Supplemental Digital Content is available in the text
Abstract
Objective:
Evaluation of the effectiveness of a workplace health promotion program on employees’ vitality, health, and work-related outcomes, and exploring the influence of organizational support and the supervisors’ role on these outcomes.
Methods:
The 5-month intervention included activities at management, team, and individual level targeting self-management to perform healthy behaviors: a kick-off session, vitality training sessions, workshops, individual coaching, and intervision. Outcome measures were collected using questionnaires, health checks, and sickness absence data at baseline, after the intervention and at 10 months follow-up. For analysis linear and generalized mixed models were used.
Results:
Vitality, work performance, sickness absence, and self-management significantly improved. Good organizational support and involved supervisors were significantly associated with lower sickness absence.
Conclusions:
Including all organizational levels and focusing on increasing self-management provided promising results for improving vitality, health, and work-related outcomes.
In the past decades, workplace health promotion emerged as a popular strategy for health and cost benefits.1,2 Workplace health promotion programs (WHPPs) aim to improve lifestyle and consequently improve health and work-related outcomes.3 Several reviews have demonstrated that WHPPs have a positive effect on overall health and wellbeing,4 mental health, that is, depression and anxiety,5,6 and nutrition and physical activity.7–10 Besides general health improvements, work-related outcomes as sickness absence,5,11 work productivity and presenteeism12 can be positively influenced by these programs. In combination with cost-effectiveness, WHPPs become attractive programs to companies.11
Recently, a new WHPP was developed focusing on two relevant company aspects: “Energy”—an important element of individual vitality13 and “Performance”—an important element of employability.14 This WHPP integrated several critical success factors that are recognized by the World Economic Forum.15 These include strong management support; effective communication and involvement of employees at both the individual and team level; and providing incentives to foster adherence. A key element of the intervention was improving self-management with regard to individual vitality. Self-management relates to the active participation of an individual in a treatment or in ensuring health maintenance.16 It includes elements as goal setting and action planning, which appear to be critical to perceived health improvements, enhance treatment compliance, and motivate behavior change.16–18 Therefore, this intervention made use of goal setting techniques, reflective counseling, and motivational interviewing by vitality coaches as effective strategies.17 It was hypothesized that by increasing (self-)awareness and knowledge of health practices, and stimulating ownership and responsibility, the employee is willing and able to improve its health behavior, resulting in improved health and vitality, which in turn should improve work performance and decrease presenteeism and sickness absence.3
The aim of the present study was to evaluate the effect of this WHPP on four primary outcome measures: employees’ vitality, work performance, presenteeism, and sickness absence. In addition, the effectiveness of the WHPP was assessed on several intermediate health and health-related outcomes, including self-management, self-rated vitality and health, attitude and intention with regard to healthy behavior, risk factors for cardiovascular diseases (total cholesterol level, systolic blood pressure, and fat percentage), lifestyle (smoking, alcohol consumption, fruit and vegetables consumption, moderate to vigorous physical activity (MVPA), sedentary behavior, and relaxation), perceived workload, emotional exhaustion, and work-life balance. Finally, organizational support and the role of the supervisor on selected observed effects were explored.
METHODS
Design and Study Population
The effectiveness of the intervention was evaluated by comparing outcome measures before and after the intervention (pre-post design). All employees of a division of a Dutch insurance company (mainly white collar workers), with a total of 502 employees including 52 supervisors, were invited to participate. The intervention had a duration of 5 months and was introduced step-wise in five diverse company clusters of the division between September 2012 and May 2014. Before the start of the program, all participants received information about the intervention and were asked to give written informed consent to retrieve information from the intervention measurements and sickness absence data from company records.
Intervention
All five clusters, each having multiple teams, received the same intervention program targeted at (self-) awareness and knowledge on vitality, lifestyle, and physical activity practices to increase self-management to perform healthy behaviors. Different activities were offered at three levels: management, team, and individual, which are shown in Fig. 1. The intervention consisted of a joint kick-off meeting per cluster, two vitality training sessions (both taking half a day) and two workshops (participants could choose out of four different topics) for all employees, training and intervision sessions for supervisors, and opportunities for individual coaching for all employees. Incentives included the distribution of mineral water and fruit, and of the implementation of activities during working hours.
FIGURE 1.
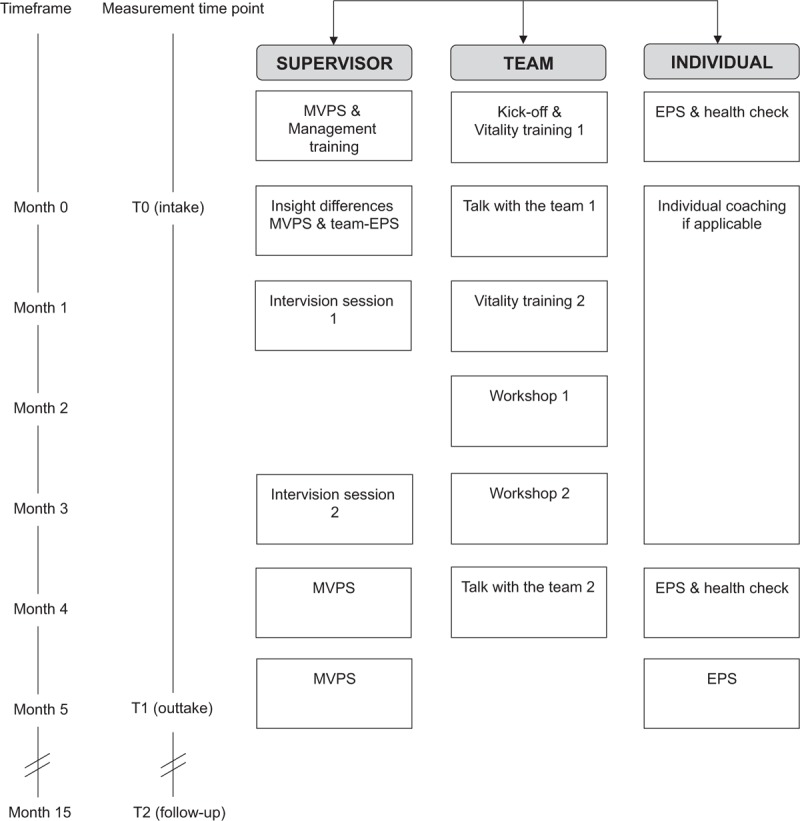
Flow diagram of the intervention program and measurements. EPS, Energy and performance scan; MVPS, management vitality perception Scan.
