Abstract
Objective:
The aim of this study was to determine the efficacy of a multimodal hand hygiene intervention program in reducing health care insurance claims for hygiene preventable infections (eg, cold and influenza), absenteeism, and subjective impact on employees.
Methods:
A 13.5-month prospective, randomized cluster controlled trial was executed with alcohol-based hand sanitizer in strategic workplace locations and personal use (intervention group) and brief hand hygiene education (both groups). Four years of retrospective data were collected for all participants.
Results:
Hygiene-preventable health care claims were significantly reduced in the intervention group by over 20% (P < 0.05). Absenteeism was positively impacted overall for the intervention group. Employee survey data showed significant improvements in hand hygiene behavior and perception of company concern for employee well-being.
Conclusion:
Providing a comprehensive, targeted, yet simple to execute hand hygiene program significantly reduced the incidence of health care claims and increased employee workplace satisfaction.
It has often been estimated that a large portion of infections are caused by hand transmission. Despite increasing awareness of the importance of hand washing and a range of other hygiene behaviors,1 many still become sick in the workplace, where viruses and bacteria can survive for hours to months on inanimate surfaces, for example, telephones and doorknobs, and spread to other individuals via direct or indirect contact.2,3 The typical office desk harbors more than 10 million bacteria, 400 times more germs than found on a standard toilet seat.4 High bacterial counts have been detected on elevator buttons, office phones, water fountains, computer keyboards, and vending machine buttons; particularly high viral counts were detected on desks, computer mice, and phones, especially in cubicles.5–7 Researchers swabbing 4800 surfaces in office buildings found “officially dirty” readings were highest on break room sink faucet handles (75% incidence of being dirty), microwave door handles (48% incidence of being dirty), computer keyboards (27% incidence of being dirty), and refrigerator door handles (26% incidence of being dirty).8
Health-related work losses cost US employers more than $260 billion each year,9 the indirect costs of poor health, most notably absenteeism and attending work while sick (known as “presenteeism”), exceed direct medical costs by two- to three-fold.10,11 The total economic cost of the common cold in the United States is estimated at $40 billion annually, only half of which is attributed to missed workdays.12 This financial burden is greater than that for many chronic conditions, including heart failure, asthma, and emphysema. In addition, cold sufferers spend more than $1.1 billion each year on antibiotic prescriptions, although antibiotics have no effect on viral illnesses.12
Despite preventative efforts, including vaccination, influenza epidemics exert considerable economic burden in the United States for adults, much of this due to lost productivity.13 U.S. workers lose approximately 3 days of work per influenza episode.14 Vaccination effectiveness may be limited by the inability to adequately target all circulating influenza virus strains; in the United States, vaccine efficacy was just 19% during the 2014 to 2015 influenza season.15 Only 28% of workers in the United States get the flu vaccine, most of them health care employees.14 A recent Cochrane review of 90 studies found that influenza vaccination had no appreciable effects on working days lost or hospitalization.16 Public health agencies and various policy groups stress the need to implement supplemental cost-effective strategies to prevent influenza infections in the workplace.14,17,18
The threat for infectious disease is high in the office setting simply because employees work in close proximity and share eating areas, workstations, and restrooms that harbor a broad spectrum of microorganisms.6 U.S. adults spend more time Monday through Friday at the workplace than anywhere else, including home, and about one-third of all workers spend an additional 5 hours at the office on weekends.7,19 The potential transmission of communicable diseases is exacerbated by the trend toward open-floor plan offices, which began in the 1990s and research suggests now applies to approximately 70% of US employees.20 Compounding the risk is that people work in closer proximity to each other, with the average amount of space per office worker in North America shrinking from 225 square feet in 2010 to 176 square feet in 2012, with a projection to be less than 100 square feet within 5 years.21 Workers sharing an open space are at a significantly higher risk for absences than occupants of private offices. A Danish national population-based study found that occupants in open-plan offices of more than six people had 62% more days of sickness absence.22 A large Swedish 2-year prospective study found a significant increase in short sick leaves and absence due to illness for those in open versus private offices.23 Workers in shared offices have, on average, two more episodes of common cold than those in private offices.24
Unplanned absence is a very significant cause for concern in controlling costs at the workplace and causes a high loss of productivity. In a 2014 survey of 512 workers, it was learned that unplanned absences have a significant negative impact on others (69% believe it adds to the workload, 61% believe it increases stress, 59% believe it disrupts the work of others, and 48% believe it hurts morale at the workplace).25 Numerous factors are increasing the financial impact of communicable disease for employers, including higher prevalence of influenza in the aging workforce, increased overtime for on-site employees due to absenteeism, and rising medical costs, such as insurance premiums.25–27 As of 2011, the majority (86%) of private sector employers in large companies (≥1000 people) were self-insured, and the trend to being a self-insured employer is growing.28 In a self-insured plan, the employer assumes the financial risk for providing health care benefits, paying out-of-pocket claims, as they are incurred rather than fixed premiums to an insurance carrier.28 The cost to insure an employee is rising, the average health care costs are projected to increase to over $11,500 per employee in 2016, of which the employer is projected to pay over $8800 per employee.29 Taken together, these developments underscore the imperative to implement simple, relatively low-cost, evidence-based strategies that prevent infectious illnesses in the workplace.
Hand hygiene has been proven to be one of the most effective means of reducing germ transmission in health care facilities and is the cornerstone of infection prevention programs. The Centers for Disease Control and Prevention (CDC), World Health Organization (WHO), and many other public health organizations issuing infection prevention guidance recommend alcohol-based hand sanitizers as the first choice for hand hygiene practice in clinical settings when hands are not visibly soiled30–33 and they are required upon hospital accreditation inspections.34 These guidelines are based on a wide body of evidence and studies that prove well-formulated alcohol-based hand sanitizers rapidly and effectively reduce a broad spectrum of bacterial and viral counts on hands, transmission of pathogens, and hospital-acquired infections, including antibiotic-resistant organisms such as methicillin-resistant Staphylococcus aureus (MRSA). The Institute for Healthcare Improvement guideline summarizes their status well: “alcohol-based hand rubs (liquids, gels, or foams) are the preferred method for hand hygiene in most settings due to the superior efficacy of these agents in rapidly reducing bacteria counts on hands and their ease of use.”33
Multiple studies demonstrate that implementing a hand hygiene program with alcohol-based sanitizers outside of health care settings significantly reduced illness-related absence and increased hand hygiene compliance.35–38 Student use of alcohol gel hand sanitizer in university dormitories reduced respiratory illness by up to 40% and missed school days by 43%.37 In one particularly successful program, implementing a “Buddies Hand Washing Program” brief education module in elementary schools combined with making alcohol-based hand sanitizers readily available reduced absenteeism by more than 50% (P < 0.001).36 In a US Army basic training facility, installation of alcohol-based handwash in mess halls and other strategic locations coupled with issuance of pocket-sized bottles resulted in 40% less respiratory illness, 48% less gastrointestinal illness, and 44% less lost training time.38 Currently, the military imposes a stringent hand hygiene protocol for new recruits, including required use of customized alcohol-based instant hand sanitizers.
