Summary
Deep burns lead to scarring and contractures for which there is little or no published data on treatment costs. The purpose of this study was to fill this gap by analysing treatment costs for burn sequelae. To do this, German-DRG for in-patient treatment was collected from the Burn Centre Lower Saxony. DRG-related T95.-coding served as a tool for burn-associated sequelae. Data on scar occurrence, plastic-reconstructive surgery and sick leave were collected by a questionnaire. The findings showed that 44.6% patients reported post-burn scarring and 31% needed surgical intervention. The expected risk for readmission was significantly higher (p=0.0002) with scars compared to without. Significantly higher costs for pressure garments were noted for scarred patients (p=0.04). No differences were found for ointments, silicone dressings or pain medication. Treatment costs for patients with scars were 5.6 times higher compared with no scar assessed by G-DRG. No differences were stated subsuming multiple readmissions for post-burn treatment per individual. Significantly higher costs (p=0.03) were noted for patients with burn sequelae other than scars with regard to individual readmissions. It has been revealed that treatment of scars causes higher costs than for other burn sequelae because of multiple surgical interventions. To reduce post-burn scarring and costs, specialized burn centres provide optimal and state-of-the-art treatment. As well as this, more emphasis should be laid on promoting research for the development of novel anti-scarring therapies.
Keywords: health care costs, burn injury, post-burn sequelae, scar treatment, G-DRG
Abstract
Les brûlures profondes entraînent des cicatrices et des contractures pour lesquels il n’existe pas de données publiées dés coûts de traitement. Le but de cette étude était de combler cette lacune en analysant les coûts de traitement des séquelles de brûlures. Nous avons recueillies les données sur les séquelles de brûlure du Centre de Brûlés de Basse-Saxe en utilisant un questionnaire. Toutes les informations sur les cicatrices, la chirurgie plastique reconstructive et les congés de maladie ont été recueillies. Les résultats ont montré que 44.6% des patients avaient des cicatrices et 31% ont eu besoin d’une intervention chirurgicale. Le risque de réadmission était significativement plus élevé (p = 0,0002) parmi les patients avec des cicatrices. Pour ces patients les coûts étaient considérablement plus élevés pour les vêtements de compression (p = 0,04) mais, en ce qui concerne les pommades, les pansements siliconés ou les médicaments contre la douleur aucune différence n’a été trouvée. Les coûts de traitement pour les patients porteurs de cicatrices étaient 5,6 fois plus élevés par rapport aux patients sans aucune cicatrice. Les coûts plus élevés (p = 0,03) ont été observés chez les patients avec des séquelles de brûlures autre que cicatrices dues aux réadmissions individuelles. Nous avons noté aussi que le traitement des cicatrices entraîne des coûts plus élevés par rapport aux autres séquelles à cause des interventions chirurgicales multiples. Pour réduire les cicatrices post-brûlures, et donc les coûts, les centres spécialisés fournissent un meilleur traitement. De plus, l’accent devrait être mis sur la recherche pour le développement de nouvelles thérapeutiques anti-cicatrices.
Introduction
In 2012, almost 2,000 burn victims were admitted to German burn ICU centres for acute medical care (http://www.verbrennungsmedizin.de/pdf/Verbrennungsstatistik-2012.pdf, accessed Dec. 1st 2013). In deep and full thickness burns necrotic tissue is surgically removed and commonly replaced with split-thickness skin grafts. Once wound healing has completed, continuous aftercare is required with ointments, physiotherapy, and silicone sheeting to prevent hypertrophic scar formation. In addition, individually tailored pressure garments are prescribed, although there is little evidence to support their beneficial effects.1-3 In a previous study, we showed that post-burn treatment of burn sequelae was significantly more expensive than that of acute burn patients without the need of intensive care.4 The incidence of pathologic scarring after burn injury varies between 30% and 91%2,5 with wound depth and total body surface area burned (TBSA) being predictors for severe scarring. 6 In cases of mutilating scarring, secondary surgical interventions are needed with scar release and plastic-surgical reconstruction.
The aim of this study was to evaluate treatment costs of patients with burn sequelae at the Burn Centre Lower Saxony using data from G-DRG-reimbursement of in-patients gathered from a patients’ questionnaire. G-DRG data were used to compare treatment costs for patients with and without scarring after burn injury. The patients’ questionnaire yielded information on incidence of scarring in our cohort, need for readmissions and surgery, an estimate on costs for adjuvant treatment, e.g. compression garments, creams, silicone sheeting and pain medication, and time of absence from work and for rehabilitation measures.
