Abstract
Introduction and objectives
To determine how robotic prostatectomy affects practice patterns of urologists, we examined the case volume characteristics among certifying urologists for the surgical treatment of prostate cancer. We hypothesized that the utilization of open and robotic prostatectomy as well as lymph node dissection changed dynamically over the last 10 years.
Methods
Six month case log data of certifying urologists from 2003 to 2013 were obtained for the American Board of Urology. Cases were identified using CPT codes for open radical prostatectomy (ORP) and laparosopic or robotic-assisted laparoscopic prostatectomy (RALP) with a corresponding diagnosis of prostate cancer as defined by ICD-9 code 185.0.
Results obtained
A total of 6,563 urologists submitted case logs, of which 68% (4470/6563) reported performing at least one radical prostatectomy (RP), totaling 46,030 RPs logged. There was a 376% increase in the performance of RALP over the study period with robotic volume increasing from 22% of all RP in 2003 to 85% in 2013. Among surgeons performing ORP, the median number performed was 2; of surgeons who performed RALP, the median number performed was 8 (p < 0.001). 39% of surgeons logging ORP performed two or fewer RP while 19% of surgeons who performed RALP performed 2 or less RP (p < 0.001). The highest volume robotic surgeons (top 10% surgical volume) performed 41% of all RALP with the highest performing robotic surgeon recording 658 prostatectomies over 6 months. Oncologists represented 4.1% of all surgeons performing RP and performed 15.1% of all RP (p < 0.001); general urologists performed the majority of RP (57.8%). When performed open, there was no influence of surgeon specialty on the performance of lymph node dissection (LND); if performed robotically, oncologists were significantly more likely to perform LND compared to general surgeons (47% vs. 25.9% respectively, p < 0.001).
Conclusions
Robotic prostatectomies are performed five-times more commonly than open prostatectomy and represent 85% of all RP performed by board-certified urologists in 2013. Compared to RALP, ORP are significantly more likely to be performed by lower volume surgeons. Oncologists perform a higher relative percentage of RPs and are significantly more likely to perform LND if performed robotically when compared to general urologists.
Keywords: Prostate cancer, robotic prostatectomy, practice patterns, american board of urology
Introduction
Prostate cancer (PC) is the most commonly diagnosed non-cutaneous malignancy among men in the United States[1]. An estimated 240,000 men are diagnosed each year and approximately one-third of these men will go on to receive treatment with radical prostatectomy (RP).[2] Historically, open RP was the gold standard for surgical treatment of prostate cancer, yet over the last fifteen years the introduction of robotic-assisted (RA) surgical technologies has changed the surgical approach to radical prostatectomy.[3]
Although the absolute proportion of RPs performed robotically is not known, estimates have ranged from 45% to 80% in the US today.[4] Despite the rapid expansion and dissemination of RALP, the effect of the adoption of robotic surgery on physician practice patterns remains undescribed. Therefore, we aim to analyze clinician practice patterns among urologists performing radical prostatectomies in the United States utilizing case-log data from urologists certifying with the American Board of Urology.
Methods
The American Board of Urology (ABU) is a surgical specialty board organized to facilitate the improvement of standards, promote competency, and improve monitoring and standards of education in the field of urology. Urologists may apply for certification by the ABU after completing residency and demonstrating an appropriate level of knowledge and expertise in the management of urological conditions.[5, 6]
Recertification is necessary every ten years for those urologists initially certifying after 1985. An important portion of certification is the completion of surgical case log reflecting a consecutive six-month period prior to certification. These logs include both patient demographics (age, gender, diagnosis code) and surgeon-specific characteristics (surgeon age, certification cycle, practice type, and state of practice). Surgeons also have the option to report a sub-specialization in one of five domains (oncology, endourology, pediatrics, andrology and female urology) or identify themselves as general urologists.