To date, only a few studies examining hand hygiene programs in the workplace have been reported in the peer-viewed literature.39–42 In a German study, city workers given alcohol-based hand sanitizer experienced significant reductions in sick days and episodes of common cold, fever, and cough.39 Compliance remained high over the course of the 1-year trial and at the conclusion, the majority of participants favored continued use of the hand sanitizer in the workplace and skin problems, including dryness, were rarely reported.40 Another recent study in a US office building showed a hygiene program, including an alcohol-based hand sanitizer and disinfecting surface wipes, reduced viral transmission of a surrogate organism introduced on employee hands, with significantly fewer counts on hands and workplace surfaces (doorknobs, telephones, computer mice, desk chairs) after the intervention.3 The sole randomized prospective trial conducted in the United States, at a Midwestern government office building, showed a significant 31% relative reduction in self-reported acute respiratory illness, influenza, and/or gastrointestinal infection after 3 months of use of an alcohol-based hand sanitizer.41
The objective of our study was to evaluate the impact of a comprehensive workplace hand hygiene program on health care claims incidences and costs, absenteeism, and employee perceptions in the workplace. This is the first prospective study of a hand hygiene intervention program, including an alcohol-based hand sanitizer and sanitizing wipes at the employee's desk, to analyze for actual health care claims due to preventable illnesses with a hand-to-mouth mode of transmission (eg, cold and influenza, adenovirus, etc.).
METHODS
Study Design
The prospective, parallel-design, randomized cluster trial was conducted in three highly populated office buildings for employees in a Midwestern mutual health insurance company (Medical Mutual of Ohio, Cleveland) over a more than 13-month period from February 2014 through March 2015. The Chesapeake Research Review Institutional Review Board (IRB) assessed the study protocol and documentation, approved the study, and provided appropriate oversight throughout the process. In an effort to start the study during typical cold and flu season, baseline surveys were administered in January 2014. This study was composed of two clusters. The building with the most (782) employees was randomly assigned (as a cluster) to the control group. The 604 employees in the other two buildings (the second cluster) were consequently assigned to the intervention group. Because the study was low risk in nature, no consent forms were required.
All employees at the three facilities who were 18 years of age or older, were enrolled in the company health insurance coverage, did not transfer between sites and worked onsite full time (≥32 hours) were eligible for the study. The three buildings used in the trial had a similar open floor plan with the majority of employees sitting in cubicles. A small percentage (<15%) of traditional-style offices with doors lined the outer perimeter of each floor. The average amount of work space per worker in the intervention site was 309 square feet, similar to the control site at 323 square feet per worker. The intervention sites had a total space of 276,000 square feet, and the control site had a total space of 381,000 square feet.
The primary endpoints were (1) the number of health care insurance claims, for a defined set of preventable illnesses, per subject per year, and (2) absenteeism, defined as the number of sick episodes per subject per year. Sick episodes were calculated for each employee based on unscheduled paid time off (PTO) events lasting at least 4 hours. An unscheduled PTO event was defined as lasting at least 4 hours, where an event was counted as a single occurrence, whether the duration was 1 day or a series of consecutive unscheduled PTO days. This approach was chosen as the most accurate measure to evaluate the trial's hypothesis that alcohol-based hand sanitizer usage prevented communicable illness, as opposed to reducing severity of the illness, which is a different study question and would best be evaluated by length of PTO. Secondary outcomes focused on employee knowledge of appropriate hand hygiene practice and satisfaction at the workplace, as assessed by a thorough knowledge, attitudes, and practices (KAPS) survey. Another secondary outcome was estimation of hand hygiene frequency by employees in the intervention group. Historic data for health care claims and absenteeism were compiled for each subject for the 4 years before the study (2010 to 2014), which allowed more robust statistical analysis and higher confidence in conclusions.
Employee Knowledge, Attitudes, and Practices (KAPS) Subjective Survey
The KAPS survey was administered to all participants before the start of the trial (baseline) and 4 months into the trial (post study). Employees were given two weeks to complete each survey. The postsurvey was conducted at four months rather than later, for example, at the study's conclusion, to allow sufficient time for employees to familiarize themselves with the hand hygiene program, but not to allow so much time that their initial reactions to the program would be lost.
The KAPS survey was a focused evaluation yielding quantifiable data that measures change in KAPS in response to a specific intervention. Questions included demographics, knowledge of, and compliance with appropriate hand hygiene practice, perceptions and usage of the alcohol-based hand sanitizer, concerns regarding illness and cleanliness in the office, and impressions of the workplace environment and its amenities.
An e-mail was sent to all employees in January, 2014, stating that a hand hygiene research study was being conducted at the office and participation was voluntary. An incentive of 25 wellness points was offered to each employee who completed both the baseline and poststudy KAPS survey. Employees at Medical Mutual of Ohio earn wellness points for various health-related activities over the course of the year. When a certain point threshold is reached, monetary compensation toward health care premiums for the next year is granted. The 25 additional wellness points for completing a hand hygiene survey contributed to as much as 7% toward participating employees attaining monetary compensation in the Medical Mutual of Ohio 2014 Wellness incentive. Entry into a raffle for 1 of 100 $25 gift cards was offered as an added incentive for completing both surveys. The baseline survey also included demographic information and important covariates including age, gender, number of people in household, number of children less than 17 years of age in household, number of children in daycare, type of transportation to work (car, car pool, public transportation, bike, walk or other), and if employee received a flu vaccination in the fall of 2013.
Intervention Materials
On February 6, 2014, 11 days before the commencement of data collection, hand hygiene supplies were placed in the offices of the two intervention sites. Alcohol-based hand sanitizer (PURELL Advanced, GOJO Industries Inc, Akron, Ohio) was installed in high traffic common areas (eg, near elevators, at entrances) and other appropriate public spaces, including the coffee area, break rooms, conference rooms, training rooms, lobbies, and reception areas, as wall-mounted dispensers, stands, or free-standing bottles (depending on the environment and space available). An 8-ounce bottle of hand sanitizer (PURELL Advanced) and a 100-count canister of hand wipes (PURELL Wipes) were delivered to each cubicle. Every employee in the intervention group was also given a 1-ounce bottle of hand sanitizer (PURELL Advanced) for personal use. Replenishment product was stored in the supply room and made easily available to individual employees upon request (a simple process in case they ran out).
The restrooms in both the control and intervention sites provided foam handwash (GOJO Green Certified Foam Handwash) as well as an alcohol-based hand sanitizer foam wall-mounted dispenser (PURELL, GOJO Industries) near the restroom exit, which had been in place at all sites for months before the study. This sanitizer product was not removed from the control group restrooms during the study. We also ensured that the soap in all restrooms was identical, so the quality or personal preference of soap (which could impact usage behaviors) and hand hygiene options at the restroom was not a variable within the study.
Hand Hygiene Education
The intervention and control groups received identical education on hand hygiene and illness prevention. A brief (less than one-minute) educational video about proper hand hygiene technique, for both washing and sanitizing hands, was embedded at the end of the baseline online KAPS survey. The same signage to “Wash Your Hands,” promoting hand hygiene compliance, was posted next to restroom exits at both the control and intervention sites, and they were in place in advance of the study, not because of the study. No additional such signage was placed at the intervention sites.
Data Analysis
To evaluate health care claims, the International Classification of Diseases, 9th Revision, Clinical Modification (“ICD-9”) codes for illnesses with a hand-to-mouth mode of transmission (eg, cold and influenza, adenovirus, etc.) were selected before the implementation of the intervention.43 The study assessed 24 of the most common and appropriate diagnosis codes for these communicable, hand-to-mouth transmitted diseases considered to be preventable through effective hand hygiene (see Table 1).
TABLE 1.
