Abstract
To date, the impacts of school-based, peer-led nutrition education initiatives have not been summarized or assessed collectively. This review presents the current evidence, identifies knowledge gaps, and provides recommendations for future research. PubMed, Scopus, ERIC and Google Scholar were searched for refereed Canadian and American primary studies published between January 2000 and November 2013, following Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. Seventeen articles (11 programs) from Canada (24%) and the United States (76%) were identified. The results were summarized in terms of the study population, program design and main outcomes. Common outcome measures included healthy eating knowledge (n = 5), self-efficacy or attitudes towards healthy eating (n = 13), dietary measures (n = 9) and body mass index (n = 4), all of which tended to improve as a result of the programs. More research is needed to ascertain the effect of improvements in knowledge, self-efficacy and attitudes towards healthy eating on food behaviors. When evaluated, programs were generally well received, while the long-term maintenance of positive impacts was a challenge. Studies of sustainability and feasibility to promote long-term impact are a logical next step.
Introduction
Obesity is a powerful contributor to adverse health outcomes including type 2 diabetes, cardiovascular diseases, osteoarthritis, hypertension, gallbladder disease and several cancers [1, 2], and represents a significant economic burden to healthcare systems [3]. Youth have not been spared from the growing burden of excess weight. Measured rates of overweight and obesity from the 2011–2012 National Health and Nutrition Examination Survey (United States Centers for Disease Control standards) showed that 14.9% and 16.9% of American youth were overweight or obese, respectively [4]. Similarly, the 2009 to 2011 Canadian Health Measures Survey (World Health Organization standards) showed that 19.8% of Canadian youth aged 5–17 years were overweight and 11.7% were obese [5]. Without intervention, prevalence rates will likely continue to escalate.
Childhood is an opportune time to address the growing problem of excess weight. Overweight and obese youth are at a 2-fold or greater risk of becoming overweight or obese adults compared with their normal weight peers [6]. Among the myriad determinants of obesity in youth, dietary intake is a promising factor to target because it is potentially amenable to change [7]. Improving diets prior to and during adolescence is important because food behaviors in adolescence are a significant predictor of diet in the adult years [8]. Moreover, improvements in diet quality can result in significant health benefits in the absence of weight loss; even minor increases in fruit and vegetable intake can reduce cancer and coronary heart disease risk [9].
The forces that collectively influence the diets of youth are complex, and it is recognized that these should be targeted via multi-level ecological approaches [10]. That said, schools are ideal locales for childhood health promotion because they serve practically all children and youth [11]. Youth spend a large portion of their waking hours in school, presenting an ideal opportunity to support the development of healthy behaviors at an age when youth are beginning to form lifelong habits [6, 12]. Although efforts have been made to increase the availability of healthier food options in schools through policies such as the National School Lunch Program in the United States [13] and school-based food and beverage policies in Canada [14], it has been suggested that more action needs to be taken to improve nutrition education in schools [10]. Nutrition education would be complementary to positive changes in the physical environments of youth because it would provide them with the knowledge and skills to get the most out of these changes [10].
Peer-led approaches to health promotion for youth have been increasing in popularity since the 1990s [15] and are promising because peer interactions exert a powerful social influence on behavior change, especially during the onset of adolescence when peer acceptance is valued [16]. Although there is limited research on the use of peer-led strategies to improve dietary behaviors in youth, qualitative data show that peer-led nutrition education approaches are practical, feasible and well accepted in schools [15, 16].
To the authors’ knowledge, there exists no recent review of peer-led nutrition education programs for school-aged youth. Previous work reviewed a small number of studies (n = 13) that evaluated school health education programs and compared the effect of peers and adults delivering the same material [17]. The review showed that peer-led approaches may be as, if not more effective than adult-led ones, although this finding was hindered by methodological weaknesses [17]. A separate review of the impact of peer nutrition education initiatives on the dietary behaviors and health outcomes of Latino people living in the United States found that peer-led nutrition education can have a positive influence on dietary behaviors, health outcomes and nutrition knowledge [18]. The purpose of this review was to (i) summarize the results of published, refereed research investigating peer-led nutrition education programs in schools in the United States and Canada, and (ii) identify research gaps and provide recommendations for future research.