Surgical procedures are identified by their corresponding Current Procedural Terminology code. The codes 55810 and 55840 were used to identify open radical prostatectomies (ORP) without pelvic lymph node dissection (PLND). The codes 55812, 55815, 55842, and 55845 were used to identify ORP with PLND. The code 55866 was used to identify laparoscopic or robotic assisted radical prostatectomies (RALP). CPT coding cannot differentiate conventional laparoscopic prostatectomy from robotic-assisted techniques; therefore, when referring to the robotic RP cohort this population will include a small number of laparoscopic RP cases without robotic assistance. Previous studies from 2008–2009 confirm that traditional laparoscopic RP represent less than 1% of all RP.[7] The additional codes 38570-38572 were utilized to identify RALP with concurrent PLND. All cases were associated with the ICD-9 code designation for prostate cancer (185.0). No cases were coded with female patient gender or patient age < 18 years.
Case logs are received from the ABU are reported as six-month representation of individual surgeon practice volume. We analyzed case logs from 2003–2013 for trends in the performance of RP for treatment of prostate cancer associated with certification cycle, submission year, state, practice type (academic affiliation versus private practice) and surgical case volume using Fisher's exact test and students t-test. 2013 was a partially-collected year at the time of analysis, and was therefore excluded from overall yearly volume estimations but was utilized to compare individual surgeon volume. For all statistical analyses, P < 0.05 was considered statistically significant. Analysis was performed using SPSS®, version 21.
Results
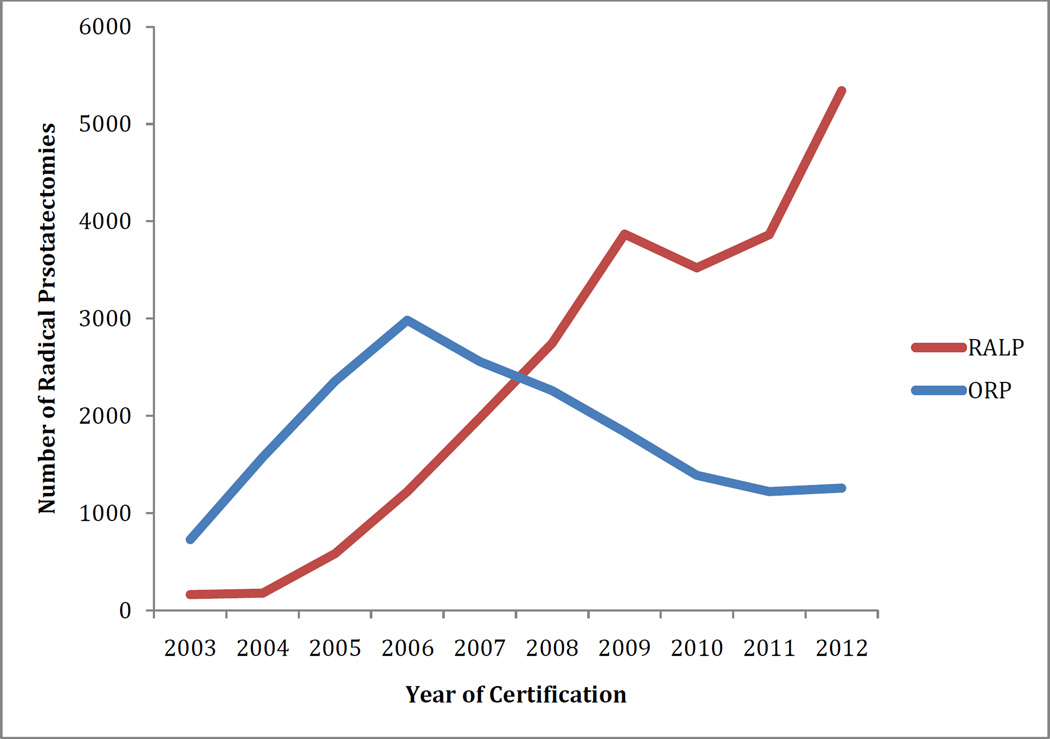
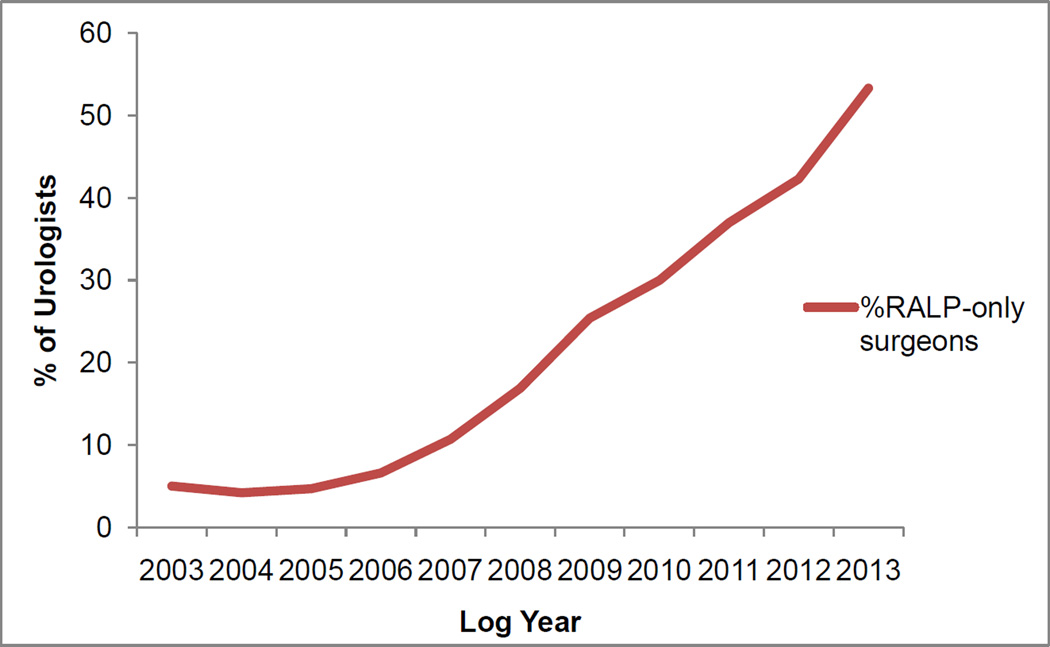
A total of 6,563 urologists submitted case logs over from 2003 to 2012 (figure 1). Among all urologists submitting case logs, 68% (4,470/6,563) reported performing at least one radical prostatectomy (RP) over the six-month certification period, with a total of 46,707 RPs captured within the database (27,737 RALP, 18,970 ORP). 3,536 of the 4,470 urologist reported performing an ORP whereas 1,863 urologists reported performing a RALP (figure 2). There was a 376% increase in the performance of RALP over the study period with robotic volume increasing from 22% of all RP in 2003 to 85% in 2013 (figure 1). The proportion of surgeons performing exclusively RALP increased from 5.1% in 2003, to 53.3% (271/508) in 2013, while the percentage of surgeons performing exclusively ORP decreased from 88% (200/228) to 29.5% (150/508), figure 4.
Figure 1.