The program started with internal communication and a kick-off at cluster level to explain the elements of the intervention and enthuse the employees. The individual in- and outtake consisted of an online assessment, the “Energy & Performance Scan” (EPS, a comprehensive questionnaire on vitality, health, and employability) and a series of physical measurements (health check) by a vitality coach. During the intake, the vitality coach indicated, together with the employee, whether individual coaching was desirable. The coaching contained personal advice on vitality, health, lifestyle and quality of life, and individual targets were set. Following the joint kick-off, employees were invited to two vitality training sessions in which they received information on vitality and specific components such as physical and mental energy, stress, and resilience. Afterwards, employees were able to join two interactive workshops of 2 hours, matching their goal or interest. Four workshops were offered: physical activity, mental resilience, healthy nutrition, and mindfulness. Halfway the intervention period, all employees had an evaluation by phone with the vitality coach.
The program activities for the supervisors were similar to the ones described for employees, including the EPS, health check, and individual coaching. Besides the EPS, supervisors were requested to fill in the Management Vitality Perception Scan (MVPS), a questionnaire containing the same elements as the EPS, translated to team level. Additional modules were provided to support supervisors in their role regarding vitality and to strengthen their capacity as a role model. At the start, they received a management training in which all aspects of vitality management were discussed. Halfway and at the end of the intervention, the supervisors had intervision sessions to share and capture experiences and lessons learned. Furthermore, the supervisors were requested to organize two “Talks with the team,” to discuss the intervention program and share ideas for sustained motivation and compliance. Similarities and differences between the results of MVPS and the results of the EPS of the team (summarized scores) were visualized and used as input for discussion during these sessions. In case of questions, the supervisors were referred to the vitality coach.
Measurements
Measurements took place at baseline (T0), at the end of the intervention (T1) and 10 months after finishing the intervention (T2). Data were collected using three measurement tools: the EPS, the MVPS, and a health check. Furthermore, individual sickness absence data from company records were used.
The EPS is a questionnaire, which provides understanding of the vitality, health, and employability of the participant. The questions relate to the primary outcomes vitality, work performance, and presenteeism, and the secondary outcomes self-management, self-rated vitality and health, attitude and intention with regard to healthy behavior, lifestyle, perceived workload, emotional exhaustion, and work-life balance. Several outcomes included dichotomized variables (smoking, alcohol consumption, intention, work-life balance). An overview of the outcome measures of the EPS, the items and response options, the reliability of the scales and the operationalization of the outcome measures can be found in the online only Appendix Table S1. Participants received an auto-generated feedback report to create awareness and stimulate the adoption of a healthy lifestyle. For risk profiling a traffic light model was used. Employees who received orange or red scores (eg, who were not complying to standard guidelines on health and health behavior) were assigned to individual coaching.
In the MVPS, supervisors were asked about the vitality, health, and employability of their team. This information was used as part of the intervention during the “Talks with the team”. In addition, they were asked to describe their perception of the organizational support they received and to evaluate their own role as supervisor regarding vitality (being a role model, stimulating employees, etc). The items used, their operationalization, and the reliability of both of these outcome measures are described in the online only Appendix Table S1.
The health check at T0 and T1 included a series of physical measurements, among which body weight and height, total cholesterol, systolic blood pressure, and fat percentage. Body weight (kg) and fat percentage were measured using a body composition analyzer (Tanita BC601, Tanita Company, Japan), with participants wearing light closing and no shoes. Body height (cm) was measured at baseline with a wall-mounted stadiometer (Seca 222, Seca GmbH & Co, Hamburg, Germany). Body weight, fat percentage, and body height were measured twice, using the mean value of both measurements as outcome measure. BMI was calculated by dividing the body weight (kg) by the square of body height (m2), and categorized as less than 25 kg/m2 and ≥25 kg/m2. Blood pressure (mm Hg) was measured twice with a fully automated blood pressure monitor (Omron M7, Omron Healthcare Europe BV, Hoofddorp, The Netherlands) after the participant had rested for 5 minutes in sitting position. In case the two measurements of the systolic blood pressure differed more than 10 bpm, the blood pressure was measured a third time. The mean value of both systolic blood pressure measurements closest to one another was computed. Total cholesterol level was assessed in non-fasting capillary blood collected by finger stick. Blood was analyzed using an Accutrend Plus (Roche Diagnostics GmbH, Mannheim, Germany). If an increased risk for cardiovascular disease was observed during the health check (eg, high blood pressure), participants were referred to their primary care practitioner.
The percentage sickness absence in a month was based on the number of absence days in a month and the amount of FTE a person was working, using data collected directly from company records. For the analysis, cumulative sickness absence data over 12-months before T0 and T2 were used. The average percentage of sickness absence for each person was calculated over the available months, including only those participants of whom data on sickness absence were available of at least 9 months. Because sickness absence has a skewed distribution with a substantial fraction clustered at the value zero, it was dichotomized into zero (average percentage of sickness absence = 0) and one (average percentage of sickness absence >0).
Statistical Analysis
Continuous outcome measures were analyzed using a linear mixed model. A generalized linear model with a log link was used for sickness absence, smoking, alcohol consumption, emotional exhaustion, attitude and work-life balance. The time variable was used at the first level of the measurement model to investigate whether there was a significant increase or decrease over time (from baseline to T1 and from baseline to T2), with the three time points being T0 (baseline), T1 (after 5 months), and T2 (after 15 months). All models included a random intercept to allow for variation between participants in baseline score. At the second level of the model, effects of covariates were estimated (gender, age [mean centered at 42.2], level of education [low vs. highly educated, ie, bachelor or master degree], and employment size [<36 vs. ≥36 hours a week]). In addition, unadjusted analyses (with only the time variable as predictor) were performed and compared with results from the adjusted analyses.