Sick Claims: ICD-9 Codes for Cold and Flu Used in Study
| ICD-9 Diagnosis Code | Long Description |
| 460 | Acute nasopharyngitis [common cold] |
| 4610 | Acute maxillary sinusitis |
| 4611 | Acute frontal sinusitis |
| 4612 | Acute ethmoidal sinusitis |
| 4613 | Acute sphenoidal sinusitis |
| 4618 | Other acute sinusitis |
| 4619 | Acute sinusitis, unspecified |
| 462 | Acute pharyngitis |
| 4660 | Acute bronchitis |
| 46611 | Acute bronchiolitis due to respiratory syncytial virus (RSV) |
| 46619 | Acute bronchiolitis due to other infectious organisms |
| 4800 | Pneumonia due to adenovirus |
| 4809 | Viral pneumonia, unspecified |
| 4870 | Influenza with pneumonia |
| 00861 | Enteritis due to rotavirus |
| 00862 | Enteritis due to adenovirus |
| 00863 | Enteritis due to norwalk virus |
| 00865 | Enteritis due to calicivirus |
| 00866 | Enteritis due to astrovirus |
| 0088 | Intestinal infection due to other organism, not elsewhere classified |
| 07999 | Unspecified viral infection |
| 4658 | Acute upper respiratory infections of other multiple sites |
| 4659 | Acute upper respiratory infections of unspecified site |
| 4871 | Influenza with other respiratory manifestations |
The study included only paid facility (inpatient and outpatient) and professional medical claims for dates of service from February 17, 2014, to March 28, 2015, allowing for a three-month claims run-out time period to increase accuracy and eliminate invalid claims. Additional historical facility and professional claims were also evaluated for trending, including claims from February 18, 2010, to February 16, 2014. Analysis and data extraction were performed using SAS (Statistical Analysis System) software. Cold and influenza claims were identified using the primary diagnosis associated with each claim and evaluated by claim volume and cost.
The number of employees to be included in this study was calculated to detect a 20% reduction in the number of unscheduled PTO events between the intervention and the control groups, assuming a 0.05 P value and 80% power. Assuming an episode sick rate of 0.7 for 6 months and taking into consideration intracluster correction between the two groups and a potential nonresponse rate of 10%, the sample size was estimated at 495 individuals for each group.
To compare the incidence of claims and absenteeism between the two groups over time, a mixed-effects Poisson model was fit separately to claims and absenteeism. The fixed effects in the model were group (control or intervention), intervention period (pre- and post-), and the two-way interaction. To account for repeated measures from each subject, office building, and time period (1 to 6: five 12-month periods over the 4-year retrospective period and the first year of the intervention, and an additional 1.5-month period at the end of the study), random effects were included for time period, building, and subject. The model accounted for the total number of months worked by the employees in each group. Because the data were zero-inflated and no significant correlation was found among subjects in the same building, the data were aggregated by group and the random effect due to office building, was dropped for the final statistical analysis. Analyses were performed in R v.3.0.244 using packages lme445 and multcomp.46 One-tailed P values less than 0.05 were considered statistically significant. Statistical analysis of the subjective survey data (KAPS) was done by Chi-square, with P values less than 0.05 considered statistically significant. Demographic variables were compared using Chi-square for categorical variables and the Student t test for continuous variables.
RESULTS
A total of 1609 employees were asked to participate in the study; 1386 were included in the study of claims and absenteeism (782 in the control group and 604 in the intervention group); 1183 completed the baseline pre-study KAPS survey (627 in the control group and 556 in the intervention group). The flow diagram for the study population is shown in Fig. 1.
FIGURE 1.
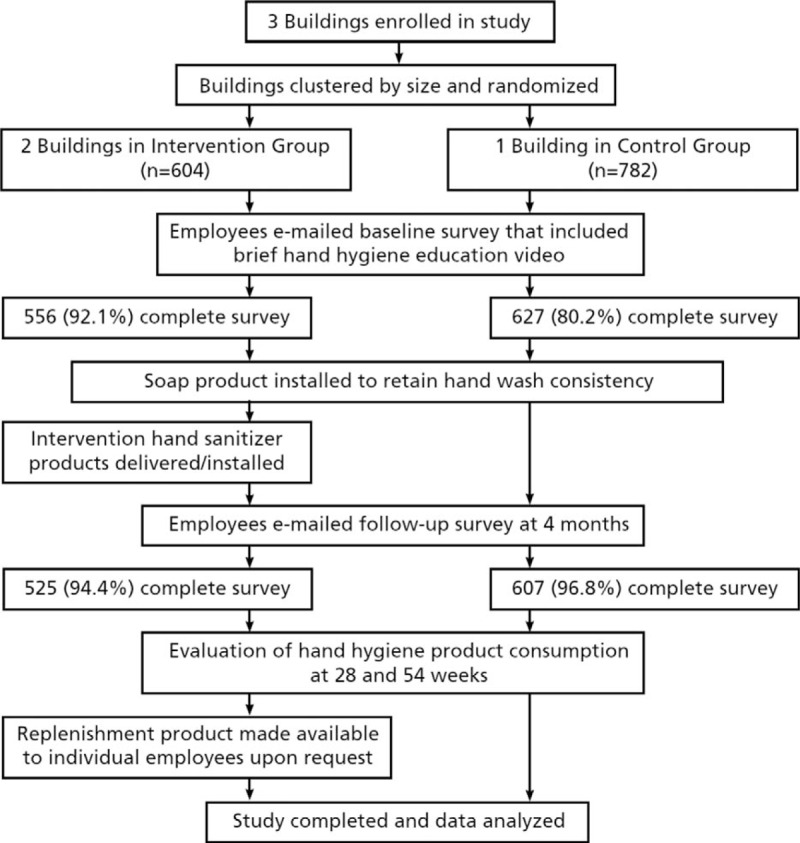
Flow diagram of study design with data collection.
The two groups did not differ significantly in gender, age, percentage receiving influenza vaccination, number of household members, or number of households with children aged 16 years or younger or in daycare. The only demographic profile characteristic that was statistically significant was mode of transportation to work. The finding that fewer employees in the control population drove their own car and took public transportation was not surprising given the more urban setting of that office building. Baseline characteristic details of the participants are shown in Table 2.
TABLE 2.
Baseline Demographics Analysis Summary
| Control Group (n = 607) | Intervention Group (n = 525) | P | |
| Mean (Std. Error) | Mean (Std. Error) | ||
| Age (yrs) | 47.0 (0.4) | 47.3 (0.4) | 0.68 |
| % (n) | % (n) | ||
| Gender (%) | |||
| Male | 22.4 (136) | 22.5 (118) | 0.97 |
| Female | 77.6 (471) | 77.5 (407) | |
| Number of people in household* | |||
| 1 | 19.2 (116) | 14.7 (77) | 0.18 |
| 2 | 35.3 (213) | 35.0 (183) | |
| 3 | 19.6 (118) | 21.6 (113) | |
| 4 | 14.9 (90) | 18.6 (97) | |
| ≥5 | 11.0 (66) | 10.1 (53) | |
| Households with children under 17 yrs of age (%) | 32.6 (198) | 34.7 (182) | 0.47 |
| Number of children under 17 yrs of age (%) | |||
| 1 | 48.0 (95) | 46.2 (84) | 0.68 |
| 2 | 33.3 (66) | 37.4 (68) | |
| ≥3 | 18.7 (37) | 16.5 (30) | |
| Households with children in daycare (%) | 6.1 (37) | 8.4 (44) | 0.14 |
| Number of children in daycare | |||
| 1 | 73.0 (27) | 75.0 (33) | 0.55 |
| 2 | 18.9 (7) | 22.7 (10) | |
| ≥3 | 8.1 (3) | 2.3 (1) | |
| Type of transportation to work | |||
| Car | 84.0 (510) | 99.6 (523) | <0.001 |
| Car pool | 2.5 (15) | 0.2 (1) | |
| Public transportation | 11.2 (68) | 0.0 (0) | |
| Bike | 0.3 (2) | 0.0 (0) | |
| Walk | 1.8 (11) | 0.2 (1) | |
| Other | 0.2 (1) | 0.0 (0) | |
| Received flu shot | 59.6 (362) | 62.7 (329) | 0.30 |
*There were six members who did not answer the specific question regarding the number of people living in their household (less than 1% of the total study population; should not impact the results).
