Abstract
Background:
Rhinocerebral mucormycosis occurs in immunocompromised hosts with uncontrolled diabetes, solid organ transplants, and hematologic malignancies. Primary disease is in the paranasal sinuses but often progresses intracranially, via direct extension or angioinvasion. Rhinocerebral mucormycosis is rapidly fatal with a mortality rate of 85%, even when maximally treated with surgical debridement, antifungal therapy, and correction of underlying processes.
Methods:
We performed a retrospective chart review of patients with rhinocerebral mucormycosis from 2011 to 2014. These patients were analyzed for symptoms, surgical and medical management, and outcome. We found four patients who were diagnosed with rhinocerebral mucormycosis. All patients underwent rapid aggressive surgical debridement and were started on antifungal therapy on the day of diagnosis. Overall, we observed a mortality rate of 50%.
Results:
An early aggressive multidisciplinary approach with surgical debridement, antifungal therapy, and correction of underlying disease have been shown to improve survivability in rhinocerebral mucormycosis.
Conclusion:
A multidisciplinary approach to rhinocerebral mucormycosis with otolaryngology, neurosurgery, and ophthalmology, infectious disease and medical intensivists can help reduce mortality in an otherwise largely fatal disease. Even despite these measures, outcomes remain poor, and a high index of suspicion must be maintained in at-risk populations, in order to rapidly execute a multifaceted approach.
Keywords: Invasive fungus, Mucor, rhinocerebral mucormycosis, skull base, zygomycetes
INTRODUCTION
Mucorales is a fungal order in the subphylum mucormycotina that can cause mucormycosis, a fulminant, opportunistic infection in immunocompromised human hosts.[3] Mucor fungi and their spores are found in decaying vegetation and is ubiquitous in the soil and commonly isolated from the sinonasal cavities of healthy, immunocompetent hosts.[8] The fungus releases spores that are inhaled and access the central nervous system (CNS) via the respiratory tract.[4,8] CNS disease is the most prevalent manifestation of mucormycosis[8] with an overall mortality of 85%.[4]
Patients with a lapse in natural immunity, such as diabetes mellitus, hematologic malignancy, and immune suppression after organ transplantation are predisposed to Mucor infection.[1,2,4,5,7,8,9] Because the relative incidence of fungal sinusitis is low, a high-index of suspicion must be maintained in order to secure an early diagnosis, which has been shown to improve prognoses.[1] Rapid and extensive surgical debridement of the sinuses as well as initiation of antifungal therapy has been shown to reduce mortality.[1,4,8] Despite these aggressive measures, overall prognosis remains bleak.
We reviewed four cases of rhinocerebral mucormycosis treated at our institution with rapid surgical and medical multidisciplinary measures, and found an overall mortality rate of 50%, with survivors living over 18 months from the time of initial diagnosis without evidence of recurrent disease.
METHODS
We performed a retrospective chart review of the four patients with rhinocerebral mucormycosis admitted to our institution from 2011 to 2014. Their medical records were reviewed for basic demographic information, clinical presentation, exam and imaging findings, surgical procedures, medical antimicrobial therapy, and follow-up care. Due to the retrospective design of this case series, Institutional Review Board approval was not required.
RESULTS
From 2011 to 2014, four patients were admitted to the University of Arizona Medical Center with a diagnosis of rhinocerebral mucormycosis. Table 1 summarizes their clinical courses and outcomes. All four patients presented with some degree of headache, facial and orbital pain, with ophthalmologic symptoms ranging from pain, ptosis, and proptosis to ophthalmoplegia and blindness. All patients had a diagnosis of diabetes mellitus, while half also were immunosuppressed following renal transplants. The patients had magnetic resonance imaging [Figure 1] and computed tomography findings consistent with fulminant sinusitis, but fungal, specifically Mucor, sinusitis was diagnosed based on histopathology.
Table 1.