Materials and methods
Two different data sources were used to assess treatment costs for patients from the Burn Centre Lower Saxony: German Diagnose Related Groups (G-DRG, Annex I) accounting for in-patient treatment for burn sequelae at the Department of Plastic, Reconstructive and Hand Surgery, Hannover Medical School, from 2006 to 2009; and a questionnaire that was sent to discharged patients from the same time period (Annex II). G-DRG collected data were published – in part – previously.4
Annex I. DRG and ICD-10 codes relevant for burn sequelae treatment.
Annex II. Questionnaire to burn patients treated at Hannover Medical School.
The Ethical Committee of Hannover Medical School had approved the study prior to its start (No. 578/2009). All data from each source were acquired anonymously without the possibility to track or identify any patient.
German-DRG of burn patients from Hannover Medical School
The Burn Centre Lower Saxony is part of the Department of Plastic, Hand and Reconstructive Surgery, Hannover Medical School. The Burn Centre hosts a highly specialized intensive care unit for patients with thermal injuries and provides highly specialized burn care for the public within an area with an average radius of 150 km and about 10 million inhabitants. The patient database of the Department of Plastic, Hand and Reconstructive Surgery was screened in order to analyse treatment costs for in-patients with burn sequelae. DRG is an economic- medical classification system grouping main and side diagnoses and different treatments per case for reimbursement by insurance companies. G-DRG of the Major Diagnostic Category (MDC) 09, i.e. skin diseases, and MDC 22, i.e. burns, were used. Patients were selected according to their diagnoses, coded by the International Statistical Classification of Diseases and Related Health Problems (ICD-10, version 2006; Annex I). Main selection criterion for followup treatment was T95.- coding for “sequelae after burn, chemical burn or frostbite” according to chapter XIX, ICD-10. Data on the DRG reimbursement were provided for follow- up treatment by the controlling department. Data were analysed within a time period of 36 months (2006 – 2009). Some patients were readmitted and treated several times. To address multiple hospital stays, these patients were analysed in two ways. Total costs for post-burn treatment were assessed “per case” or episode, e.g. several readmissions for one single patient counted separately. To account for individual costs “per patient”, treatment costs for multiple readmissions and interventions at different time periods were added and stated as cost per individual patient. Patients’ files were screened for scarring and other post-burn sequelae.
Burn patient questionnaire
Treatment costs for aftercare and occurrence of burn scars were assessed by an anonymous questionnaire (Annex II) that was sent to patients with previous treatment in the Burn Centre between 2006 and 2009. Among other information, data on total burned body surface area, burned body parts, aftercare, scar formation with or without need for readmission and surgery were retrieved. Statement of scar formation was provided by patients without further physical examination. Therefore, no detailed data on type of scarring, e.g. hypertrophic scarring, could be gained from this data source. Post-burn scarring leading to surgical procedures was interpreted as pathological, e.g. excessive scarring.
In Germany, costs for medical care are covered by public health care providers (90%), private insurances (ca 9%) and workmen compensation funds, without the need for patients to directly pay for prescriptions or hospital stays. Therefore, exact prices for pressure garments, creams or pain killers could not be stated by patients but rather amounts of items or substances used during the treatment period. In order to estimate total costs, the lowest price for each particular item was used for cost calculation, e.g. 400 EUR per pressure garment, 10 EUR per 50g tube of cream, 25 EUR per silicone sheet, and 15 EUR per package of analgetic medication (30 pills). Costs were adjusted if specific prices or brands were stated in the questionnaire.
Although G-DRG assessment and patient survey were conducted during the same time period, data could not be linked or compared due to anonymous data sampling.
Statistics
Two-tailed Student’s t-test for paired observations was applied when normal distribution was assumed. The Wilcoxon Signed Rank test was used for paired observations when normal distribution did not apply, using the software MATLAB® (version 7.12.0.635 (R2011a); The MathWorks Inc, Natick, MA, USA). P < 0.05 was considered statistically significant. The Chi Square Test was used to assess the expected risk for scar patients to undergo several operations. Numerical data are presented as mean ± SEM (standard error of mean) or median ± SEM.