All participants of whom data were available at baseline, whether or not they completed the study, were included in the analyses. All distributions were considered normal, except for moderate to vigorous physical activity (MVPA) and emotional exhaustion. For MVPA, a square root transformation was taken. Emotional exhaustion was dichotomized into “no emotional exhaustion” and “emotional exhaustion,” based on the cut-off value of 3.2 defined by Schaufeli and van Dierendonck.22
Participants who completed all EPS measurements (“completers”) were compared with background characteristics with participants who had missing measurements at T1 and/or T2 (“dropouts”). Variables were evaluated with independent t tests for continuous variables and chi-square tests for categorical variables. Significant variables could be taken into account in the models to increase the likelihood that the data were missing at random. In addition, we compared “completers” with “dropouts” on the outcome measures at baseline to investigate whether participants with at least one missing measurement scored (already) differently at baseline. Furthermore, we analyzed the dropout pattern and concluded that most participants dropped out after T1 (N = 162). We, therefore, performed an analysis of variance to check whether this specific group differed from the completers in scores at T0 and T1 on the primary outcome measures (sickness absence was only checked for at T0, because this measure was not available at T1). Results from the linear mixed models and generalized linear models (unadjusted) for all outcome measures were compared with results from complete case analyses (sensitivity analysis).
Exploratory analyses were performed on the MVPS data. Mann–Whitney U tests were used to investigate whether teams who dropped out after T0 differed on baseline MVPS scores from teams who had data on both T0 and T1 and/or T0 and T2. Wilcoxon signed rank were used to test whether the median scores of the MVPS (at team level) changed over time (from baseline to T1 and from baseline to T2). The role of the organizational support and the supervisors over time was investigated. Besides, it was examined whether the significant primary outcome measures were related to these MVPS team scores, using independent t test for continuous outcome measures and chi-square tests for binary outcome measures. The binary scores (for T0–T1, and for T0–T2) were calculated for teams, with a zero indicating a deterioration or equality on scores over time, and a one indicating improvement. Only scores of employees who had complete outcome data for T0 and T1, and for T0 and T2, were included. All analyses were performed using SPSS (Version 20.0; Armonk, NY: IBM Corp). Significance for all analyses was determined at P ≤ 0.05 (two-tailed).
RESULTS
In Table 1, the characteristics of the study population are presented. At baseline, 433 participants (86%) provided valid data. A total of 167 participants completed all three measurements, and 266 participants missed T1 and/or T2 (83 dropped out after T0, 21 participants had missed T1 [but not T0 and T2], and 162 participants dropped out after T1). There were no significant differences on any of the baseline characteristics between completers and participants who had missing observations at T1 and/or T2. Since almost all participants were Dutch (98.6%), ethnic background was not taken into account in the analyses. In addition, Table 1 shows the baseline values of the outcomes measures for all participants, “completers,” and “dropouts.” Results of participants who had at least one missing measurement (ie, T1 and/or T2) were comparable to the results of participants who completed all measurements, except for work performance and MVPA. Participants with at least one missing measurement scored significantly lower on these outcome measures than participants who completed all measurements.
TABLE 1.
Characteristics and Outcome Measures# at Baseline of All Participants, Completers, and Participants Who Missed At Least One Measurement (T1 and/or T2)
| All Participants at Baseline (N = 433) | Completers (N = 167) | Participants With Missing Measurements (N = 266) | P^ | |
| Demographic characteristics* | ||||
| Age (years, mean) | 42.2 (8.6) | 42.2 (8.4) | 42.1 (8.8) | 0.98 |
| Gender (% women) | 52.9 | 51.5 | 53.8 | 0.65 |
| Education (% highly educated)a | 66.3 | 63.5 | 61.3 | 0.65 |
| Work status (% ≥36 hours/week) | 62.1 | 67.1 | 65.8 | 0.78 |
| BMI (% ≥25)b | 47.8 | 46.7 | 48.5 | 0.72 |
| Continuous outcomes* | ||||
| Primary outcome measures | ||||
| Vitality (scale 0–6) | 3.9 (0.8) | 3.9 (0.8) | 3.8 (0.8) | 0.34 |
| Work performance (scale 1–5) | 3.6 (0.7) | 3.7 (0.7) | 3.5 (0.7) | 0.02 |
| Presenteeism (scale 1–7) | 5.9 (0.7) | 6.0 (0.6) | 5.9 (0.7) | 0.22 |
| Secondary outcome measures | ||||
| Self-management (scale 4–12) | 7.1 (1.9) | 7.2 (2.0) | 7.1 (1.8) | 0.61 |
| Self-rated vitality (scale 1–10) | 7.1 (1.1) | 7.2 (1.2) | 7.1 (1.1) | 0.19 |
| Self-rated health (scale 1–10) | 7.3 (1.2) | 7.4 (1.2) | 7.2 (1.2) | 0.15 |
| Risk factors for cardiovascular disease | ||||
| Total cholesterol level (mmol/L) | 5.1 (1.0) | 5.1 (0.8) | 5.2 (1.0) | 0.39 |
| Systolic blood pressure (mm Hg) | 131 (18) | 131 (19) | 131 (18) | 0.74 |
| Fat percentage | 28 (8) | 28 (9) | 28 (8) | 0.99 |
| Lifestyle | ||||
| Fruit consumption (days/week) | 3.9 (2.3) | 3.7 (2.4) | 4.0 (2.3) | 0.33 |
| Vegetable consumption (days/week) | 5.0 (1.7) | 4.9 (1.7) | 5.0 (1.7) | 0.41 |
| MVPAc (minutes/week) | 432 (357) | 469 (375) | 409 (344) | 0.03d |
| Sedentary behavior (minutes/working day) | 648 (150) | 643 (148) | 652 (151) | 0.54 |
| Relaxation (scale 1–5) | 3.0 (0.8) | 3.0 (0.8) | 2.9 (0.7) | 0.25 |
| Perceived workload (scale 1–4) | 2.4 (0.5) | 2.4 (0.5) | 2.4 (0.5) | 0.26 |
| Categorical outcomes | ||||
| Primary outcome measure | ||||
| Sickness absencee (% absent) | 48.4 | 47.4 | 49.6 | 0.67 |
| Secondary outcome measures | ||||
| Attitude (% [totally] agree) | 80.4 | 76.0 | 83.0 | 0.19 |
| Intention (% [totally] agree) | 85.7 | 85.6 | 85.7 | 0.98 |
| Lifestyle | ||||
| Smoking (% not smoking) | 80.4 | 83.2 | 78.6 | 0.23 |
| Alcohol consumption (% healthy drinking behavior) | 82.2 | 82.6 | 82.0 | 0.86 |
| Emotional exhaustion (% not exhausted) | 91.2 | 94.6 | 89.1 | 0.05 |
| Work-life balance (% [very] often) | 88.2 | 89.2 | 87.6 | 0.61 |
#Higher values indicate better results, except for risk factors for cardiovascular disease, sedentary behavior, perceived workload, and sickness absence.