Methods
The literature search began in November 2013 and subsequent analyses were performed throughout 2014. The search of peer-reviewed, published literature reporting the results of peer-led school nutrition education programs for youth was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines [19, 20]. The protocol for the review was decided prior to the start of the study, and involved consideration for the study design and validity of methodology. PubMed (Medline), Scopus and Education Resources Information Center (ERIC) databases were selected because of their scope of coverage across disciplines in the life, health, biomedical and social sciences, as well as education. Google Scholar was searched for articles that were not indexed in the aforementioned databases, and reference lists were scanned to retrieve articles that were not previously identified. Records published prior to January 2000 were excluded to avoid historical biases related to changes in schools, demographics and technology in the previous 14 years. The online search strategy is shown in Box 1. Multi-component programs that incorporated a peer component (either same-age or older peers) were eligible, but only results relevant to peer influences were included for the purposes of this review. The setting was restricted to schools in Canada and the United States to limit heterogeneity in school systems.
Box I. Online search strategy
|
|
Full PubMed search strategy: (child* or kid* or youth* or adolescen* or teen*) and (nutrition or diet* or eating habit* or food habit* or feeding behavior*) and (peer* or peer led or peer-led) and (school*)
The articles retrieved were initially selected by title and abstract. The full text was then scanned to confirm the relevance and eligibility of each article for review. To ensure the transparency and accuracy of the search, the search process was repeated in May 2014 by two independent researchers. Any disagreements as to which studies should be included in the review were resolved via discussion until a consensus was reached.
Data from the studies were summarized in terms of the population, the study and program design, and main outcomes. Only quantitative data related to diet, measures of body size or composition, health indicators (e.g. blood pressure) or those describing the perceptions of the programs were reported. Although some programs reported results related to physical activity levels, these data were beyond the scope of this review and therefore were not reported. The main outcomes of interest were pre-to-post-program changes in the aforementioned variables. No further analyses were performed on the extracted data. With respect to the assessment of the risk of bias, the methodologies of the studies included in the review were accounted for. Based on the sum of the findings from studies included in the review, research gaps were identified and suggestions for areas of future research were described.
Results
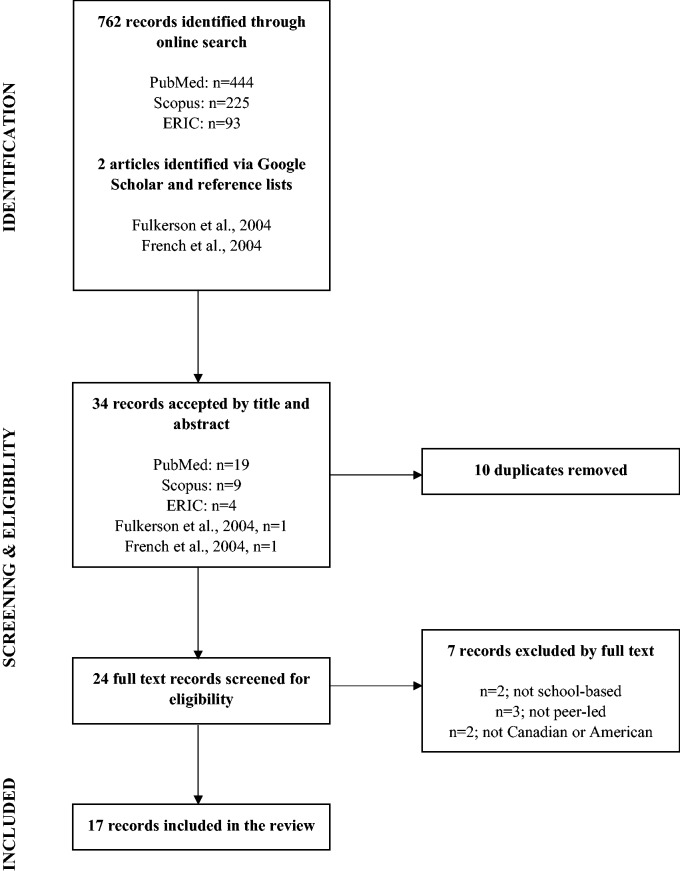
The search strategy resulted in the retrieval of 17 articles (Fig. 1) reporting results from 11 unique school-based, peer-led nutrition education initiatives (Table I). Among the articles reviewed, four (24%) evaluated programs implemented in Canadian schools and 13 (76%) evaluated programs in schools in the United States. The majority of studies (n = 12, 71%) evaluated outcomes among Kindergarten to grade 6 students, four (24%) evaluated outcomes among grade 7–12 students and one (6%) evaluated outcomes among Kindergarten to grade 12 students. The programs ranged from relatively small-scale initiatives (a minimum of n = 72; n = 1 school) [21–23] to large initiatives (a maximum of n = 3503) in many (n ≥ 20) schools [11, 24–27].