Results
Patient questionnaire
The survey addressed 276 surviving burn patients treated at the Burn Centre Lower Saxony for burn sequelae between 2006 and 2009. Seventy-five questionnaires out of 276 could not be delivered; 59 patients out of the remaining 201 (29.4%) participated in the survey. The questionnaire responses revealed that 68.5% of the cohort were men; the average age was 42.5 years; and the average TBSA of the initial burn injury was 27.9% with 2nd and 3rd degree burns. Ninety per cent of the patients were initially admitted to the burn intensive care unit for 7 ± 2.9 days (n=51; median ± SEM, max=98 and min=0.5 days). The majority of burn injuries were due to leisure or domestic accidents (54.2%), followed by work-related accidents (35.6%) and others (10.2%). Burned body sites were in 69% upper limb (n=41), in 54% head/neck (n=32), in 51% trunk (n=30) and in 42% lower limb (n=25). After initial treatment for acute burn, a secondary readmission was necessary in 23.7% of all patients with surgical intervention (n=14; noscar= 1, scar=12, n.s.=1; Table I).
Table I. Summary patient survey: Readmissions, reoperations, professional consequences.
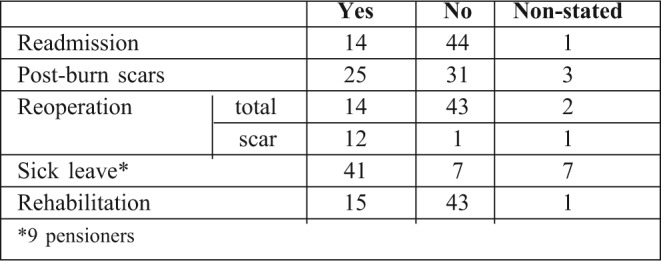
Scar formation after burn injury
Scar formation was noted by 42.4% of patients (n=25) whereas 52.5% (n=31) did not state scars and 5.1% (n=3) did not answer this question (Table I). Scar patients had previously burned their hands and arms in 72% (n=18), in 56% the trunk (n=14), head and neck in 52% (n=13), and in 40% feet and legs (n=10). No detailed clinical data is given on the nature of scarring because a postal questionnaire was used without re-examination of each patient. “Excessive scarring” could be stated by patients on the survey form (Annex II). The necessity for in-hospital treatment and surgical interventions implies the pathological nature of patients’ stated scarring. Accordingly, in the following, the term “scar” is used equivalently for pathological scarring. Reoperations were necessary in 3.2% of no-scar (n=1/31) and in 48% (n=12/25) of scar patients. To assess the expected risk for surgical intervention, the Chi Square test was used. Scar patients were at significantly higher risk (p=0.0001) to endure more than one hospital stay for surgical procedures compared to patients without scars.
Sick leave and rehabilitation
Burn sequelae led to sick leave for 41 patients, e.g. 14 scar and 23 no-scar patients. Nine patients were pensioners and not included, 2 patients did not answer the question. When asked about the time period out of work, 36 patients (n.s.=7) answered the questionnaire and stated 8 ± 4.5 weeks (median ± SEM, max=130, min=2). Significant differences (p=0.0017) were found for scar patients (n=14) with a median of 16.8 ± 10.5 (max=130, min=4.5) weeks compared to no-scar patients (n=23) with 5 ± 0.9 weeks (max=20, min=2; Fig. 1).
Fig. 1. Time out of work was stated by 36 patients.
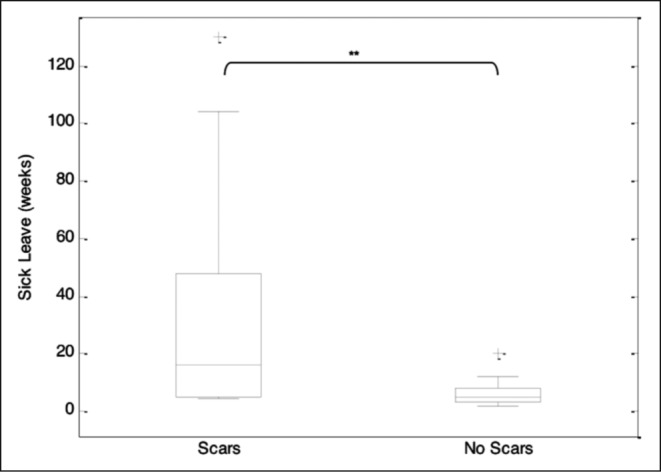
Time out of work was stated by 36 patients with significantly longer absent periods for scar patients (16±10.5 weeks; max=130, min=4.5; n=14) compared to no-scar patients (5±0.9 weeks max=20, min=2; n=23). Both cohorts were compared using the Wilcoxon Signed Rank test. Boxes represent 25th to 75th percentile range (interquartile range), whiskers 5th to 95th percentile range and horizontal lines within the boxes indicate the median values. p-values are given for statistical significant outcomes. median+SEM **p=0.0017.