Changing trends in surgical management of prostate cancer over time (2003–2012)
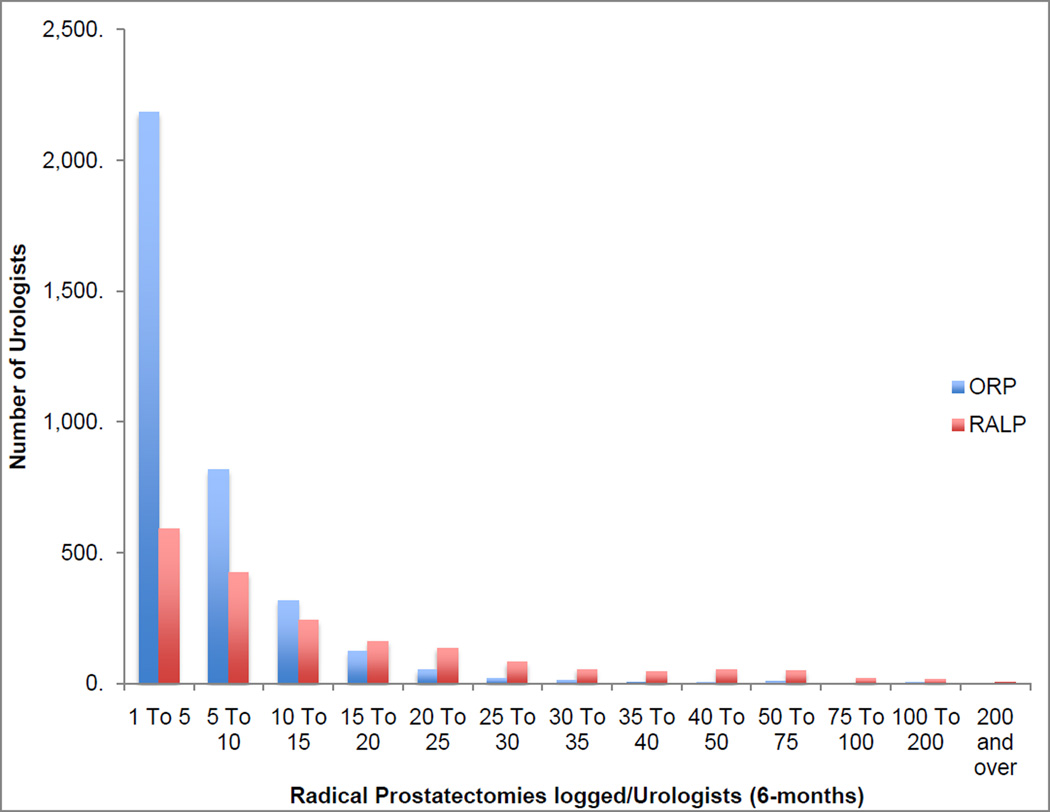
Figure 2.
individual Robotic Surgical Volume (minimum number logged=1, maximum logged 658)
Figure 4.
Change in percentage of urologists who performed exclusively laparoscopic radical prostatectomies.
Among surgeons performing ORP, the median number performed over the 6-month case log period was three RPs (IQR 2-7) while the median number of RALPs performed for robotic surgeons was eight (IQR 3-19) (p < 0.001). 39% of surgeons logging ORP performed two or fewer RP over six months while 19% of surgeons who performed RALP performed 2 or less RP (p < 0.001). The highest volume robotic surgeons (top 10% surgical volume) performed 41% of all RALP; the highest-volume robotic surgeon recorded 658 prostatectomies over 6-months.
We compared individual certification groups, acting as a surrogate for surgeon age, to determine if there is a difference in the performance of RALP vs. ORP in 2013. We found that urologists completing logs for their first recertification (~ after 10 years of practice) performed a significantly higher proportion of RP robotically (90.7%) compared to both initial certification and second recertification (81.7, 81.6% respectively, P < 0.001).
Oncologists represented 4.1% of all surgeons performing prostatectomies and accounted for 15.1% of all RP logged (p < 0.001). Among all other self-appointed urologic sub-specialty groups, general urologists performed the highest number of RP and account for 57.8% of all RPs performed. When comparing general urologists to surgical subspecialists performing the highest number of prostatectomies (oncology, endourology), there was no difference in the percentage of prostatectomies that were performed robotically (60.2% general urologists; 59.6 oncologists, 60.2% endourologists). When performed open, there was no influence of surgeon specialty on the performance of lymph node dissection (PLND) as general urologists performed PLND at a similar frequency to both oncologists and endourologists (table 1). When performed robotically, however, oncologists and endourologists were twice as likely to perform a PLND compared to general urologists (OR 2.46, p < 0.001).
Table 1.