Fig. 1.
Flow diagram of study selection for inclusion in the review.
Table I.
Peer-led nutrition education programs for school-aged youth published between January 2000 and November 2013a
| Program nameb Reference | Population | Program design | Main outcomes |
|---|---|---|---|
|
>800 Kindergarten to grade 6 youth from five schools in California, United States |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
805 students from three middle schools in a primarily rural northeastern region in North Carolina, United States |
|
|
|
399 grade 7 students from a middle school in Los Angeles, California, United States |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
aBMI, body mass index; CATCH, coordinated approach to child health; TACOS, Trying Alternative Cafeteria Options in Schools; TEENS, Teens Eating for Energy and Nutrition at School.
bListed alphabetically.
Of the studies reviewed, 15 (88%) employed a pre-post design. Of these, 10 (67%) evaluated the active intervention phase and five (33%) evaluated the maintenance of the peer-led programs following the initial post-program evaluation (3 months to 2 years). Most studies (n = 15, 88%) used a control group to ascertain the effects of the program. Of these, three (20%) used non-participants from the same school and 12 (80%) used nearby non-participating schools as controls. A variety of outcome measures were used, including program satisfaction, behavior change constructs, self-esteem and body image, self-reported diet and health behavior changes, anthropometric measures (e.g. body mass index [BMI], waist circumference), and cafeteria sales and promotions.
The four studies that reported on satisfaction collectively showed that these types of programs were well received by students, staff and parents [15, 47–48]. All 13 studies that evaluated self-efficacy, knowledge, intentions and attitudes related to health behaviors showed improvement at program completion [11, 21, 23, 24, 27–29, 32, 37, 45–47, 50]. Two studies also reported improvements in self-esteem [37, 49], and while one study reported an improvement in body image over time, this improvement did not differ from that in the control group [37]. Of the studies that used diet or health behavior change as an outcome measure (n = 13), 11 (85%) found improvement in these variables immediately post-program. Changes included increases in fruit and vegetable intake [24, 30, 42], reductions in sugar-sweetened beverage intake [22, 31], reductions in fat intake [11, 38] and improvements in self-reported habit and behavior scores [21, 23, 27, 46]. These changes tended not to be maintained when longer-term impacts (i.e. 3 months to 2 years) were assessed [11, 22, 24, 26].
Results were promising in the four studies that investigated anthropometric measures as a program outcome, revealing either decreases in BMI z-scores or percentiles, expected changes in BMI related to normal growth, or increases that were less than in the control group [21, 23, 37, 47]. A significant difference in blood pressure was reported in one study where increases were less among participants compared with controls [37]. The study also noted a decrease in waist circumference among program participants [37]. Three studies investigated the dose-response relationship for varying levels of involvement in the Teens Eating for Energy and Nutrition at School (TEENS) and Trying Alternative Cafeteria Options in School (TACOS) programs [24, 26, 28], unanimously finding that the highest dose had the greatest impact on food choices and health behaviors.