Calculation of the loss of productivity was performed according to the Theory of Human Capital and the previously published equation of the Hanover Consensus group.7 For calculation, the mean income between 2006 and 2009 was taken and converted into income per day, e.g. 92 EUR per worker and day.7,8 With 117.5 ± 67.6 (mean ± SEM) days of absence per patient, the total loss of productivity was 10,819 EUR per day (n=37) for our patient cohort.9 With regard to patients stating scarring (235.5 ± 73.5 days of sick leave), the loss of productivity was 21,664 EUR compared to 4,213 EUR for patients without reported scars (45.6 ± 6.1 days of sick leave).
Rehabilitation measures were stated by 15 patients, e.g. 10 scar and 5 no-scar patients (Table I) whereas 43 patients had no rehabilitation and one did not answer the question.
Adjuvant treatment
Adjuvant treatment such as physiotherapy, manual therapy and massages was prescribed for 12.9% patients without and for 40% with scars (Table II). Auxiliary material costs were assessed for the patient cohort subsuming expenses for pain medication, ointments, silicone sheets and compression garments. Of note, costs for patients with scars more than doubled compared to expenses for burn patients without scars (Table III). Significantly higher costs were noted for pressure garments for scar patients compared to no-scar patients (p=0.04, Table II, Fig. 2).
Table II. Summary patient survey: Costs for adjuvant therapy and auxiliary material.
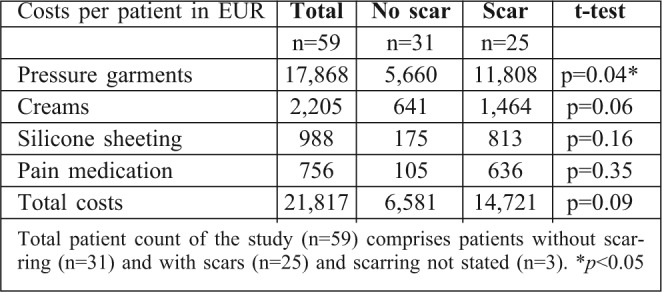
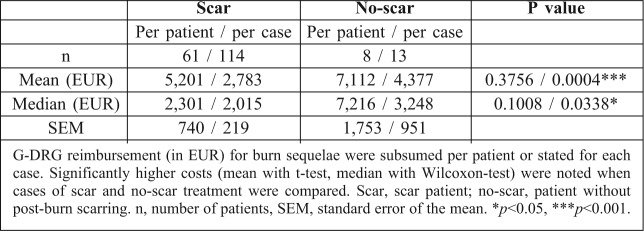
Table III. Number of reoperations and G-DRG costs for burn sequelae.
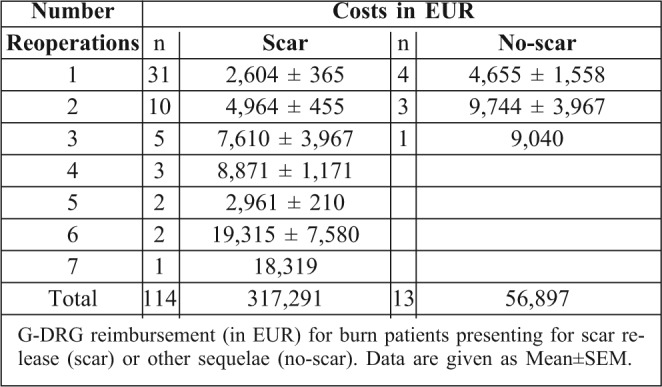
Fig. 2. Questionnaire data on auxiliary treatment.