During the first full year of the intervention period versus the prior 12 months, the intervention group had a statistically significant 24.3% lower incidence of hand hygiene preventable health care claims compared with the control group (P = 0.016). When factoring in the full 13.5-month intervention period and full 4 years of historical data, the intervention group still had a statistically significant 20.9% lower incidence of claims than the control group (P = 0.030), which is an even stronger conclusion regarding the efficacy and health outcome benefit of the intervention. The average number of health care claims per employee was 0.30 in the intervention group (179 claims among 604 subjects) compared with 0.37 for the control group (293 claims among 782 subjects). The claims data comparing the two groups for the intervention period and the four years before the study initiation is shown in Fig. 2. In the year before the study began, the intervention group actually had a 17.2% higher incidence of claims than the control group. If there had been no effect of the intervention (ie, no interaction between time and the intervention group), the claims rates would have risen similarly to the control group. However, the actual incidence of claims in the intervention group was 32.5% less than this prediction, which was statistically significant (P = 0.002).
FIGURE 2.
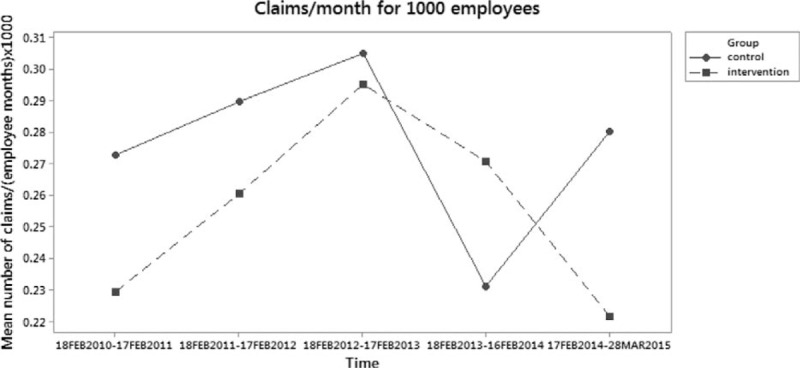
Health care claims per month per 1000 employees for the study period and prior four years.
For the second primary outcome measure of absenteeism, during the first full year of the intervention period versus the prior 12 months, the intervention group had 7.7% less absences (unscheduled PTO) compared with the control group, which was not statistically significant (P = 0.344). When factoring in the full 13.5-month intervention period and full 4 years of historical data, the intervention group had 5.0% less absenteeism episodes than the control group (P = 0.302). The average number of absences per employee in the intervention group was 1.45 (875 episodes among 604 subjects) compared with 1.53 for the control group (1193 episodes among 782 subjects). The absences data comparing the two groups for the intervention period and the four years before the study initiation are shown in Fig. 3. Analysis within the intervention group only was executed because it was hypothesized that the survey and video may have increased hand hygiene awareness of the control group. For the intervention group only during the first full year of the intervention period versus the prior 12 months showed employees with the intervention had a statistically significant 13.4% lower incidence of absences (P = 0.012), whereas the control group during the same one-year time interval had no significant change in absences. In the year before the study began, the intervention group actually had a 7.3% higher incidence of absences than the control group. If there had been no effect of the intervention (ie, no interaction between time and the intervention group), the absence rates would have risen similarly to the control group. However, the actual incidence of absences in the intervention group was 11.5% less than predicted that was statistically significant (P = 0.030).
FIGURE 3.
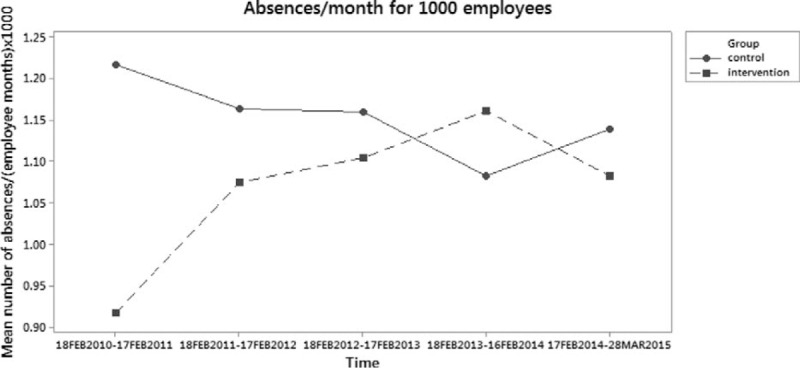
Absences per month per 1000 employees for the study period and prior four years.
The average cost of each claim for the hygiene-preventable illnesses included in both the control and intervention groups was $104 for the intervention period versus an average of $89 for the four years prior (see Table 3). In total, across the entire approximately five-year timeframe, the average cost per claim was $92. It should be noted that the cost of the health care claims assessed in the study does not necessarily translate into the severity of the illness, that is, a lower cost of a claim should not be construed to mean that the illness treated was less severe than a more costly claim. This is due to the fact that multiple factors comprise the claim's cost, including type of facility visited (doctor's office vs emergency room, etc.), cost differences due to geography, variance in negotiated contract rates by insurer with provider, etc.
TABLE 3.
Average Costs per Hygiene-Preventable Illness Claim
| Study Groups | Time Periods | No. of Claims | No. of Employees per Year | Total Cost | Cost per Claim |
| Both | Feb. 2010–Feb. 2014 | 1619 | 1161–1386 | $144,122 | $89.10 |
| Both | Feb. 2014–Mar. 2015 | 472 | 1386 | $49,170 | $104.06 |
| Both | Feb. 2010–Mar. 2015 | 2091 | 1161–1386 | $193,292 | $92.44 |
Table 4 assesses 14 companies’ health care expenditures across a broad range of industries for the year 2013. The % of total costs for the ICD-9 codes analyzed in this study was determined by comparison to each company's total health care cost. The % of total costs is similar across the employer categories, with a range of 0.7 to 1.6% and a midpoint of 1.2%. Neither the size of the company nor the level of the copay appears to have a notable effect on the result.
TABLE 4.
The Cost of Study Claims as a Percent of Total Employer Costs
| Employer Category | Number of Employees | Copays | Study ICD-9 Claims as % of Total Costs |
| Consumer products | >1000 | $20 or $35 | 1.3% |
| Automatic merchandising Machine operator | >1000 | $20 or $35 | 0.9% |
| Installation of building equipment | >1000 | $20 | 0.9% |
| Religious organization | >5000 | $15 | 0.7% |
| Commercial banking | >1000 | $25 | 0.9% |
| Electric services | >5000 | $0 | 0.8% |
| General contractors | >1000 | $15 or $25 | 0.9% |
| Construction and mining | >1000 | $15 or $30 | 1.4% |
| Commercial banking | >10,000 | $20 or $40 | 0.9% |
| Mortgage bankers | <1000 | $15 or $25 | 1.6% |
| Jewelry Industry | >5000 | $30 | 1.2% |
| Pension, Health, and Welfare Fund | >10,000 | $0 | 1.0% |
| General Contractors | >10,000 | $15 or $35 | 0.7% |
| School | >10,000 | $15 or $20 | 1.0% |
| Range = | 0.7%–1.6% |
Hand hygiene knowledge at baseline did not differ between the control and intervention groups (see Table 5). Knowledge of hand hygiene practice was high, with at least nine in 10 employees citing the need of hand hygiene in six of the nine situations presented. Knowledge regarding technique and reason hand hygiene is effective were also high and did not differ between control and intervention groups.