Discussion
Knowledge, self-efficacy and attitudes
The current review found that peer-led school nutrition education programs have the potential to improve knowledge, self-efficacy and attitudes towards healthy eating, but more research is needed to determine the impact of these changes on diet quality. Social cognitive theory suggests that outcome expectations and self-efficacy are key determinants of change in health behaviors [32]. Thus, improvements in knowledge, along with the enhancement of self-efficacy to change one’s health habits, may address important barriers to making healthier choices.
Despite the promising findings, it is recognized that the diets of youth are affected at multiple levels of influence. These include individual factors, as well as social, physical and macro-level environments; improvements in knowledge and attitudes are not necessarily sufficient to provoke improved dietary habits [10, 33]. Future research aimed at determining the extent to which such improvements may influence diet in the context of peer-based school nutrition programs would be of interest, as the only study investigating knowledge, self-efficacy or attitudes towards healthy eating in addition to dietary intake did not explore the relationship between these variables [11]. Further, the use of validated tools to strengthen results must be stressed given that six [11, 27, 29, 42, 45, 47] out of 12 studies reporting self-efficacy or attitudes did not indicate the use of validated tools to measure outcomes.
Dietary intake
Of the studies investigating self-reported dietary intake, findings were overwhelmingly positive; all but one of the studies [28] that examined vegetable and fruit consumption reported at least some improvement among those exposed to the program. The importance of increasing vegetable and fruit intake is underscored by the fact that in Canada, only about 50% of girls and <40% of boys aged 12 years or older consume five or more servings of vegetables and fruit daily [34]. Five servings already falls below the recommendations set by Canada’s Food Guide, a Health Canada publication that outlines a pattern of eating associated with reducing the risk of chronic disease and optimizing overall health [35]. A similar trend has been seen in the United States, where only about a third of adults, and even fewer secondary school students, meet daily recommendations for vegetable and fruit intake [36].
One program was associated with an increase in the mean consumption of ‘nutritious foods’ [37] and another with a decrease in mean sugary beverage consumption [22]. This is promising because sugary beverages, particularly in the form of soft drinks, have been associated with a number of adverse health outcomes including weight gain [38], dental caries, and an inadequate intake of vitamins and minerals [39]. Moreover, an increase in soft drink intake is associated with a decrease in milk intake in adolescence [40], suggesting that instances of soft drink consumption could represent lost opportunities for milk, calcium and vitamin D intake, nutrients associated with achievement of peak bone mass [41]. Although the TACOS studies found the program to be associated with significant increases in the sales of lower-fat food items in school cafeterias, it would be of interest in future studies to investigate the impact of the program on dietary intake. Future research should also ensure that validated tools are used to assess diet. Although many studies reporting dietary intake as an outcome indicated the use of measurement tools that were either validated [23, 24, 28, 37, 46] or tested and revised [22], this was not the case in three of the studies [11, 29, 31].
Anthropometric measures
The only consistent anthropometric result was that participants in the intervention group saw either a significant reduction or a lesser increase in some measure of BMI (including z-scores and percentiles) compared with controls. Notably, all studies that described the process of obtaining BMI measures reported using measured (rather than self-reported) values of height and weight [21, 23, 37]. The BMI outcomes were surprising, considering the short time frame of most of the studies (<1 year) and the fact that the school is only one of the many environments that influence choices (e.g. diet, physical activity) that may lead to changes in BMI. Although the results show promise, longer-term follow-up is needed to determine if the BMI changes seen would be sustained over time, or if attenuation effects would occur. It remains likely that peer-led programs, while valuable, would be more effective in achieving clinically significant BMI changes among the population if accompanied by policies and programs aimed at multiple levels of influence (e.g. family, public policy) beyond the school environment.