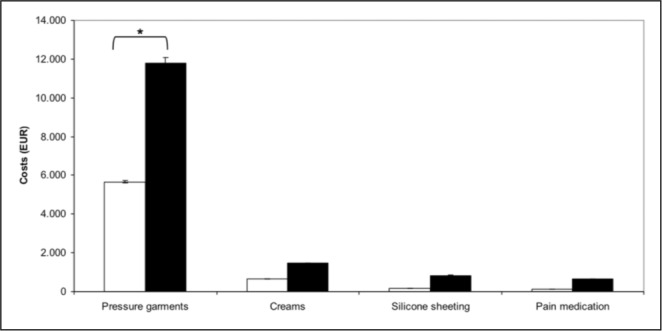
e.g. costs for pressure garments, silicone sheeting, creams or pain medication are given. Significant differences were solely found with regard to pressure garment prescriptions between scar and no-scar patients. White bars, no-scar patients; black bars, scar patients. Costs in EUR; *p=0.04.
DRG reimbursement for treatment of burn sequelae
Within the observation period of 36 months, 127 patients were admitted to the department for treatment of burn sequelae. This cohort comprised 114 cases (or 61 patients) with scars needing release or plastic-reconstructive surgery, and 13 cases (or 8 patients) for treatment of other burn sequelae, e.g. skin defects needing coverage (n=5), chronic wounds with infection (n=2) or cancer (n=1). To facilitate the description of both patient cohorts, patients presenting for scar release will be named further on as “scar patients” and those needing reconstructive surgery for other burn sequelae as “no-scar patients”.
Frequency of readmissions for patients needing surgical treatment after burn injury differed between both groups. Patients presenting with scars were treated up to seven times (Table III) whereas no-scar patients needed reoperation for a maximum of 3 times. When all G-DRG costs were added up per each individual patient, no significant differences were found between patients without or with scars (p=0.1008; Wilcoxon Sign Test; Table IV, Fig. 3). With regard to costs per case, e.g. each readmission was counted separately regardless of patient’s identity, significantly higher costs (p=0.0338) were stated for no-scar patients (Table IV, Fig. 4).
Table IV. Total G-DRG costs in EUR for burn sequelae.
Fig. 3. G-DRG reimbursement for treatment of burn sequelae.
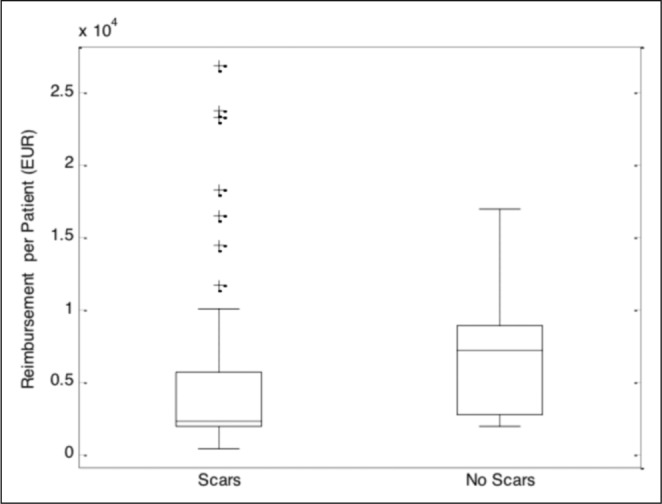
G-DRG reimbursement for treatment of burn sequelae (ICD- 10, T95. – coding) for patients without scars (n=8) or with scars (n=61). In case of multiple readmissions and treatments, all costs were subsumed per each individual patient. Boxes represent 25th to 75th percentile range (interquartile range), whiskers 5th to 95th percentile range and horizontal lines within the boxes indicate the median values. No significant differences were found between groups (p=0.375). Data are given as median ± standard error of the mean (SEM).
Fig. 4. G-DRG reimbursement for treatment of all cases.