TABLE 5.
Hand Hygiene Knowledge at Baseline
| Control Group n = 627 | Intervention Group n = 557 | P | |
| % (n) | % (n) | ||
| Situations where hand hygiene should be performed | |||
| After using the restroom | 99% | 98% | 0.08 |
| After coming into contact with someone who is ill | 96% | 97% | 0.70 |
| After touching items that could be contaminated (trash, diapers, elevator buttons, etc.) | 95% | 96% | 0.47 |
| After sneezing or coughing | 94% | 94% | 0.56 |
| Before eating | 93% | 92% | 0.37 |
| While preparing food | 93% | 91% | 0.26 |
| After coming into contact with someone who is injured | 66% | 68% | 0.30 |
| After eating | 59% | 61% | 0.48 |
| Before using the restroom | 33% | 34% | 0.65 |
| Expert recommended length of time to wash (s) | |||
| 10–15 | 6% | 4% | 0.31 |
| 15–20 | 17% | 17% | |
| 20–25 | 18% | 20% | |
| 25–30 | 22% | 19% | |
| 30–35 | 19% | 19% | |
| More than 35 | 18% | 21% | |
| Reason hand hygiene is effective in reducing risk of illness | |||
| Hand hygiene reduces risk of letting germs into your body | 81% | 82% | 0.78 |
| Hand hygiene kills germs | 81% | 82% | 0.78 |
| Hand hygiene keeps your hands clean | 67% | 69% | 0.50 |
| None of the above | 1% | 1% | 0.75 |
Implementation of the program significantly improved self-reported hand hygiene practice and attitudes in the intervention group, with increased frequency of hand washing (self-reported), employee satisfaction with office cleanliness, and perception that company cared for their well-being and disease prevention in the workplace (P < 0.05). At the intervention sites, the availability of the product significantly increased participant's sense of control of their health/well-being, ability to interact with coworkers in the workplace environment without worry about transmissible illness, satisfaction with hand hygiene products provided by their employer, likelihood to comply with optimum hand hygiene practice, and overall positive impression of their company (P < 0.05).
Following introduction of an alcohol-based hand sanitizer in the office, 40% more employees in the intervention group reported cleaning their work area regularly to prevent illness compared with both the baseline (P < 0.001) and control group (P < 0.001). The intervention group was also significantly more likely to keep the hand sanitizer with them and use it throughout the day—at work (P < 0.001), home (P = 0.017), and in public places (P = 0.037), such as grocery stores, malls, restaurants, health care facilities, banks, and airports (see Fig. 4). Employees in the intervention group reported significant increases in alcohol-based hand sanitizer use for every activity assessed, including before eating (P = 0.001), after sneezing (P < 0.001), coughing (P < 0.001), handling money (P < 0.001), using the restroom (P = 0.005), returning to their desk (P < 0.001), and interacting with others who may be sick (P < 0.001).
FIGURE 4.
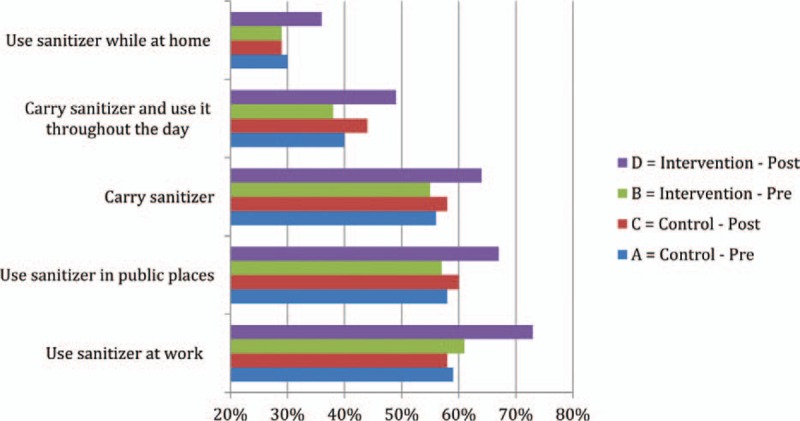
Overall frequency of carrying and using alcohol-based hand sanitizer per study group and pre- versus postsurvey.
Surprisingly, the availability of PURELL hand wipes at individual desks had a stronger impact on workers’ impression of the office space than many other amenities, including filtered water, a recycling program, low-cost food, free coffee/soda, and ATM/banking. A total of 81% employees in the intervention group ranked the availability of alcohol-based hand sanitizer wipes at their individual desk as one of the top two amenities in the workplace compared with 69% before the intervention (P < 0.001) and 71% of controls (P = 0.001).
Employees in the intervention group were significantly more likely than the control group to have a positive impression of Medical Mutual of Ohio because of the presence of alcohol-based hand sanitizers in the workplace (80% vs 69%, P < 0.001). There was also a significant increase in employee perception that their company was concerned about the spread of germs and illness in the workplace (80% vs 60%, P < 0.001). The intervention group reported higher satisfaction with the overall cleanliness of the office space than control group personnel as well (P < 0.001). Importantly, 88% of the employees in the intervention group postsurvey liked the intervention products provided.
DISCUSSION
This is the first prospective workplace study evaluating a comprehensive hand hygiene program with an alcohol-based hand sanitizer to report actual medical insurance claims. The results clearly demonstrate that intervention of a healthy office program with provision of alcohol-based hand sanitizer throughout a building and hand sanitizer along with hand wipes in the personal workspace improves employee health outcomes and job satisfaction.
For the intervention group, there were significant increases in frequency of hand hygiene for all activities assessed in the study. The intervention group was significantly more likely to clean their work area with sanitizing wipes as well as a surface spray (not provided) in order to prevent illness. Increased hand hygiene practice was documented in all of the settings recommended by CDC guidance: after sneezing, coughing, and contact with others who may be sick, before eating, and after use of the restroom.47 The CDC states that hand hygiene is one of the best ways to reduce absenteeism and avoid contracting and spreading illness in the workplace and recommends that employers promote handwashing among employees and their family.48 To prevent influenza in the workplace, the CDC recommends that employers provide alcohol-based hand sanitizers and gels when sinks and soaps are not available and place handwashing reminders in bathrooms, kitchens, break rooms, and other communal areas with sinks.17
Antibiotic resistance has grown into a crisis of alarming proportion, with the hospital setting currently recognized by public health agencies and the US government as posing an unacceptable risk for infection; one of every 25 inpatients in acute care hospitals in the United States contracts one or more infections.49,50 Each year, in the United States, approximately 2 million people become infected with drug-resistant bacteria, resulting in at least 23,000 deaths.51 Antibiotic-resistant pathogens cost the U.S. health care system an estimated $20 billion each year.52 Moreover, few new antibiotics are being invented, due to the expense and time it takes to develop novel drug classes coupled with limited projected revenue.53 Prevention of infections in any setting, including workplaces, reduces the need for antibiotics and thereby reduces the risk of developing antibiotic resistance.