Dose-response effects
Of particular interest for the current review was the significance of peers in the positive effects resulting from the reported initiatives. Three studies of two distinct programs (TEENS and TACOS) explicitly distinguished between various participation levels. In both cases, the addition of the peer-led component to other program activities resulted in a greater impact (more improvement) in outcome measures compared with lower-dose versions that excluded peers. Similarly, the ‘Youth Can’ program was compared with a control group that received all other program components except for peer involvement [42]. Only the peer intervention group saw improvements in vegetable and fruit intake, suggesting that the peer influence provided additional benefits. This is consistent with evidence on preventing and reducing tobacco and other forms of drug use, where peers tend to have a greater impact than adults [17, 43], perhaps because peer influence and acceptance is a particularly powerful force of social influence during adolescence [16].
The use of peers in health education is beneficial not just to program recipients, but also to the peer leaders themselves, who have reported improvements in healthy eating knowledge, consumption of healthier foods and confidence in leadership skills [24]. However, there remains limited insight into the impact of same-age versus older peers on program recipients. With consideration for positive impacts being found across studies using peers of all ages and the heterogeneity in outcome measures, the impact of same-age peers versus older peers could not be teased apart. Even in the one study that included two intervention groups (older versus same-aged peers), differences could not be assessed because the same-aged peer group also included older peers [22]. Future studies aimed at addressing this knowledge gap would be of interest.
Methodological considerations
To draw conclusions about program impacts, most articles (n = 12, 71%) reported a control group that received either no intervention or a lower dose of the intervention without the inclusion of peers. Control groups were often comparable youth of the same age from nearby schools, allowing for the inference of cause-and-effect. However, only 10 of 17 articles (59%) reported random assignment of intervention and control conditions [11, 15, 21, 24–29, 46]. There were cases where some members of the control group attended the same school as the intervention group, meaning some diffusion of the intervention to non-participating controls may have occurred. In such cases, it is possible that the magnitude of the effect of an intervention was underestimated. Future studies should aim to minimize these methodological weaknesses, though the evaluation of programs that may be of benefit to students should not be discouraged should this not be possible. Furthermore, the importance of using validated measures to strengthen findings even in a well-designed study must be noted, as there were several cases where outcomes were not measured using validated tools.
Though the review was limited to programs in Canada or the United States, the populations studied varied with respect to age, heterogeneity and ethnicity. As such, peer-led programs can likely be successfully adapted to a variety of target audiences, though programs must ideally be tailored to the population of interest to maximize the possibility of a positive impact. Notably, two of the programs reviewed included students in the planning and design of the program, although the advantages of this involvement were not assessed. Assessments of such advantages would be of interest in the future, as involving students in program development could help ensure the program meets their needs and desires for change, while also identifying potential problems from the perspectives of students [44].
Feasibility, sustainability and maintenance of program impact
Even a program that has been demonstrated to be effective in changing dietary behavior may not have utility for health promotion if it is not feasible or practical to implement and maintain. Fortunately, in the studies that evaluated perceptions of parents, students and staff, peer-led nutrition education programs were positively received and well accepted [15, 45–47]. This is important because overweight and obesity are complex problems requiring long-term solutions, so programs need to be sustainable in order to make a lasting impact on behavior. Of the studies that conducted follow-up assessment (n = 3), all reported a disappearance of at least one significant positive outcome over time. This is consistent with the literature on school-based obesity interventions where short-term positive results tended not to persist over longer time periods [48]. When resources allow, longer-term follow-ups assessing the maintenance of improvements attributed to peer-led school nutrition initiatives would be of interest.
With the numerous opportunities to improve health behaviors in youth in the school environment, there are also a number of potential hindrances to the long-term success of school-based health promotion programs, including budget constraints and environmental barriers [48, 49]. Budget constraints are a concern because they may not allow a program to be adequately implemented as intended [49], meaning that even a well-designed program will not be utilized to their fullest potential. Budget constraints may also act as catalysts for environmental barriers, as limited funding may prevent schools from building a supportive environment through changes such as improvements in the availability of healthier food options [48]. With respect to peer-led nutrition education programs, further investigation into the barriers, challenges, opportunities and supports to the sustainability of the initiatives from the perspectives of students, teachers, staff and administrators would allow for the development of program designs that can be feasibly maintained and continuously evaluated, updated and improved.