Patient demographics, presentation, and clinical course
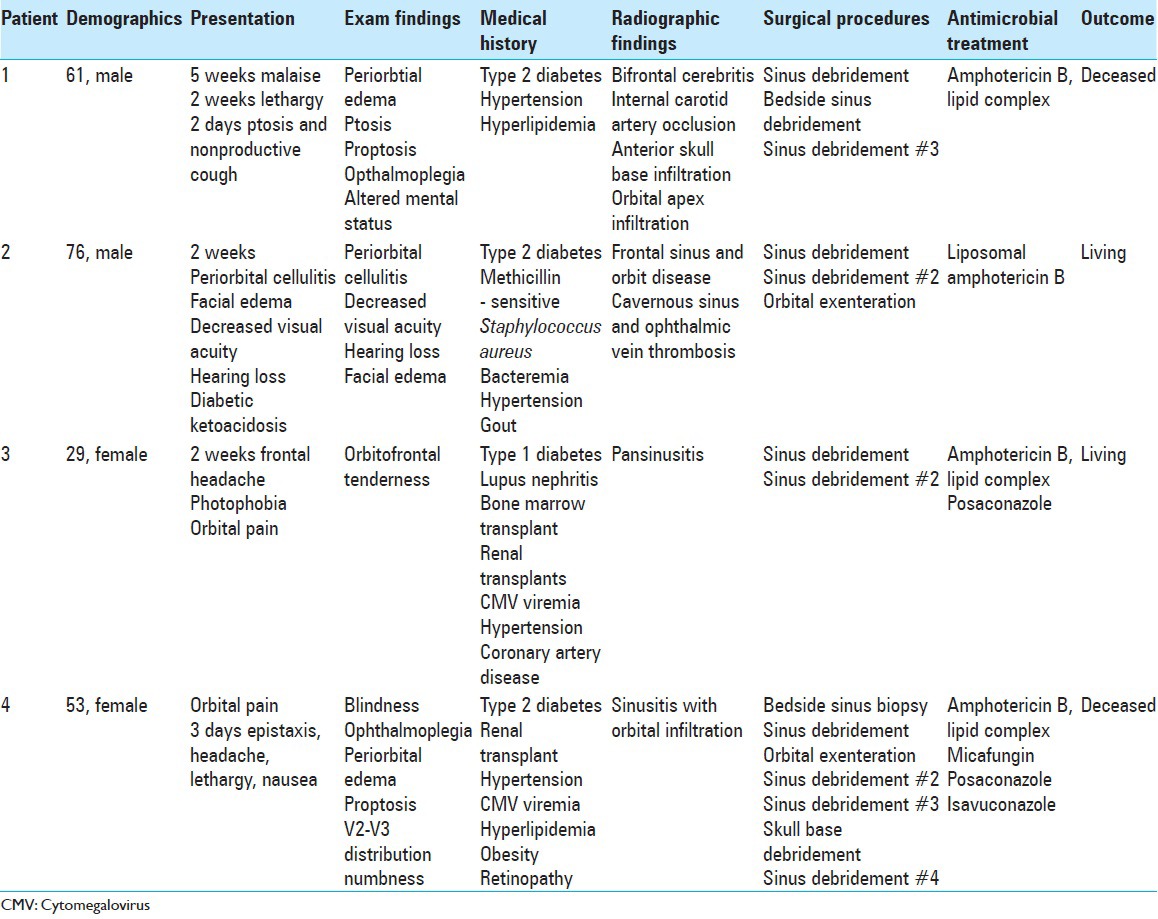
Figure 1.