According to the National Institutes of Health, the best strategy to prevent the spread of drug-resistant bacteria is “for everyone to keep their hands clean.”54 Many leading professional medical associations and the recently convened White House Task Force on Antibiotic Stewardship also recommend prevention as one of most important strategies to combat the crisis of antibiotic resistance and rising health care costs.50,55 Hygiene and alcohol-based hand sanitizers are an important modality in the fight to combat antibiotic resistance, because, unlike other interventions, there is no mechanism for bacteria to develop resistance to alcohol. Alcohol kills bacteria by physically destroying the cell membrane and denaturing proteins within the bacteria; doing so while evaporating from skin within seconds, leaving no residual active behind that could lead to mutation.
Another important, yet often ignored aspect of hygiene is product selection. Proper formulation of soaps, surface cleaners, and alcohol-based hand rubs is required to maximize antimicrobial efficacy and achieve satisfying human factors (eg, likeability, skin feel, skin conditioning, etc.). It has been found that poor formulation and delivery system design in hand soaps can lead to microbial contamination and growth.56,57 A study of 12 hand sanitizer gel and foam products evaluating antibacterial efficacy on hands found that formulation matters and is a more important factor than alcohol concentration alone.58,59 Therefore, it should not be assumed that intervention with different hand hygiene products will produce similar health benefits.
As a corollary to product selection, this study sets out to understand the impact the specific products and their placement had on product usage. This was achieved through monitoring of product shipments into the sites and physical collection of the soap, sanitizer, and wipes products from the intervention sites at two times in the study (evening collection with full replacement product was provided, so there was no disruption of the intervention test conditions). The collected samples were measured and usage rates were estimated (given that the office worker could use product at their desk or in the general work areas, the results should be considered directional in nature). Our estimates suggest that an average employee used the sanitizer 1.8 to 3.0 times per day, the soap 2.1 to 4.4 times per day, and the wipes at their desk 1.4 to 1.5 times per week. These data suggest very reasonable, realistic levels of usage, and contradict any notion that the positive health outcomes were due to extremely high frequency of hand hygiene. Rather, an average sanitizer usage rate of two to three times per day per employee and sanitizing wipes usage rates of one to two times per week per employee should be considered highly attainable and fits well with expected behaviors (eg, to clean hands before eating, after sneezing, etc.). Further study of the relationship of hand hygiene rates and timing with health outcomes would be interesting.
The practice of attending work while sick, also known as presenteeism, hinders employee productivity and has negative economic implications. The estimated annual cost of presenteeism caused by respiratory disorders exceeds $33 per employee.11 Although this study did not attempt to quantify the impact of the hand hygiene intervention on costs linked to presenteeism, it is reasonable to assume that the intervention's demonstrated reduction in health care claims would have a similarly positive impact on reducing presenteeism costs caused by respiratory disorders. This is especially relevant given that the hygiene-preventable infections assessed in this study do not frequently lead a person to seek professional medical attention. In fact, frequency of doctor visits for common cold-type illness has been reported to be as low as 4%.60
Workplaces share some of the same risks of health care settings: employees work in close quarters, share open spaces, are often a significant distance from sinks, and may be too occupied with the task at hand to go to the restroom to wash their hands with soap and water. Recommendations accrued from years of study of hand hygiene techniques and compliance in health care settings are now starting to be applied to other settings, such as schools,35–37 military,38 and more recently office based workplaces. Hospital-based public health researchers have learned that a key factor influencing adherence to optimum hand hygiene protocol is the product's availability at the point of need.32 The World Health Organization promotes the alcohol-based handrub as the international standard of care for hand hygiene, as it is “the most efficacious, well-tolerated and well-researched product which can be placed ergonomically and safely at the point of care.”32
Research accumulated over the past three decades shows that well-designed wellness programs based on evidence-based principles of health achieve significant positive health and financial outcomes in the workplace, for both the employer and employees. The impact is highest when programs emphasize a “culture of health.”61 A meta-analysis of 72 studies revealed that every $1 spent on workplace wellness programs yielded an average return of $3.50.62 A Harvard study found that, over a 3-year period, medical costs fell by $3.27 for every dollar spent on wellness programs and absenteeism costs fell by about $2.73 for every dollar spent.63 According to another meta-analysis evaluating 62 peer-reviewed studies that met stringent inclusion criteria, worksite health programs reduce sick leave absenteeism by 25% on average and worker's compensation and disability claims costs by 32% on average, with an overall $5.56 to $1 savings-to-cost ratio.64
There are some important limitations in our study. The control group having more exposure to other people via public transportation may have impacted employee health outcomes, but that is not well understood. Other factors besides hygiene preventable illnesses likely contributed to absences, and it is well known that absenteeism, self-reported or measured by unscheduled PTO as in this case, is an ambiguous metric prone to error for a variety of reasons (eg, staying home to care for a loved one, etc.). The rough estimation of actual hand hygiene frequency in this study still does not determine what level of hand hygiene is needed to reduce illnesses at an individual level. Finally, the seasonal effects and relationship with this hygiene intervention are not well understood. Further analysis should be done with these data and future studies should attempt to better determine whether health outcome results are different in the winter germ season, during peak cold and flu season, or during the summer.
In summary, the simplest and most cost-effective strategy to combat common infectious agents in the workplace is to provide hand hygiene options at the point of exposure. Alcohol-based hand rubs are more effective than routine hand washing in reducing viable bacteria and viruses on hands, require less time to use, are more accessible at the point of care, increase adherence to recommended hand hygiene protocol, and cause less hand irritation and dryness with repeated use than other products.32
CONCLUSION
This prospective, randomized, cluster-controlled trial demonstrated that a healthy office program based on comprehensive hand hygiene improvement at the individual employee level, used in conjunction with alcohol hand sanitizers strategically placed in the workplace, significantly reduced actual health care claims for hand hygiene preventable infections (eg, cold and influenza). Furthermore, implementation significantly improved employee satisfaction and hand hygiene knowledge and behavior. These findings support the recommendations of many leading public health organizations to implement hygiene programs as a key nonpharmaceutical strategy to reduce the health and economic burden of illness and reduce the risk of infection during work.
Acknowledgments
The authors thank Thom Wojtkun from GOJO Industries, Inc. for critical thinking, problem solving, and substantial effort in bringing the study to closure from start to finish. The authors also thank other GOJO Industries, Inc contributors including Sarah Edmonds Wilson and Jeb Bingham for input on study design and support during the IRB review and Jane Kirk for draft manuscript editorial input, Ken Payne, Jeff Williamson, Nancy Ross-Bell, Connie Beutel (MMO), and Carin Crislip (GOJO) for critical support in logistics and execution of the study, and Lee Williams and Todd Carley from Writing Assistance, Inc for technical writing support.
Footnotes
No funding was received for this work from any of the following organizations: National Institutes of Health (NIH); Wellcome Trust; Howard Hughes Medical Institute (HHMI); and other(s).
There are no significant conflicts of interest.
GOJO Industries, Inc. provided all products at no cost to Medical Mutual of Ohio and covered all expenses associated with the study (eg, the cost of the IRB, consultant fees, etc.). Medical Mutual of Ohio provided the study locations and subjects at no cost.
There were no other sources of support.