Limitations
Because few studies investigated dietary intake and many focused solely on constructs such as self-efficacy or knowledge, the effect of peer-led school nutrition education programs on diet quality cannot be established with certainty. Further, as only Canadian and American studies were included, the findings cannot be generalized beyond these countries. Although the studies reviewed included a variety of different populations (e.g. rural, urban, Indigenous), needs assessments and formative evaluations should help guide the development of initiatives for unique populations. Finally, although it is possible that relevant studies may have been overlooked, the fact that the search was replicated by two independent researchers has reduced this possibility.
Conclusion
Based on the evidence reviewed, peer-led nutrition education programs in schools have the potential to improve knowledge, self-efficacy and attitudes towards healthy eating, at least in the short-term. Though few dose-response studies exist, those available demonstrate that the peer influence is a contributor to improved program outcomes compared with programs that did not include peer guidance. More studies are needed to investigate the impact of improvements in behavior change constructs attributable to the programs on dietary behavior. Further, care should be taken to ensure program sustainability, feasibility and practicality in order to promote long-term impact. Continuous program evaluation and the use of qualitative methodology to understand the perspectives of program staff, teachers, parents and students are recommended.
Funding
This work was supported by Frederick Banting and Charles Best Canada Graduate Scholarships from the Canadian Institutes of Health Research, and President's Graduate Scholarships from the University of Waterloo [to AG and MG]. The funders played no role in the design of the study, the data extraction, the analysis or interpretation of the results, nor in the writing of the manuscript or decision to submit it for publication.
Conflict of interest statement
None declared.
References
- 1.Tjepkema M. Adult obesity. Health Rep 2006; 17: 9–25. [PubMed] [Google Scholar]
- 2.Guh DP, Zhang W, Bansback N, et al. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health 2009; 9: 88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Withrow D, Alter DA. The economic burden of obesity worldwide: a systematic review of the direct costs of obesity. Obes Rev 2011; 12: 131–41. [DOI] [PubMed] [Google Scholar]
- 4.Ogden CL, Carroll MD, Kit BK, et al. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014; 311: 806–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roberts KC, Shields M, de Groh M, et al. Overweight and obesity in children and adolescents: results from the 2009 to 2011 Canadian Health Measures Survey. Health Rep 2012; 23: 37–41. [PubMed] [Google Scholar]
- 6.Singh AS, Mulder C, Twisk JWR, et al. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obesity Rev 2008; 9: 474–88. [DOI] [PubMed] [Google Scholar]
- 7.Craigie AM, Lake AA, Kelly SA, et al. Tracking of obesity-related behaviours from childhood to adulthood: a systematic review. Maturitas 2011; 70: 266–84. [DOI] [PubMed] [Google Scholar]
- 8.Lake AA, Mathers JC, Rugg-Gunn AJ, et al. Longitudinal change in food habits between adolescence (11–12 years) and adulthood (32–33 years): the ASH30 Study. J Public Health 2006; 28: 10–6. [DOI] [PubMed] [Google Scholar]
- 9.Glasson C, Chapman K, Gander K, et al. The efficacy of a brief, peer-led nutrition education intervention in increasing fruit and vegetable consumption: a wait-list, community-based randomised controlled trial. Public Health Nutr 2012; 15: 1318–26. [DOI] [PubMed] [Google Scholar]
- 10.Story M, Kaphingst KM, Robinson-O’Brien R, et al. Creating healthy food and eating environments: policy and environmental approaches. Annu Rev Public Health 2008; 29: 253–72. [DOI] [PubMed] [Google Scholar]
- 11.Forneris T, Fries E, Meyer A, et al. Results of a rural school-based peer-led intervention for youth: goals for health. J School Health 2010; 80: 57–65. [DOI] [PubMed] [Google Scholar]
- 12.Lake AA, Adamson AJ, Craigie AM, et al. Tracking of dietary intake and factors associated with dietary change from early adolescence to adulthood: the ASH30 study. Obes Facts 2009; 2: 158–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.United States Department of Agriculture. National School Lunch Program (2013). Available at: http://www.fns.usda.gov/sites/default/files/NSLPFactSheet.pdf. Accessed: July 2014.
