteaux S, Rodero M, Simon T, Pezard A, Esposito B, Merval R, Proudfoot A, Tedgui A, Mallat Z. Combined inhibition of CCL2, CX3CR1, and CCR5 abrogates Ly6C(hi) and Ly6C(lo) monocytosis and almost abolishes atherosclerosis in hypercholesterolemic mice. Circulation. 2008;117:1649–57. doi: 10.1161/CIRCULATIONAHA.107.745091. [DOI] [PubMed] [Google Scholar]
- 6.Fang P, Zhang D, Cheng Z, Yan C, Jiang X, Kruger WD, Meng S, Arning E, Bottiglieri T, Choi ET, Han Y, Yang XF, Wang H. Hyperhomocysteinemia potentiates hyperglycemia-induced inflammatory monocyte differentiation and atherosclerosis. Diabetes. 2014;63:4275–90. doi: 10.2337/db14-0809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ait-Oufella H, Salomon BL, Potteaux S, et al. Natural regulatory T cells control the development of atherosclerosis in mice. Nat Med. 2006;12:178–80. doi: 10.1038/nm1343. [DOI] [PubMed] [Google Scholar]
- 8.Xiong Z, Yan Y, Song J, Fang P, Yin Y, Yang Y, Cowan A, Wang H, Yang XF. Expression of TCTP antisense in CD25(high) regulatory T cells aggravates cuff-injured vascular inflammation. Atherosclerosis. 2009;203:401–8. doi: 10.1016/j.atherosclerosis.2008.07.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Du F, Zhou J, Gong R, Huang X, Pansuria M, Virtue A, Li X, Wang H, Yang XF. Endothelial progenitor cells in atherosclerosis. Front Biosci. 2012;17:2327–49. doi: 10.2741/4055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li YF, Ren LN, Guo G, Cannella LA, Chernaya V, Samuel S, Liu SX, Wang H, Yang XF. Endothelial progenitor cells in ischemic stroke: an exploration from hypothesis to therapy. Journal of hematology & oncology. 2015;8:33. doi: 10.1186/s13045-015-0130-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li YF, Li RS, Samuel SB, Cueto R, Li XY, Wang H, Yang XF. Lysophospholipids and their G protein-coupled receptors in atherosclerosis. Frontiers in bioscience. 2016;21:70–88. doi: 10.2741/4377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Portman OW, Alexander M. Lysophosphatidylcholine concentrations and metabolism in aortic intima plus inner media: effect of nutritionally induced atherosclerosis. Journal of lipid research. 1969;10:158–65. [PubMed] [Google Scholar]
- 13.Wilensky RL, Shi Y, Mohler ER, 3rd, et al. Inhibition of lipoprotein-associated phospholipase A2 reduces complex coronary atherosclerotic plaque development. Nature medicine. 2008;14:1059–66. doi: 10.1038/nm.1870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goncalves I, Edsfeldt A, Ko NY, Grufman H, Berg K, Bjorkbacka H, Nitulescu M, Persson A, Nilsson M, Prehn C, Adamski J, Nilsson J. Evidence supporting a key role of Lp-PLA2-generated lysophosphatidylcholine in human atherosclerotic plaque inflammation. Arteriosclerosis, thrombosis, and vascular biology. 2012;32:1505–12. doi: 10.1161/ATVBAHA.112.249854. [DOI] [PubMed] [Google Scholar]
- 15.Steinbrecher UP, Parthasarathy S, Leake DS, Witztum JL, Steinberg D. Modification of low density lipoprotein by endothelial cells involves lipid peroxidation and degradation of low density lipoprotein phospholipids. Proceedings of the National Academy of Sciences of the United States of America. 1984;81:3883–7. doi: 10.1073/pnas.81.12.3883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kume N, Cybulsky MI, Gimbrone MA., Jr. Lysophosphatidylcholine, a component of atherogenic lipoproteins, induces mononuclear leukocyte adhesion molecules in cultured human and rabbit arterial endothelial cells. J Clin Invest. 1992;90:1138–44. doi: 10.1172/JCI115932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Erdogan A, Schaefer MB, Kuhlmann CR, Most A, Hartmann M, Mayer K, Renner FC, Schaefer C, Abdallah Y, Hoelschermann H, Schaefer CA. Activation of Ca2+ -activated potassium channels is involved in lysophosphatidylcholine-induced monocyte adhesion to endothelial cells. Atherosclerosis. 2007;190:100–5. doi: 10.1016/j.atherosclerosis.2006.02.035. [DOI] [PubMed] [Google Scholar]