REFERENCES
- 1.American Society for Microbiology, American Cleaning Institute. A Survey of Handwashing Behavior. Rochester, NY: Harris Interactive; 2010August [Google Scholar]
- 2.Department of Occupational and Environmental Health in the College of Public Health at The University of Iowa. Hand hygiene = healthier workplace. A health and safety bulletin from UI HealthWorks and WORKSAFE IOWA. Published December 2013. Available at: http://cph.uiowa.edu/worksafe/pubs/bulletin/Dec-2013.html Accessed July 13, 2015. [Google Scholar]
- 3.Reynolds KA, Beamer PI, Plotkin KR, Sifuentes LY, Koenig DW, Gerba CP. The Healthy Workplace Project: reduced viral exposure in an office setting. Arch Environ Occup Health 2015; [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gerba CP via personal communication. Germs in the workplace. An unpublished observational study conducted at the University of Arizona. 2013. [Google Scholar]
- 5.Boone SA, Gerba CP. The prevalence of human rainfluenza virus 1 on indoor office fomites. Food Environ Virol 2010; 2:41–46. [Google Scholar]
- 6.Hewitt KM, Gerba CP, Maxwell SL, Kelley ST. Office space bacterial abundance and diversity in three metropolitan areas. PLoS One 2012; 7:e37849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sheldon PJ. Top 5 germiest places in the workplace. OH&S (Occupational Health & Safety) E News. December 21, 2010. Available at: https://ohsonline.com/articles/2010/12/21/top-5-germiest-places-in-the-workplace.aspx Accessed July 13, 2015. [Google Scholar]
- 8.DeNoon DJ. The 6 dirtiest places in your office: where office germs lurk in break rooms, on desks. WebMD. Available at: http://www/webmd.com/news/2012023/the-6-dirtiest-work-places. Published May 22, 2012 Accessed July 13, 2015. [Google Scholar]
- 9.Davis K, Collins SR, Doty MM, Ho A, Holmgren AL. Health and productivity among US workers. Issue Brief (Commonw Fund) 2005; 856:1–10. [PubMed] [Google Scholar]
- 10.Hemp P. Presenteeism: at work—but out of it. Harv Bus Rev 2004; 82:49–58. [PubMed] [Google Scholar]
- 11.Goetzel RZ, Long SR, Ozminkowski RJ, Hawkins K, Wang S, Lynch W. Health, absence, disability, and presenteeism cost estimates of certain physical and mental health conditions affecting US employers. J Occup Environ Med 2004; 46:298–412. [DOI] [PubMed] [Google Scholar]
- 12.Fendrick AM, Monto AS, Nightengale B, Sarnes M. The economic burden of non–influenza-related viral respiratory tract infection in the United States. Arch Intern Med 2003; 163:487–494. [DOI] [PubMed] [Google Scholar]
- 13.Molinari NA, Ortega-Sanchez IR, Messonnier ML, et al. The annual impact of seasonal influenza in the US: measuring disease burden and costs. Vaccine 2007; 25:5086–5096. [DOI] [PubMed] [Google Scholar]
- 14.Tsai Y, Zhou F, Kims IK. The burden of influenza-like illness in the US workforce. Occup Med (Lond) 2014; 64:341–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. CDC Presents Updated Estimates of Flu Vaccine Effectiveness for the 2014-2014 Season. Available at: http://www.cdc.gov/flu/news/updated-vaccine-effectiveness-2014-15.htm Published March 2, 2015 Accessed July 10, 2015. [Google Scholar]
- 16.Demicheli V, Jefferson T, Al-Ansary LA, Ferroni E, Rivetta A, Di Petrantonj C. Vaccines for preventing influenza in healthy adults (review). Cochrane Database Syst Rev 2014; 3:CD01269. [DOI] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention. Seasonal Influenza (flu) in the Workplace. Available at: http://www.cdc.gov/niosh/topics/flu/guidance.html Updated February 1, 2013 Accessed July 10, 2015. [Google Scholar]
- 18.National Business Group on Health. Vaccinating Against the Flu: a Business Case. Issue Brief. Washington, DC: National Business Group on Health, Center for Prevention and Health Services; September 2010. [Google Scholar]
- 19.White C, Kolble R, Carlson R, Lipson N, Dolan M, Ali Y, Cline M. The effect of hand hygiene on illness rate among students in university residence halls. Am J Infect Control 2003;31:364–370. [DOI] [PubMed] [Google Scholar]
- 20.International Facilities Management Association (IFMA). Space and Project Management Benchmarks: IFMA Research Report #34. Houston, TX: IFMA; 2010. [Google Scholar]
- 21.PR Newswire. Office Space Per Worker Will Drop to 100 Square Feet or Below for Many Companies Within Five Years, According to New Research From CoreNet Global. Published February 2012. Available at: http://www.prnewswire.com/news-releases/office-space-per-worker-will-drop-to-100-square-feet-or-below-for-many-companies-within-five-years-according-to-new-research-from-corenet-global-140702483.html Accessed July 15, 2015. [Google Scholar]
- 22.Pejtersen JH, Fevell H, Christensen KB, Burr H. Sickness absence associated with shared and open-plan offices—a national cross sectional questionnaire survey. Scand J Work Environ Health 2011; 37:376–382. [DOI] [PubMed] [Google Scholar]
- 23.Danielsson CB, Chungkham HS, Wulff C, Westerlund H. Office design's impact on sick leave rates. Ergonomics 2015; 57:139–147. [DOI] [PubMed] [Google Scholar]
- 24.Jakkola JK, Heinonen OP. Shared office space and the risk of the common cold. Eur J Epidemiol 1995; 11:213–216. [DOI] [PubMed] [Google Scholar]
- 25.Society for Human Resource Management. Executive Summary: Total Financial Impact of Employee Absences in the U.S. Published August 2014. Available at: http://www.shrm.org/research/surveyfindings/documents/kronos_us_executive_summary_final.pdf Accessed July 15, 2015. [Google Scholar]
- 26.McLaughlin JM, McGinnis JJ, Tan L, Mercatante A, Fortuna J. Estimated human and economic burden of four major adult vaccine-preventable diseases in the United States, 2013. J Primary Prevent 2015; 36:259–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Conner SC. Building wellness programs with impact. Occup Health Saf 2013; 82:62–63. [PubMed] [Google Scholar]
- 28.Fronstin P. Self-insured health plans: state variation and recent trends by firm size. Employee Benefit Research Institute Notes 2012; 33:2–10. [Google Scholar]
- 29.CFO.com. Hike in Health-Care Costs Sinks to 20-Year Low, Costs for large companies rose just 3.2% this year, according to Aon Hewitt. Available at: http://ww2.cfo.com/health-benefits/2015/11/hike-health-care-costs-sinks-20-year-low/ Published and Accessed November 12, 2015. [Google Scholar]
- 30.Boyce JM, Pittet D. Healthcare Infection Control Practices Advisory Committee; HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Guideline for hand hygiene in health-care settings: recommendations of the Healthcare Infection Control Practices Advisory Committee and the HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. MMWR Recomm Rep 2002; 51 (RR-16):1–45. [PubMed] [Google Scholar]
- 31.World Health Organization. WHO Guidelines on Hand Hygiene in Health Care: First Global Patient Safety Challenge Clean Care is Safer Care. Geneva, Switzerland: WHO; 2009. [PubMed] [Google Scholar]
- 32.World Health Organization. System Change—Changing Hand Hygiene Behavior at the Point of Care. Available at: http://www.who.int/gpsc/tools/faqs/system_change/en/ Published 2015. Accessed July 10, 2015. [Google Scholar]