^P value for comparing completers with participants with at least one missing measurement; for continuous variables this is the P value from an independent t test, for categorical variables this is the P value from a chi-square test. Significant results are presented in bold.
*Standard deviations are presented between brackets.
aHighly educated = bachelor or master degree.
bBMI, Body Mass Index (kg/m2).
cMVPA, moderate to vigorous physical activity, respondents with MVPA of 0 minute were excluded from the analyses (all participants n = 422, completers n = 161, participants with missing measurements n = 261).
dAnalysis were performed on the log transformed variable.
eRespondents with absence data of at least 9 months were included in the analyses (all participants n = 392, completers n = 154, participants with missing measurements n = 238).
More in detail, to check whether participants who dropped out after T1 differed from the completers on the primary outcome measures at T0 and T1, analysis of variance was performed. No significant differences emerged between these two groups at either time point for the primary outcome measures.
As a result of scheduling all intervention components during working hours, participation rates of the kick-off session, the in- and outtake, the vitality training sessions, and the evaluation by phone were very high (95 to 100%). About 30% of the participants received intensive individual coaching and the interactive workshops were attended by 75% (first workshop) and 54% (second workshop) of the participants.
Table 2 shows the descriptives of the outcome measures at each time point, including the results of the multilevel regression analyses. The random intercept was significant in all multilevel models, which means that there was individual variation in the baseline level of the outcome measures. Results in terms of significant predictors were comparable between the adjusted and unadjusted analyses (in which time was the only predictor variable). Therefore, the results of the unadjusted analyses are shown.
TABLE 2.
Available Number of Participants, Means (SD) of Outcome Measures# at Baseline (T0), at 5 Months (T1) and at 15 Months (T2), and Results of Multilevel Regression Analyses
| Unadjusted Analyses | ||||||||||
| T0 (n = 433) | T1 (n = 329) | T2 (n = 188) | T0–T1 | T0–T2 | ||||||
| Continuous Outcomes | Mean | SD | Mean | SD | Mean | SD | b (95% CI) | P | b (95% CI) | P |
| Primary Outcome Measures | ||||||||||
| Vitality (scale 0–6) | 3.9 | 0.8 | 3.9 | 0.8 | 4.0 | 0.8 | 0.03 (−0.03;0.09) | 0.385 | 0.08 (0.00;0.15) | 0.039 |
| Work performance (scale 1–5) | 3.6 | 0.7 | 3.7 | 0.6 | 3.7 | 0.6 | 0.12 (0.06;0.19) | <0.001 | 0.15 (0.08;0.23) | <0.001 |
| Presenteeism (scale 1–7) | 5.9 | 0.7 | 6.0 | 0.6 | 6.0 | 0.7 | 0.03 (−0.03;0.10) | 0.298 | 0.03 (−0.05;0.11) | 0.403 |
| Secondary outcome measures | ||||||||||
| Self-management (scale 4–12) | 7.1 | 1.9 | 7.9 | 1.7 | 7.9 | 1.7 | 0.87 (0.70;1.05) | <0.001 | 0.77 (0.55;0.98) | <0.001 |
| Self-rated vitality (scale 1–10) | 7.1 | 1.1 | 7.5 | 1.0 | 7.4 | 1.1 | 0.30 (0.19;0.41) | <0.001 | 0.24 (0.10;0.38) | 0.001 |
| Self-rated health (scale 1–10) | 7.3 | 1.2 | 7.6 | 1.0 | 7.5 | 1.2 | 0.26 (0.15;0.37) | <0.001 | 0.17 (0.04;0.31) | 0.013 |
| Risk factors for cardiovascular disease | ||||||||||
| Total cholesterol level (mmol/L) | 5.1 | 1.0 | 5.1 | 1.0 | na | −0.00 (−0.08;0.07) | 0.93 | na | na | |
| Systolic blood pressure (mm Hg) | 131 | 18 | 126 | 16 | na | −4.31 (−5.73;−2.90) | <0.001 | na | na | |
| Fat percentagea (%) | 28 | 8 | 28 | 8 | na | −0.29 (−0.58;0,00) | 0.053 | na | na | |
| Lifestyle | ||||||||||
| Fruit consumption (days/week) | 3.9 | 2.3 | 4.4 | 2.3 | 4.5 | 2.1 | 0.63 (0.44;0.82) | <0.001 | 0.65 (0.41;0.89) | <0.001 |
| Vegetable consumption (days/week) | 5.0 | 1.7 | 5.1 | 1.5 | 5.2 | 1.4 | 0.20 (0.05;0.35) | 0.007 | 0.24 (0.06;0.42) | 0.009 |
| MVPAb (minutes /week) | 432 | 357 | 453 | 305 | 465 | 278 | 0.76 (0.14;1.37)c | 0.015 | 0.76 (−0.01;1.52)c | 0.052 |
| Sedentary behavior (minutes/working day) | 648 | 150 | 613 | 136 | 610 | 138 | −32.84 (−50.10;−15.59) | <0.001 | −34.53 (−55.83;−13.24) | 0.002 |
| Relaxation (scale 1–5) | 3.0 | 0.8 | 3.1 | 0.8 | 3.1 | 0.7 | 0.12 (0.05;0.18) | 0.001 | 0,07 (−0.01;0.16) | 0.081 |
| Perceived workload (scale 1–4) | 2.4 | 0.5 | 2.4 | 0.5 | 2.4 | 0.5 | −0.00 (−0.05;0.04) | 0.962 | −0,00 (−0.06;0.06) | 0.976 |
| Categorical outcomes | % | % | % | OR (95% CI) | P | OR (95% CI) | P | |||
| Primary outcome measure | ||||||||||
| Sickness absenced (% absent) | 48.4 | na | 32.0 | na | na | 0.51 (0.33;0.80) | 0.003 | |||
| Secondary outcome measures | ||||||||||
| Attitude (% [totally] agree) | 80.4 | 98.2 | 98.9 | 2.37 (1.70;3.31) | <0.001 | 2.46 (1.65;3.67) | <0.001 | |||
| Intention (% [totally] agree) | 85.7 | 86.9 | 80.3 | 1.06 (0.76;1.48) | 0.719 | 0.77 (0.52;1.15) | 0.196 | |||
| Lifestyle | ||||||||||
| Smoking (% not smoking) | 80.4 | 81.8 | 87.2 | 1.07 (0.77;1.49) | 0.688 | 1.4 (0.94;2.08) | 0.098 | |||
| Alcohol consumption (% healthy drinking behavior) | 82.2 | 87.2 | 87.2 | 1.28 (0.92;1.78) | 0.149 | 1.28 (0.86;1.90) | 0.227 | |||
| Emotional exhaustion (% not exhausted) | 91.2 | 91.2 | 93.1 | 1.00 (0.72;1.40) | 0.991 | 1.1 (0.74;1.63) | 0.654 | |||
| Work-life balance (% [very] often) | 88.2 | 91.5 | 96.3 | 1.17 (0.84;1.63) | 0.347 | 1.48 (1.00;2.20) | 0.052 | |||
Bold, significant change; CI, confidence interval; Max, maximum; Min, minimum; na, not available; SD, standard deviation.