Comparison of radical prostatectomies performed to surgical specialty
| Surgery Performed |
all urologists (n) |
General | Oncologists | endourologists | p-value |
|---|---|---|---|---|---|
| RP performed | 46707 | 31661 | 6965 | 2937 | |
| Open no PLND | 24% (4530) | 24.5% (3079) | 24.2% (678) | 24.6% (133) | 0.67 |
| Open + PLND | 76% (14440) | 75.5% (9498) | 75.8% (2134) | 75.3 (407) | |
| RALP no PLND | 58.5% (16204) | 73.8% (14068) | 53.3% (2211) | 53.8% (1266) | 0.01 |
| RALP + PLND | 41.5% (11533) | 26.2% (5016) | 46.7% (1942) | 47.1% (1131) |
Discussion
The diffusion of robotic-assisted prostatectomy is well described in the literature yet the impact on the surgical practice patterns of urologists in the United States is still not well understood. Work by Chang et al has described the adoption of RALP as corresponding to the ‘law of diffiusion of innovation’ with growth corresponding to three phases: “innovator phase’, early adopter phase’, and ‘early majority phase’.[8] Our data closely mirrors these results and we found that the shift to robotic technology to be well disseminated, with robotic prostatectomies representing 85% of all prostatectomies in 2013.
In our study we found a consistent, continuing trend toward the adoption of robotic prostatectomy as seen by Lowrance et al.[9] We found that radical prostatectomies are performed by a majority of urologists in the US; however, when exploring individual surgeon volume we found that, in reality, RP is performed at a high volume in only a subset of urologic surgeons. More than half of urologists who logged an open radical prostatectomy performed 3 or less in a 6-month period and among robotic surgeons the median number of prostatectomies logged in 6-months was eight procedures. Furthermore, we found that surgeons who are specialists in oncology tended to be higher-volume surgeons and account for a larger proportion of RP. Our findings are consistent with those of Denberg et al who completed a nationwide survey of 1170 urologist and found that the 37% of urologists complete less than 10 RP a year, with only 9.3% completing greater than 30/year.
The influence of surgeon volume on patient outcomes is a hotly debated topic in surgery today, with studies showing that surgeons who perform a low-volume of specialized procedures per year have increased mortality, post-operative infections, and revision rates.[10, 11] High volume surgeons have been shown to have superior patient outcomes across many surgical specialties, with improved outcomes following total hip replacements, cystectomy, and prostatectomy [12–14]
Interestingly, surgeons logging 2 or fewer prostatectomies per year performed 27% of all RP in our study. These findings suggest that although many patients may be either self-referred or physician-referred to those who specialize in prostatectomies, many cases continue to be performed by very low volume surgeons. There was no relationship between rural vs urban practice location and tendency-toward low volume surgeons. Recently, the urologic literature has seen an emerging emphasis on the role of high-volume referral centers and the increasing prevalence of centers of excellence (COE).[15, 16] For example, in the United Kingdom, the National Health services recently initiated a quality assurance programme a whole-scale reconfiguration of cancer services including referral of prostatectomy candidates to large-volume centers, with significant improvements in both potency and continence.[17]
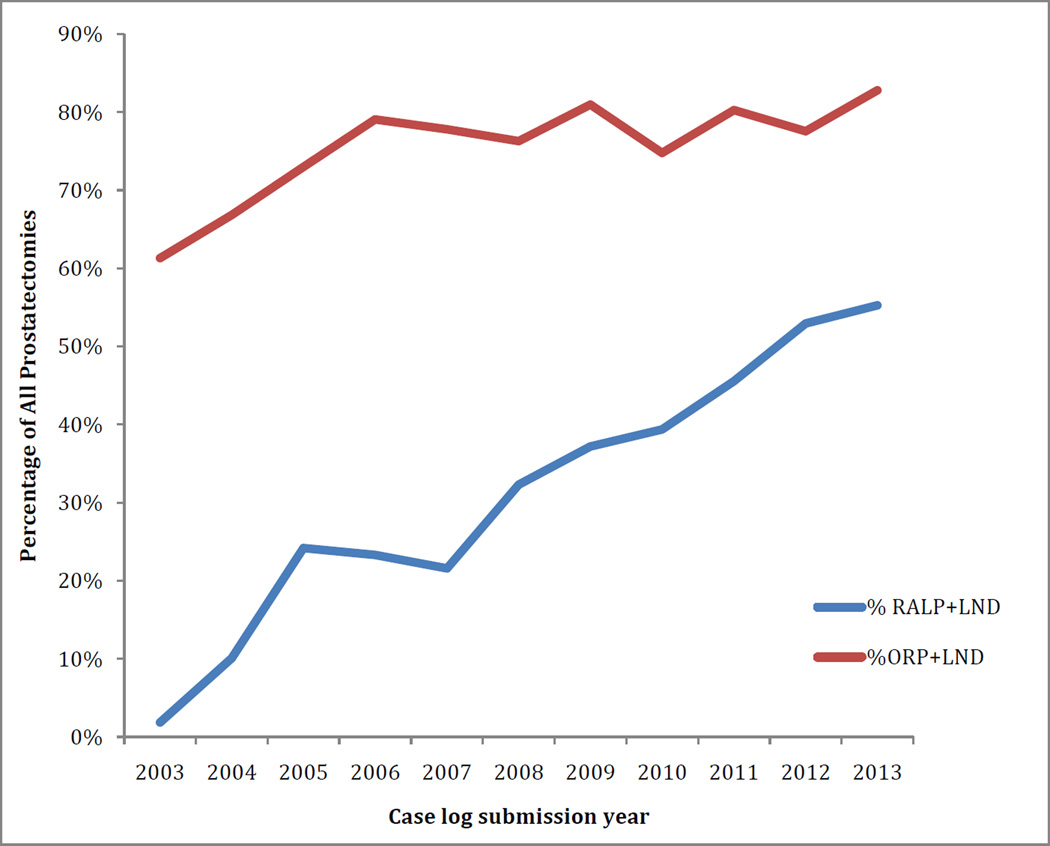