- 18.Sugiyama S, Kugiyama K, Ogata N, Doi H, Ota Y, Ohgushi M, Matsumura T, Oka H, Yasue H. Biphasic regulation of transcription factor nuclear factor-kappaB activity in human endothelial cells by lysophosphatidylcholine through protein kinase C-mediated pathway. Arteriosclerosis, thrombosis, and vascular biology. 1998;18:568–76. doi: 10.1161/01.atv.18.4.568. [DOI] [PubMed] [Google Scholar]
- 19.Li X, Fang P, Mai J, Choi ET, Wang H, Yang XF. Targeting mitochondrial reactive oxygen species as novel therapy for inflammatory diseases and cancers. Journal of hematology & oncology. 2013;6:19. doi: 10.1186/1756-8722-6-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bulua AC, Simon A, Maddipati R, Pelletier M, Park H, Kim KY, Sack MN, Kastner DL, Siegel RM. Mitochondrial reactive oxygen species promote production of proinflammatory cytokines and are elevated in TNFR1-associated periodic syndrome (TRAPS). The Journal of experimental medicine. 2011;208:519–33. doi: 10.1084/jem.20102049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nakashima Y, Plump AS, Raines EW, Breslow JL, Ross R. ApoE-deficient mice develop lesions of all phases of atherosclerosis throughout the arterial tree. Arterioscler Thromb. 1994;14:133–40. doi: 10.1161/01.atv.14.1.133. [DOI] [PubMed] [Google Scholar]
- 22.Schmitz G, Ruebsaamen K. Metabolism and atherogenic disease association of lysophosphatidylcholine. Atherosclerosis. 2010;208:10–8. doi: 10.1016/j.atherosclerosis.2009.05.029. [DOI] [PubMed] [Google Scholar]
- 23.Weinberg SE, Sena LA, Chandel NS. Mitochondria in the regulation of innate and adaptive immunity. Immunity. 2015;42:406–17. doi: 10.1016/j.immuni.2015.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Watanabe N, Zmijewski JW, Takabe W, et al. Activation of mitogen-activated protein kinases by lysophosphatidylcholine-induced mitochondrial reactive oxygen species generation in endothelial cells. The American journal of pathology. 2006;168:1737–48. doi: 10.2353/ajpath.2006.050648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brookes PS, Yoon Y, Robotham JL, Anders MW, Sheu SS. Calcium, ATP, and ROS: a mitochondrial love-hate triangle. American journal of physiology Cell physiology. 2004;287:C817–33. doi: 10.1152/ajpcell.00139.2004. [DOI] [PubMed] [Google Scholar]
- 26.van de Stolpe A, van der Saag PT. Intercellular adhesion molecule-1. J Mol Med (Berl) 1996;74:13–33. doi: 10.1007/BF00202069. [DOI] [PubMed] [Google Scholar]
- 27.Bagher P, Segal SS. The mouse cremaster muscle preparation for intravital imaging of the microcirculation. Journal of visualized experiments : JoVE. 2011 doi: 10.3791/2874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ley K, Mestas J, Pospieszalska MK, Sundd P, Groisman A, Zarbock A. Chapter 11. Intravital microscopic investigation of leukocyte interactions with the blood vessel wall. Methods Enzymol. 2008;445:255–79. doi: 10.1016/S0076-6879(08)03011-5. [DOI] [PubMed] [Google Scholar]
- 29.Back M, Hansson GK. Anti-inflammatory therapies for atherosclerosis. Nature reviews Cardiology. 2015;12:199–211. doi: 10.1038/nrcardio.2015.5. [DOI] [PubMed] [Google Scholar]
- 30.Fraser H, Hislop C, Christie RM, Rick HL, Reidy CA, Chouinard ML, Eacho PI, Gould KE, Trias J. Varespladib (A-002), a secretory phospholipase A2 inhibitor, reduces atherosclerosis and aneurysm formation in ApoE−/− mice. Journal of cardiovascular pharmacology. 2009;53:60–5. doi: 10.1097/FJC.0b013e318195bfbc. [DOI] [PubMed] [Google Scholar]