- 33.Institute for Healthcare Improvement. How-to Guide: Improving Hand Hygiene: A Guide for Improving Practices Among Health Care Workers. Cambridge, MA: 2006. pp. 1–28. Available at: http://www.ihi.org/resources/pages/tools/howtoguideimprovinghandhygiene.aspx Accessed April 6, 2016. [Google Scholar]
- 34.Joint Commission. Measuring Hand Hygiene Adherence: Overcoming the Challenges. Oakbridge Terrace, IL: The Joint Commission; 2009. [Google Scholar]
- 35.Hammond B, Ali Y, Fendler E, Dolan M, Donovan S. Effect of hand santizer use on elementary school absenteeism. Am J Infect Control 2000; 28:340–346. [DOI] [PubMed] [Google Scholar]
- 36.Guinan M, McGuckin M, Ali Y. The effect of a comprehensive handwashing program on absenteeism in elementary schools. Am J Infect Control 2002; 30:217–220. [DOI] [PubMed] [Google Scholar]
- 37.White C, Kolble R, Carlson R, Lipson N. The impact of a health campaign on hand hygiene and upper respiratory illness among college students living in residence halls. J Am Coll Health 2005; 53:175–181. [DOI] [PubMed] [Google Scholar]
- 38.Mott PJ, Sisk BW, Arbogast JW, Ferrazzano-Yaussy C, Bondi CA, Sheehan JJ. Alcohol-based instant hand sanitizer use in military settings: a prospective cohort study of army basic trainees. Mil Med 2007; 172:1170–1176. [DOI] [PubMed] [Google Scholar]
- 39.Hübner NO, Hübner C, Wodny M, Kampf G, Kramer A. Effectiveness of alcohol-based hand disinfectants in a public administration: impact on health and work performance related to acute respiratory symptoms and diarrhoea. BMC Infect Dis 2010; 10:250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hübner NO, Hübner C, Kramer A. Impact of health campaign on hand hygiene with alcohol-based hand rubs in a non-clinical setting. J Hosp Infect 2013; 83 suppl 1:S23–S28. [DOI] [PubMed] [Google Scholar]
- 41.Stedman-Smith M, Dubois CL, Grey SF, et al. Outcomes of a pilot hand hygiene randomized cluster trial to reduce communicable infections among US office-based employees. J Occup Environ Med 2015; 57:374–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Savolainen-Kopra C, Haapakoski J, Peltola PA, et al. Hand washing with soap and water together with behavioral recommendations prevents infections in common work environments: an open cluster randomized trial. Trials 2012; 13:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Centers for Medicare & Medicaid Services. ICD-9-CM Diagnosis and Procedure Codes: Abbreviated and Full Code Titles, Version 31 Full and Abbreviated Code Titles – Effective October 1, 2013, https://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes.html Accessed November 2013. [Google Scholar]
- 44.R Core Team (2013). R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria. Available at: http://www.R-project.org/ Accessed November 18, 2015. [Google Scholar]
- 45.Bates D, Maechler M, Bolker B, Walker S. lme4: Linear mixed-effects models using Eigen and S4. R package version 1.1-5. 2014. Available at: http://CRAN.R-project.org/package=lme4 Accessed November 18, 2015. [Google Scholar]
- 46.Hothorn T, Bretz F, Westfall P. Simultaneous inference in general parametric models. Biom J 2008;50(3):346–363. [DOI] [PubMed] [Google Scholar]
- 47.Centers for Disease Control and Prevention. Clean Hands Save Lives! Available at: http://www.cdc.gov/h1n1flu/pdf/handwashing.pdf Updated July 22, 2015. Accessed July 29, 2015. [Google Scholar]
- 48.Centers for Disease Control and Prevention. Everyday Preventive Actions That Can Help Fight Germs, Like Flu. Available at: http://www.cdc.gov/flu/pdf/freeresources/updated/everyday_preventive_9-24.pdf Updated August 21, 2012. Accessed December 19, 2015. [Google Scholar]
- 49.Magill SS, Edwards JR, Bamberg W, et al. Emerging Infections Program Healthcare-Associated Infections and Antimicrobial Use Prevalence Survey Team. Multistate point-prevalence survey of health care-associated infections. N Engl J Med 2014; 370:1198–1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.National Action Plan for Combating Antibiotic-resistant Bacteria. Washington, DC: The White House; March 2015. Available at: https://www.whitehouse.gov/sites/default/files/docs/national_action_plan_for_combating_antibotic-resistant_bacteria.pdf Accessed December 19, 2015. [Google Scholar]
- 51.Centers for Disease Control and Prevention. Antibiotic Resistance Threats in the United States, 2013. Available at: http://www.cdc.gov/drugresistance/threat-report-2013 July 17, 2104. Accessed July 29, 2015. [Google Scholar]
- 52.Hughes JM. Preserving the lifesaving power of antimicrobial agents. JAMA 2011; 305:1027–1028. [DOI] [PubMed] [Google Scholar]
- 53.Leff J, Coukell A. How to end the regulatory slowdown for new antibiotics. Wall Street Journal. July 3, 2015. [Google Scholar]
- 54.National Institutes of Health. NIH Clinical Center Patient Education Materials Vancomycin-Resistant Enterococcus (VRE). Bethesda, MD: US Department of Health and Human Services; Available at: http://cris.cc.nih.gov/pptemp/pt_care/pdfs/vre.pdf Accessed December 19, 2015. [Google Scholar]
- 55.Special Committee on Health. Productivity, and Disability Management, American College of Occupational and Environmental Medicine. Healthy workforce/healthy economy: the role of health, productivity, and disability management in addressing the nation's health care crisis: why an emphasis on the health of the workforce is vital to the healthy of the economy. J Occup Environ Med 2009; 51:114–119. [DOI] [PubMed] [Google Scholar]
- 56.Chattman M, Maxwell SL, Gerba CP. Occurrence of heterotrophic and coliform bacteria in liquid hand soaps from bulk refillable dispensers in public facilities. J Environ Health 2011; 73:26–29. [PubMed] [Google Scholar]
- 57.Zapka CA, Campbell EJ, Maxwell SL, et al. Bacterial hand contamination and transfer after use of contaminated bulk-soap-refillable dispensers. Appl Environ Microbiol 2011; 77:2898–2904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Edmonds SL, Macinga DR, Mays-Suko P, et al. Comparative efficacy of commercially available alcohol-based hand rubs and World Health Organization-recommended hand rubs: formulation matters. Am J Infect Control 2012; 40:521–555. [DOI] [PubMed] [Google Scholar]
- 59.Macinga D, Shumaker D, Werner P, Edmonds S, Leslie R, Parker A, Arbogast J. The relative influences of product volume delivery format and alcohol concentration on dry-time and efficacy of alcohol-based hand rubs. BMC Infect Dis 2014;14:511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Keast D, Marshall JN, Stewart M, et al. Why do patients seek family physicians’ services for cold symptoms? Canadian Family Physician 1999; 45:335–340. [PMC free article] [PubMed] [Google Scholar]
- 61.Goetzel RZ, Henke RM, Tabrizi M, et al. Do workplace health promotion (wellness) programs work? J Occup Environ Med 2014; 56:927–934. [DOI] [PubMed] [Google Scholar]
- 62.Aldana SG, Merrill RM, Price K, Hardy A, Hager R. Financial impact of a comprehensive multisite workplace health promotion program. Prev Med 2005; 40:131–137. [DOI] [PubMed] [Google Scholar]
- 63.Baicker K, Cutler D, Song Z. Workplace wellness programs can generate savings. Health Aff 2010; 29:304–311. [DOI] [PubMed] [Google Scholar]
- 64.Chapman LS. Meta-evaluation of worksite health promotion economic return studies: 2012 update. Am J Health Promot 2012; 26:TAH1–TAH12. [DOI] [PubMed] [Google Scholar]