We investigated the performance of PLND at time of RP and found no difference among subspecialists when performed open; yet, when performed robotically, significantly fewer general urologists were found to perform a PLND than both oncologists and endourologists. In addition, we compared the performance of PLND in ORP vs. RALP and found that significantly more patients undergoing ORP undergo a concurrent PLND.
Our study raises concern about the quality of care provided in the treatment of men with prostate cancer and calls into question why surgical approach could potentially influence whether a patient received a PLND, especially in an era when robotic surgery in in the post-dissemination phase. In addition, it is a striking finding that node dissection rates are similar among subspecialties when performed open, but not when performed robotically. Unfortunately, without additional clinical information, we can only postulate why these patterns are seen. In particular, we are cautious to conclude that because general urologist, on average, perform a smaller percentage of lymph node dissection than specialists, that the clinical decision-making is not indicated. Potential reasons to suggest the decreased performance of PLND observed during RALP include patients with higher clinical stage or grade being managed by open prostatectomy, a more technically challenging procedure when performed robotically, and a lower Gleason score among patient in the robotic than open population.
These conclusions, however, must be considered with caveats. First, minimal surgical volume for proficiency has yet to be established and it is unclear if a total experience or yearly volume thresholds influence RP outcomes in the modern era. Recently, three prominent medical institutions-- Dartmouth–Hitchcock Medical Center, the Johns Hopkins Hospital and Health System, and the University of Michigan Health System announced the “Take the Volume pledge” campaign, an effort to prevent specific surgical operations from being performed by relatively low volume surgeons or hospitals. The idea that volume matters is simple and intuitive: with better practice and experience, we create better surgeons, and the literature has clearly supported the notion that surgical mortality is improved at high-volume hospitals. [10] In addition to the ten surgeries described, several complex urologic surgeries such as retroperitoneal lymph node dissection (RPLND), radical cystectomy (RC), and inguinal lymph node dissection for penile cancer carry a potential for significant morbidity and mortality.[13] Our research utilizing surgical case logs from the American Board of Urology shows that among these technically advanced, potentially morbid surgeries, the average number of procedures performed is often less than what one might predict.
Our study is not without limitations or bias. First, given that case logs are from a self-defined six-month period, they may not represent the most accurate surgical volume of each urologist. In addition, urologist certified by the ABU prior to 1985 are exempt from submitting logs, and therefore the data derived will be bias towards a younger cohort of urologists and will not include more senior urologists in the US. In addition, although there is an overall increase in the total number of prostatectomies performed, this is attributed to an increased number of urologists captured in the logs over time and we did not find a significant increase in surgical volume per surgeon over time.