#Higher values indicate better results, except for risk factors for cardiovascular disease, sedentary behavior, perceived workload, and sickness absence.
aOne person was excluded from the analysis due to a (unrealistic) percentage of 65 at follow-up.
bMVPA, moderate to vigorous physical activity; respondents with MVPA of 0 minute were excluded from the analyses (n = 16 participants: T0: n = 11, T1: n = 5, T2: n = 4).
cAnalysis were performed on the square root transformed variable.
dRespondents with absence data of at least 9 months were included in the analyses (T0 = 392, T2 = 143).
Positive outcomes were observed for the primary outcomes measures vitality, work performance, and sickness absence on the long-term (T0–T2). The positive effect on work performance was already seen on the short-term, directly after the intervention (T0–T1). No significant changes were observed for vitality on the short-term and for presenteeism on the short- and long-term. Regarding secondary outcomes, self-management, self-rated vitality, self-rated health, and attitude showed positive results (T0–T1 and T0–T2). Risk factors for cardiovascular disease were only measured at T0 and T1 and positive changes for systolic blood pressure were observed (T0–T1). Regarding lifestyle factors, outcome measures fruit and vegetable intake, MVPA, sedentary behavior, and relaxation showed improvements between T0 and T1. For fruit and vegetable intake, and sedentary behavior this effect was still present at T2.
Sensitivity analyses based on complete cases (N = 167) showed comparable results in terms of significance and parameter estimates (results not shown). Two exceptions were found; for work performance and MVPA no (significant) improvements were found between T0 and T1 for the complete cases. For vitality, only a trend (P = 0.06) was found for improvement between T0 and T2 for completers, which is very plausible due to the reduced sample size since parameter estimates are equal.
At baseline, MVPS data were available of 33 different teams (Table 3). Sixteen teams completed all three measurements, and 17 teams missed T1 and/or T2. Of those 17 teams, 11 dropped out after T0, 4 teams had missed T1 (but not T0 and T2), and 2 teams dropped out after T1. Analysis on the MVPS data showed that teams who dropped out after baseline (N = 11) did not differ significantly from teams who were included in the analyses (results not shown). A significant improvement on median scores on organizational support (T0–T1 and T0–T2) as well as on the role of the supervisors (T0–T2) was shown in those teams who had complete data for T0–T1 and T0–T2, respectively.
TABLE 3.
Median (IQR) Scores of the MVPS#, Averaged Over Teams, at Baseline (T0), After 5 Months (T1), and at 15 Months (T2)§
| T0 (n = 33) | T1 (n = 18) | T2 (n = 20) | |
| Med [IQR] | Med [IQR] | Med [IQR] | |
| Organizational support (scale 1–10) | 7.4 [6.4;8.1] | 8.2 [7.6;8.9]* | 8.0 [7.0;9.0]** |
| Role of the supervisors (scale 1–10) | 7.4 [6.8;8.3] | 8.1 [7.2;8.7] | 8.0 [7.4;8.9]* |
IQR, interquartile range; Med, median; MVPS, Management Vitality Perception Scan.
#Higher values indicate better results.
§Analyses were performed for those teams who had complete data for T0–T1 and T0–T2, respectively.
*P < 0.05.
**P < 0.01.
When studying the relation between the primary outcome measures that improved significantly during the intervention and changes in the team scores of the MVPS, significant associations were found for sickness absence. Individual records on sickness absence were associated with team scores on organizational support over time (χ2 (1) = 9.823, P < 0.01): employees who were not or less absent at T2, were more often part of a team with improved scores on organizational support. A similar relation was found for the role of the supervisor (χ2 (1) = 10.825, P < 0.01): employees who were not or less absent at T2, were more often part of a team with improved scores on the role of the supervisor. No significant relation was found between long-term difference scores on vitality and team scores on organizational support (t(87) = 0.426, P > 0.1) or the role of the supervisor (t(87) = 1.472, P > 0.1. Also, there was no significant relation between work performance on the short (T0–T1) or long-term (T0–T2), and organizational support (t(163) = 1.066, P > 0.05 and t(87) = 1.652, P > 0.1, respectively) or the role of the supervisor (t(163) = 0.052, P > 0.1 and t(87) = 1.837, P > 0.05, respectively).
DISCUSSION
This study showed a significant effect of the WHPP on the primary outcome measures vitality (long-term), work performance (directly after the intervention as well as on the long-term), and sickness absence (long-term). No significant effect on presenteeism was found. Self-management, an important secondary outcome measure for performing healthy behavior, also significantly increased after the intervention as well as on the long-term. Furthermore, significant effects were observed for some other vitality and health-related outcome measures (self-rated vitality, self-rated health, attitude, systolic blood pressure, fruit and vegetable consumption, MVPA, sedentary behavior, and relaxation). In general, significant improvements were observed on median scores of organizational support and the role of the supervisor (only on the long-term). More specifically, an association between sickness absence and perceived organizational support and the supervisors’ role was found.