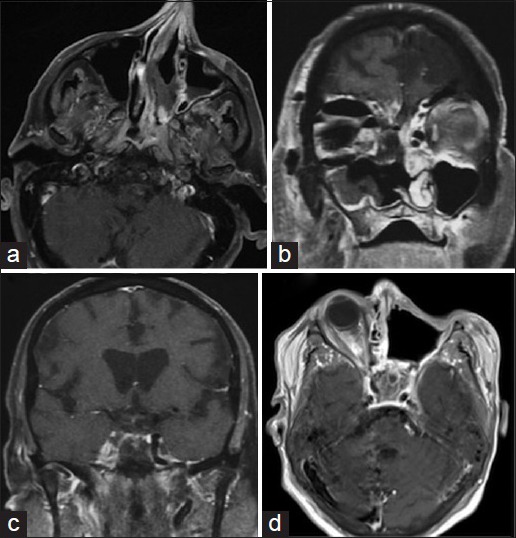
Axial and coronal T1-weighted, gadolinium enhanced, magnetic resonance imaging showing (a and b) sinonasal and (c and d) cavernous sinus invasive fungal infiltration
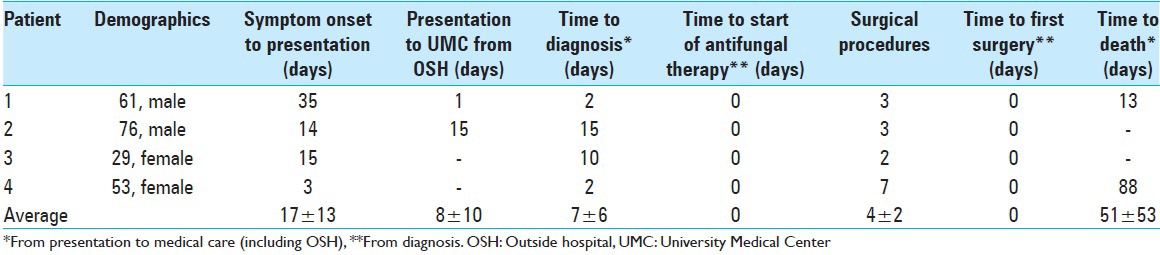
The patients all underwent several sinus debridements with otolaryngologists with intraoperative neurosurgical collaboration, and then subsequently were treated with amphotericin B. Half of the patients also underwent orbital exenteration of the infiltrated globe with ophthalmology. Ultimately 50% of the patients succumbed to their disease. Overall time to diagnosis was an average of 7 days. There was an average of four surgical debridements in the four patients. Both antifungal therapy and surgical debridement were launched on the day of diagnosis, and average prognosis after the presentation was approximately 51 days in the two patients who died [Table 2]. The other two patients have survived 18–24 months at the time of publication.
Table 2.
Timing of presentation and treatment
DISCUSSION
Rhinocerebral mucormycosis often occurs in patients who are immunocompromised, most commonly secondary to hematologic malignancy, diabetes mellitus, or iatrogenically following organ transplantation.[1,4,8] Patients with diabetes mellitus are predisposed to the rhinocerebral variant of mucormycotic infection.[1,4,7,8] With the increasing prevalence of diabetes in the US and around the world and ubiquitous nature of the filamentous fungi, an increased incidence of rhinocerebral mucormycosis, is expected.[1,5,7]
It is essential for the clinician to maintain a high index of suspicion in populations at risk, as early diagnosis can be life-saving.[4] Clinical symptoms usually begin as nonspecific malaise and headache, progressing to acute sinusitis, facial edema and pain, orbital symptoms, rhinorrhea, and eventual ophthalmoplegia, blindness, and lethargy.[8] This can make differentiation from the more common and less morbid bacterial sinusitis challenging, and often these patients fail antibiotic treatment prior to histopathologic diagnosis of fungal sinusitis and commencement of appropriate antimicrobial therapy.[1]
Mucor sinusitis can rapidly progress from isolated sinus involvement to direct orbital extension leading to pain, ptosis, proptosis, ophthalmoplegia, and eventual blindness.[1,8] Intracranial extension occurs in 80% of cases and causes encephalopathy, cerebritis, and angioinvasion leading to cavernous sinus thrombosis and cerebrovascular accidents.[2,5,8] Early diagnosis and subsequent treatment has been shown to portend higher survivability.[1,4,8]
A review if 929 reported cases of mucormycosis showed survivability was only 3% in patients who were untreated, none of whom had the rhinocerebral variant of the disease.[7] The mainstay of treatment remains aggressive surgical debridement, antifungal therapy, and reversal of underlying predisposing factors. Surgical debridement is often performed primarily by otolaryngologists with the involvement of ophthalmologists and neurosurgeons for orbital and intracranial extension, respectively. Often multiple, progressively aggressive debridements are required. Pharmacologic treatment should also be commenced rapidly with intravenous amphotericin B. Specifically, liposomal formulations of amphotericin B are preferred to classic preparations of the antifungal agent as they have more favorable side effect profiles and are far more tolerable in these already systemically compromised patients. Liposomal amphotericin B has also been shown to have fewer adverse reactions than amphotericin B lipid complex, though the latter is much less costly and, therefore, more readily available, though highly variable between organizations. Aside from discontinuation of therapy from intolerable side effects, no difference has been shown in efficacy between the three formulations of the drug.[6] Some studies have shown that addition of posaconazole as a second line agent might improve survivability in refractory cases.[9]
The key to management of this rapidly progressive fulminant disease is swift commencement of multidisciplinary treatments. These patients should be treated in tertiary care centers with the availability of otolaryngology, ophthalmology, neurosurgery, and infectious disease specialists so as to execute efficient and expeditious treatment. We feel that the rapid initiation of an aggressive multifaceted surgical and medical treatment regiment can confer an improved overall prognosis, and propose treating rhinocerebral mucormycosis as any other neurosurgical emergency.