Over a 10-year period, 46,707 prostatectomies were recorded from 6-month logs, or when annualized, 93,414 over 10 calendar years. If we assume these logs represent two-thirds of all urologists in the US and 10% of all urologists are certified or recertified each year, we can extrapolate that ~140,000 prostatectomies are performed each year based on ABU data. This estimation of prostatectomy volume is substantiated by data from the hospital discharge surveys published by the Center for Disease Control, estimating that 138,000 radical prostatectomies are performed each year in the US.[18] Ultimately, ABU case logs are one of the most accurate sources of the actual practice patterns of urologists in the United States; indeed, the case logs described covered a period of 10 years and include the complete practice patterns of 6,563 urologists or two-thirds of all urologist in the US based on work force estimations by Pruthi et al and recently corroborated by the AUA census of 2015.[19] Our data, therefore, is one of the largest databases of radical prostatectomies to date and is a representation of the actual practice patterns of urologists in the US.
Conclusion
Among board-certified urologists in the United States, there was a substantial increase in the performance of RALP from 2003 to 2013, with 85% of radical prostatectomies being performed robotically by 2013. We found that nearly a quarter of surgeons performed 2 or less RALP over 6-months and surgical subspecialists were twice as likely to perform a robotic PLND compared to general urologists. Redirecting patients requiring complex surgical procedures such as radical prostatectomies to high-volume hospitals may improve patient outcomes but ultimately will require more widespread adoption of minimum volume initiatives to succeed. These data provide estimates of current RP practice patterns and enhance our understanding of the surgical treatment of PC in the US today.
Figure 3.
Change in percentage of open and laparoscopic radical prostatectomies performed with concurrent pelvic lymph node dissection over time.
Highlights.
Robotic prostatectomies are performed five-times more commonly than open prostatectomy in the United States
RALP represent 85% of all RP performed by board-certified urologists in 2013
Compared to RALP, ORP are significantly more likely to be performed by lower volume surgeons.
Oncologists perform a higher relative percentage of RPs and are significantly more likely to perform LND if performed robotically when compared to general urologists
Abbreviations
- RALP
Robotic-Assisted laparoscopic Prostatectomy
- ORP
Open Radical Prostatectomy
- ABU
American Board of Urology
- US
United States
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014. CA: A Cancer Journal for Clinicians. 2014;64:9–29. doi: 10.3322/caac.21208. [DOI] [PubMed] [Google Scholar]
- 2.Underwood W, Jackson J, Wei JT, Dunn R, Baker E, DeMonner S, et al. Racial treatment trends in localized/regional prostate carcinoma, 1992–1999. Cancer. 2005;103:538–545. doi: 10.1002/cncr.20796. [DOI] [PubMed] [Google Scholar]
- 3.Makarov DV, Yu JB, Desai RA, Penson DF, Gross CP. The Association Between Diffusion of the Surgical Robot and Radical Prostatectomy Rates. Medical Care. 2011:1. doi: 10.1097/MLR.0b013e318202adb9. [DOI] [PubMed] [Google Scholar]
- 4.Liu JS, Hofer MD, Oberlin DT, Milose J, Flury SC, Morey AF, et al. Practice Patterns in the Treatment of Urethral Stricture Among American Urologists: A Paradigm Change? Urology. 2015 doi: 10.1016/j.urology.2015.07.020. [DOI] [PubMed] [Google Scholar]
- 5.Oberlin DT, Flum AS, Bachrach L, Matulewicz RS, Flury SC. Contemporary surgical trends in the management of upper tract calculi. The Journal of urology. 2015;193:880–884. doi: 10.1016/j.juro.2014.09.006. [DOI] [PubMed] [Google Scholar]