In contrast to the results of all participants, results from participants who completed all three measurements showed no significant improvement on the short-term on MVPA. However, this group of employees already showed a significantly higher baseline score on MVPA compared with employees with at least one missing measurement. This relatively high baseline score of the completers leaves little room for improvement, which might be a reason for the lack of a significant short-term effect. A comparable contrast was found for work performance: the significant short-term improvement of all participants was not observed in the group of participants who completed all three measurements, and the completers showed a significantly higher baseline score on work performance compared with employees with at least one missing measurement. The significant short-term effect we have found using all employees might be caused by the lower baseline scores for employees with at least one missing measurement (employees scored comparable at T1).
In the literature, program outcomes of WHPP are typically distinct by three main categories as described by Goetzel et al23: improvements in the health and well-being of employees; enhanced individual and business performance; and cost savings. This intervention showed positive results on both the first and second category, the third was not examined.
The primary outcome measure vitality relates to the first category of program outcomes. Vitality consists of both physical (high energy levels and feeling strong and fit) and mental factors (well-being, fatigue, resilience, and perseverance).13 The observed positive long-term effect on vitality was not in correspondence with other WHPPs targeting vitality, which did not find significant effects.13,24–26 Although these studies used the same measurement instrument, that is, the Utrecht Work Engagement Scale questionnaire,19 comparison of the results is hampered by the fact that in our study the Utrecht Work Engagement Scale was adapted to a non-work context. In the study of Strijk et al,13 general vitality was also measured using the RAND-36 vitality scale,27 and although general vitality improved at 12-months follow-up compared with the control group, this was not statistically significant. The fact that the participants were relatively healthy was mentioned as a possible explanation of the lack of significant effects on vitality in these studies. Their mean baseline values on vitality corresponded to the upper limit range of the scale (between 4.6 and 5.2), probably resulting in a ceiling effect. These values were substantially higher than the baseline values of our study (almost 3.9), which provided more room for improvement. Furthermore, in the study of Van Scheppingen et al,25 the intervention aimed at inducing a self-regulatory health-promotion social change process was found to be effective in openness toward health and vitality at work. Like in our study, they used self-management as one of the main principles in their approach. In their historical overview on self-management, Lorig and Holman present evidence of the effectiveness of self-management interventions, referring to programs that reached significantly improved healthful behaviors.16
The other primary outcomes—work performance, presenteeism, and sickness absence—relate to the category individual and business performance.23 The positive effect on sickness absence is in coherence with other studies indicated by systematic reviews.3,5,11 The observed significant decrease of sickness absence was not expected, because the average percentage sickness absence was already relatively low at baseline (just above 2%).
The significant improved work performance at both short- and long-term is not confirmed by Lerner et al.28 In their review on the economic impact of WHPPs, they concluded that at-work performance and productivity loss are the least studied outcome measures and evidence regarding these outcomes is limited and inconsistent. According to the authors, this may reflect the relatively recent widespread adoption of these measures in health assessment surveys. However, in a recent study also using the Individual Work Performance Questionnaire,20 including the sub-set of questionnaire items of the current study, a significant but small improvement was found compared with the control group.26 The fact that relatively low organizational and supervisor support for the intervention was found, was mentioned by the authors as a possible explanation of finding small effects. The significant effect on work performance in our study might be attributed to the fact that the WHPP was more adequately embedded within the organization. This result might be a first indication that WHPP can improve work performance, but high quality research is needed to confirm these findings.
The lack of effect on presenteeism is difficult to relate to other intervention studies, since the literature is young and heterogeneous, and presenteeism is a difficult outcome variable to measure.12 The lack of consensus in measuring presenteeism has resulted in a multitude of instruments with heterogeneous content.29 Furthermore, many of these instruments are specifically developed for workers with health complaints making them unsuitable for general employee populations.30 There is preliminary evidence that some WHPP can positively affect presenteeism. Programs that were successful offered organizational leadership, health risk screening, individually tailored programs, and a supportive workplace culture.12 Although these aspects were also offered in the current intervention, they did not result in a positive effect on presenteeism. Possibly, when a reliable and validated questionnaire for presenteeism had been available at the start of this study, similar results could have been found in our study too.
Regarding the secondary outcomes, no significant effects were found for intention, risk factors for cardiovascular disease (cholesterol level, fat percentage), lifestyle (smoking, alcohol consumption, long-term MVPA), long-term relaxation, emotional exhaustion, work-life balance, and perceived workload. The lack of effects could be explained by the difficulty to change these indicators in a 5-month intervention. Goetzel and Ozminkowski17 reviewed the state-of-the-art in work site health promotion and emphasized the assurance of sufficient duration of programs of at least 1 to 3 years to bring about risk reductions among employees and measure health and financial benefits. With regard to perceived workload, the fact that the intervention focused primary on vitality and health determinants using training, workshops, and coaching and was not aimed at decreasing workload, might explain the lack of effect on perceived workload.
The WHPP showed improvements on organizational support and the role of the supervisor, which was an important element of this intervention. A relation with sickness absence was found, which is confirmed by other studies that show leadership style can reduce absenteeism.31 As by demonstrating higher levels of job satisfaction and commitment32 or providing support to provide an environment in which the employee is more likely to attend work.33 No relation between organizational support and the role of the supervisor with vitality and work performance was found, which could be clarified by the importance of the role of the employees themselves (eg, their feeling about the ability to perform and achieve organizational goals) besides the supervisors’ style.34
Strengths and Limitations
A major strength of this study is the inclusion of a variety of activities on both the individual, as well as the team and management level, which is in coherence with elements of most effective programs in the literature. This relates to offering individualized risk-reduction counseling to the highest risk employees, within the context of a broader health awareness program, and a “healthy company” culture.17 Furthermore, the longitudinal design with a long-term follow-up measurement after 10 months, including work-related outcomes measures as well as a large number of measurements concerning health and health behavior, offered the opportunity to evaluate its effect on important primary and secondary outcomes, including self-management. It is also one of the few studies examining the influence of attitude and behavior of the supervisor on the observed effects of a WHPP.