- 14.Centre for Science in Public Interest. School Nutrition Policies Across Canada (2007). Available at: http://www.cspinet.org/canada/pdf/makingthegrade_1007.pdf. Accessed: July 2014.
- 15.Story M, Lytle LA, Birnbaum AS, et al. Peer-led, school-based nutrition education for young adolescents: feasibility and process evaluation of the TEENS study. J School Health 2002; 72: 121–7. [DOI] [PubMed] [Google Scholar]
- 16.Venditti EL, Elliot DL, Faith MS, et al. Rationale, design and methods of the HEALTHY study behavior intervention component. Int J Obes 2009; 33: 544–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mellanby AR, Rees JB, Tripp JH. Peer-led and adult-led school health education: a critical review of available comparative research. Health Educ Res 2000; 15: 533–45. [DOI] [PubMed] [Google Scholar]
- 18.Pérez-Escamilla R, Hromi-Fiedler A, Vega-López S, et al. Impact of peer nutrition education on dietary behaviors and health outcomes among Latinos: a systematic literature review. J Nutr Educ Behav 2008; 40: 208–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 2009; 6: e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6: e1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smith LH. Piloting the use of teen mentors to promote a healthy diet and physical activity among children in Appalachia. J Spec Pediatr Nurs 2011; 16: 16–26. [DOI] [PubMed] [Google Scholar]
- 22.Lo E, Coles R, Humbert ML, et al. Beverage intake improvement by high school students in Saskatchewan, Canada. Nutr Res 2008;28:144–50. [DOI] [PubMed] [Google Scholar]
- 23.Stock S, Miranda C, Evans S, et al. Healthy Buddies: a novel, peer-led health promotion program for the prevention of obesity and eating disorders in children in elementary school. Pediatrics 2007;120:e1059–68. [DOI] [PubMed] [Google Scholar]
- 24.Birnbaum AS, Lytle LA, Story M, et al. Are differences in exposure to a multicomponent school-based intervention associated with varying dietary outcomes in adolescents?. Health Educ Behav 2002;29:427–43. [DOI] [PubMed] [Google Scholar]
- 25.French SA, Story M, Fulkerson JA, et al. An environmental intervention to promote lower-fat food choices in secondary schools: Outcomes of the TACOS study. Am J Public Health 2004;94:1507–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fulkerson JA, French SA, Story M, et al. Promotions to increase lower-fat food choices among students in secondary schools: description and outcomes of TACOS (Trying Alternative Cafeteria Options in Schools). Public Health Nutr 2003;7:665–74. [DOI] [PubMed] [Google Scholar]
- 27.Hamdan S, Story M, French SA, et al. Perceptions of adolescents involved in promoting lower-fat foods in schools: associations with level of involvement. J Am Diet Assoc 2005; 105: 247–51. [DOI] [PubMed] [Google Scholar]
- 28.Lytle LA, Murray DM, Perry CL, et al. School-based approaches to affect adolescents’ diets: results from the TEENS study. Health Educ Behav 2004; 31: 270–87. [DOI] [PubMed] [Google Scholar]
- 29.Wilson DB, Jones RM, McClish D, et al. Fruit and vegetable intake among rural youth following a school-based randomized controlled trial. Prev Med 2012; 54: 150–6. [DOI] [PubMed] [Google Scholar]
- 30.Wilson N, Minkler M, Dasho S, et al. Getting to social action: the Youth Empowerment Strategies (YES!) project. Health Promot Pract 2008; 9: 395–403. [DOI] [PubMed] [Google Scholar]
- 31.Bogart LM, Elliott MN, Uyeda K, et al. Preliminary healthy eating outcomes of SNaX, a pilot community-based intervention for adolescents. J Adolesc Health 2011; 48: 196–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bandura A. Health promotion by social cognitive means. Health Educ Behav 2004; 31: 143–64. [DOI] [PubMed] [Google Scholar]
- 33.Croll JK, Neumark-Sztainer D, Story M. Healthy eating: what does it mean to adolescents?. J Nutr Educ 2001; 33: 193–8. [DOI] [PubMed] [Google Scholar]
- 34.Statistics Canada. Fruit and vegetable consumption (2010). Available at: http://www.statcan.gc.ca/pub/82–229-x/2009001/deter/fvc-eng.htm#n7. Accessed: July 2014.