- 31.Rosenson RS, Hislop C, Elliott M, Stasiv Y, Goulder M, Waters D. Effects of varespladib methyl on biomarkers and major cardiovascular events in acute coronary syndrome patients. Journal of the American College of Cardiology. 2010;56:1079–88. doi: 10.1016/j.jacc.2010.06.015. [DOI] [PubMed] [Google Scholar]
- 32.Serruys PW, Garcia-Garcia HM, Buszman P, et al. Effects of the direct lipoprotein-associated phospholipase A(2) inhibitor darapladib on human coronary atherosclerotic plaque. Circulation. 2008;118:1172–82. doi: 10.1161/CIRCULATIONAHA.108.771899. [DOI] [PubMed] [Google Scholar]
- 33.Nicholls SJ, Kastelein JJ, Schwartz GG, Bash D, Rosenson RS, Cavender MA, Brennan DM, Koenig W, Jukema JW, Nambi V, Wright RS, Menon V, Lincoff AM, Nissen SE. Varespladib and cardiovascular events in patients with an acute coronary syndrome: the VISTA-16 randomized clinical trial. Jama. 2014;311:252–62. doi: 10.1001/jama.2013.282836. [DOI] [PubMed] [Google Scholar]
- 34.White HD, Held C, Stewart R, et al. Darapladib for preventing ischemic events in stable coronary heart disease. The New England journal of medicine. 2014;370:1702–11. doi: 10.1056/NEJMoa1315878. [DOI] [PubMed] [Google Scholar]
- 35.O'Donoghue ML, Braunwald E, White HD, et al. Effect of darapladib on major coronary events after an acute coronary syndrome: the SOLID-TIMI 52 randomized clinical trial. Jama. 2014;312:1006–15. doi: 10.1001/jama.2014.11061. [DOI] [PubMed] [Google Scholar]
- 36.Soga T, Ohishi T, Matsui T, et al. Lysophosphatidylcholine enhances glucose-dependent insulin secretion via an orphan G-protein-coupled receptor. Biochemical and biophysical research communications. 2005;326:744–51. doi: 10.1016/j.bbrc.2004.11.120. [DOI] [PubMed] [Google Scholar]
- 37.Nguyen LN, Ma D, Shui G, Wong P, Cazenave-Gassiot A, Zhang X, Wenk MR, Goh EL, Silver DL. Mfsd2a is a transporter for the essential omega-3 fatty acid docosahexaenoic acid. Nature. 2014;509:503–6. doi: 10.1038/nature13241. [DOI] [PubMed] [Google Scholar]
- 38.Ballinger SW, Patterson C, Knight-Lozano CA, Burow DL, Conklin CA, Hu Z, Reuf J, Horaist C, Lebovitz R, Hunter GC, McIntyre K, Runge MS. Mitochondrial integrity and function in atherogenesis. Circulation. 2002;106:544–9. doi: 10.1161/01.cir.0000023921.93743.89. [DOI] [PubMed] [Google Scholar]
- 39.Zhang H, Luo Y, Zhang W, He Y, Dai S, Zhang R, Huang Y, Bernatchez P, Giordano FJ, Shadel G, Sessa WC, Min W. Endothelial-specific expression of mitochondrial thioredoxin improves endothelial cell function and reduces atherosclerotic lesions. The American journal of pathology. 2007;170:1108–20. doi: 10.2353/ajpath.2007.060960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wang Y, Wang GZ, Rabinovitch PS, Tabas I. Macrophage mitochondrial oxidative stress promotes atherosclerosis and nuclear factor-kappaB-mediated inflammation in macrophages. Circulation research. 2014;114:421–33. doi: 10.1161/CIRCRESAHA.114.302153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Takeshita S, Inoue N, Gao D, Rikitake Y, Kawashima S, Tawa R, Sakurai H, Yokoyama M. Lysophosphatidylcholine enhances superoxide anions production via endothelial NADH/NADPH oxidase. Journal of atherosclerosis and thrombosis. 2000;7:238–46. doi: 10.5551/jat1994.7.238. [DOI] [PubMed] [Google Scholar]
- 42.Jang C, Arany Z. Metabolism: Sweet enticements to move. Nature. 2013;500:409–11. doi: 10.1038/nature12549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Monet M, Gkika D, Lehen'kyi V, Pourtier A, Vanden Abeele F, Bidaux G, Juvin V, Rassendren F, Humez S, Prevarsakaya N. Lysophospholipids stimulate prostate cancer cell migration via TRPV2 channel activation. Biochimica et biophysica acta. 2009;1793:528–39. doi: 10.1016/j.bbamcr.2009.01.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.