An important limitation is the lack of a control group. The participating company wanted to involve all employees in a relatively short period of time, which made it impossible to use teams that did not receive the intervention at the start of the study as control group. As a result, it is not possible to directly link the results to the intervention. Another methodological limitations are the questions used in the EPS. Although the EPS is based on questions from validated questionnaires, most of them were adapted to fit the target audience. As a result, the scientific validity is most likely lower compared with the original questionnaires. Besides, several questions were developed specifically for this study and some of them contained only one item (self-rated vitality and health, attitude, intention, and work-life balance). This may have contributed to less reliable findings and, therefore, the results should be interpreted with caution.
Furthermore, the high dropout rate of employees during the intervention might have biased the results, although we found similar results for most outcome measures using data from employees with data at all measurements points.35 Dropout is commonly encountered in health promotion programs. Explanations of the high dropout in this study could be related to both personal as well as organizational factors. Groeneveld et al36 investigated factors for non-participation and dropout in lifestyle interventions for employees and results showed that main reasons for dropout were “lack of motivation,” “current (para-) medical treatment,” and “disappointment.” With regard to this particular WHPP, a reorganization that took place shortly after the intervention could have been an important organizational factor for dropout. This made it impossible to collect data at T2 of participants who were no longer working for the company.
Recommendations
Our conclusions on the effect of this WHPP must be considered preliminary, because of the limitations of the current study. Nevertheless, for future development of WHPPs, including all organizational levels (manager, team, individual) and using multiple intervention elements to increase vitality, health, and work-related outcomes might be worthwhile. Increasing self-management by using elements as goal setting, action planning, reflective counseling, and stimulating ownership, and responsibility, seems to be relevant. To effectuate health improvements on the long-term, a short intensive intervention period, similar to the current program, should be observed by a medium to low intensity program for the following years, up to 5 years after the program. Ideally, health promotion is structurally part of the daily work routine of employees. For future research, it is recommended to develop high-quality evaluation studies including a control group and validated outcome measures to confirm the observed effects of the current study. Finally, as company decision makers are not only interested in the effectiveness of the interventions, it is also recommended to explore the cost-effectiveness and cost-benefits.
CONCLUSIONS
This new 5-month multilevel WHPP, focusing on improvement of self-management, provided promising results on vitality, work performance, and sickness absence. Significant effects were also observed for self-rated vitality and health, attitude, systolic blood pressure, and several lifestyle factors. Organizational support and the role of the supervisor seemed to be important, especially in relation to sickness absence. As a result, it is recommended to include all organizational levels and use multiple interventions that increase self-management in future WHPPs. The current findings are preliminary and should be confirmed using high-quality studies that include examination of cost-effectiveness and cost-benefits.
Supplementary Material
Acknowledgments
The authors want to acknowledge the company and the employees that participated in the study, and the authors kindly thank Hilco Regterschot (Pim Mulier) and Ernest de Vroome (TNO) for collecting and preparing the data. Vincent Hildebrandt provided significant support in initiating the project and allocating resources to it.
Footnotes
This project was supported by the Stichting Achmea Gezondheidszorg (SAG, Leiden, The Netherlands), who made it possible to develop and implement the innovative WHPP, and who funded this effectiveness study.
List of the authors’ contribution to the study: IH, MS and V. Hildebrandt conceived the study. IH and BdK drafted the initial manuscript and HH performed the statistical analysis. MS and JvV provided intellectual input. All authors have read and approved the final version of the manuscript. The authors declare that they have no competing interests.
The authors declare no conflicts of interest.
REFERENCES
- 1.Holmqvist M. Corporate social responsibility as corporate social control: the case of work-site health promotion. Scand J Manag 2009; 25:68–72. [Google Scholar]
- 2.WHO/WEF (2013). World Economic Forum. The Workplace Wellness Alliance Making the Right Investment: Employee Health and the Power of Metrics. Report, January 2013. https://www.weforum.org/reports/workplace-wellness-alliance-making-right-investment-employee-health-and-power-metrics Accessed April 8, 2016. [Google Scholar]
- 3.Rongen A, Robroek SJ, van Lenthe FJ, Burdorf A. Workplace health promotion: a meta-analysis of effectiveness. Am J Prev Med 2013; 44:406–415. [DOI] [PubMed] [Google Scholar]
- 4.Groeneveld IF, Proper KI, van der Beek AJ, Hildebrandt VH, van Mechelen W. Lifestyle-focused interventions at the workplace to reduce the risk of cardiovascular disease - a systematic review. Scand J Work Environ Health 2010; 36:202–215. [DOI] [PubMed] [Google Scholar]
- 5.Kuoppala J, Lamminpää A, Husman P. Work health promotion, job well-being, and sickness absences—a systematic review and meta-analysis. J Occup Environ Med 2008; 50:1216–1227. [DOI] [PubMed] [Google Scholar]
- 6.Martin A, Sanderson K, Cocker F. Meta-analysis of the effects of health promotion intervention in the workplace on depression and anxiety symptoms. Scand J Work Environ Health 2009; 35:7–18. [DOI] [PubMed] [Google Scholar]