- 35.Health Canada. Food Guide Basics (2007). Available at: http://www.hc-sc.gc.ca/fn-an/food-guide-aliment/basics-base/quantit-eng.php. Accessed: July 2014.
- 36.Centers for Disease Control and Prevention. Majority of Americans not Meeting Recommendations for Fruit and Vegetable Consumption (2009). Available at: http://www.cdc.gov/media/pressrel/2009/r090929.htm. Accessed: July 2014.
- 37.Ronsley R, Lee AS, Kuzeljevic B. Healthy Buddies reduces body mass index z-score and waist circumference in Aboriginal children living in remote coastal communities. J Sch Health 2013; 83: 605–13. [DOI] [PubMed] [Google Scholar]
- 38.Malik VS, Schulze MB, Hu FB. Intake of sugar-sweetened beverages and weight gain: a systematic review. Am J Clin Nutr 2006; 84: 274–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vartanian LR, Schwartz MB, Brownell KD. Effects of soft drink consumption on nutrition and health: a systematic review and meta-analysis. Am J Public Health 2007; 97: 667–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rampersaud GC, Bailey LB, Kauwell GP. National survey beverage consumption data for children and adolescents indicate the need to encourage a shift toward more nutritive beverages. J Am Diet Assoc 2003; 103: 97–100, last accessed July 2014. [DOI] [PubMed] [Google Scholar]
- 41.Caroli A, Poli A, Ricotta D, et al. Invited review: dairy intake and bone health: a viewpoint from the state of the art. J Dairy Sci 2011; 94: 5249–62. [DOI] [PubMed] [Google Scholar]
- 42.Jones S, Spence M, Hardin S, et al. Youth Can! Results of a pilot trial to improve the school food environment. J Nutr Edu 2011; 43: 284–7. [DOI] [PubMed] [Google Scholar]
- 43.Black DR, Tobler NS, Sciacca JP. Peer helping/involvement: an efficacious way to meet the challenge of reducing alcohol, tobacco, and other drug use among youth? J Sch Health 1998; 68: 87–93. [DOI] [PubMed] [Google Scholar]
- 44.Nichols L. Participatory program planning: including program participants and evaluators. Eval Program Plann 2002; 25: 1–14. [Google Scholar]
- 45.Bergmann L, Clifford D, Wolff C. Edutainment and teen modeling may spark interest in nutrition and physical activity in elementary school audiences. J Nutr Educ Behav 2010; 42: 139–41. [DOI] [PubMed] [Google Scholar]
- 46.Campbell AC, Barnum D, Ryden V, et al. The effectiveness of the implementation of Healthy Buddies, a school-based, peer-led health promotion program in elementary schools. Can J Diabetes 2012; 36: 181–6. [Google Scholar]
- 47.Thomas AB, Ward E. Peer power: how Dare County, North Carolina, is addressing chronic disease through innovative programming. J Public Health Manag Pract 2006; 12: 462–7. [DOI] [PubMed] [Google Scholar]
- 48.Shaya FT, Flores D, Gbarayor CM, et al. School-based obesity interventions: a literature review. J Sch Health 2008; 78: 189–96. [DOI] [PubMed] [Google Scholar]
- 49.Deschesnes M, Martin C, Hill AJ. School-based obesity interventions: a literature review. J Sch Health 2008; 78: 189–96. [DOI] [PubMed] [Google Scholar]
- 50.French SA, Story M, Fulkerson JA, et al. An environmental intervention to promote lower-fat food choices in secondary schools: outcomes of the TACOS study. Am J Public Health 2004; 94: 1507–12. [DOI] [PMC free article] [PubMed] [Google Scholar]