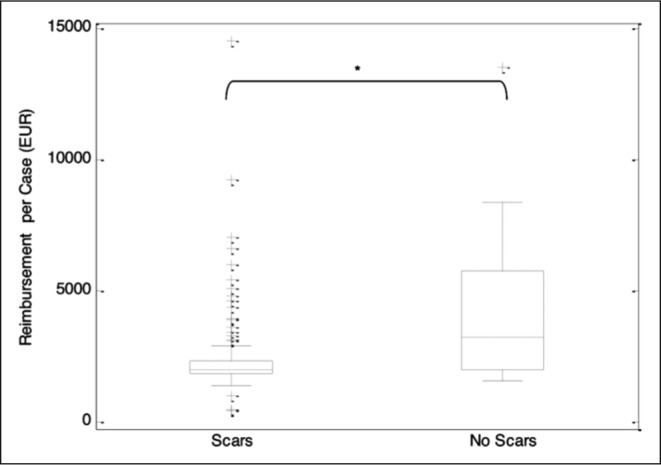
G-DRG reimbursement for treatment of all cases (each single admission counted) with burn sequelae (ICD-10, T95.—coding) for patients without scars (n=13) or with scars (n=114). Significantly higher costs were generated by patients treated for other burn sequelae than scarring (p=0.0338). Boxes represent 25th to 75th percentile range (interquartile range), whiskers 5th to 95th percentile range and horizontal lines within the boxes indicate median values. Data are given as median ± SEM; *p<0.05.
Discussion
In this retrospective study, treatment costs for postburn sequelae were analysed. Data from a burn patient survey on follow-up treatment and occurrence of scarring and G-DRG from the Burn Centre Lower Saxony, Hannover Medical School were collected and analysed for treatment costs.
Full-thickness burn injury requires radical debridement and defect coverage by plastic-reconstructive surgery, e.g. skin grafting or flap surgery. Skin grafting is followed by a variable extent of scarring.2,10-13 In our patient cohort, 42% of the questioned patients reported excessive scarring albeit detailed data on the nature of scarring or grafting was not available. The percentage of scar formation in the present study compares well to data of Caucasian patients’ prevalence of hypertrophic scarring after burns from different studies varying between 7%,13 15%,12 63%,14 67%10 and 77%.11 Due to the wide-spread admission area of the Burn Centre, it was impossible to recruit patients for scar assessment. A clinical examination of scarring and more details concerning initial treatment, e.g. skin grafting, would have certainly yielded valuable data consolidating our findings.
Pathological scarring can lead to mutilating contractures with immobilization of joints and reduced limb motility. 11,15 Because of the latter, surgical interventions become necessary to release joints, improve function and restore professional and social reintegration. Forty-two percent of all questioned patients reported excessive scarring which corresponds to the prevalence of hypertrophic scarring in 15-91% after burns published by various authors.2,10-12,16 With regard to scar contractures, considerably lower incidences were stated by Gangemi et al11 with 5% or by Kraemer et al with 2% in adults and 7.8% in children.15 Admittedly, no detailed data is available in the present study concerning the type and severity of scarring that patients stated in the questionnaire.
As stated previously,2,11,17 scar recurrence rates are high especially with regard to burned sites on hands and head/neck and upper trunk. Thus, patients are prone to undergo multiple operations for scar release. In our patient survey, 48% (n=12) of all scar patients (n=25) stated a surgical intervention with 40% (n=10) due to excessive scarring. The expected risk for patients to endure more than one surgical intervention due to scarring was significantly higher (p=0.0002) compared to no-scar burn patients. G-DRG data from the Burn Centre Lower Saxony corroborates this finding with multiple reoperations for scar patients, e.g. with up to seven operations in one case. Sixty- one scar patients underwent a total of 114 surgical interventions in comparison with 8 no-scar patients and 13 operations, e.g. 1.9 or 1.6 procedures per patient, respectively. Gangemi et al. stated 1.7 reoperations per patient with hypertrophic scarring or 2.5 for contracture release11 which corresponds well to our data.
Expenses for scar release equalled costs for patientsExpenses for scar release equalled costs for patients with sequelae other than scars when costs for multiple readmissions and procedures were added up per patient (p=0.1). Unexpectedly, when costs were analysed for each admission and treatment, e.g. per case, significantly higher costs arose for no-scar patients (p=0.03). One important fact might explain this intriguing finding. Post-burn patients with sequelae other than scars presented with chronic wounds, soft tissue defects or post-burn cancer that were treated by surgical excision and subsequent plastic-reconstructive defect coverage including microvascular flap surgery. Reimbursement for distant or free-flap surgery is higher (ca. 8.400-13.000 EUR) compared to scar corrections (ca. 2.200 EUR) depending on the patient’s co-morbidities. This finding is of central importance because the incidence of post-burn scarring, scar re-occurrence after release and the need for repeated hospital stays and surgical interventions are the major reasons for higher scar treatment costs compared to other post-burn sequelae.