- 7.Conn VS, Hafdahl AR, Cooper PS, Brown LM, Lusk SL. Meta-analysis of workplace physical activity interventions. Am J Prev Med 2009; 37:330–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hutchinson AD, Wilson C. Improving nutrition and physical activity in the workplace: a meta-analysis of intervention studies. Health Promot Int 2012; 27:238–249. [DOI] [PubMed] [Google Scholar]
- 9.Maes L, van Cauwenberghe E, van Lippevelde W, et al. Effectiveness of workplace interventions in Europe promoting healthy eating: a systematic review. Eur J Public Health 2012; 22:677–683. [DOI] [PubMed] [Google Scholar]
- 10.Malik SH, Blake H, Suggs LS. A systematic review of workplace health promotion interventions for increasing physical activity. Br J Health Psychol 2014; 19:149–180. [DOI] [PubMed] [Google Scholar]
- 11.Chapman LS. Meta-evaluation of worksite health promotion economic return studies: 2012 update. Am J Health Promot 2012; 26:TAH1–TAH12. [DOI] [PubMed] [Google Scholar]
- 12.Cancelliere C, Cassidy JD, Ammendolia C, Côté P. Are workplace health promotion programs effective at improving presenteeism in workers? A systematic review and best evidence synthesis of the literature. BMC Public Health 2011; 11:395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Strijk JE, Proper KI, van Mechelen W, van der Beek AJ. Effectiveness of a worksite lifestyle intervention on vitality, work engagement, productivity, and sick leave: results of a randomized controlled trial. Scand J Work Environ Health 2013; 39:66–75. [DOI] [PubMed] [Google Scholar]
- 14.Fugate M, Kinicki AJ, Ashforth BE. Employability: a psycho-social construct, its dimensions, and applications. J Vocat Behav 2004; 65:14–38. [Google Scholar]
- 15.WHO/WEF (2008). Preventing Noncommunicable Diseases in the Workplace Through Diet and Physical Activity. WHO/World Economic Forum Report of a joint event. Report, 2008. http://whqlibdoc.who.int/publications/2008/9789241596329_eng Accessed April 8, 2016. [Google Scholar]
- 16.Lorig KR, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med 2003; 26:1–7. [DOI] [PubMed] [Google Scholar]
- 17.Goetzel RZ, Ozminkowski RJ. The health and cost benefits of work site health-promotion programs. Annu Rev Public Health 2008; 29:303–323. [DOI] [PubMed] [Google Scholar]
- 18.Lovato CY, Green LW. Maintaining employee participation in workplace health promotion programs. Health Educ Q 1990; 17:73–88. [DOI] [PubMed] [Google Scholar]
- 19.Schaufeli W, Bakker AB. Utrecht work engagement scale. Utrecht Preliminary Manual 2003; Available at: http://www.wilmarschaufeli.nl/publications/Schaufeli/Test%20Manuals/Test_manual_UWES_English.pdf. Accessed April 8, 2016. [Google Scholar]
- 20.Koopmans L, Bernaards CM, Hildebrandt VH, van Buuren S, van der Beek AJ, de Vet HCW. Development of an individual work performance questionnaire. Int J Prod Perform Manage 2013; 62:6–28. [Google Scholar]
- 21.Nationale Enquête Arbeidsomstandigheden (NEA) 2013. [Netherlands Working Conditions Survey 2013]. http://www.monitorarbeid.tno.nl/publicaties/nea-2013 Accessed April 8, 2016. [Google Scholar]
- 22.Schaufeli W, van Dierendonck D. Handleiding van de Utrechtse Burnout Schaal (UBOS). [Manual of the Utrecht Burnout Scale (UBOS)]. Lisse: Swets & Zeitlinger; 2000. [Google Scholar]
- 23.Goetzel RZ, Henke RM, Tabrizi M, et al. Do workplace health promotion (wellness) programs work? J Occup Environ Med 2014; 56:927–934. [DOI] [PubMed] [Google Scholar]
- 24.Viester L, Verhagen EA, Bongers PM, van der Beek AJ. The effect of a health promotion intervention for construction workers on work-related outcomes: results from a randomized controlled trial. Int Arch Occup Environ Health 2015; 88:789–798. [DOI] [PubMed] [Google Scholar]
- 25.Van Scheppingen AR, de Vroome EM, ten Have KC, Zwetsloot GJ, Wiezer N, van Mechelen W. Vitality at work and its associations with lifestyle, self-determination, organizational culture, and with employees’ performance and sustainable employability. Work 2015; 52:45–55. [DOI] [PubMed] [Google Scholar]
- 26.Coffeng JK, Hendriksen IJ, Duijts SF, Twisk JW, van Mechelen W, Boot CR. Effectiveness of a combined social and physical environmental intervention on presenteeism, absenteeism, work performance, and work engagement in office employees. J Occup Environ Med 2014; 56:258–265. [DOI] [PubMed] [Google Scholar]
- 27.Van der Zee KI, Sanderman R. Het meten van gezondheidstoestand met de RAND-36: een handleiding [Measurerement of health status using the RAND-36 questionnaire: a practical manual]. Groningen: Noordelijk Centrum voor Gezondheidsvraagstukken; 1993. [Google Scholar]
- 28.Lerner D, Rodday AM, Cohen JT, Rogers WH. A systematic review of the evidence concerning the economic impact of employee-focused health promotion and wellness programs. J Occup Environ Med 2013; 55:209–222. [DOI] [PubMed] [Google Scholar]
- 29.Ospina MB, Dennett L, Waye A, Jacobs P, Thompson AH. A systematic review of measurement properties of instruments assessing presenteeism. Am J Manag Care 2015; 21:e171–e185. [PubMed] [Google Scholar]
- 30.Koopmans L, Bernaards CM, Hildebrandt VH, de Vet HC, van der Beek AJ. Measuring individual work performance—identifying and selecting indicators. Work 2014; 48:229–238. [DOI] [PubMed] [Google Scholar]
- 31.Elshout R, Scherp E, van der Feltz-Cornelis CM. Understanding the link between leadership style, employee satisfaction, and absenteeism: a mixed methods design study in a mental health care institution. Neuropsychiatr Dis Treat 2013; 9:823–837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Walumbwa FO, Wang P, Lawler JJ, Shi K. The role of collective efficacy in the relations between transformational leadership and work outcomes. J Occup Organ Psych 2004; 77:515–530. [Google Scholar]
- 33.Tharenou P. A test of reciprocal causality for absenteeism. J Organ Behav 1993; 14:269–290. [Google Scholar]
- 34.McColl-Kennedy JR, Anderson RD. Impact of leadership style and emotions on subordinate performance. Leadership Quart 2002; 13:545–559. [Google Scholar]
- 35.Higgins JPT, Green S. (eds). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration; 2011:H8.13.1. Available at: www.cochrane-handbook.org Accessed April 8, 2016. [Google Scholar]
- 36.Groeneveld IF, Proper KI, van der Beek AJ, Hildebrandt VH, van Mechelen W. Factors associated with non-participation and drop-out in a lifestyle intervention for workers with an elevated risk of cardiovascular disease. Int J Behav Nutr Phys Act 2009; 6:80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