CONCLUSION
Given the high morbidity and mortality of invasive rhino-orbito-cerebral fungal infections, a comprehensive and efficient multidisciplinary approach must be executed. This includes early and aggressive surgical debridement of disease in the paranasal sinuses, foramina of the skull base, and intracranial components, as well as initiation of a robust anti-fungal medical regimen with close follow-up. Despite aggressive measures, the overall mortality of rhinocerebral mucormycosis remains high, and future studies must focus on avenues of securing an early diagnosis, enacting aggressive multidisciplinary management, and pursuing new avenues of treatment.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Contributor Information
Sheri K. Palejwala, Email: spalejwala@email.arizona.edu.
Tirdad T. Zangeneh, Email: tzangeneh@deptofmed.arizona.edu.
Stephen A. Goldstein, Email: sgoldstein@oto.arizona.edu.
G. Michael Lemole, Email: mlemole@surgery.arizona.edu.
REFERENCES
- 1.Blyth CC, Gomes L, Sorrell TC, da Cruz M, Sud A, Chen SC. Skull-base osteomyelitis: Fungal vs.bacterial infection. Clin Microbiol Infect. 2011;17:306–11. doi: 10.1111/j.1469-0691.2010.03231.x. [DOI] [PubMed] [Google Scholar]
- 2.Chan LL, Singh S, Jones D, Diaz EM, Jr, Ginsberg LE. Imaging of mucormycosis skull base osteomyelitis. AJNR Am J Neuroradiol. 2000;21:828–31. [PMC free article] [PubMed] [Google Scholar]
- 3.Hibbett DS, Binder M, Bischoff JF, Blackwell M, Cannon PF, Eriksson OE, et al. A higher-level phylogenetic classification of the Fungi. Mycol Res. 2007;111(Pt 5):509–47. doi: 10.1016/j.mycres.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 4.Islam MN, Cohen DM, Celestina LJ, Ojha J, Claudio R, Bhattacharyya IB. Rhinocerebral zygomycosis: An increasingly frequent challenge: Update and favorable outcomes in two cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:e28–34. doi: 10.1016/j.tripleo.2007.06.014. [DOI] [PubMed] [Google Scholar]
- 5.Kolekar JS. Rhinocerebral mucormycosis: A retrospective study. Indian J Otolaryngol Head Neck Surg. 2015;67:93–6. doi: 10.1007/s12070-014-0804-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moen MD, Lyseng-Williamson KA, Scott LJ. Liposomal amphotericin B: A review of its use as empirical therapy in febrile neutropenia and in the treatment of invasive fungal infections. Drugs. 2009;69:361–92. doi: 10.2165/00003495-200969030-00010. [DOI] [PubMed] [Google Scholar]
- 7.Roden MM, Zaoutis TE, Buchanan WL, Knudsen TA, Sarkisova TA, Schaufele RL, et al. Epidemiology and outcome of zygomycosis: A review of 929 reported cases. Clin Infect Dis. 2005;41:634–53. doi: 10.1086/432579. [DOI] [PubMed] [Google Scholar]
- 8.Safar A, Marsan J, Marglani O, Al-Sebeih K, Al-Harbi J, Valvoda M. Early identification of rhinocerebral mucormycosis. J Otolaryngol. 2005;34:166–71. doi: 10.2310/7070.2005.04023. [DOI] [PubMed] [Google Scholar]
- 9.Yoon YK, Kim MJ, Chung YG, Shin IY. Successful treatment of a case with rhino-orbital-cerebral mucormycosis by the combination of neurosurgical intervention and the sequential use of amphotericin B and posaconazole. J Korean Neurosurg Soc. 2010;47:74–7. doi: 10.3340/jkns.2010.47.1.74. [DOI] [PMC free article] [PubMed] [Google Scholar]