Needless to say, the expenses for scarring after burn injury (317,291 EUR) and the high patient number requiring scar release (n=114) were 5.6 times higher compared to the costs for patients treated for other postburn sequelae (56,897 EUR, n=13). As a consequence, expensive novel treatment concepts, e.g. with dermal matrix substitutes, might prove cost-effective in the long run, reducing post-burn scarring and costs for reconstructive surgery.
Beyond surgical interventions and inhospital stays, costs for scar treatment arise for local therapy with pressure garments and silicone sheeting, for pain medication and manual therapy.18 Despite the fact that there is no hard evidence for clinical effectiveness of pressure garments,13,19 compression therapy is currently the golden standard for scar prevention.20 In our questionnaire, significantly more scar patients received pressure garment therapy compared to no-scar patients. One can only speculate if this treatment efficiently prevented the occurrence of contractures and the need for readmission and surgery in our scar patient cohort, as stated by others.20,21
Costs for burn patient treatment can be divided into direct costs that consider consumption of health system resources, e.g. in-hospital stay with interventions and outpatient treatment etc., and indirect costs, e.g. loss of productivity due to premature mortality or absence from work attributable to disease.9 Loss of productivity was higher with post-burn scarring because scar patients stated significantly longer out-of-work periods compared to patients without reported scars. Sanchez et al published data on sick leave and indirect costs for acute burn patients.22 Absence from work amounted to 158 ± 99 (mean ± SD; n=898) days with indirect costs for labour of 48,509 USD or 35,015 EUR (exchange rate 2006, 1:0.722)22 in comparison with our patient cohort with 117.5 ± 67.6 days (mean ± SEM) with a loss of productivity of 10,819 EUR. In contrast, patients with post-burn scarring stated 235.5 ± 73.5 days out of work with a productivity loss of 21,664 EUR, five times more than patients without reported scars and twice the amount of the total cohort. Data on salaries of Spanish employees were unfortunately not available for comparison of loss of productivity in both countries. Similar periods of absence from work for acute and postburn patients and the resulting socio-economic costs underpin the high relevance and economic impact of burn sequelae.
Conclusion
Costs for burn sequelae arise mainly for scar treatment, with five times higher costs compared to other burn sequelae. High incidence of scarring after burn injury with multiple reoperations are the main reasons for scar treatment expenses. For prevention of excessive scarring, acute burn care should be performed at specialized burn centres to minimize post-burn sequelae. The lack of effective scar prevention measures implies the demand for increased funding of anti-scarring research.
Acknowledgments
Conflict of interest. All authors declare no financial or personal relationships with other people or organisations that could inappropriately influence (bias) the present work.
References
- 1.Anzarut A, Olson J, Singh P, et al. The effectiveness of pressure garment therapy for the prevention of abnormal scarring after burn injury: a meta-analysis. J Plast Reconstr Aesthet Surg. 2009;62:77–84. doi: 10.1016/j.bjps.2007.10.052. [DOI] [PubMed] [Google Scholar]
- 2.Bloemen MC, van der Veer WM, Ulrich MM, et al. Prevention and curative management of hypertrophic scar formation. Burns. 2009;35:463–75. doi: 10.1016/j.burns.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 3.Engrav LH, Heimbach DM, Rivara FP, et al. 12 year withinwound study of the effectiveness of custom pressure garment therapy. Burns. 2010;36:975–83. doi: 10.1016/j.burns.2010.04.014. [DOI] [PubMed] [Google Scholar]