- 6.Oberlin DT, Matulewicz RS, Bachrach L, Hofer MD, Brannigan RE, Flury SC. National Practice Patterns for Treatment of Erectile Dysfunction with Penile Prosthesis Implantation. The Journal of urology. 2014 doi: 10.1016/j.juro.2014.11.095. [DOI] [PubMed] [Google Scholar]
- 7.Hofer MD, Meeks JJ, Cashy J, Kundu S, Zhao LC. Impact of increasing prevalence of minimally invasive prostatectomy on open prostatectomy observed in the national inpatient sample and national surgical quality improvement program. Journal of endourology / Endourological Society. 2013;27:102–107. doi: 10.1089/end.2012.0315. [DOI] [PubMed] [Google Scholar]
- 8.Chang SL, Kibel AS, Brooks JD, Chung BI. The impact of robotic surgery on the surgical management of prostate cancer in the USA. BJU international. 2015;115:929–936. doi: 10.1111/bju.12850. [DOI] [PubMed] [Google Scholar]
- 9.Lowrance WT, Eastham JA, Savage C, Maschino AC, Laudone VP, Dechet CB, et al. Contemporary open and robotic radical prostatectomy practice patterns among urologists in the United States. The Journal of urology. 2012;187:2087–2092. doi: 10.1016/j.juro.2012.01.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Halm EA, Lee C, Chassin MR. Is volume related to outcome in health care? A systematic review and methodologic critique of the literature. Annals of internal medicine. 2002;137:511–520. doi: 10.7326/0003-4819-137-6-200209170-00012. [DOI] [PubMed] [Google Scholar]
- 11.Kreder HJ, Deyo RA, Koepsell T, Swiontkowski MF, Kreuter W. Relationship between the volume of total hip replacements performed by providers and the rates of postoperative complications in the state of Washington. The Journal of bone and joint surgery American volume. 1997;79:485–494. doi: 10.2106/00004623-199704000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Bianco FJ, Jr, Riedel ER, Begg CB, Kattan MW, Scardino PT. Variations among high volume surgeons in the rate of complications after radical prostatectomy: further evidence that technique matters. The Journal of urology. 2005;173:2099–2103. doi: 10.1097/01.ju.0000158163.21079.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barbieri CE, Lee B, Cookson MS, Bingham J, Clark PE, Smith JA, Jr, et al. Association of procedure volume with radical cystectomy outcomes in a nationwide database. The Journal of urology. 2007;178:1418–1421. doi: 10.1016/j.juro.2007.05.156. discussion 21-2. [DOI] [PubMed] [Google Scholar]
- 14.Birkmeyer JD, Stukel TA, Siewers AE, Goodney PP, Wennberg DE, Lucas FL. Surgeon volume and operative mortality in the United States. New England Journal of Medicine. 2003;349:2117–2127. doi: 10.1056/NEJMsa035205. [DOI] [PubMed] [Google Scholar]
- 15.Henry GD, Kansal NS, Callaway M, Grigsby T, Henderson J, Noble J, et al. Centers of excellence concept and penile prostheses: an outcome analysis. The Journal of urology. 2009;181:1264–1268. doi: 10.1016/j.juro.2008.10.157. [DOI] [PubMed] [Google Scholar]
- 16.Al-Shaiji TF, Brock GB. Surgery: centers of excellence for penile prosthesis: yes or no? Nature reviews Urology. 2009;6:352–354. doi: 10.1038/nrurol.2009.109. [DOI] [PubMed] [Google Scholar]
- 17.Cathcart P, Sridhara A, Ramachandran N, Briggs T, Nathan S, Kelly J. Achieving Quality Assurance of Prostate Cancer Surgery During Reorganisation of Cancer Services. European urology. 2015 doi: 10.1016/j.eururo.2015.02.028. [DOI] [PubMed] [Google Scholar]
- 18.Statistics NCFH. Annual National Hospital Discharge Survey Data Files. 2010. [Google Scholar]
- 19.Pruthi RS, Neuwahl S, Nielsen ME, Fraher E. Recent trends in the urology workforce in the United States. Urology. 2013;82:987–994. doi: 10.1016/j.urology.2013.04.080. [DOI] [PubMed] [Google Scholar]