- 4.Mirastschijski U, Sander JT, Weyand B, et al. Rehabilitation of burn patients: an underestimated socio-economic burden. Burns. 2013;39:262–8. doi: 10.1016/j.burns.2012.06.009. [DOI] [PubMed] [Google Scholar]
- 5.Stella M, Castagnoli C, Gangemi EN. Postburn scars: An update. Int J Low Extrem Wounds. 2008;7:176–81. doi: 10.1177/1534734608323057. [DOI] [PubMed] [Google Scholar]
- 6.van der Wal MB, Vloemans JF, Tuinebreijer WE, et al. Outcome after burns: An observational study on burn scar maturation and predictors for severe scarring. Wound Repair Regen. 2012;20:676–87. doi: 10.1111/j.1524-475X.2012.00820.x. [DOI] [PubMed] [Google Scholar]
- 7.Graf von der Schulenburg JM, Greiner W, Jost F, et al. German recommendations on health economic evaluation: third and updated version of the Hanover Consensus. Value in health : the Journal of the International Society for Pharmacoeconomics and Outcomes Research. 2008;11:539–44. doi: 10.1111/j.1524-4733.2007.00301.x. [DOI] [PubMed] [Google Scholar]
- 8.Office FS, editor. Statistical Yearbook 2010 for the Federal Republic of Germany including international tables. Wiesbaden; 2010. Volkswirtschaftliche Gesamtrechnung; pp. 622–59. [Google Scholar]
- 9.GSfHEe V, editor. Gesundheitsökonomie & Qualitätsamanagment. Thieme; Stuttgart: 2007. Deutsche Empfehlungen zur gesundheitsökonomischen Evaluation - dritte aktualisierte Fassung des Hannoveraner Konsens; pp. 285–90. [Google Scholar]
- 10.Bombaro KM, Engrav LH, Carrougher GJ, et al. What is the prevalence of hypertrophic scarring following burns? Burns. 2003;29:299–302. doi: 10.1016/s0305-4179(03)00067-6. [DOI] [PubMed] [Google Scholar]
- 11.Gangemi EN, Gregori D, Berchialla P, et al. Epidemiology and risk factors for pathologic scarring after burn wounds. Arch Facial Plast Surg. 2008;10:93–102. doi: 10.1001/archfaci.10.2.93. [DOI] [PubMed] [Google Scholar]
- 12.Deitch EA, Wheelahan TM, Rose MP, et al. Hypertrophic burn scars: analysis of variables. J Trauma. 1983;23:895–8. [PubMed] [Google Scholar]
- 13.McDonald WS, Deitch EA. Hypertrophic skin grafts in burned patients: a prospective analysis of variables. J Trauma. 1987;27:147–50. doi: 10.1097/00005373-198702000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Elliot D, Cory-Pearce R, Rees GM. The behaviour of presternal scars in a fair-skinned population. Annals of the Royal College of Surgeons of England. 1985;67:238–40. [PMC free article] [PubMed] [Google Scholar]
- 15.Kraemer MD, Jones T, Deitch EA. Burn contractures: incidence, predisposing factors, and results of surgical therapy. J Burn Care Rehabil. 1988;9:261–5. [PubMed] [Google Scholar]
- 16.Bach AD, Kneser U, Beier JP, et al. Aesthetic correction of tuberous breast deformity: lessons learned with a single-stage procedure. Breast J. 2009;15:279–86. doi: 10.1111/j.1524-4741.2009.00717.x. [DOI] [PubMed] [Google Scholar]
- 17.Mustoe TA, Cooter RD, Gold MH, et al. International clinical recommendations on scar management. Plast Reconstr Surg. 2002;110:560–71. doi: 10.1097/00006534-200208000-00031. [DOI] [PubMed] [Google Scholar]
- 18.Mirastschijski U, Sander JT, Weyand B, et al. Rehabilitation of burn patients: An underestimated socio-economic burden. Burns. 2012 doi: 10.1016/j.burns.2012.06.009. [DOI] [PubMed] [Google Scholar]
- 19.Macintyre L, Baird M. Pressure garments for use in the treatment of hypertrophic scars—a review of the problems associated with their use. Burns. 2006;32:10–5. doi: 10.1016/j.burns.2004.06.018. [DOI] [PubMed] [Google Scholar]
- 20.Herndon DN, editor. Total Burn Care. 3rd ed. Philadelphia: Saunders Elsevier; 2007. [Google Scholar]
- 21.Ward RS. Pressure therapy for the control of hypertrophic scar formation after burn injury. A history and review. J Burn Care Rehabil. 1991;12:257–62. doi: 10.1097/00004630-199105000-00011. [DOI] [PubMed] [Google Scholar]
- 22.Sanchez JL, Pereperez SB, Bastida JL, et al. Cost-utility analysis applied to the treatment of burn patients in a specialized center. Arch Surg. 2007;142:50–7. doi: 10.1001/archsurg.142.1.50. discussion 7. [DOI] [PubMed] [Google Scholar]